 Statin Drug Side Effects: Symptoms and Support Strategies
Statin Drug Side Effects: Symptoms and Support Strategies
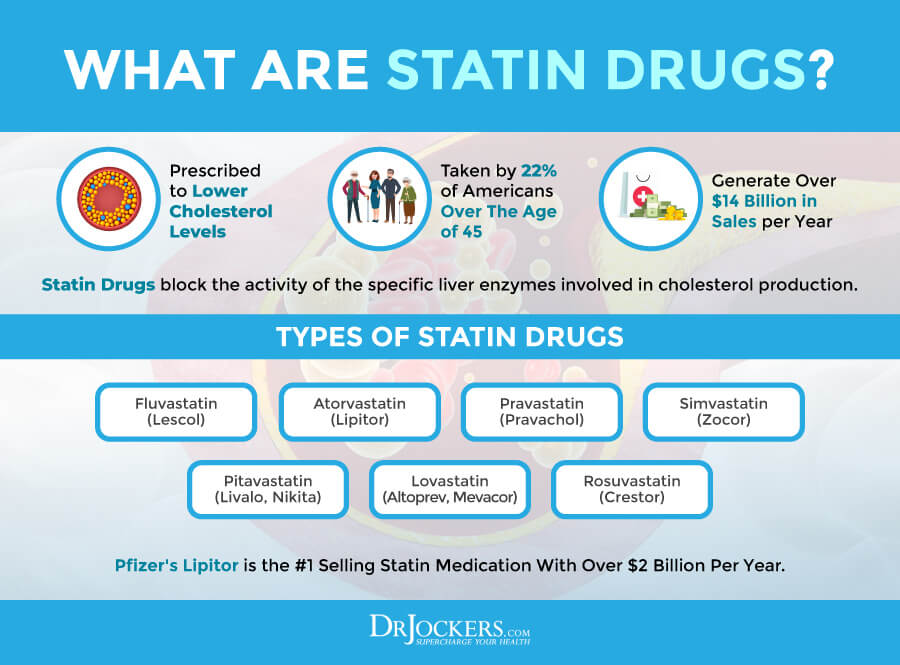
Statin drugs are some of the most commonly prescribed medications. They are used to lower your bad cholesterol levels and supposedly reduce your risk of cardiovascular disease, heart attacks, and stroke. Statin drugs may be common, but they don’t come without side effects. There are some fantastic natural support strategies that you can use to protect your health and reduce your risk of statin drug side effects or needing the medication in the first place.
In this article, you will learn about statin drugs. You will understand what statin drugs are and how they work. I will discuss common side effects and major risk factors for these side effects from statin drugs. You will learn about how statin drugs may damage your mitochondrial function. I will discuss whether or not high cholesterol is really a problem. I will also offer some natural support strategies to help you overcome statin drug side effects.
What Are Statin Drugs?
Statins are a type of medication that is commonly used to lower low-density lipoprotein (LDL), or bad cholesterol, reduce the risk of cardiovascular disease and stroke, and prevent cardiovascular disease from getting worse. They may also help protect your arteries and improve your high-density lipoprotein (HDL) or good cholesterol levels (1).
There are seven types of statin drugs available on the market today that are currently approved by the US Food and Drug Administration (FDA). They include fluvastatin, atorvastatin (Lipitor), pravastatin (Pravachol), simvastatin (Zocor), pitavastatin (Livalo, Nikita), lovastatin (Altoprev, Mevacor), and rosuvastatin (Crestor) (1).
Statins are the most commonly prescribed pharmaceutical drugs in the world. While most people don’t experience too many noticeable adverse side effects, some people experience some negative side effects that can interfere with their daily lives. There are also some risk factors that you need to know about that I will go over in this article.
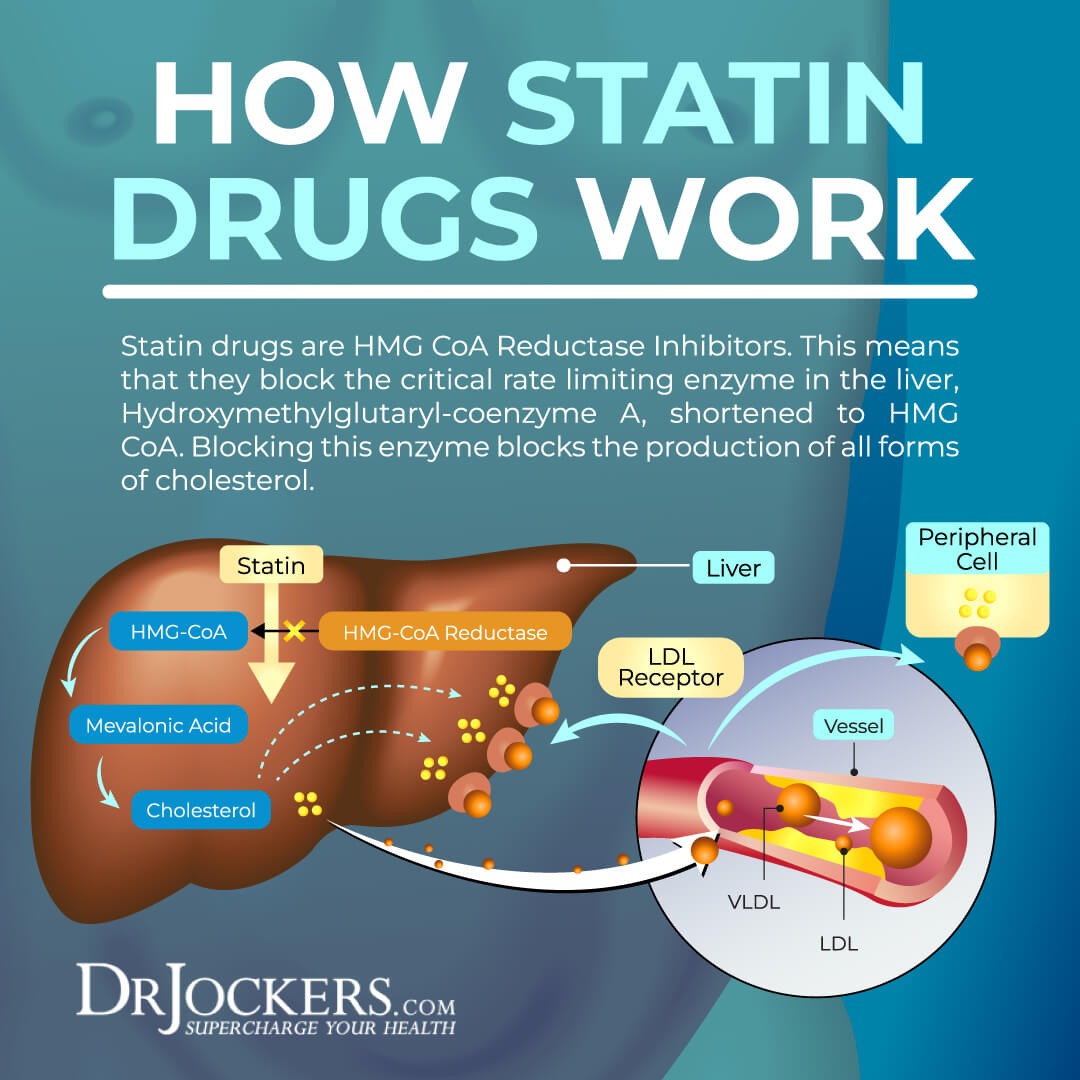
How Do Statin Drugs Work?
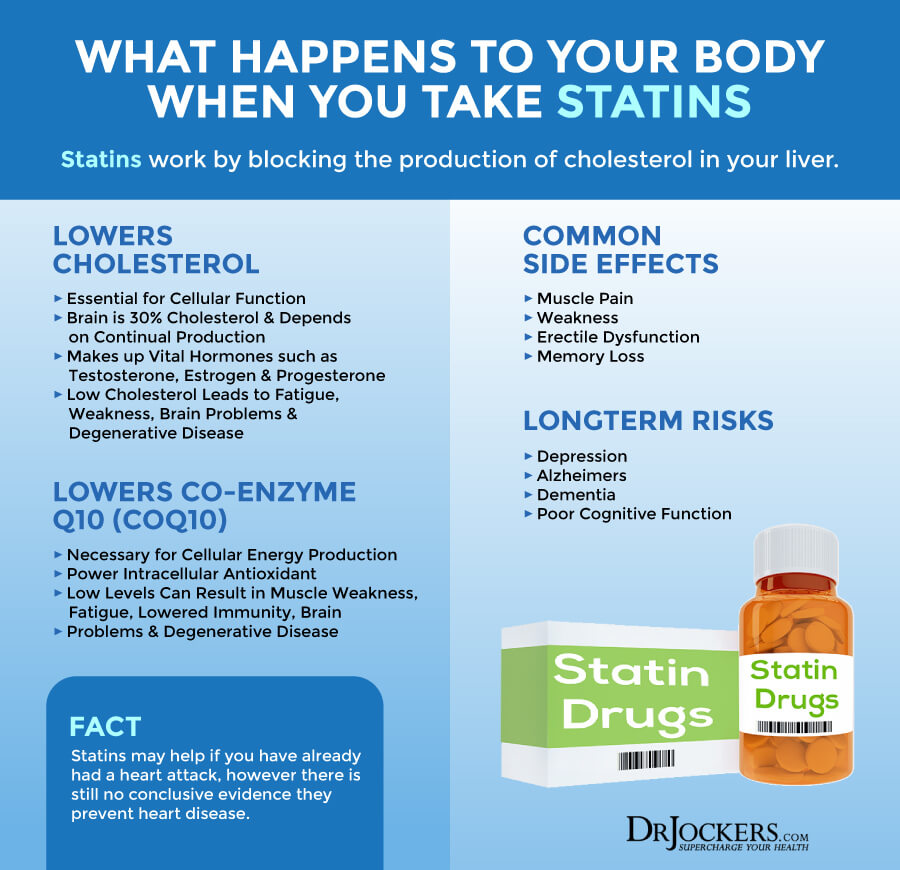
Statin drugs block the activity of the specific liver enzyme, HMG CoA Reductase, that is in charge of cholesterol production. The general theory is that if you have too much cholesterol in your blood, it can result in plaque buildup on the artery walls, which can lead to the narrowing or hardening of your arteries.
This increases the risk of blood clots, heart disease, heart attacks, and stroke. By reducing cholesterol production, the idea is that statins lower the chance of plaque buildup, and consequently, blood clots, heart disease, heart attacks, and stroke. But is this theory true and does reducing cholesterol production really save lives?
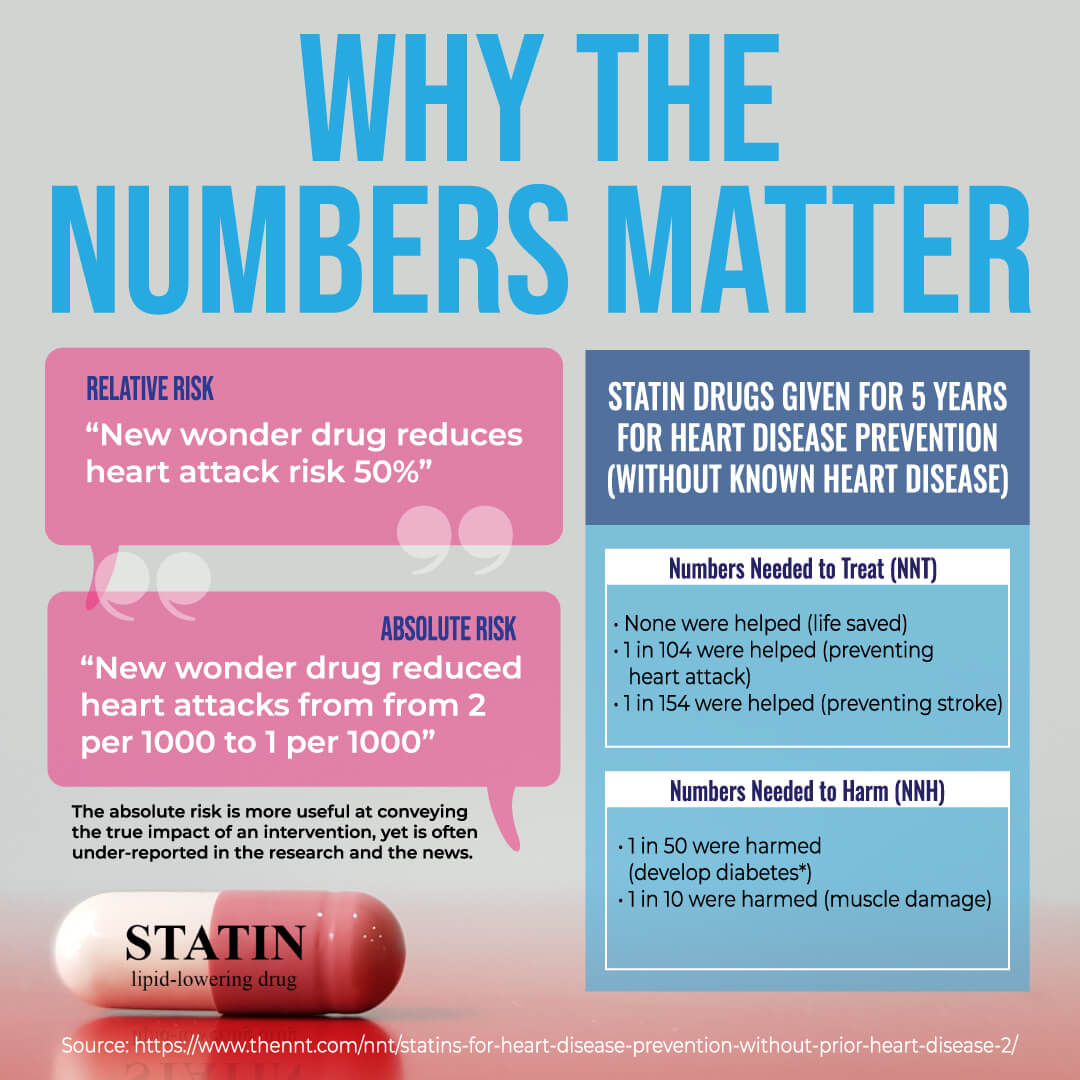
A 2017 study published in Circulation found that statin drugs can decrease coronary heart disease-related death by 28 percent in men (20). While this may sound great, once you dig deeper into the research, it may not be as impressive.
