 Osteoarthritis: Symptoms, Causes & Natural Support Strategies
Osteoarthritis: Symptoms, Causes & Natural Support Strategies
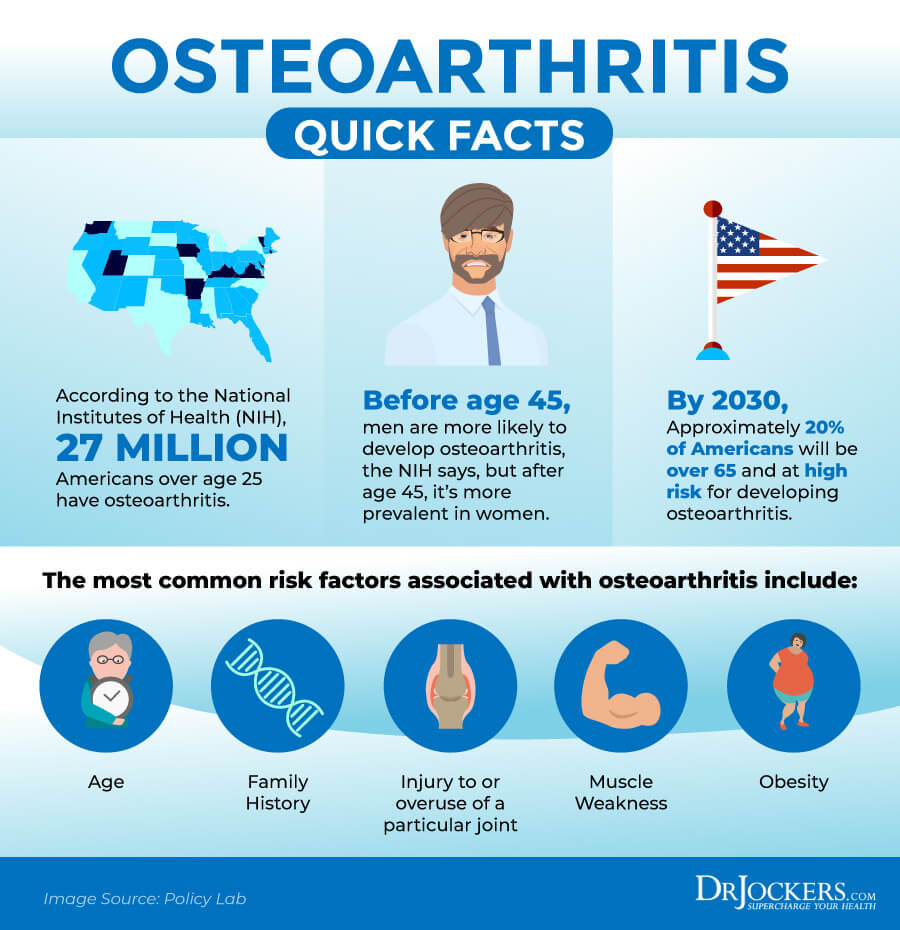
Did you know that there is more than one form of arthritis? Osteoarthritis is the most common form of arthritis that affects about 32.5 million people in the United States. Osteoarthritis or degenerative joint disease is characterized by the breakdown of your joints, cartilage, and bones most commonly in your hips, knees, hands, lower back, neck, and spine.
Osteoarthritis may cause pain, swelling, inflammation, and loss of movement. It can become a debilitating condition that leads to disability in millions of people. You don’t have to become one of them. You can improve your joint health and reduce your symptoms with the help of some simple natural support strategies, including diet and lifestyle changes and appropriate supplementation.
In this article, you will learn what osteoarthritis is. I will discuss its four stages and the most common symptoms. You will understand the root causes of osteoarthritis. I will share my best natural support strategies to support your joints and improve your health.
What Is Osteoarthritis
According to the Centers for Disease Control and Prevention 32.5 million adults are dealing with osteoarthritis in the United States alone (1). Osteoarthritis is also referred to as OA, ‘wear and tear arthritis’, or degenerative joint disease. It is the most common form of arthritis that you may develop. Osteoarthritis develops most commonly in your hips, knees, hands, and spine, but it doesn’t mean that it can’t affect other joints (1).
