 Skin Rashes: Symptoms, Causes and Natural Support Strategies
Skin Rashes: Symptoms, Causes and Natural Support Strategies
Rashes are inflamed, irritated, red, or swollen skin that may be itchy, burning, or painful. They may develop due to allergic reactions, infections, medication, autoimmune conditions, bug bites, food, and other issues. Fortunately, rashes are rarely dangerous and can be treated with natural support strategies.
In this article, you will learn what rashes are. You will learn about different types of rashes, there signs and symptoms, causes, and risk factors. You will understand the difference between rashes and hives. You will learn about conventional treatment options for rashes. You will understand the functional root cause factors that may contribute to rashes. I will offer my best natural support strategies for rashes.
What Are Rashes
Rashes refer to inflamed, irritated, or swollen skin. A rash is a very broad term and depending on the type of rash, it may look o different. They may include swollen skin, red skin, scaly skin, blotchy skin, itchy skin, burning skin, dry skin, pimples, or sores.
Rashes may affect only one area of your skin, multiple areas, or your entire body. Some may develop right away due to an allergic reaction or trigger, others may take their time and develop slower (1).
While most rashes are relatively harmless and go away with home remedies, other rashes can become chronic, problematic, or even serious. If you are experiencing fever, blisters or open sores around your mouth, genitalia, or elsewhere on your skin, painful, rashes that spread rapidly all over your body, or rashes that don’t improve despite home care, seek medical attention to rule out infections or other serious issues (2).

Types of Rashes
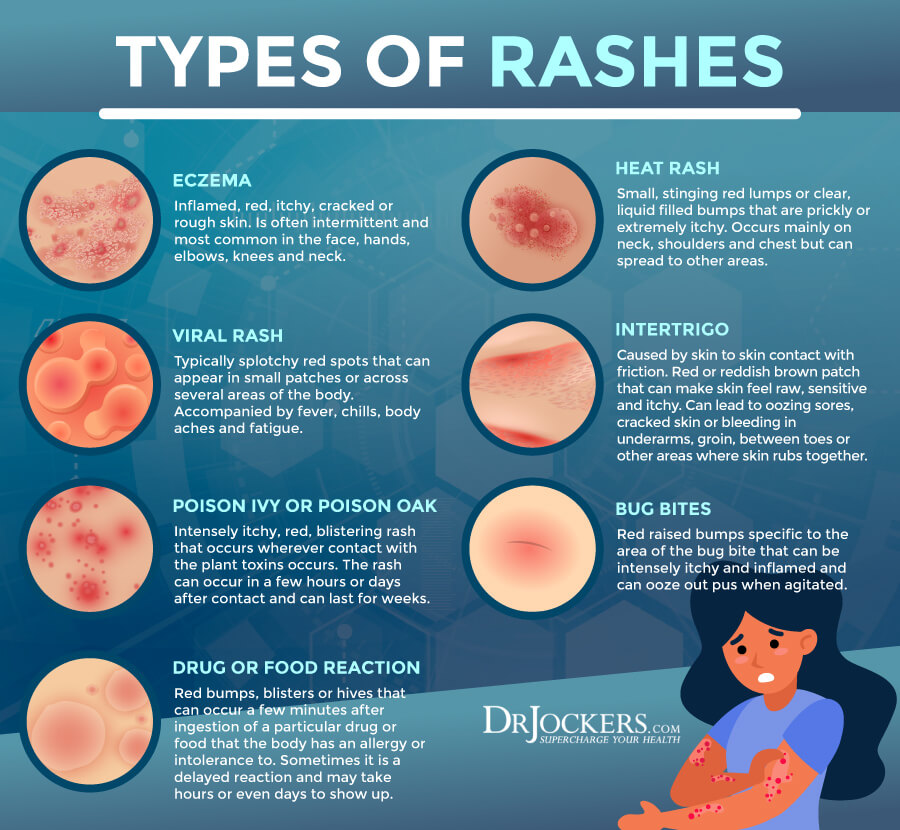
There are different types of rashes, including (1):
- Eczema
- Contact dermatitis
- Rosacea
- Psoriasis
- Seborrheic dermatitis
- Perioral dermatitis
- Shingles
- Chickenpox
- Measles
- Scarlet fever
- Impetigo
- Scabies
- Lichen planus
- Ringworm
- Flea bites
- Thick bite rashes
- Bull’s eye rash from some Lyme disease-carrying tick bites
- Cellulitis
- Butterfly rash from lupus
- Drug rash
Signs & Symptoms of Rashes
Signs and symptoms of rashes may include:
- Redness
- Swollen skin
- Scaling of the skin
- Blotchy skin
- Itchiness
- Burning
- Dry or crusty skin
- Blisters or oozing
- Pain
- Skin infection around open areas

Causes and Risk Factors
You may develop rashes for a variety of reasons. Causes and risk factors of rashes include (1):
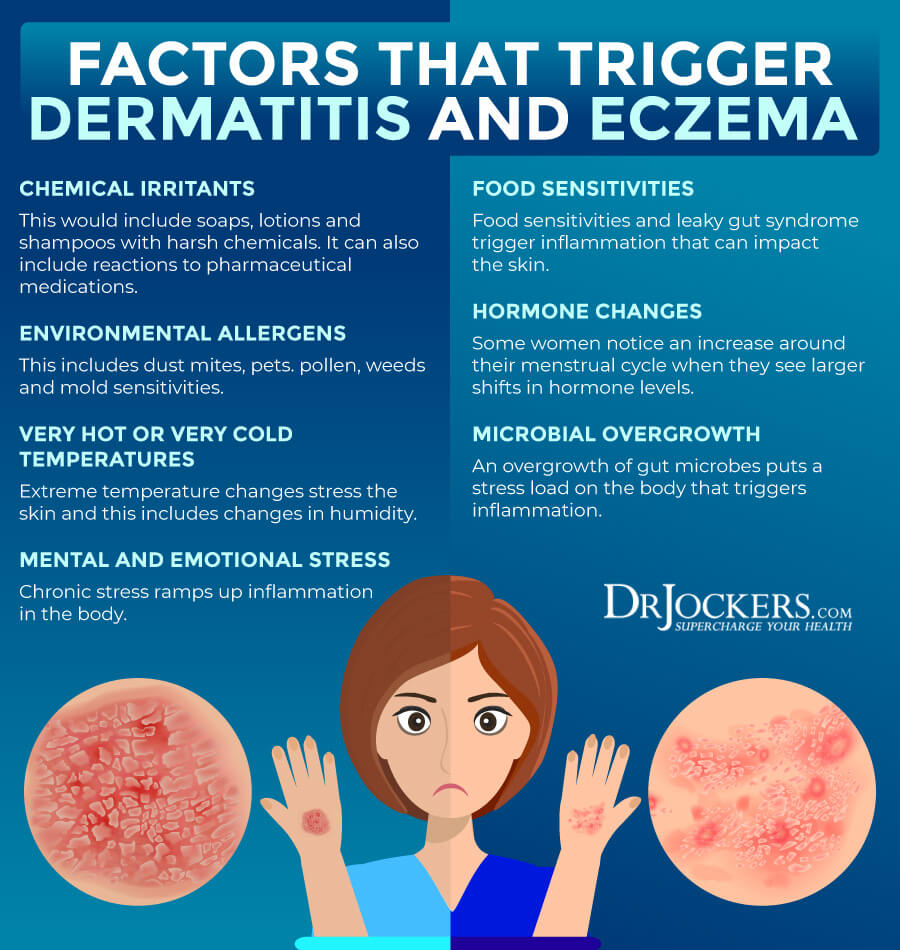
- Contact dermatitis: Contact dermatitis is a very common cause of skin rashes. It may develop if your skin is in contact with a substance that causes an allergic or adverse reaction. Conventional cleaning, body, and beauty products, dyes in clothing, latex, elastic, chemicals, and certain plants, such as poison ivy are common culprits of contact dermatitis.