There is a difference between relative and absolute risk. Let’s say, Drug A can reduce your risk of developing your risk of a condition by 0.5 percent. That’s your absolute risk. On the other hand, Drug B can decrease your risk by bringing it down from 0.5 to 0.25 percent.
How do you report this? There is two way to go about this. Your relative risk was lowered by 50 percent from 0.5 to 0.25 percent when using Drug B. Or you can report the absolute risk, which means that Drug B only lowered the risk by a mere 0.25 percent. Reporting the relative risk sounds much more impressive and can inflate the benefits of a medication or other treatment. This is what happened with statin drug studies as well.
Are Statin Drugs Effective?
A 2017 meta-analysis published in Lancet looked at 26 randomized trials (21). They found that statin drugs can decrease mortality by 10 percent for every 39 mg/dL. However, if you look at the trials closer, the mortality rates went from 2.3 to 2.1 percent for every 39 mg/dL resulting in only a 0.2 percent absolute risk reduction. Looking at vascular-related death, statin drugs only decreased death from 1.3 to 1.2 percent.
Of course, every single life matters. Some may argue that even 0.2 percent risk reduction matters. But if we are looking at the big picture, 98.2 out of 100 high-risk people will not see any heart health benefits from statin drugs. The 1.8 remaining individuals who do see benefits, will only live about 6 months longer on average and a maximum of one year longer versus those who didn’t take statin drugs.
Not to mention, that these statistics are only true for high-risk individuals, middle-aged men who have already had at least one heart attack. There is currently not much evidence that statin drugs can benefit men without pre-existing heart disease. There is also no evidence that they can help women with or without a heart condition.
 Major Side Effects of Statin Drugs
Major Side Effects of Statin Drugs
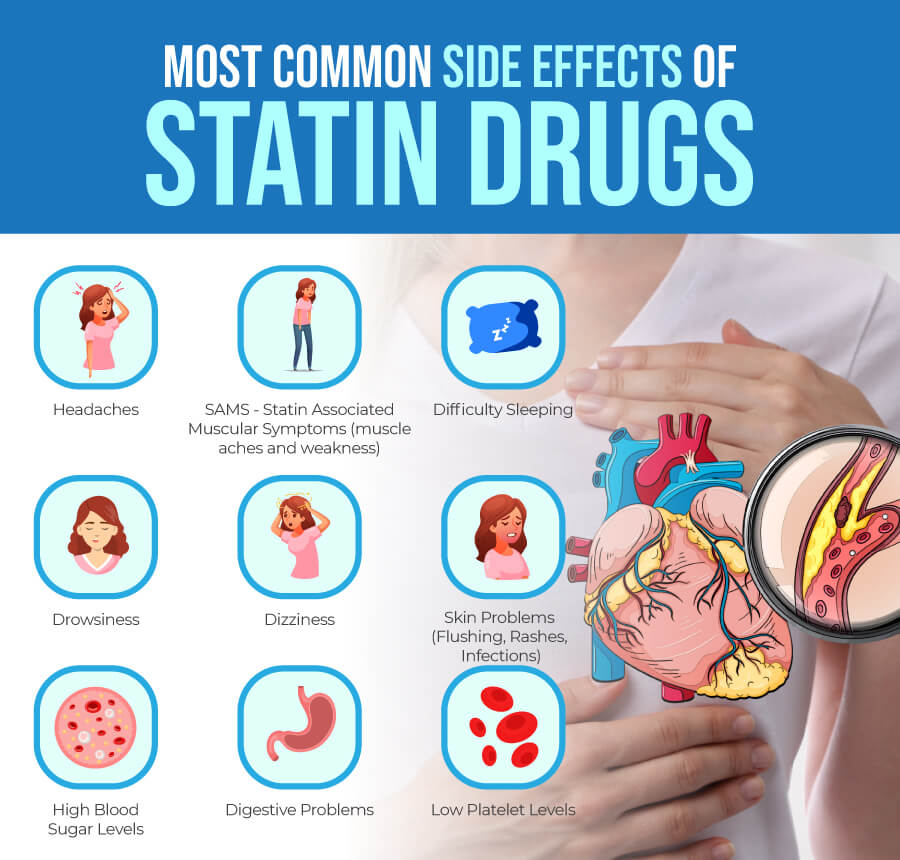
Muscle pain is one of the most common side effects of statin drugs. However, you may experience some other mild or more severe side effects using this medication.
Some of the most common side effects of statin drugs include:
- Headaches
- Muscles aches, weakness, or tenderness
- Difficulty sleeping or sleep issues
- Drowsiness
- Dizziness
- Skin flushing
- Rashes
- Acne or other skin issues
- Stomach pain or cramps
- Nausea
- Vomiting
- Gas
- Bloating
- Constipation
- Diarrhea
- Low platelet levels
- High blood sugar levels
Furthermore, statin drugs may also increase your risk of diabetes and skin conditions.
Statin drugs may decrease your risk of a heart attack and increase your life by a little if you are a man with pre-existing heart disease. However, a 2019 study published in Diabetes Metabolism found that statin drugs can double your risk of diabetes (22). Your risks are the highest if you’ve been taking them for 2 years or longer.
Another 2019 study published in the British Journal of Clinical Pharmacology found that statin drugs can also increase the risk of staph skin infections by 40 percent (23). They found similar rates of skin infections in those with and without diabetes, which suggests that the infections were not only a complication of diabetes but the side effect of statin drugs.
Less Common Statin Drug Side Effects May Include:
- Hair loss
- Tingling, numbness, prickling, or pins and needles feeling on your skin
- Liver inflammation
- Pancreatic inflammation
- Erectile dysfunction, low sex drive, or other sexual difficulties
- Memory loss or confusion
- Neuropathy
Serious side effects of statin drugs may include:
- Myositis or muscle inflammation
- Elevated CPK causing inflammation, weakness, and muscle pain
- Rhabdomyolysis causing serious muscle fatigue or muscle damage
If you are experiencing any of these side effects, it’s important to call your doctor. Call your doctor right away if you are experiencing any of the following as they may be signs of rhabdomyolysis or another serious issue:
- Fever
- Fatigue or tiredness
- Unusual muscle cramps or pain
- Diarrhea
- Dark urine
Risk Factors for Statin Side Effects
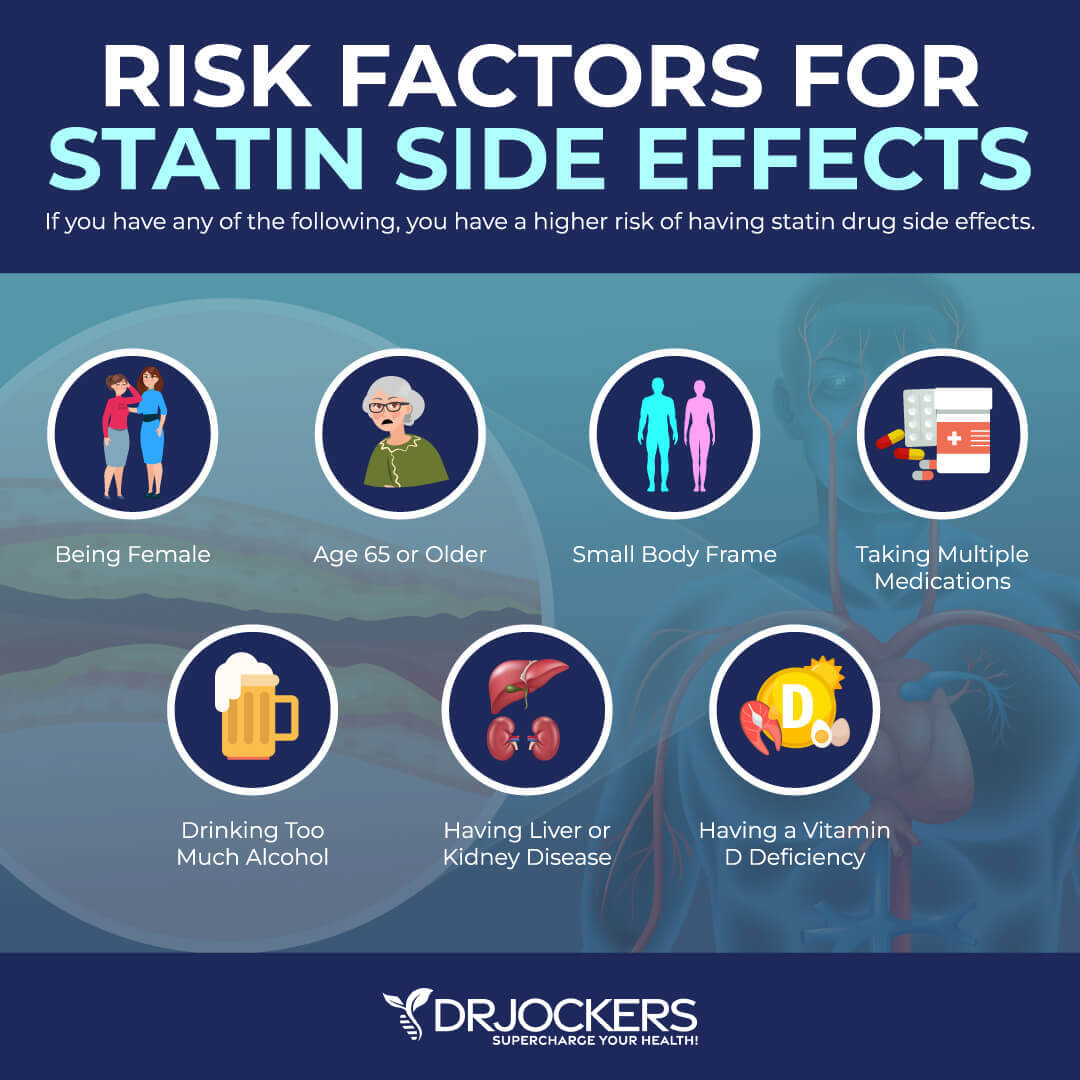
There are certain risk factors that can increase your risk of side effects from statin drugs, including:
- Taking more than one medication for bad cholesterol
- Being female
- Being 65 or older
- Having a small body frame
- Drinking too much alcohol
- Having liver or kidney disease
- Vitamin D deficiency
Most of these risk factors are pretty straightforward and are commonly mentioned by doctors. However, despite research evidence, vitamin D deficiency is a relatively less-known risk factor.
A 2019 study published in Disease Markers found that low vitamin D levels increase the risk of statin-induced musculoskeletal pain (2). The study looked at 1,210 patients, 287 with statin-associated muscle symptoms (SAMS) and 923 control participants without SAMS. They found that over two-thirds of patients with vitamin D deficiency had SAMS.