Osteoarthritis is a chronic, long-lasting, and progressive condition. While it shares many of the same symptoms with rheumatoid arthritis (RA), osteoarthritis is a degenerative joint condition while rheumatoid arthritis is an autoimmune one. Rheumatoid arthritis involves an autoimmune process and inflammation, while osteoarthritis occurs because of the breakdown of your cartilage, joints, and bones.
Symptoms of rheumatoid arthritis may come in flares while osteoarthritis is more constant. Rheumatoid arthritis tends to affect both sides symmetrically while osteoarthritis is usually unilateral and may affect only one knee or hip.
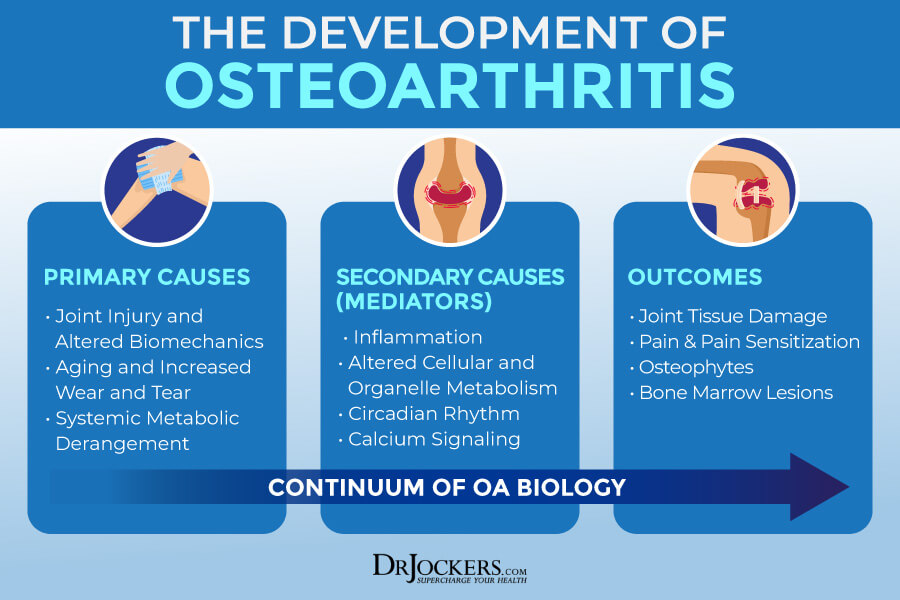
Pathogenesis of Osteoarthritis
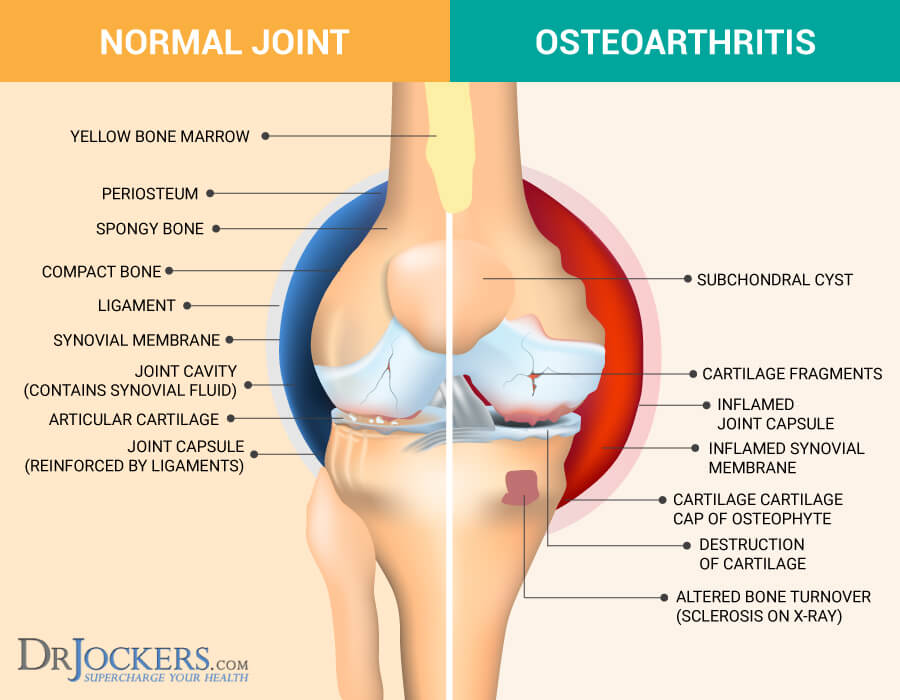
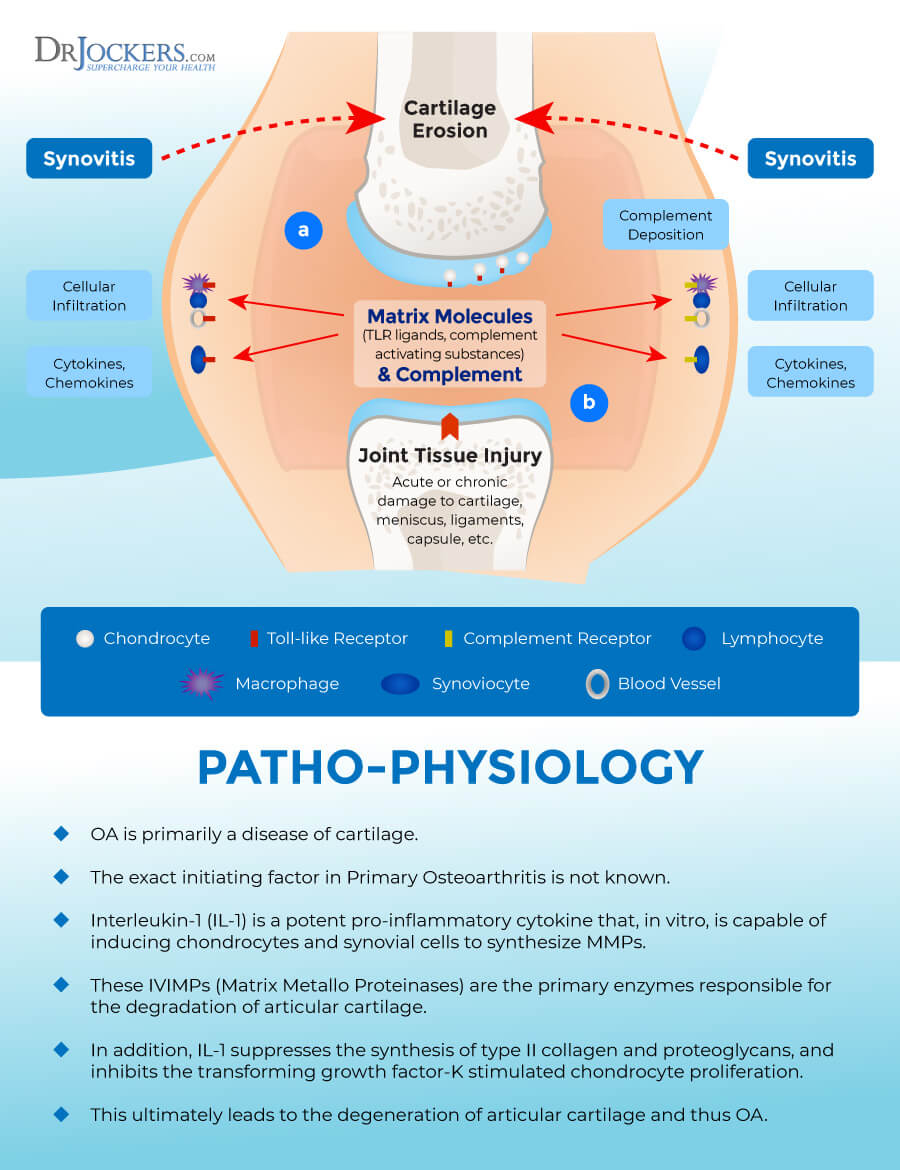
Your joints are areas of your body where two bones come together and are protected by a tissue called cartilage. Having osteoarthritis means that the cartilage in your joints starts to break down. This causes the bones within your joints to rub together. As a result, your bones underneath and near the joints start to change. This is a gradual process that develops slowly and gets worse over time, so it’s not surprising that your risk of osteoarthritis increases with age (1).
Osteoarthritis is characterized by joint pain, stiffness, and swelling that may reduce function. Severe osteoarthritis can lead to disability. Many people with osteoarthritis are unable to participate in activities, do their work, and perform daily tasks that they were used to (1).
Stages of Osteoarthritis
Osteoarthritis is a degenerative, chronic, and progressive condition that can worsen over time. It has 4 stages that we can determine through x-rays and imaging.
Stage 0 – Normal
This stage means that your joints are healthy. There is no sign of osteoarthritis. Your joints, bones, and cartilage are healthy without any signs of damage or impairment.