- Insect bites: Bug bites, such as flea bites, tick bites, and scabies (tiny mites) can result in rashes.
- Fungal infections: Certain fungal infections such as ringworm or candidiasis can cause rashes.
- Bacterial infections: Certain bacterial infections such as impetigo and cellulitis can also lead to rashes.
- Viral infections: Certain viral infections, including chickenpox and measles also cause rashes.
- Rosacea: Rosacea is a skin rash that affects the face.
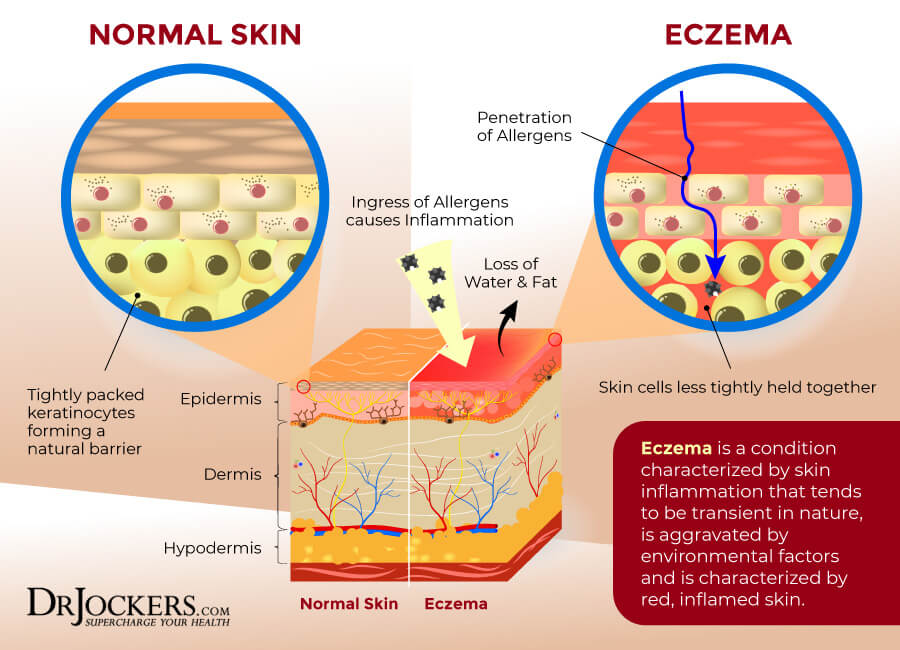
- Eczema: Eczema is a common skin problem. It is more common in those with allergies or asthma.
- Medications: Certain medications may cause an allergic skin reaction or photosensitivity.
- Diaper rash: Diaper rash is common in babies or anyone who needs to wear a diaper.
- Autoimmunity: Psoriasis is an autoimmune condition that causes skin rashes. Lupus can cause a so-called butterfly rash.
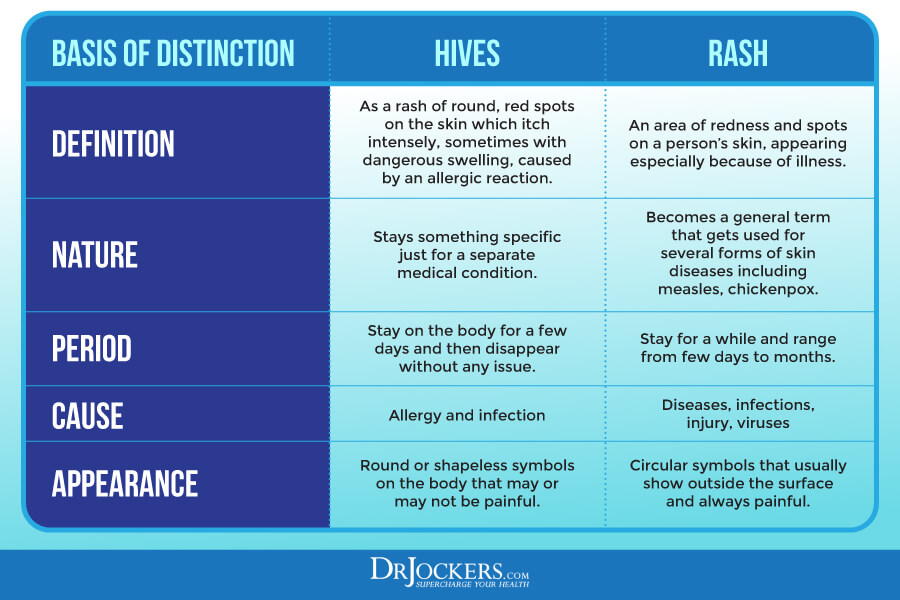
Difference Between Hives vs Rashes
Hives and rashes are not the same, but differentiating between the two is not always easy. Hives are characterized by raised and itchy bumps. They may be small or large, localized or spread across your body, red or skin-colored. They may appear quickly and disappear quickly but they may last for a longer time. They may reoccur. They are caused by some sort of allergy or allergic reaction.
Rashes are characterized by changes in your skin color or texture. They may feel rough, scaly, or bumpy. They may cause blisters, welts, or swelling. They may be itchy, but not always. They may also feel painful, scratchy, or irritated depending on the rash.
They may feel warm to the touch. They usually last for a longer time, days or weeks. They may reoccur. They may be caused by various issues, including allergies, eczema, contact dermatitis, infections, autoimmunity, medications, and diaper rash. You can find out more about the differences between rashes and hives here.
Conventional Treatment Options
Conventional treatment options include home care options, such as (2):
- Keeping the area clean
- Avoiding using hot water
- Allowing the rash to dry and avoiding the use of BandAids
- Avoiding cosmetics or other triggering products on the skin
- Over-the-counter (OTC) corticosteroids for itching and inflammation
- Antihistamine medications to reduce itching and inflammation
- Calamine for chickenpox, poison ivy, poison oak, and other painful rashes
- OTC NSAID’s such as Ibuprofen for pain
- OTC antibiotics or antifungal for bacterial or fungal rashes
Rashes that don’t go away may require medical attention. If your rash is caused by a bacterial infection, your doctor will likely recommend an antibiotic ointment. If your rash is caused by an autoimmune disease, you may be prescribed steroids, immunosuppressants, or other medications.