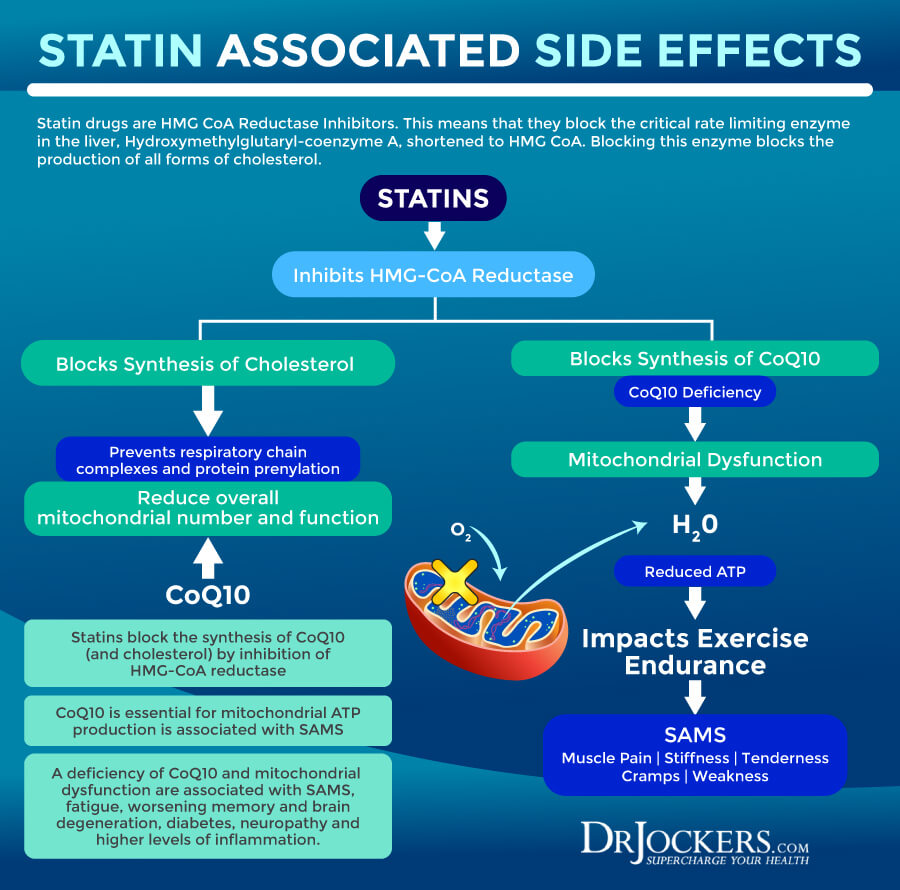
How Statin Drugs Damage Mitochondrial Function
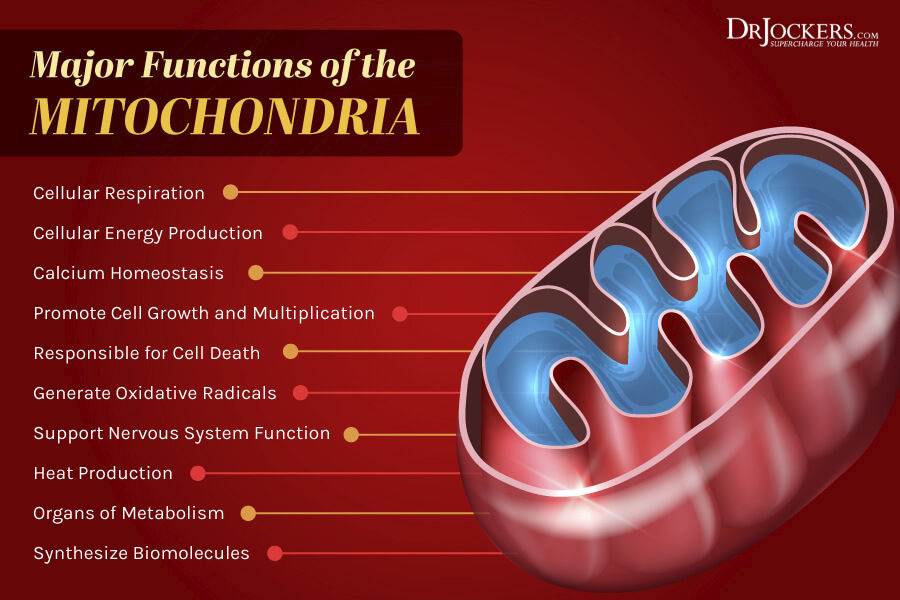
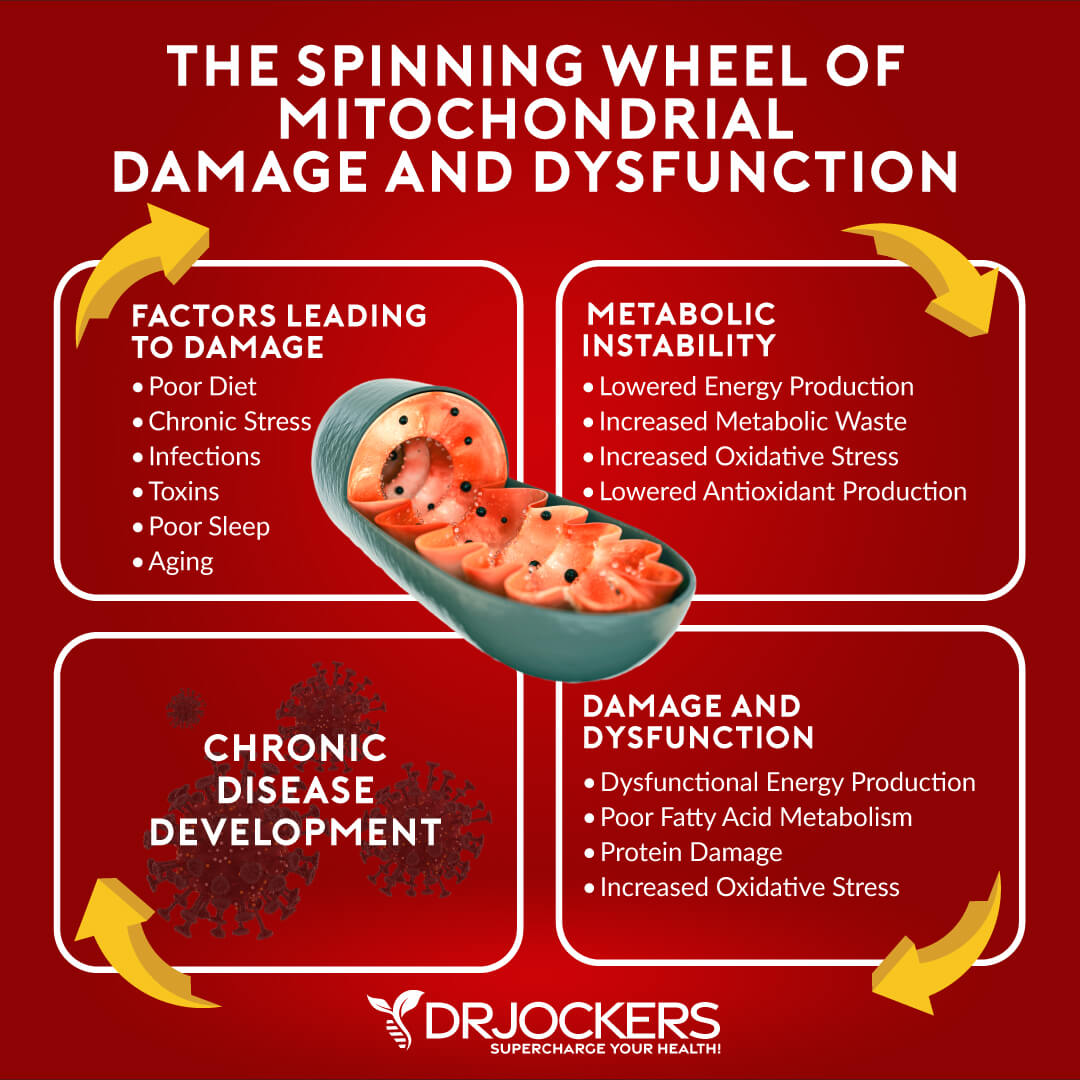
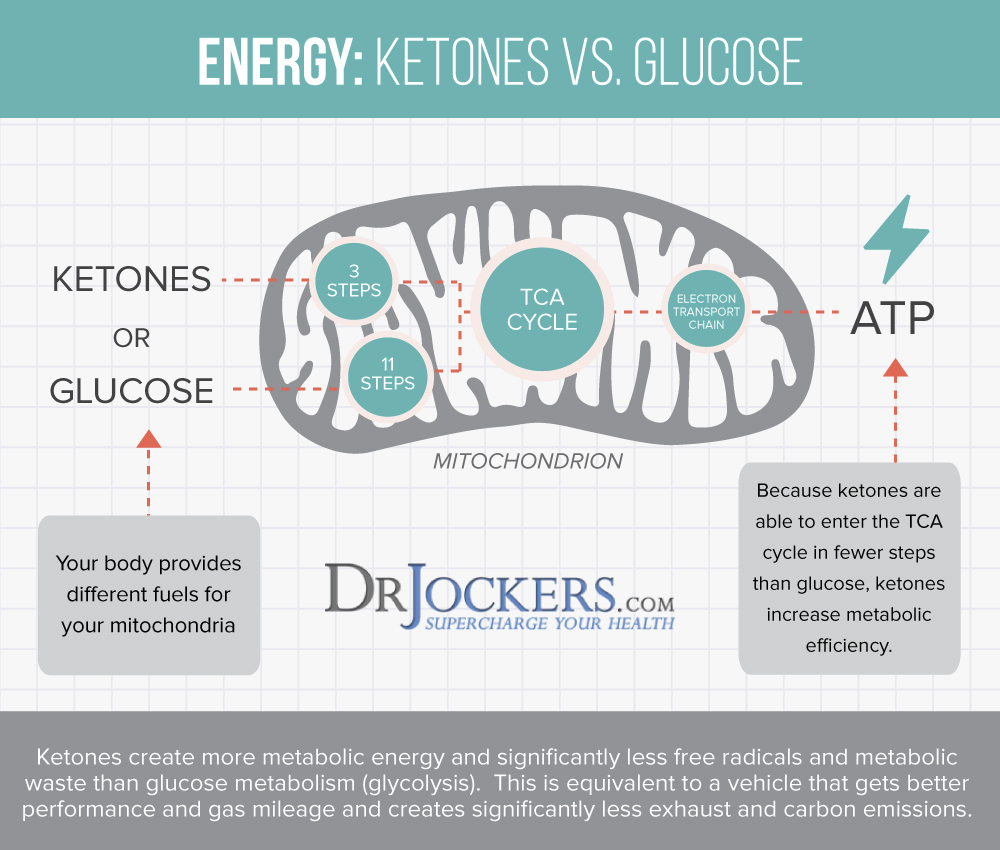
Your mitochondria are the powerhouse of your cells. They are unique organelles found in every cell of your body. It contains its own DNA. Your mitochondria generate about 90 percent of cellular energy in your body in the form of adenosine triphosphate (ATP). It also plays a role in major metabolic functions. Mitochondria are found in varying concentrations in different tissues in your body and are specialized for the purpose of that tissue.
Clearly, your mitochondrial health is critical for your overall function and well-being. Mitochondrial dysfunction can cause problems throughout your body. You can learn more about mitochondrial dysfunction by reading this article.
One of the main problems with statin drugs is that they may damage your mitochondrial function. A 2017 review published in the Journal of Clinical Medicine found that while statin drugs are highly effective, SAMS is one of the main reasons for discontinuation (3). Researchers speculate that the cause of SAMS may be mitochondrial dysfunction caused by statin drugs.
A 2016 review published in Postepy Biochemii has also found that statin drugs may impair mitochondrial functions (4). They noted abnormal mitochondrial morphology, reduced mitochondrial membrane potential, lower mitochondrial activation, and reduced oxidative phosphorylation capacity. While we don’t have enough evidence to fully understand why statin drugs may interfere with mitochondrial function, researchers believe that four factors may play a role.
Coenzyme Q10 plays an important role in the mitochondrial respiratory chain and deficiency may result in mitochondrial dysfunction when using statin drugs. Statin drugs may also prevent respiratory chain complexes, prevent protein prenylation, or trigger mitochondrial apoptosis, all of which may cause mitochondrial dysfunction.
Is High Cholesterol Really a Problem?
When we talk about statin drugs, it’s important that you understand what cholesterol is and whether high cholesterol is actually bad. Cholesterol is a waxy substance in your blood that helps your body to build healthy cells. It is produced in your liver. You also gain cholesterol from your diet by eating animal products.
Cholesterol is a lipid, which means it’s a fatty substance. Lipids include cholesterol, triglycerides, high-density lipoprotein (HDL), low-density lipoprotein (LDL), and very-low-density lipoprotein (VLDL).
Dyslipidemia means that your lipid levels are outside the normal range. You may have hypercholesterolemia, an increase in cholesterol, hypertriglyceridemia, an increase in triglycerides only, or hyperlipidemia, an increase in both cholesterol and triglycerides.
Of course, you want good cholesterol levels as they are critical for your health. They’re important for your brain and nervous system health, cognitive function, hormonal health, digestion, and the transportation of fat-soluble nutrients.
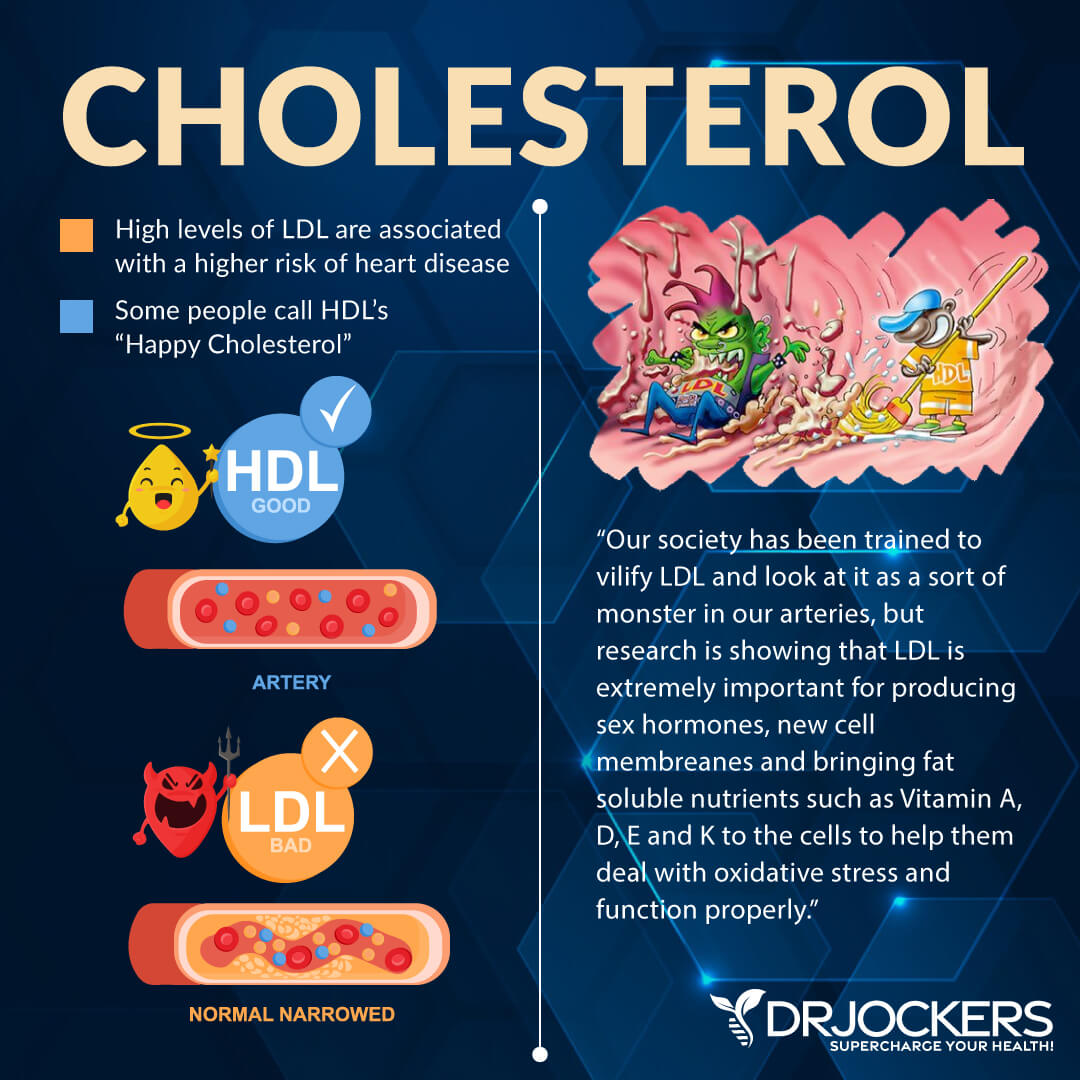
LDL Cholesterol: Good or Bad?
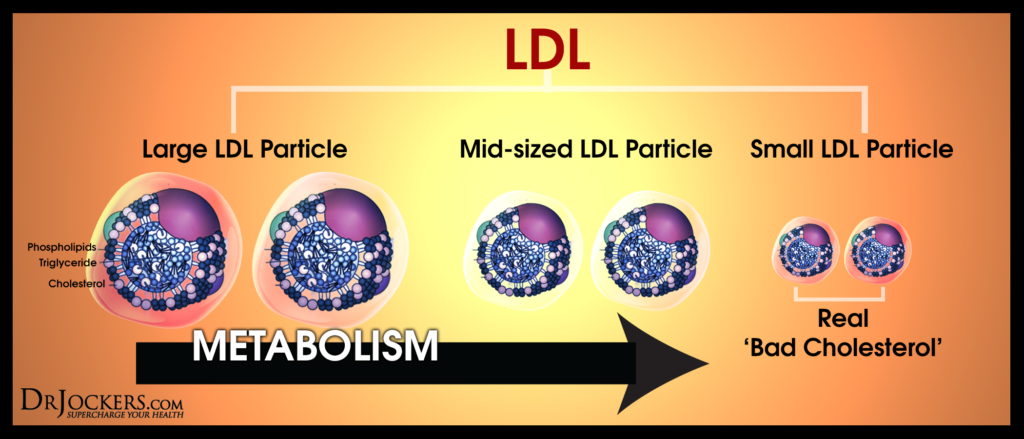
The primary role of low-density lipoprotein (LDL) is to transport cholesterol and fat-soluble nutrients into the cell membrane. While LDL cholesterol is generally considered ‘bad’ cholesterol, the issue is more complex than that. The truth is that there are more than one type of LDL particles. They differ in size. The size of the LDL particle determines whether it is “bad” or not, or rather, whether it contributes to heart disease or protects you from it.
Your LDL levels may also be increased because of poor thyroid activity. T3 helps to sensitize the LDL receptor of your cell membranes. Thus lower T3 activity can cause increased LDL cholesterol levels.
Ideal LDL Range: 100–200
Pattern A vs Pattern B
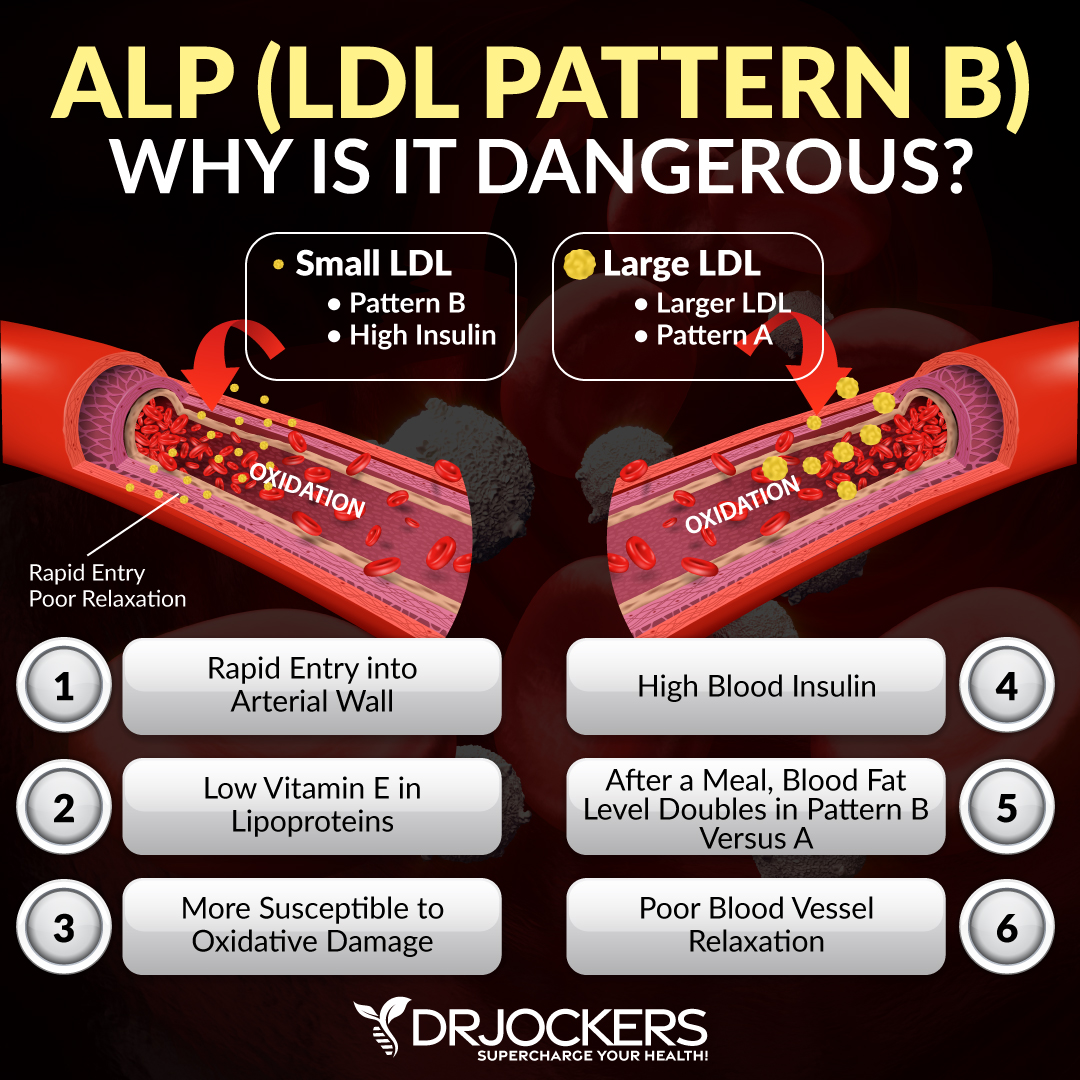
Pattern A LDL refers to a larger particle that can carry more fat-soluble nutrients and antioxidants. Pattern A actually offers cardioprotective benefits and helps to reduce your insulin and HbA1C levels.
Pattern B LDL is smaller and is more prone to oxidation. It is associated with a higher risk of cardiovascular disease, higher fasting insulin, and higher HbA1C levels. The NMR test can help us to look at size of LDL particles in your body. You can learn more about the NMR test by reading this article.
VLDL Cholesterol
VLDL cholesterol helps to transport triglycerides to your tissues. Triglycerides make VLDL denser than LDL. Once it’s released, certain enzymes can change VLDL to LDL.
Ideal VLDL Range: 5 – 30 mg/dl
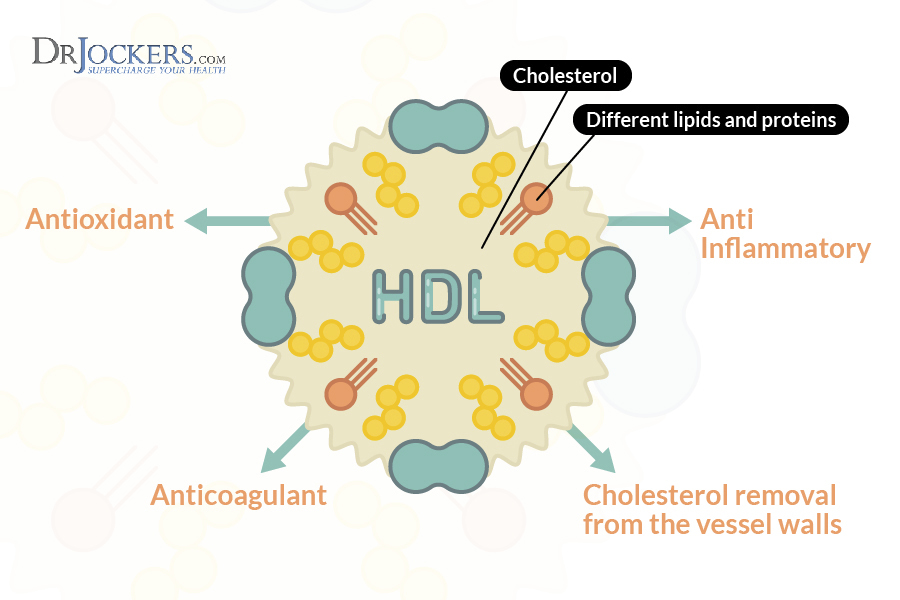
HDL Cholesterol
HDL cholesterol has high cholesterol to protein ratio at around 45 to 50 percent protein. HDL cholesterol helps to clean up LDL particles and take them to the liver for recycling. Cleaning up LDL is important because of its high susceptibility to oxidation. If LDL stays in your bloodstream for too long, it increases the risk of chronic inflammation and heart disease. High levels of HDL cholesterol (over 100 mg/dl) may indicate chronic inflammation or having an active infection.
Ideal HDL Range: 55 – 80 mg/dl
Triglycerides
Triglycerides are a type of lipid that helps to supply your body with energy. While they are critical for your health, high levels can increase your risk of heart disease. Lipoproteins are responsible for transporting triglycerides into the cell membrane, where they can be broken down into fatty acids and converted into ATP for energy. Insulin resistance, high insulin levels, and fatty liver disease may cause high triglyceride levels.
Ideal Triglyceride Range: 40 – 80 mg/dl
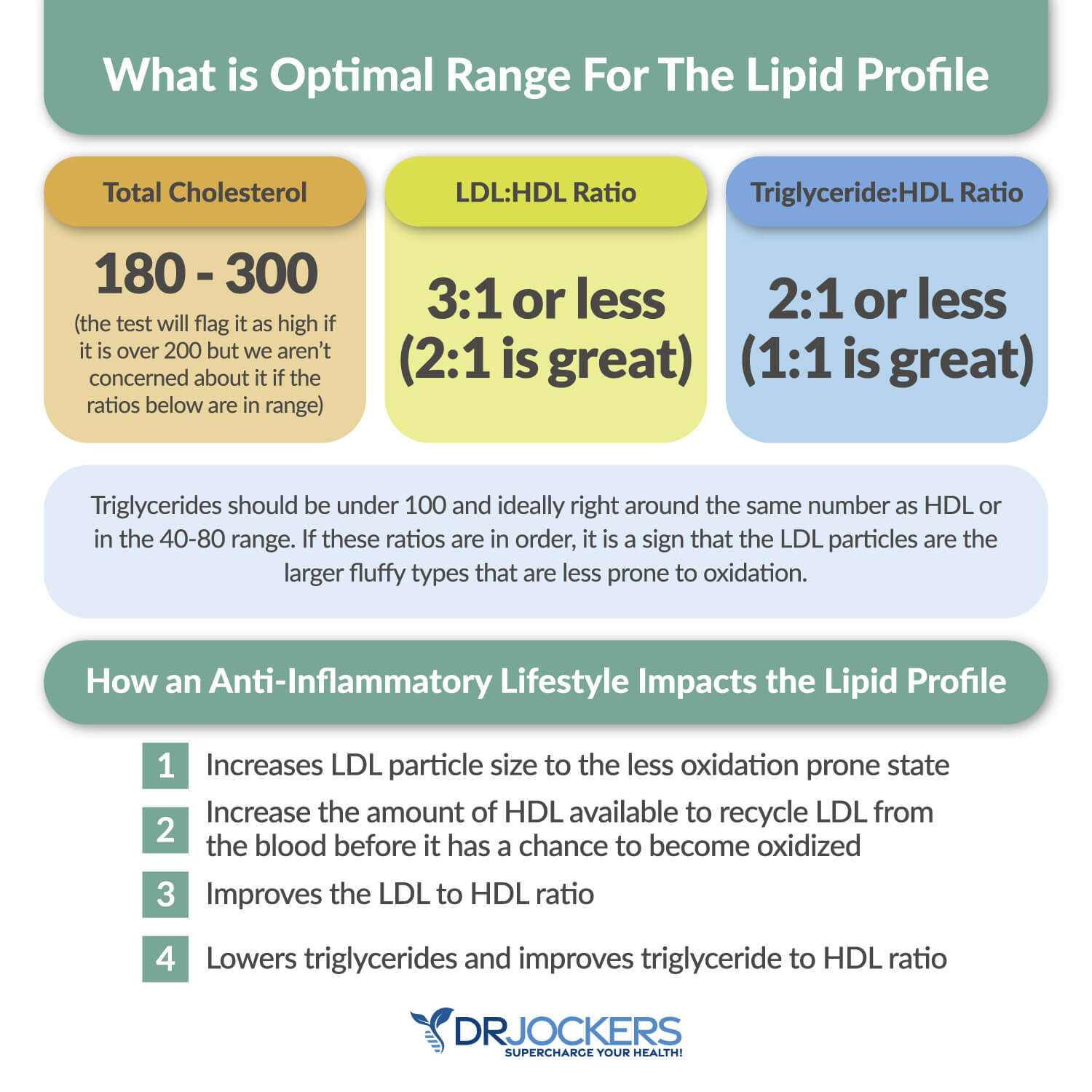
Healthy Ratios
When looking at your cholesterol levels, the most important thing to look at is a balanced ratio of LDL and HDL cholesterol and triglycerides to HDL ratio. High ratios often indicate insulin resistance and high fasting insulin levels, and the risk of chronic inflammation and consequent health issues.