Functional Root Cause Factors
Now that you understand the potential causes and risk factors for skin rashes, it’s important that we talk about their functional root cause factors. While these functional root cause factors may not always cause a rash directly, they can make your body vulnerable and increase your risk of developing a rash.
Understanding these functional root cause factors, you can learn to improve your health and reduce your risks.

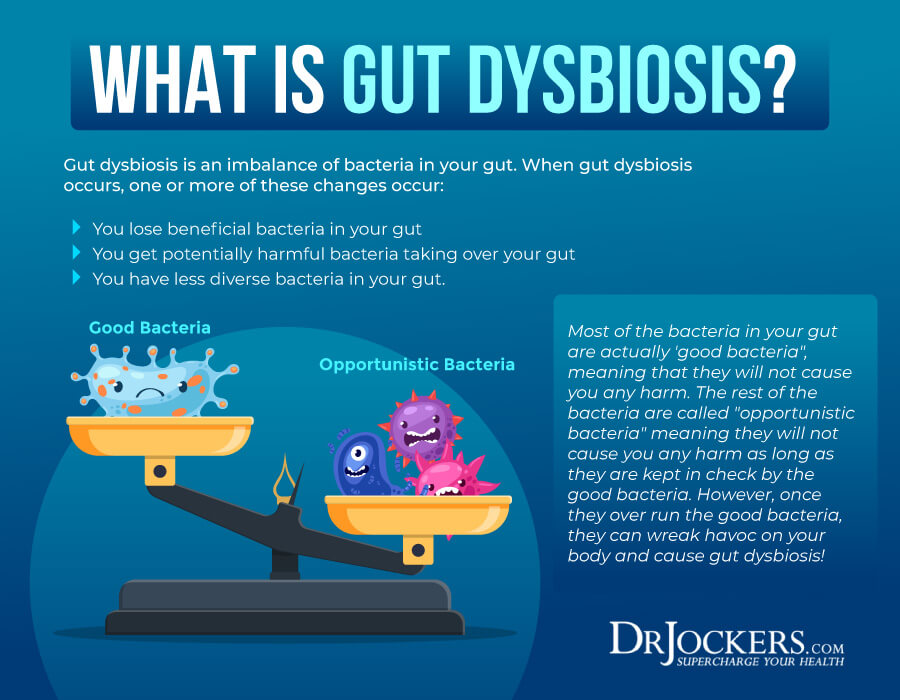
Gut Dysbiosis & Infections
Gut dysbiosis means that your gut microbiome is out of balance. There are too many harmful bacteria but too few beneficial bacteria to protect you. It may be surprising, but what happens in your gut doesn’t only affect your gut, but your entire body. Gut dysbiosis can seriously affect your skin. Rashes may be one of the signs that something is out of balance in your gut flora.
A 2021 review published in Microorganisms discussing the gut-skin axis has found a connection between gut dysbiosis and skin problems (3). Researchers found that your gut plays an important role in your immune system health.
Gut dysbiosis can affect your body’s immune response to allergens, toxins, and pathogens, causing dermatitis, psoriasis, dandruff, acne, or even skin cancer. Researchers found that diet also plays a critical role in the development of gut dysbiosis and consequent skin conditions.
Gut infections, especially H. pylori infection can often trigger skin reactions. A 2014 review published in the Hong Kong Medical Journal has found that H. pylori infections can trigger a chronic systemic immune response and inflammatory response, which can cause rosacea, idiopathic urticaria, and other skin problems characterized by rashes (4). A 2018 study published in BMC Infectious Diseases has also found that H. pylori infections can play a role in skin issues like rosacea (5).
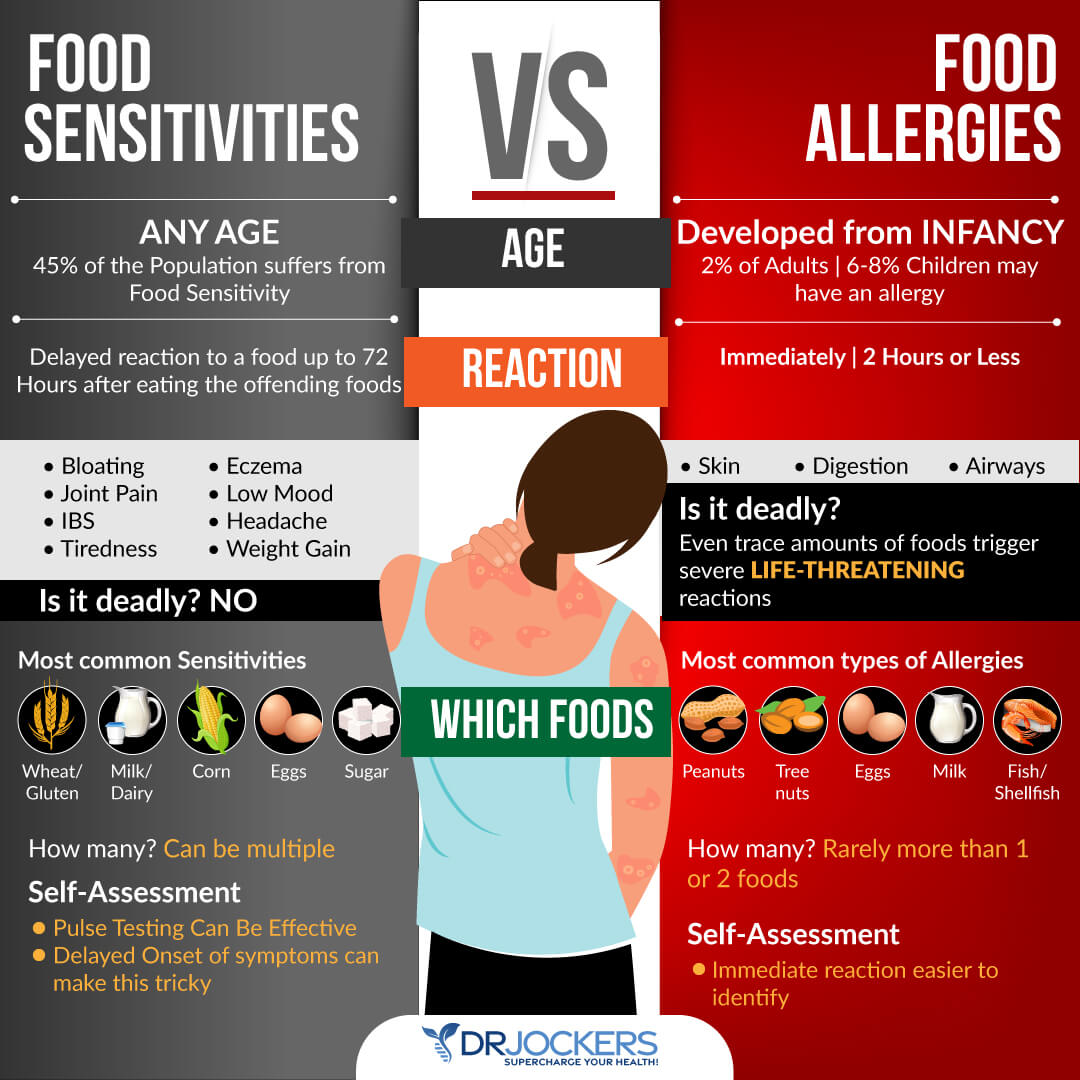
Food Sensitivities
Food allergies and sensitivities are some of the most common culprits behind rashes. A 2014 review published in the Journal of Clinical Aesthetic Dermatology has found that diet can trigger dermatitis (6). Food can trigger an immunoglobulin E-mediated hypersensitivity that may result in atopic dermatitis or eczema characterized by rashes.