Normal LDL: HDL Ratio: 3:1 or less (2:1 is ideal)
Normal Triglyceride: HDL Ratio: 2:1 or less (1:1) is ideal.
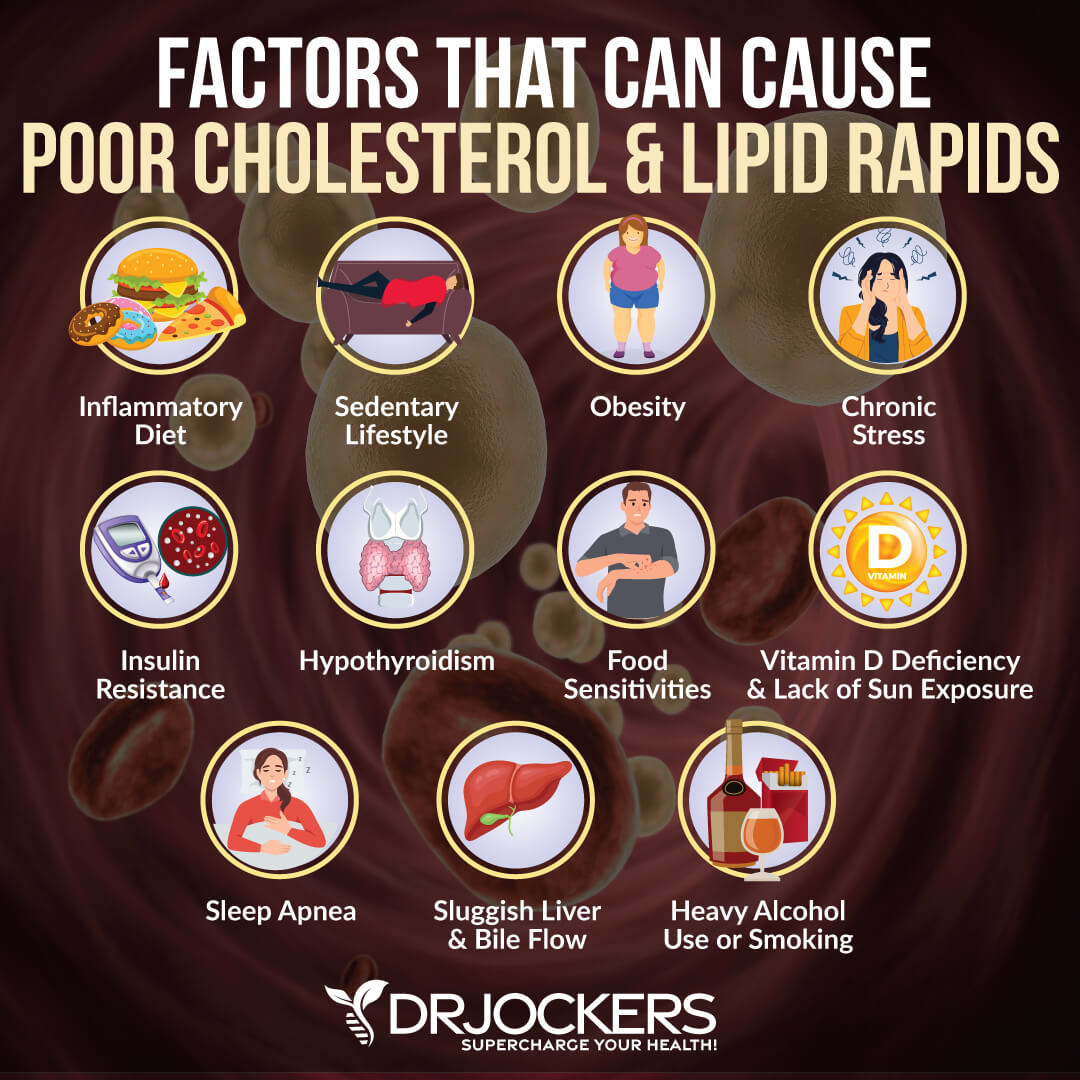
Factors That Can Cause Poor Cholesterol and Lipid Ratios
Factors that can cause poor cholesterol and lipid ratios may include:
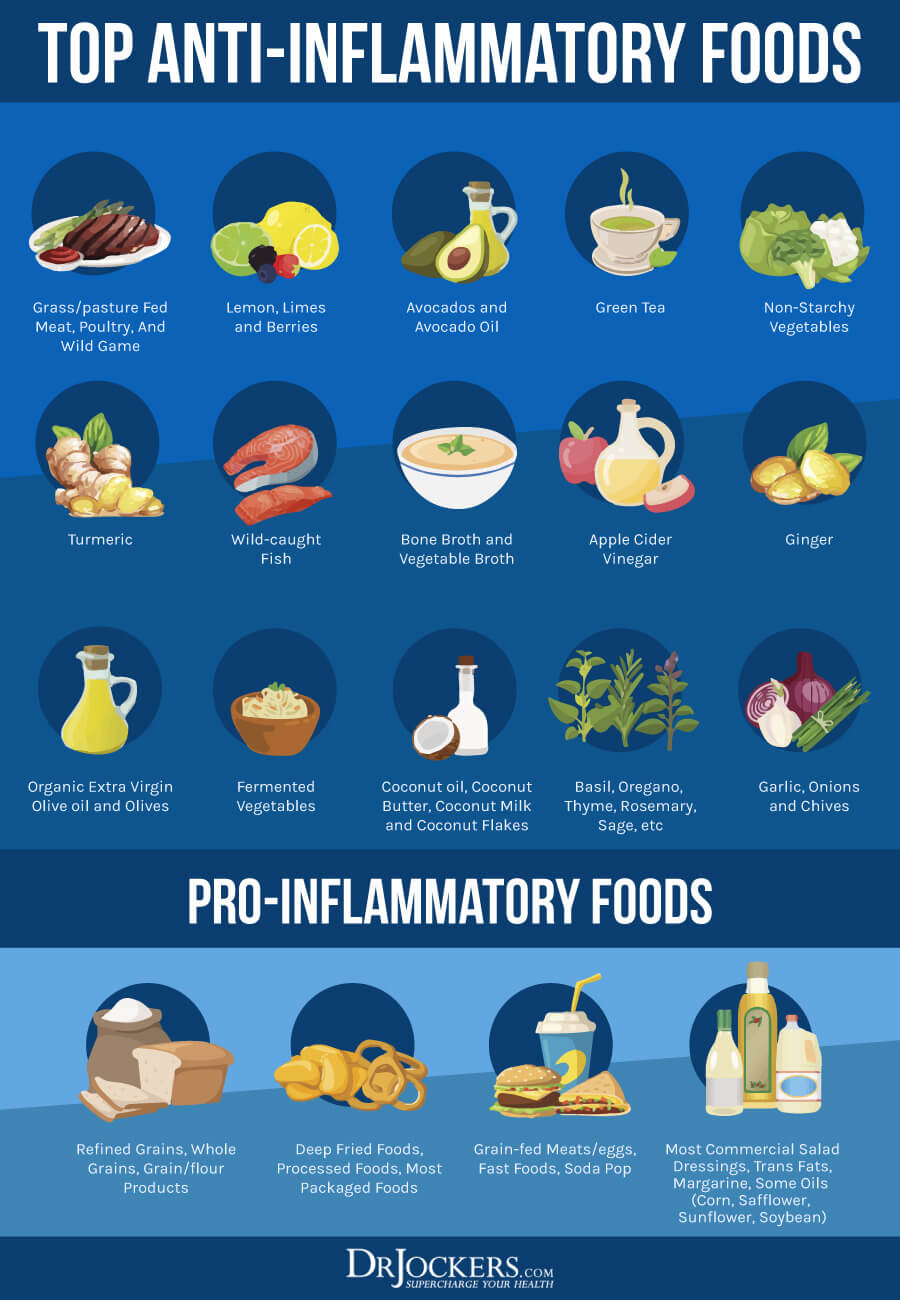
- A pro-inflammatory diet
- Sedentary lifestyle
- Obesity
- Chronic stress
- Insulin resistance
- Hypothyroidism
- Food sensitivities
- Vitamin D deficiency and lack of sunshine exposure
- Poor sleep and sleep apnea
- Sluggish liver and poor bile flow
- Smoking
You can learn more about these factors that can result in poor cholesterol and lipid ratios and what to do about them by reading this article.
Support Strategies for Healing from Statin Drug Side Effects
If you have taken or are taking statin drugs, I recommend some natural support strategies for healing from statin drug side effects. These natural strategies support your overall health, energy, and function. Here is what I recommend.
Anti-Inflammatory Nutrition Plan
According to a 2000 study published in Current Control Trials in Cardiovascular Medicine found that statin drugs have anti-inflammatory effects (5). While this may be true, experiencing side effects on a regular basis can put extra stress on your body. This may lead to chronic inflammation and consequent chronic health issues. Statin drugs may also lead to mitochondrial dysfunction, which may cause chronic inflammation (3, 4). Reducing inflammation with lifestyle strategies can help to improve your symptoms.
Natural anti-inflammatory strategies may also help to improve your overall health and reduce your risk of bad cholesterol ratios, cardiovascular disease, and stroke. These strategies can help you to reduce side effects while on statin drugs. These strategies may also help you to not rely on statin drugs anymore but stay healthy through natural anti-inflammatory strategies. However, you should never stop any medication without your doctor’s knowledge and guidance.
If your goal is to stop relying on statin drugs, I recommend that you talk with your doctor and make a plan that’s right for your health. Nonetheless, reducing your inflammation levels is in favor of your health and important regardless of your current medication regimen. One of the best ways to reduce inflammation levels in your body is by eating an anti-inflammatory diet.
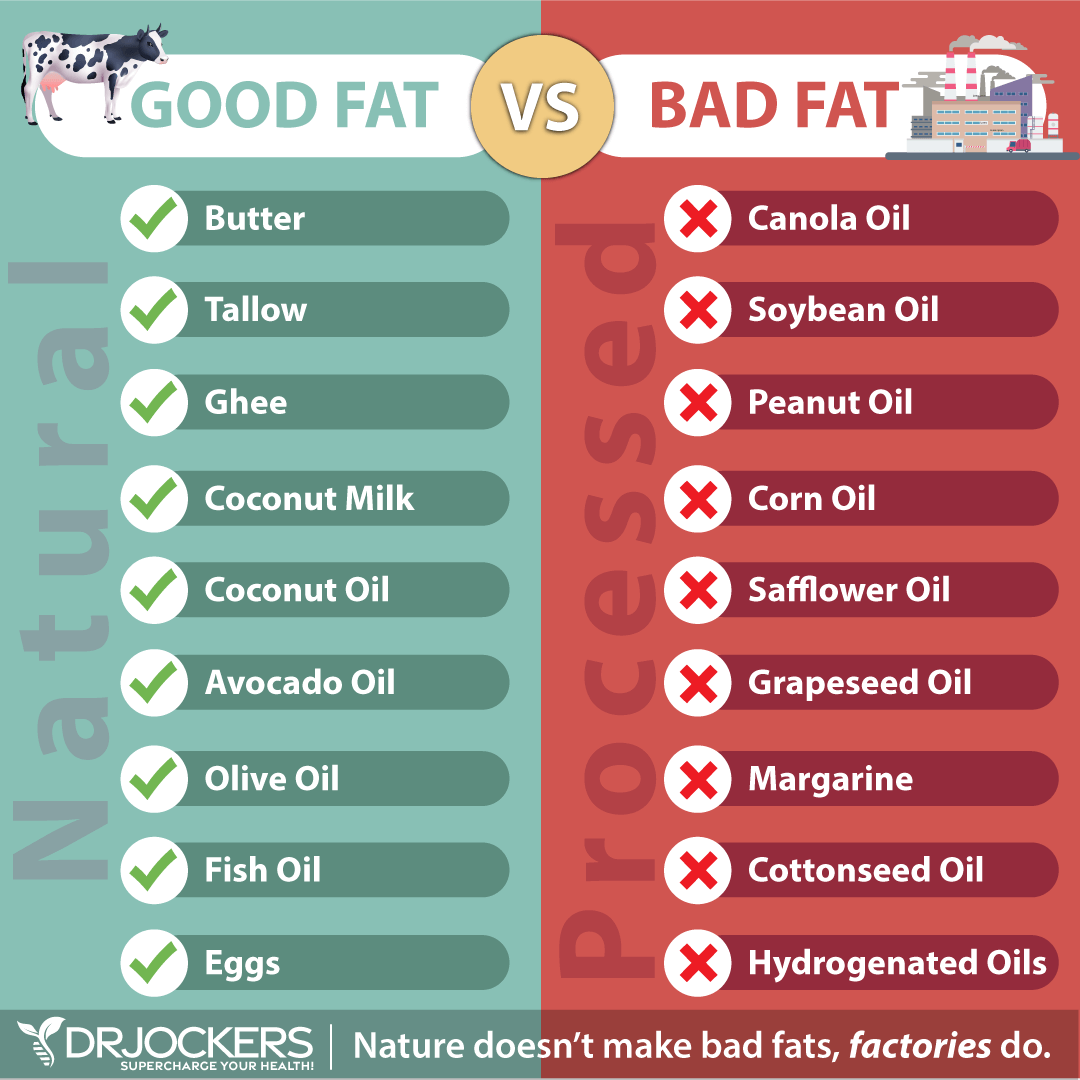
I recommend that you follow an anti-inflammatory nutrient plan. First, cut out all refined sugar, refined oils, gluten, conventionally raised dairy, conventionally raised and processed meat, artificial ingredients, additives, food allergens, junk food, and highly processed food. Instead, eat a diet rich in greens, vegetables, low-glycemic index fruits, herbs, spices, fermented foods, grass-fed beef, grass-fed butter and ghee, pasture-raised poultry and eggs, wild-caught fish and seafood, and wild game.
I recommend that you choose organic food whenever it’s possible and available to you. If you are unable to find or afford organic options, it’s critical that you always follow the rule of the dirty dozen and clean fifteen. If a food is on the list of dirty dozen, always choose organic.
If it’s on the clean fifteen list, organic is still ideal, but if it’s not available, you may choose non-organic. If your produce is not organic, make sure to wash it very well and peel it if possible. If it’s something you can’t peel, like greens or herbs, organic is the best choice. To learn more about the anti-inflammatory nutrition plan I recommend, you may read this article.
Ketosis & Intermittent Fasting
Two other great ways to reduce inflammation are getting into ketosis and intermittent fasting. A 2021 study published in Science Reports found that the ketogenic diet can reduce inflammation and pain (6). A 2014 study published in the International Journal of Health Sciences (Qassim) found that intermittent fasting can decrease inflammation, reduce the risk of disease, and improve your health (7).
Under normal circumstances, your body uses dietary glucose for energy. However, if you are following a high-fat, low-carb diet, your body will start relying on fat for energy instead of glucose. It starts to make ketones in the process. Ketosis has many health benefits, from reduced inflammation, increased insulin sensitivity, improved cellular renewal to a decreased risk of disease. Intermittent fasting can also help your body to experience a ketogenic state and enhance the benefits of a ketogenic diet.
The ketogenic diet is a simple treatment approach since it only involves a dietary change. The keto diet is a high-fat, low-carb diet with carbohydrate levels very low at 5 to 10 percent, protein levels moderate at 30 to 35 percent, and fats high at 55 to 60 percent of your calories. It’s important, however, that you follow a real food keto diet.
Keeping to your macronutrient ratios is necessary for achieving ketosis. However, loading up on high-fat, low-carb, keto-friendly, such as low-nutrient junk foods, such as a burger with cheese without the bun, chicken deep-fried in refined oil, processed or canned meat, or diet sodas can be detrimental to your health even if they are high-fat and low-carb. Real food micronutrients, such as vitamins and minerals, by following an anti-inflammatory, nutrient-dense plan are just as critical as your macronutrient ratios.
Follow an anti-inflammatory, real food ketogenic diet rich in greens, vegetables, herbs, spices, fermented foods, low glycemic index fruits, healthy fats, such as coconut oil, MCT oil, organic grass-fed butter or ghee, avocadoes, nuts, and seeds, and clean animal protein, such as grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game.
Most of your diet should be abundant in healthy fats, including avocados, coconut oil, coconut butter, coconuts, avocado oil, extra-virgin olive oil, pasture-raised butter and ghee, lard, flax seeds, hemp seeds, chia seeds, pumpkin seeds, other seeds, olives, nuts, and any fats from clean animal foods, such as grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game. You may learn more about the benefits of ketosis by reading this article.
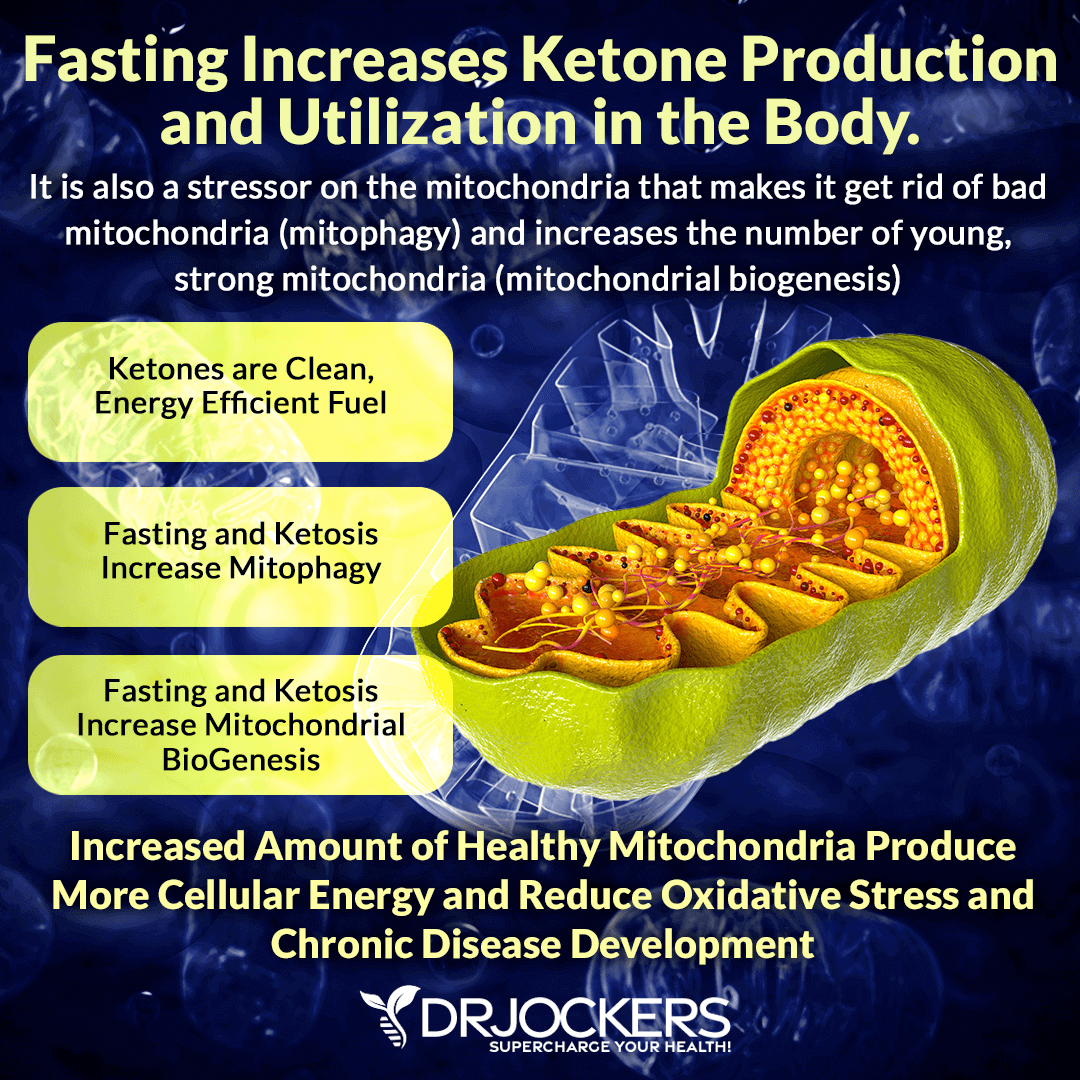
Intermittent fasting is a dietary strategy that cycles between periods of fasting and periods of eating within one day. Intermittent fasting is not as unusual as you may think. Just think about it. You are already fasting overnight between your last meal or night-time snack and breakfast.
With intermittent fasting, you are simply extending this fasting window. Intermittent fasting is not a caloric restriction or fad diet either. During your eating window, you will be eating nutrient-dense, anti-inflammatory foods to meet all your nutrient and caloric needs for the day within a shorter period.
If you are new to intermittent fasting, I recommend that you start with the Simple Fast. A Simple Fast involves 12 hours of fasting, including your overnight sleep. Start your fast after dinner, and don’t eat for 12 hours until breakfast. Gradually increase your fasting window until you find what feels the best for your body and works for your lifestyle.
Most people feel their best with a 16-hour fasting window using the 16:8 method. However, you may find that a slightly shorter or longer window feels better for your body. To learn more about the benefits of intermittent fasting, I recommend reading this article. To learn more about different intermittent fasting strategies, I recommend reading this article.
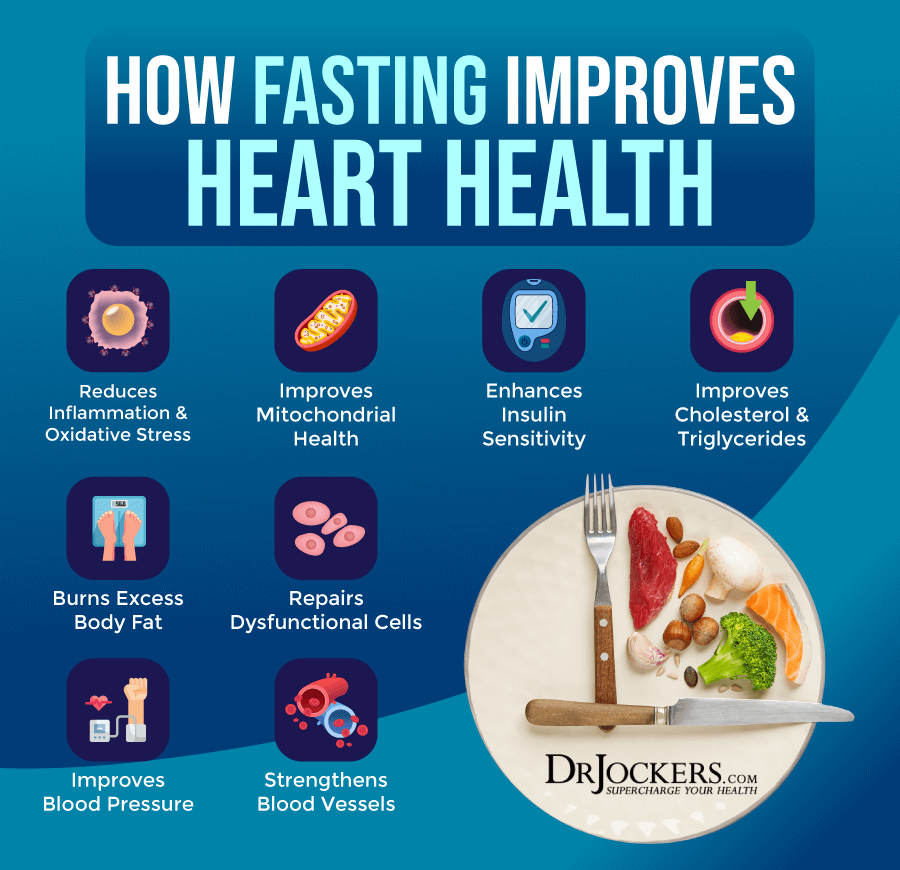
Reduce Stress & Improve Sleep Quality
Another way to reduce your inflammation levels is by reducing your stress levels and improving your sleep quality. A 2017 study published in Frontiers in Human Neurosciences found a connection between stress, inflammation, and stress-related disease (8). Poor sleep can be a consequence of chronic stress, but poor sleep can also lead to chronic stress.
Sleep troubles can also be a side effect of statin drugs. This can set you up for chronic inflammation and an array of health issues. A 2010 study published in the Best Practices in Research in Clinical Endocrinology and Metabolism found a link between poor sleep and inflammation (9). Tackling stress and sleep are clearly very important for your overall health.
To lower your stress levels, try to reduce stressful activities and interactions with people that stress you out. Mindset shifts, positive thinking, counting to ten before responding, gratitude, positive affirmations, and prayer can respond to and handle stress better. I recommend regular meditation, breathwork, guided relaxation, gratitude work, journaling, and prayer. They are fantastic stress-reducing strategies. Working with a therapist or spiritual counselor can also help you cope with stress better and learn coping strategies.