Food allergies tend to cause an immediate reaction, while food sensitivities cause a delayed reaction. You may not notice a rash until hours or even days after eating a food that you are sensitive to. If you are consuming a food that you are sensitive to on a regular basis, it will cause chronic inflammation and ongoing symptom, such as rashes.
Rashes from food allergies often develop in the area where you came in contact with the food, such as your mouth, face, or neck. Food allergies may also cause other serious reactions such as wheezing or vomiting. Rashes from food sensitivities may develop anywhere. Food sensitivities may also cause other reactions, but it is usually difficult to connect the seemingly unrelated symptoms.
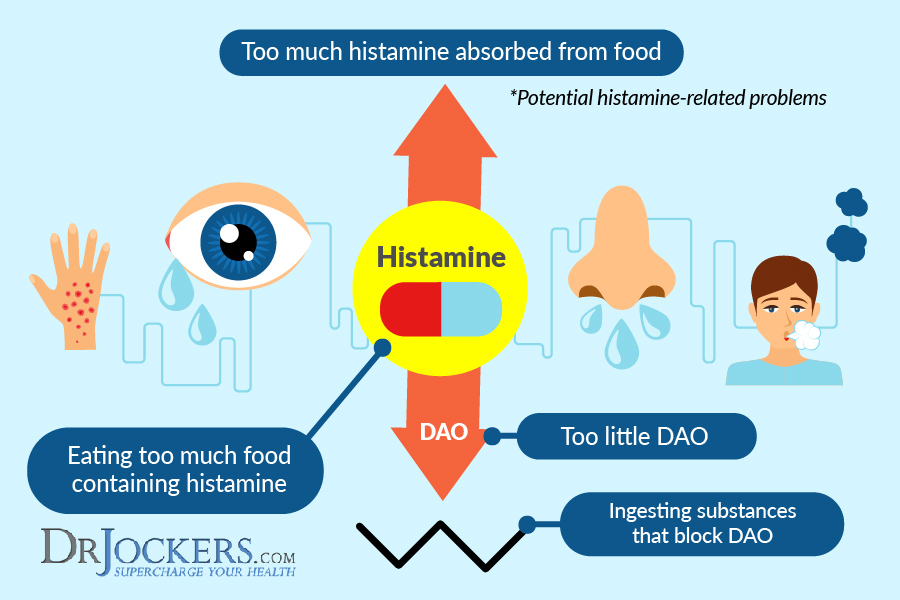
Histamine Intolerance
Histamines are important neurotransmitters and immune messengers that help your immune system in getting rid of allergens, toxins, and pathogens. They also support your gut health by releasing hydrochloric acid to break down food and gut bacteria. They also support your brain and mental health by serving as a messenger between your brain and the rest of your body.
Histamine is important. However, if you have too much histamine, it can become a problem. Histamine intolerance means that you have too much histamine causing a histamine build-up in your body. Histamine intolerance can affect your entire body and cause a variety of symptoms, including skin issues, migraines, digestive problems, brain fog, anxiety, and more.
Rashes, itching, and hives are some of the most common symptoms of histamine intolerance. A 2011 study published in the Annals of Dermatology has found that histamine intolerance may play a role in dermatitis (7). Researchers also found that a low-histamine diet may help to reduce symptoms and the risk of symptoms.
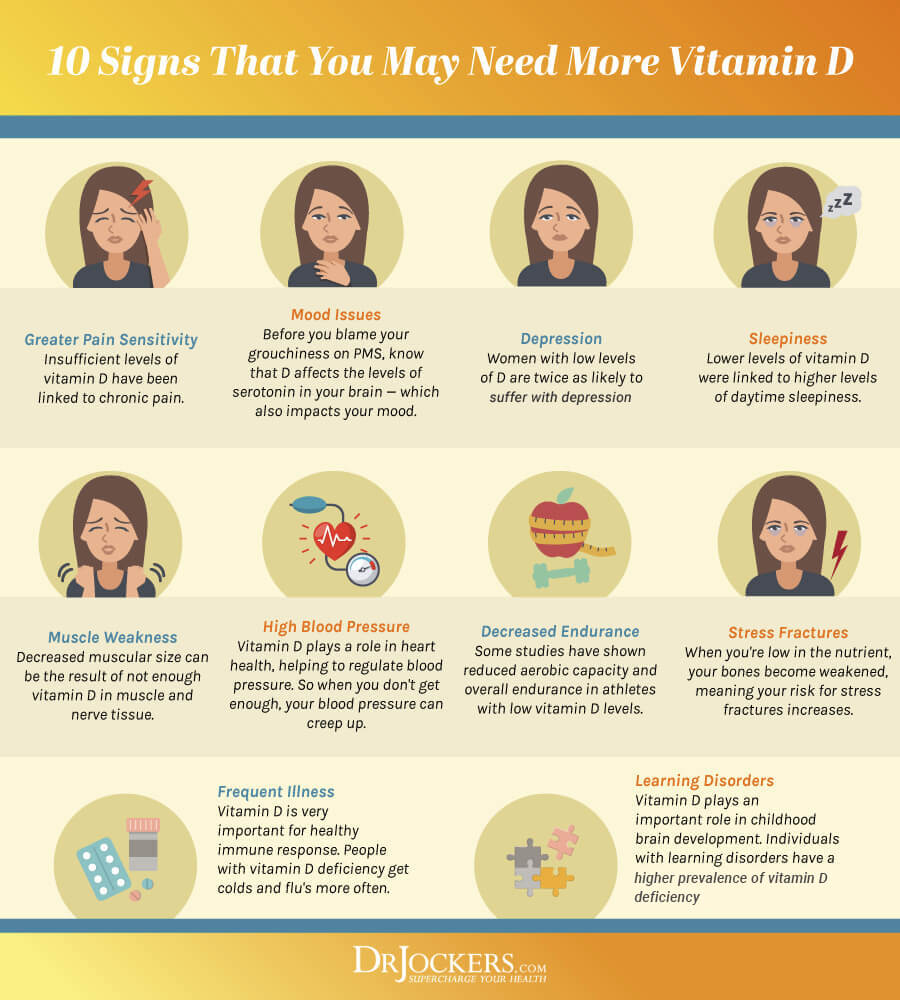
Vitamin D Deficiency
Vitamin D is one of the most important vitamins. Your body can convert vitamin D from sunshine and certain foods, including fatty fish, egg yolks, and beef liver. However, without adequate sunshine due to our modern, indoor life, and without supplementation, vitamin D deficiencies are very common. Beyond your skin health, vitamin D is vital for muscle and bone health, immune health, brain, and mental health.