To improve your sleep quality, avoid stress, electronics, heavy foods, sugar, caffeine, and alcohol in the evening and at night. Engage in relaxing activities, such as reading, crossword puzzles, board games, crafts, coloring, or journaling a few hours before bedtime.
Taking a relaxing bath or sipping on herbal tea may help you to wind down. Make sure that you have a supportive bed, pillows, and bedding. Try blackout curtains or eye masks.

Get Regular Sun Exposure & Optimize Vitamin D Levels
Vitamin D is an essential vitamin for muscle, bone, brain, and immune health in everyone. It may be particularly important if you are taking statin drugs. A 2011 study published in Medical Hypotheses found that vitamin D deficiency can increase myositis-myalgia in those taking statin drugs (10).
A 2015 study published in the National American Journal of Medical Sciences found that vitamin D deficiency can result in statin intolerance and statin-induced myalgia, myositis, or myonecrosis (11). Researchers found that vitamin D supplementation can resolve these issues in most cases.
Most people are not getting enough sunshine or consuming enough vitamin D from food. Therefore, most people need to supplement to optimize their vitamin D levels. Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and inflammation control. I recommend taking a vitamin D3 supplement with at least 3,000–5,000 IUs of vitamin D3 and at least 90 mcg of vitamin K2. I recommend taking D3/K2 Power for your daily dose of vitamin D3 and K2.
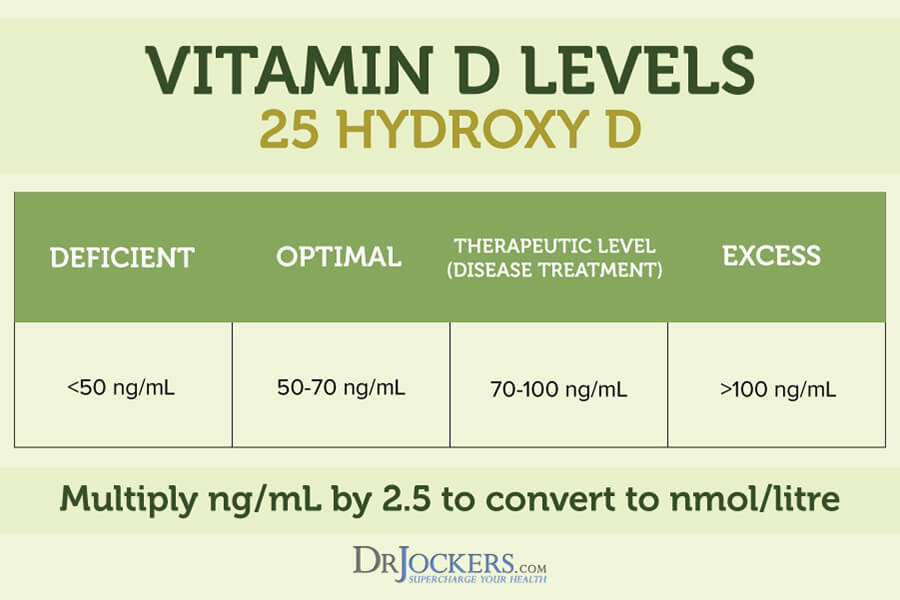
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1–2 times each year and get your levels between 50–100 ng/ml. It has been hypothesized that a therapeutic level for major health conditions is going to be between 70–100 ng/ml.
Take High Dose CoQ10
Coenzyme Q10 or CoQ10 is an antioxidant that your body produces naturally for growth and health. It is vital for heart health, skin health, healthy blood sugar levels, energy, brain health, lung health, and the prevention of cancer.
A 2018 meta-analysis of randomized controlled trials published in the Journal of the American Heart Association found that coenzyme Q10 may help with statin-induced myopathy (12). Another 2018 study published in Advances in Nutrition has also found the coenzyme Q 10 may help with statin-related muscle symptoms (13). I recommend that you take Super CoQ10 daily for recovering from statin drug side effects. I recommend taking 600 to 1200 mg daily in divided doses.
Regular Movement and Exercise
Another way to improve inflammation and support your health is with regular movement and exercise. I recommend that you stay active throughout the day and exercise regularly. Start your day with some stretching, yoga, or a short walk. Go for a walk during lunch or in the evening. Get up to stretch regularly. Take a leisurely bike ride or hike. Exercise regularly, five times a day if you can, engaging in a mix of cardiovascular workouts, strength- and resistance training exercises, and low-impact activities.
If you have myopathy, exercise can be more difficult. However, according to a 2000 study published in Current Opinions in Neurology, strength training and cardiovascular exercise can be beneficial for those with myopathy (14). I recommend that you start out easy and stay with low-impact activities at first.
Strength- and resistance training with resistance bands, body weight, or light weights may help to improve your muscles. Yoga or Pilates may also be strengthening yet low-impact. For cardiovascular workouts, start easy and slow at first. Build up your strength and fitness gradually. You may benefit from working with a physical therapist who can help you with the right exercises.

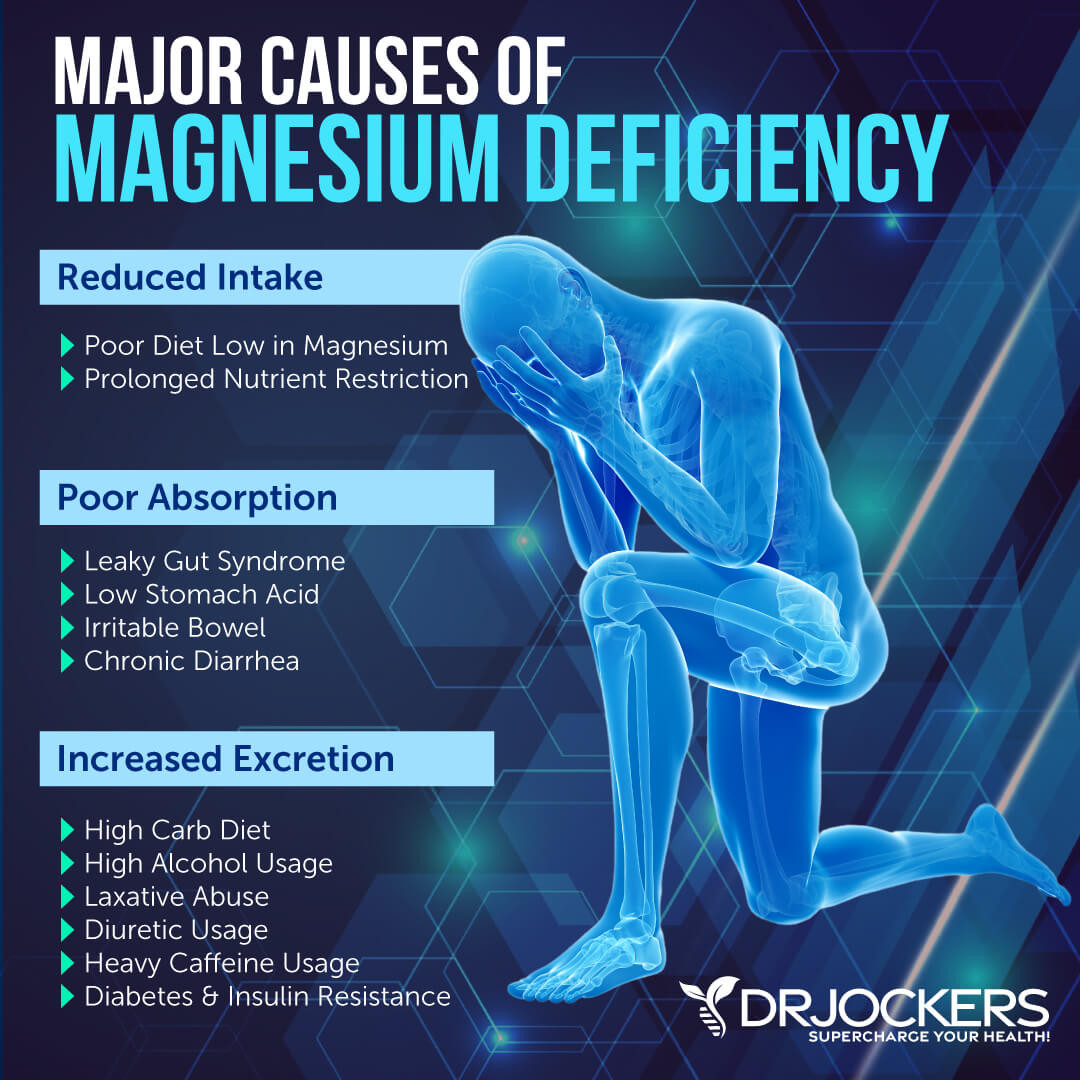
Support Magnesium Levels
Magnesium is an important mineral for muscle health, stress, tension, neurological health, brain health, and mental health. A 2004 study published in the Journal of American College of Nutrition found that magnesium can have similar benefits as statin drugs (15). They also don’t interfere with statin drugs if you are taking them.
I recommend that you take Brain Calm magnesium. It is great for brain health, pain relief, muscle relaxation, bone and joint health, healthy blood pressure, and energy. I also recommend supplementing with CalMag Support. This supplement is great for neurological health, nerve function, mental health, muscle health, bone health, and energy production.
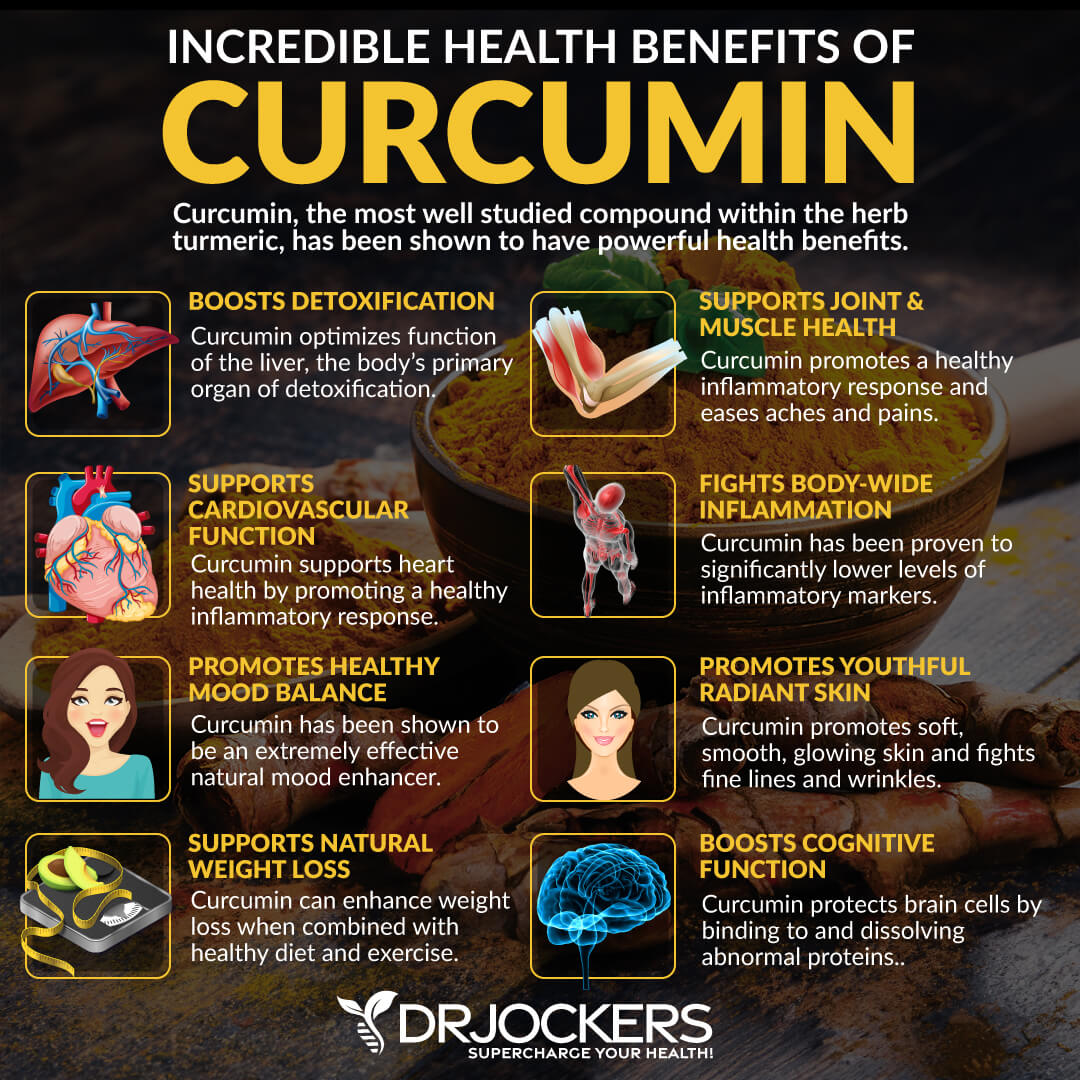
Consider Using Curcumin
Curcumin is the active compound of the most researched anti-inflammatory herb, turmeric. A 2016 study published in the Journal of Cachexia Sarcopenia Muscle found that curcumin may help patients with statin-related muscle issues (15). They also found that curcumin may help to improve mitochondrial health and cholesterol levels.
A 2016 study published in the International Journal of Immunopathology and Pharmacology found that curcumin may improve statin-related myotoxicity (16). I recommend taking curcumin supplements daily and cooking with turmeric regularly.