A 2011 retrospective case series have found that vitamin D deficiency can cause idiopathic rash, itching, or hives (8). Researchers found that only an average of 4.2 weeks of vitamin D supplementation was able to improve the condition.
A 2015 study published in the Iranian Journal of Allergy, Asthma, and Immunology has found that vitamin D deficiency can cause idiopathic urticaria of the skin and vitamin D supplementation may help (9). A 2018 study published in Skin Pharmacology and Physiology has also found that vitamin D deficiency may contribute to psoriasis and atopic dermatitis (10).
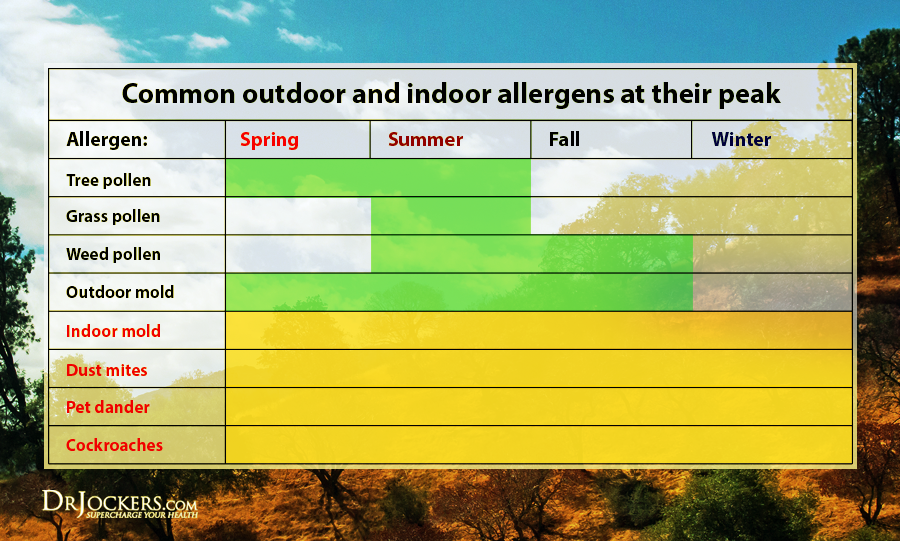
Environmental Allergy or Irritation
Environmental allergies or irritations are some of the most common causes of skin rashes (1). Exposure to chemicals, cotton or polyester, mold, bug bites, and other irritants can cause allergic reactions, irritation, and rashes.
A 2019 study published in the Journal of Preventive Medicine and Hygiene has found that many chemicals found in cosmetic products can cause allergic reactions, dermatitis, and other acute side effects (11). According to the United States Environmental Protection Agency, mold exposure can increase inflammation, an immune reaction, allergic reactions, and a list of symptoms, including skin rashes (12).
A 2008 paper published in the Journal of Family Health Care has found that certain fabrics cause atopic dermatitis (13). They found that synthetic fabrics and wool often cause itching, the dyes in cotton cause irritation and sensitivity, cotton can increase the risk of fungal and bacterial infections, and silk can cause allergic reactions.
A 2013 study published in the Indian Journal of Dermatology has found that dermatitis from insect bites is very common (14). According to the Asthma and Allergy Foundation of America, fleas, bedbugs, mosquitoes, kissing bugs, certain flies, cockroaches, ticks, dust mites, bees, hornets, wasps, and fire ants are common culprits of rashes, redness, pain, itching, swelling, and other skin inflammation (15).
Natural Support Strategies
There are a number of natural support strategies that you can use to improve your skin and overall health and reduce your risk for rashes. Here is what I recommend:
Anti-Inflammatory Nutrition Plan
A 2021 review published in Microorganisms has found that diet can play a role in the connection between gut dysbiosis and skin problems (3). Following an anti-inflammatory diet can help.
Beginning by removing inflammatory foods, such as refined sugar, refined oils, deep-fried foods, additives, artificial ingredients, conventional dairy, gluten, junk food, and highly processed food. Follow a diet rich in anti-inflammatory foods, including greens, vegetables, herbs, spices, low-glycemic index fruits, mushrooms, grass-fed beef, pasture-raised poultry and butter, wild-caught fish and seafood, and wild game. Choose organic to reduce exposure to pesticides, herbicides, hormones, and other toxins.
I recommend an anti-inflammatory diet that’s rich in healthy fats, such as good fats, such as avocados, coconut oil, grass-fed ghee or butter, olives, and extra virgin olive oil, and foods rich in omega-3 fatty acids, including wild-caught fish, flaxseeds, chia seeds, and hemp seeds.
I recommend using anti-inflammatory herbs and medicinal foods, such as ginger, turmeric, cinnamon, chili, cayenne, and black pepper, rosemary, cloves, and raw honey. You can learn more about an anti-inflammatory diet to rejuvenate your skin here.

Avoid Food Sensitivities and Intolerances
Food sensitivities and intolerances often cause rashes and other skin reactions (6). As a first step, I recommend testing for food sensitivities and food intolerances. Gluten, dairy, corn, soy, shellfish, seafood, tree nuts, and sugar are some of the most common food sensitivities behind rashes, however, any other food can cause reactions.
You can identify your personal food sensitivities with the combination of some blood tests, pulse testing, and an elimination diet. Once you identified your triggers, remove them from your diet.
Since food sensitivities can change over time, I recommend testing yearly or if you notice new symptoms. You can learn more about how to identify your food sensitivities in this article and how to reduce your food sensitivities in this article.