Consider Using Resveratrol
Resveratrol is found in the skin of grapes, red wine, and berries. It is a plant compound that acts as an antioxidant. A 2020 study published in the Journal of Biochemical and Molecular Toxicology found that resveratrol may help to protect your body against statin muscle cell toxicity (17).
A 2014 study published in Experimental Therapies and Medicine found that resveratrol may have similar cardiovascular health benefits as statins (18). I recommend eating resveratrol-rich foods, such as blueberries, cranberries, grapes, and pistachios regularly and taking resveratrol supplements daily.

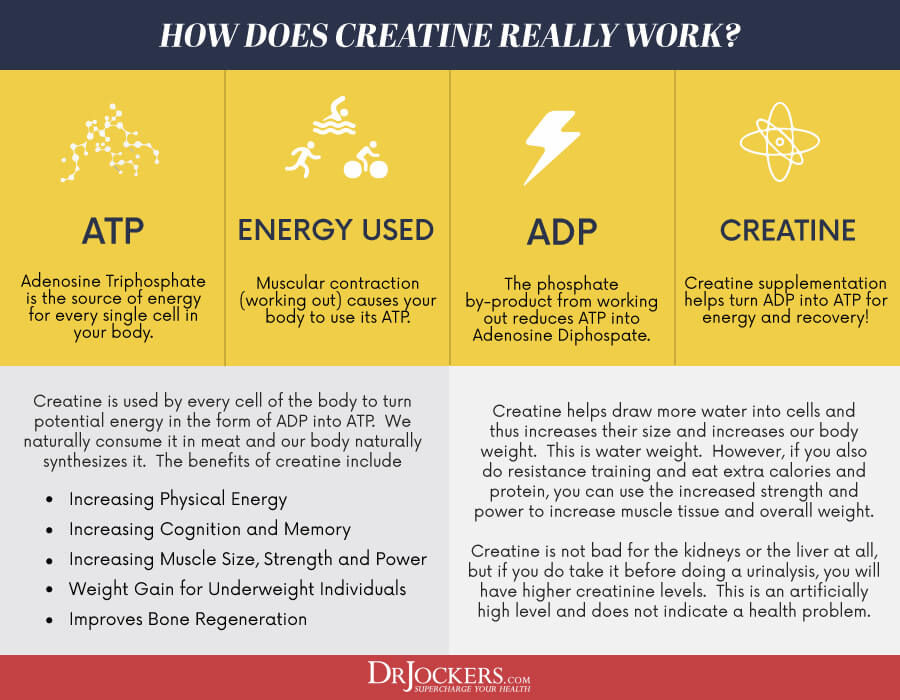
Consider Taking Creatine
Creatine is naturally found in your muscle cells. It helps your muscles create energy during high-intensity workouts or lifting heavy weights. Creatine supplements are often used to increase muscle gains, exercise performance, and brain health.
They may also help if you are taking statin drugs. A 2019 study published in Biomolecules found that taking creatine may help to reduce the risk of statin-related myopathy (19). To reduce myopathy as a statin drug side effect, I recommend that you take creatine daily.
Use a Mitochondrial Support Supplement
I recommend that you try a mitochondrial support supplement, Mito Support™. This supplement has curcumin, resveratrol, creatine, and magnesium in it as well as B vitamins, D-Ribose, and other important nutrients that support efficient mitochondrial metabolism and energy (ATP) production for increased vitality.
Mito Support™ was designed to support the function of the mitochondria, “the powerhouse of the cell.” This formula may be appropriate for anyone wishing to promote overall cellular- and tissue vitality and health.
It helps to improve your cellular function, cardiovascular health, energy, cognition, mental health, and athletic performance. Take two capsules twice a day or for an advanced dose, four capsules twice a day with meals.
Final Thoughts
Statins are some of the most commonly prescribed medications. They are used to improve your bad cholesterol levels and reduce your risk of cardiovascular disease, heart attacks, and stroke. Statin drugs may be common, but they don’t come without side effects. If you are taking or have taken statin drugs, I recommend that you try the natural support strategies I discussed in this article to help your overcome statin drug side effects.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!





Good morning Dr Jockers ,
Taking statins for the last 20 years , can i stop taking this drug immediatlly? Knowing that i have side effects especialy regarding my muscles, i am taking Q10+ VD 5000IU and k2 the active form’ with magnesium+ ……i am sleeping better and feel all together better but still taking my statins…can i stop them ? What are the side effects if i do so ? I also eat on an anti-inflammatory diet and do rgularly intermittent fasting ….….thank you to reply .
Hello Maika,
Great question and good news…there are no side effects to coming off the statin medications completely. You can do this right away safely! Sounds like you are following a great natural health plan. Blessings!
Hi Dr Jockers,
Im 40 years old and just been diagnosed with familial hypercholesterolemia. My cardiologist wants me to consider taking a low dose of statin. Im very cautious of statins. Am i best to avoid them at all costs? Or should i take a low dose statin along with this regimine and its ok?
Blessings,
Meg
Hello Meg, it is very rare that a statin drug ever provides any real benefits. Unfortunately, we can not give medical advice here but I would get a second opinion with a functional health practitioner.
I HAVE RECENTLY BEEN DIAGNOSED WITH FOLLICULAR LYMPHOMA STAGE 3A, I AM 73, EAT NATURAL AND EAT HEALTHY FOODS, EXERCISE DAILY AND A POSITIVE THINKER. SUFFERED HORRIFIC STRESS OVER MANY YEARS WHICH WAS UNAVOIDABLE BUT LEARNED TO MANAGE IT BEFORE IT KILLED ME. 3 YEARS AGO SURVIVED 4 CVA STROKES WITH DAILY REHAB FOR 9 MONTHS TO RELEARN TO WALK, TALK ETC AGAIN & NOW RIDING DAILY. SURVIVED ACUTE PANCREATITIS YEARS AGO & HAD COMPLICATIONS BUT OK. ALSO SURVIVED A MELANOMA 4 YEARS AGO, LOW BP AND LOW CHLORESTROL MOST OF MY LIFE BUT GIVEN CRESTOR POST STROKES. ??? LOVE TO STOP IT. NO KNOWN CAUSE OF THE CLOTS THAT CAUSED MY STROKES SO COULD HAVE MORE. DELAYING CHEMO FOR LYMPHOMA WITH A ‘WAIT AND WATCH’ STRATEGY WITH 6 WEEKLY BLOODS AND 3 MONTHLY PET SCANS. LOTS OF RADIATION & EMFs AGAIN BUT HAVE TO FLOW WITH THAT I GUESS…WOULD APPRECIATE ANY HEATH SUMMITS ON LYMPHOMA OR RELATED CANCER TOPICS OR ANYTHING ELSE RELEVANT. HAVE WATCHED A NUMBER OF HEALTH SUMMITS AND LOVE THEM. KEEN TO TALK WITH A GOID FUNCTIONAL MEDICINE PRACTITIONER FOR GUIDANCE ON LYMPHOMA ETC…BUT LIVE IN QUEENSLAND AUSTRALIA. DELAYING COVID JABS AS FEEL THE CORRECT DATA IS NOT BEING PUBLISHED YET. GENERALLY SUPPORT VACS THAT HAVE BEEN FULLY TRIALLED. THANKS FOR YOUR TIME. MERRY CHRISTMAS. VAL LAWTON val.lawton@outlook.com
LYMPHOMA maybe due to gluten. Gluten is in wheat/barley/rye….oats/corn/rice. Rice is low in gluten. Wild rice has no gluten…is a grass. Clots maybe due to low thyroid due to gluten. Gluten may make antibodies to the thyroid. Amour thyroid may help and Zn/Se/enough iron/probiotic to help convert T4 to T3 to make the thyroid hormone work. Statin drugs may cause heart failure due to blocking also the production of coenzyme Q10 the spark plug to the cell. NO gluten/dairy/soy/sugar/GMO/food with a label/heated oils…taking vitamins/good oils/minerals…probiotic…LDN..detoxing may help. Chemo/radiation may not be needed if you fix the root cause which maybe gluten. Gluten issues can be due to low sunlight heritage/current low sunlight.
Wow, this article provided a clearer picture than I have ever had! Thank you for the breadth and complexities you included especially about variations and interpretations of statistical assertions.
Glad to hear this Joann! Blessings to you!
Is the product “Nilstat” (used to treat candida) a statin drug or is the name a mere and unfortunate coinsidence?
High cholesterol is a big pharma invented disease, they changed parameters of what was normal to sell their poison. Why does the cholesterol level go up? Our bodies are brilliant and know what we need. Cholesterol is vital for many processes in the body….Thank you for discussing this Dr J and crew. If your cholesterol is elevated it most likely is associated with infection or hypothyroid. It used to be known that elevated cholesterol should be treated as hypothyroid. When cholesterol became measurable and pharma had the chemical to lower it, a disease and the gang buster drug was created. We have been played!
The body is electric…..electrical control of our body functions have been destroyed by increasing levels of EMF which have been in our environment since the telegram was invented. Now people die because they are poisoned and ZAPPED and our cells can’t communicate and beneficial microbes become pathogenic.
Very long writing about Cholesterol, concerning which I own 17 books since my wife in 2008 by doctor told to be to high in cholesterol with 270, and 117 for HDL. It took 7 years before the actual doctor admit that I am right. He wanted to put her on Statin, and hed didn’t know that Stain stopped the producing of Q10.
I continued in falling caused by stress, down i Cholesterol until only 167 now 11 month ago, but then sometimes 100 mg Niacin, besides also for other things, and the September up on 172, and after rereading my private written 500 side A4, lexicon and then discovering advise on 800 mg Niacin a day for higher Cholesterol. So now I am asking for bloodmeasure. Niacin i fine for correcting Cholesterol, and don’t har Q10.
Statistically it has been found that havin 240 then statistically higher IQ than if 220, og 260 better than only 240.
Thanks for sharing that!
I used to walk 5 miles nonstop three or four times a week. Eleven years ago after just a few months on statins I developed a condition called intermittent claudication which eventually reduced my maximum nonstop walking distance to a quarter of a mile. Once I figured out that statins were the cause of that I stopped taking them (along with all of the other toxic Big Pharma chemicals my cardiologist told me I would have to take for the rest of my life if I wanted to live very long), and I switched to eating what was effectively what my doctor told me was a “heart healthy diet” turned on its head, e.g. eating plenty of whole eggs and healthy saturated fats like butter and coconut oil instead of yolk-free omelets and margarine made from processed seed oils.
Unfortunately, although I eventually cured my heart disease completely by having a holistic dentist remove a decades old infected root canalled tooth that was the cause of it (as discovered by Weston A. Price), my maximum walking distance never increased above half a mile. Eventually I just resigned myself to the fact that the statins had left me effectively crippled for life.
Then a veritable miracle happened. I was taking Co-Q10 as a supplement for heart health, and I asked the manager of the supplements department in a health food store if she could tell me more about the differences among them, like ubiquinone vs. ubiquinol. She told me that she had recently learned about a new product called PQQ-10 that combines 20 mg of PQQ (short for “pyrroloquinoline quinone”) with 200 mg of Co-Q10. Not even imagining that it might be good for my legs, I decided to give it a try. Just three weeks later I noticed that my legs were feeling quit a bit better and found that I suddenly could walk one entire mile nonstop. Within three months I was all the way back up to 5 miles nonstop.
Trying to figure out what might be responsible for that I thought about everything that I had recently changed in my diet and supplements, and the only thing I could think of was replacing plain Co-Q10 with PQQ-10. A little online research led me to guess that the intermittent claudication was caused by statin-induced lasting damage to the mitochondria in my leg muscles, and that the addition of PQQ to Co-Q10 was somehow reversing that.
Because the PQQ-10 is a bit more expensive than plain Co-Q10 I eventually switched back to taking just the Co-Q10, hoping that the mitochondrial repair that PQQ had enabled would be permanent. Unfortunately it was not, and in a couple of months my maximum nonstop walking distance was down to two miles. I switched back to PQQ-10 and in just a couple of weeks I was back up to 5 miles, so I am continuing to take it on a daily basis.
It would be really cool if somebody who is treating statin-induced damage to patients’ muscles could do a randomized control study to see if others could receive the same benefit from PQQ + Co-Q10 that I have.
Thank for sharing in detail your experience I so want my walking life back and I’m fighting to not damage my opportunity by taking statins, I have PAD, and because I decline statins I have been seeing a soft sell cardiologist who is pushing me from one to another. I’m going to try the one you have successfully taken. So appreciate
Your input. All the best NH
Yes agreed. Thanks for sharing that!
Statin drugs are the most prescribed drugs in the world. We have been programmed to “fear” LDL cholesterol. If there was a drug that could totally halt the liver’s production of LDL, life would not exist for those taking the drug.
It is when LDL becomes oxidized it becomes small and dense. Now it becomes a problem.
A cholesterol test that is significant is a Lipid Subclass Detail, which measures the size of LDL-S. It provides a more accurate picture of cardiovascular risk by providing the number of the healthy LDL and the oxidized (smaller) LDL cholesterol.
New patient, I’m using Synthroid 25 mcg due to Thyroiditis .Because of the increased vascularity. Using the drug for 2 weeks and I feel dizzy. Never had this before. I don’t use other drugs, no smoker, no drinks. Healthy in eating. Need something else.Hope you can help me.