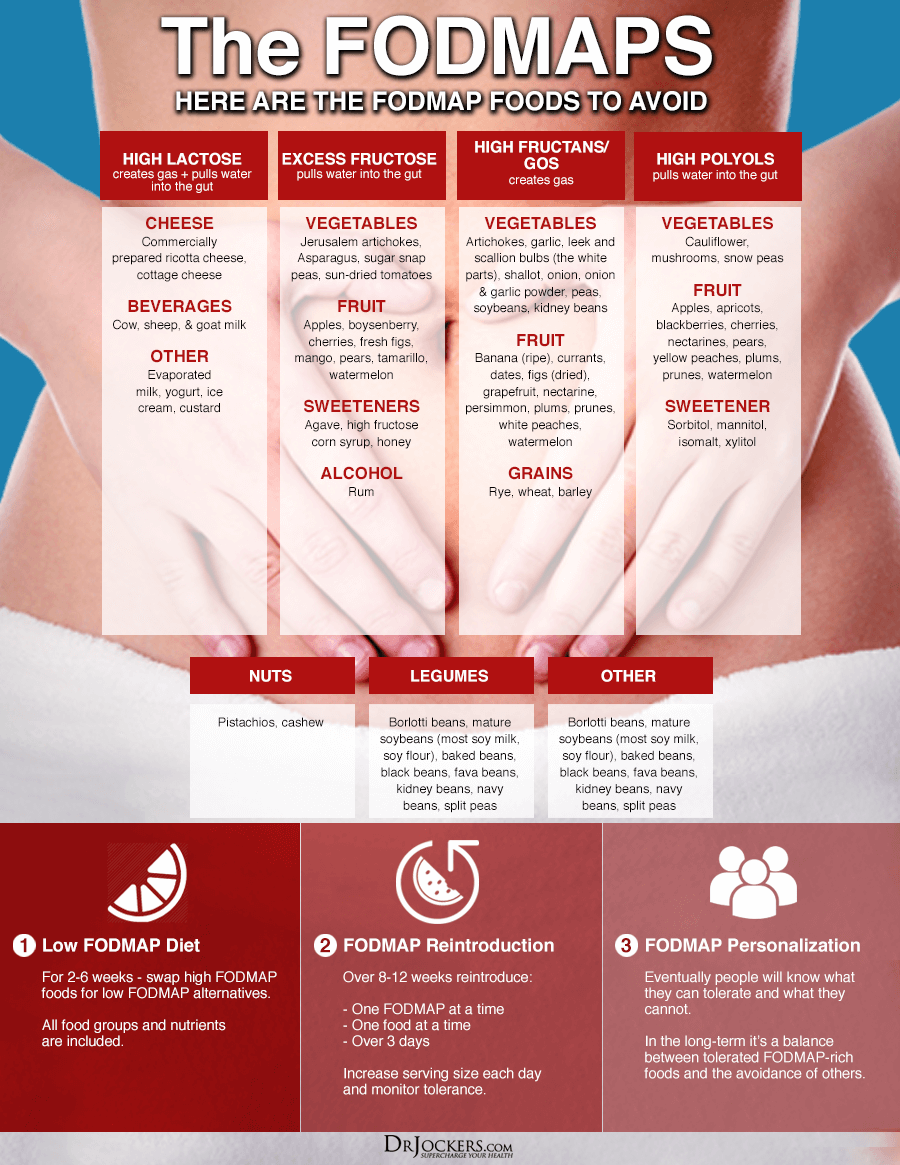
Consider Low-FODMAP Diet Trial
Gut dysbiosis and infections are some of the most common underlying functional root cause factors behind rashes (3, 4, 5). A 2020 systematic review published in Microorganisms has found that a low-FODMAP diet may help to improve gut microbiome health (16).
Thus a low-FODMAP diet may also reduce rashes due to gut dysbiosis and gut infections. FODMAP stands for Fermentable, Oligo, Di-, and Monosaccharides, and Polyols. The low-FODMAP diet is mainly used for small intestinal bacterial overgrowth (SIBO) and similar gut health symptoms because higher FODMAP foods, such as beans, grains, cruciferous veggies, and many fruits tend to increase SIBO symptoms.
Low-FODMAP vegetables include carrots, green beans, arugula, mint, basil, pepper, olive, pumpkin, tomato, potatoes, sweet potatoes, cucumber, zucchini, Swiss chards, lettuce, radishes, parsnip, sprouts, kale, and collard greens.
Low-FODMAP fruits include lemon, lime, kiwi, grapes, papayas, strawberries, raspberries, blueberries, melon, pineapples, and tangerines. Other low-FODMAP foods include egg, meats, fish, brazil nuts, chestnuts, butter, bone broth, seafood, quinoa, millet, rice, walnuts, and pine nuts. To learn more about the low-FODMAP diet, I recommend this article.
Consider Low-Histamine Diet Trial
Histamine intolerance and histamine reactions are common causes behind rashes (7). To rule out or improve histamine intolerance, I recommend a low-histamine diet trial. High-histamine foods include avocados, tomatoes, bananas, strawberries, dried fruits, most citrus, eggplant, spinach, vinegar, vinegar-containing foods, cashews, walnuts, peanuts, fermented foods, cheeses, smoked fish, cured meat, many spices, processed foods, and leftovers.
I recommend that you remove all high-histamine foods for about a month. If you don’t feel better, you may need to try another month, or there may be other causes behind your rashes.
If you feel better, you can start re-introducing higher histamine foods one by one at limited amounts depending on how you tolerate them. Everyone’s tolerance is different. If you are prone to histamine intolerance, you may need to limit high-histamine foods long-term.
Beyond foods, other factors, such as chronic stress, toxins, environmental issues, gut health issues, and certain medications can also increase your histamine load. To reduce histamine intolerance and related symptoms, it is important that you address these health and lifestyle factors as well beyond your diet. You may learn more about histamine intolerance and what to do about it by reading this article.

Use Non-Toxic Personal Hygiene Products
Conventional personal hygiene, skin care, beauty, and cleaning products tend to be full of chemicals and toxins that can irritate your skin and cause allergic reactions, dermatitis, and other acute side effects (11). I recommend that instead of conventional products, you choose non-toxic personal hygiene products, such as natural, organic, and homemade options.
Watch out for any perfumes or chemicals on the ingredient list that may cause irritation. You can learn more about natural skin, beauty, and hygiene products in this article. You can learn more about my wife, Angel’s natural skin care regimen from this video.

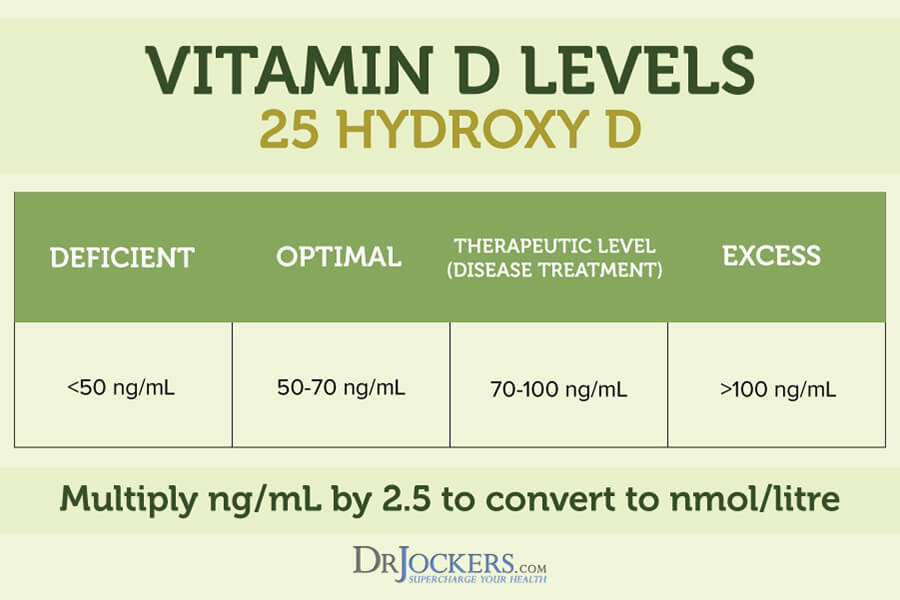
Optimize Vitamin D Levels
Research has found that vitamin D deficiencies may increase your risk for rashes and skin issues and vitamin D supplementation may help (8, 9, 10). To optimize your vitamin D levels I recommend spending time out in the sun and eating vitamin D-rich fatty fish, egg yolks, and beef liver. However, sunshine and food are not enough. I recommend daily supplementation with vitamin D3.
Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and inflammation control. I recommend taking a vitamin D3 supplement with at least 3,000-5,000 IU’s of vitamin D3 and at least 90 mcg of vitamin K2. I highly recommend this Vitamin D3/K2 Power. This supplement supports your immune, skin, cardiovascular, and bone health.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for major health conditions is going to be between 70-100 ng/ml.
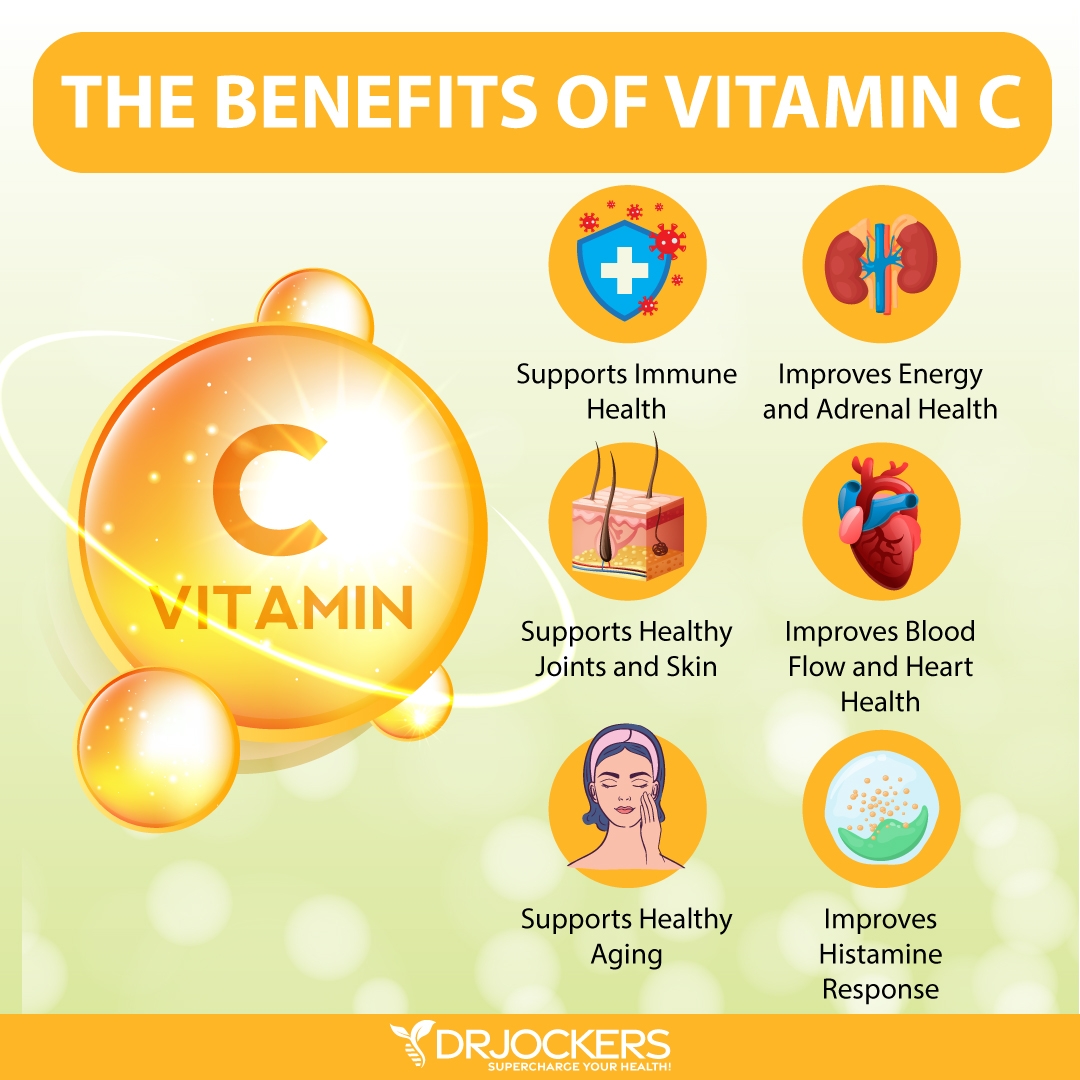
Boost Vitamin C Levels
Vitamin C is a powerful vitamin that offers antioxidant and immune support, as well as skin health benefits. It is found in a number of foods including, lemon, lime, oranges, mandarins, other citrus, strawberries, kiwi, blackcurrant, pineapple, peppers, broccoli, Brussels sprouts, and potatoes.
A 2017 review published in Nutrients has found that vitamin C offers protection from UV photodamage and oxidative stress (17). A 2018 review published in Frontiers in Physiology has found that vitamin C helps to protect you from skin oxidation and the development of certain skin conditions, including atopic dermatitis (18).
To support your skin health, I recommend using Super C with high-potency vitamin C and bioflavonoid protection.
Use Quercetin and Bioflavonoids
Quercetin is a plant flavonol with anti-inflammatory and histamine-reducing benefits. It can be found in grapes, apples, blueberries, black plums, cherries, cranberries, chokeberries, black currants, cruciferous vegetables, red leaf lettuce, romaine lettuce, kale, cabbage, kale, chicory greens, sprouts, red onions, snap peas, asparagus, peppers, herbs, and olive oil.
A 2019 review published in Molecules has found that quercetin offers anti-allergic benefits (19). A 2020 review published in Allergy, Asthma, and Clinical Immunology has found that quercetin may inhibit histamine production, reduce inflammation, and reduce an inflammatory immune response (20).
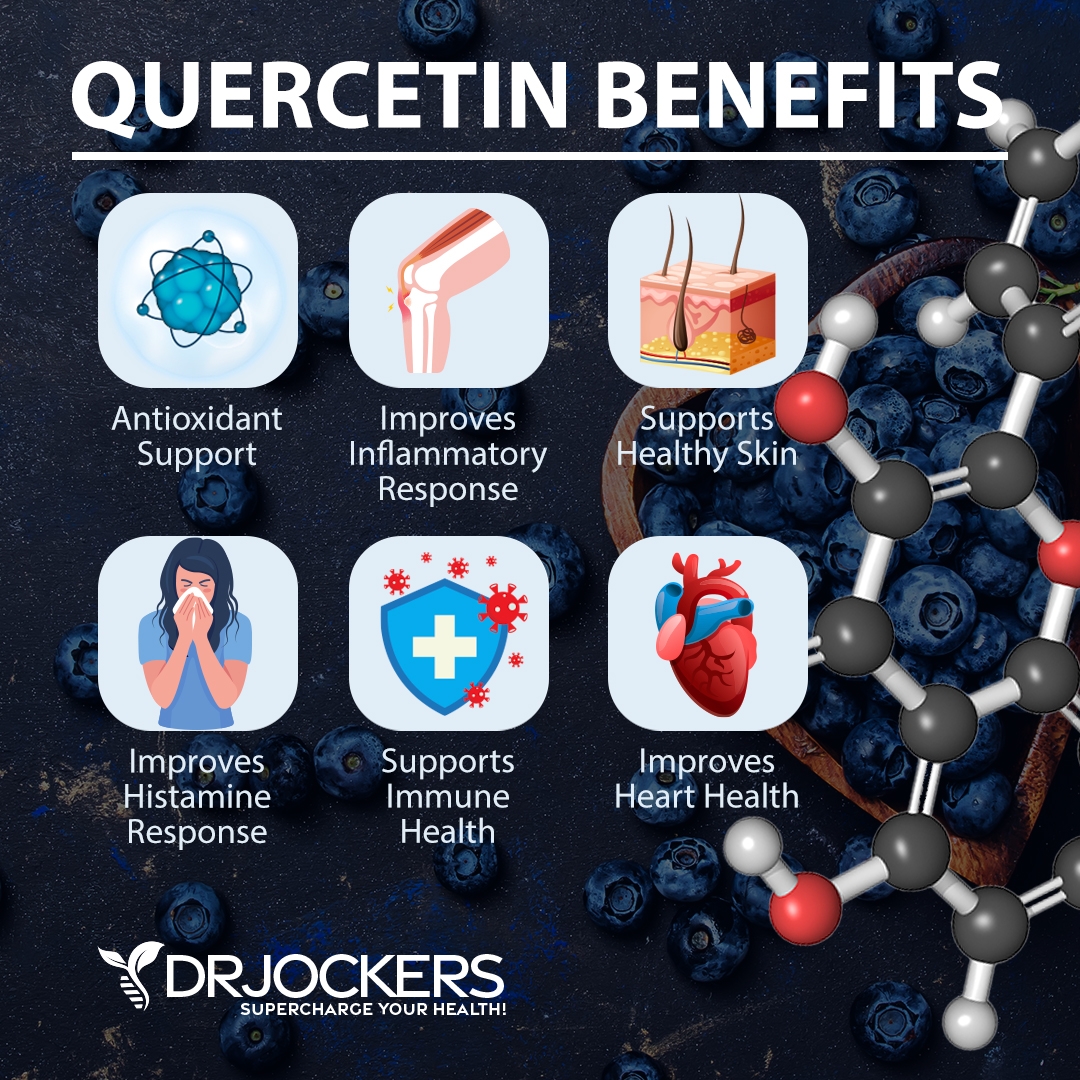
A 2016 study published in Clinical, Cosmetic, and Investigative Dermatology has found that quercetin may offer anti-itch benefits when used as a cream (21). These studies show that quercetin may reduce the risk of allergy- and histamine-related rashes.
Bioflavonoids are protective compounds found in citrus and berries mainly. Bioflavonoids are phytochemicals that are often found together with vitamin C in nature and are generally considered to be among the most important and interesting classes of biologically active compounds in contemporary research.
They offer anti-aging and other health benefits. A 2012 study published in Dermato Endocrinology has found that bioflavonoids may improve skin health and reduce skin aging (22).
I recommend Resveratrol Power with both quercetin and resveratrol for anti-inflammatory and anti-histamine benefits.
Consider Using Aloe Vera and Lavender on Rash
Aloe vera is a plant that has been used as a natural remedy for over 6,000 for sunburn, burn, and various skin problems. Aloe vera used typically offers soothing, hydrating, cooling, and healing properties. It is anti-inflammatory and antibacterial.
A 2012 clinical study published in Hindawi has found that aloe vera may be effective for diaper rash (23). It may be helpful for eczema, heat rash, allergic reactions, and irritation. Scoop out the inside of an aloe vera leaf to use it on your rash as needed.
Lavender essential oil is another natural remedy that may be helpful for rashes. A 2015 study published in Scientifica has found that lavender essential oil may offer anti-fungal benefits (24). It may help rashes from ringworm and other fungal infections. It’s also very moisturizing and soothing.
A 2002 study published in the Archives of Pharmaceutical Research has found that lavender essential oil may also be beneficial against staphylococcus aureus that may cause eczema (25). Mix two drops of lavender oil with two tablespoons of coconut oil and use it on your rash daily until it feels better.

Consider Using Bentonite Clay
Bentonite clay is a natural healing clay that helps to remove dirt, toxins, and oils from your skin. A 1995 study published in the Journal of American Academy of Dermatology has found that bentonite clay may help to prevent an allergic reaction from poison ivy and poison oak (26). A 2014 study published in the Journal of Research in Medical Sciences has found that bentonite clay may help to improve diaper rash (27).
To use bentonite clay on a rah, first wash your skin where the rash is is. Then mix bentonite clay with water. Apply it to the skin on the affected area. Let it dry. Rinse within an hour. Use daily as needed.

DIY Rash Cream
If you are experiencing a rash, I highly recommend trying this simple, natural DIY rash cream with bentonite clay, aloe vera, and lavender. You can prepare this recipe ahead of time, store it in a glass jar, and use it when needed. Here is how to make it:
Ingredients:
- ¼ cup cocoa butter or coconut oil
- ⅛ cup olive oil
- 2 tbsp bentonite clay
- 2 tbsp aloe vera gel
- 10-12 drops lavender essential oils
- 1-2 tbsp witch hazel
Directions:
- Add the cocoa butter and olive oil to a pan. Using a double boiler on low, melt it while stirring.
- Add and stir in the aloe vera gel.
- Remove from the heat.
- Add and stir in the bentonite clay, lavender, and witch hazel until blended.
- Once done, put it in a glass jar with a tight-fitting lid to keep it for later use as needed.
- If you have a rash, apply it to the affected skin area twice a day.
- Let it dry for about 15 minutes, then rinse it off with warm water. Pat dry with a clean washcloth.

Purity Woods Age-Defying Dream Cream
Healthy, radiant looking skin is certainly a confidence booster. It is a goal that everyone tries to achieve (and keep) throughout their lives. As we begin to get older, there are millions of tricks, tips and procedures out there to maintain the same healthy-looking skin we had when we were younger.
That’s why I would like to share my top choice for keeping skin looking young and healthy – the USDA Certified Organic Age-Defying Dream Cream from Purity Woods.
This anti-aging cream is truly a game changer when it comes to achieving and KEEPING your skin looking and feeling spectacular. Now you can save up to 38% on this amazing product, simply click here to learn more!
Final Thoughts
Rashes are inflamed, irritated, red, or swollen skin that may be itchy, burning, or painful. Fortunately, rashes are rarely dangerous and can be treated at home naturally. I recommend trying my natural support strategies for rashes and skin health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!





Does it matter which type of bentonite clay is used? I’ve read somewhere else that calcium bentonite is used for topical and internal use, and that sodium bentonite is used for more industrial applications – like pond sealants! But most of the bentonite I see for sale, even food-grade, says it is sodium bentonite. I was hoping to use it for foot soaks or clay masks on irritated skin and rashes like you suggest here. Is sodium bentonite safe and effective for these uses? Thank you!
Sulphur soap or ointments or sulphur bath soaks can be very helpful as well.
Thanks for sharing!
Is unscented all natural goats milk soap a good remedy for contact dermatitis? I’ve read many testimonials about how it helped and even restored their inflamed skin! People with eczema and psoriasis have found excellent results!
Your thoughts?
Not familiar with it but I am sure the short chain fatty acids and immunoglobulins in the goat’s milk may have benefit.
Is unscented all natural goats milk soap a good remedy for contact dermatitis? I’ve read many testimonials about how it helped and even restored their inflamed skin! People with eczema and psoriasis have found excellent results!
Your thoughts?
Yes that can be very helpful!