Stage 1 – Minor
At this early stage of osteoarthritis, there is very minor wear and tear or bone spur growth at the end of the joints. At this stage, you may not even be aware that you have osteoarthritis since pain or discomfort is rare. At this stage, besides lifestyle changes and supplementation that support joint health, your orthopedic doctor will likely not recommend any special treatment.
Stage 2 – Mild
Though this stage is not yet serious, diagnostic imaging will show more bone spur growth. The cartilage and other soft tissues are at a healthy size, however, the proteolytic cartilage breakdown has begun.
At this point, you may start noticing joint pain and other symptoms, especially stiffness after sitting for a longer period of time, in the morning, or after working out. At this point, you may be recommended strength training and physical therapy for joint stability, braces, shoe inserts, or other supportive devices, and in some cases, pain-relieving medication by your orthopedic doctor.
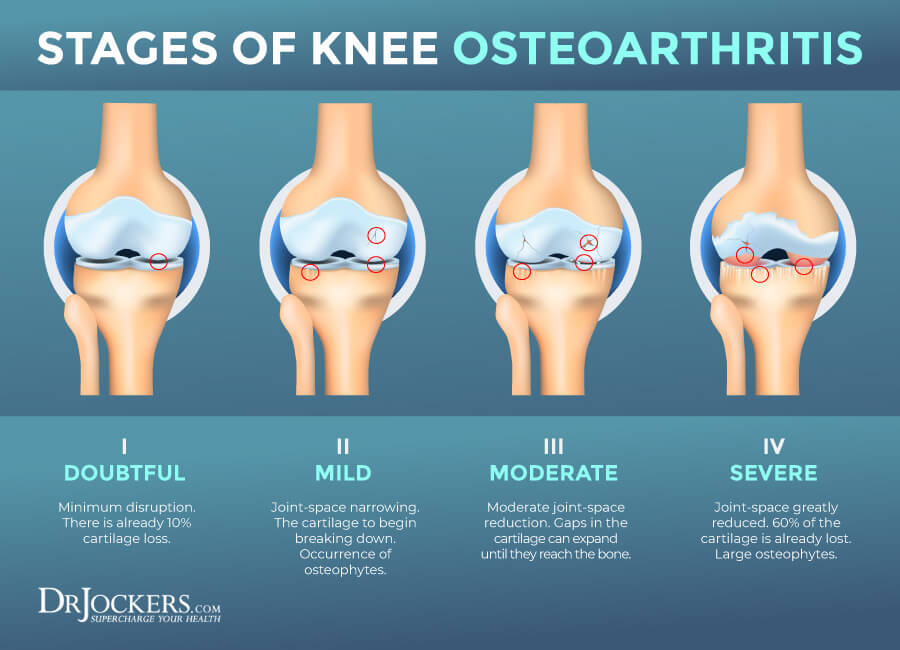
Stage 3 – Moderate
It may be called moderate, but osteoarthritis at this point can get really uncomfortable. There is a clear erosion to the cartilage surface and a visible gap between bones. There are bone spurs and your joints feel rougher.
At this stage, the inflammation is more serious and you will likely experience pain and discomfort when walking, kneeling, squatting, running, or otherwise moving.. Sitting for too long can cause stiffness. You may also feel very stiff upon waking. You may experience popping and snapping sounds as well.
At stage 3, orthopedic doctors tend to start recommending over-the-counter pain-reliever and NSAID medication, or if those don’t help, stronger drugs, including oxycodone and codeine. Besides medication, physical therapy, weight loss, intra-articular injections may be part of your treatment working with a traditional doctor.

Stage 4 – Severe
This is the most severe stage of osteoarthritis where the cartilage wear-off is serious with more bone damage and reduces joint space between the bones. There are more bone spurs as well. The creation of cytokines, TNF, and synovial metalloproteinases increases that may diffuse back into your cartilage leading to the destruction of your soft tissues.
This will also cause chronic inflammation, increased pain, and joint stiffness. Walking, moving, standing up, and in some cases, even sitting can become difficult and painful. Disability is very common at this stage.
At this stage of osteoarthritis, orthopedic surgeons often recommend surgery. They may recommend osteotomy or bone realignment surgery. The goal is to cut the bone above or below the joint to shorten and realign it to relieve stress and protect your bones from further bone damage and bone spur growth.
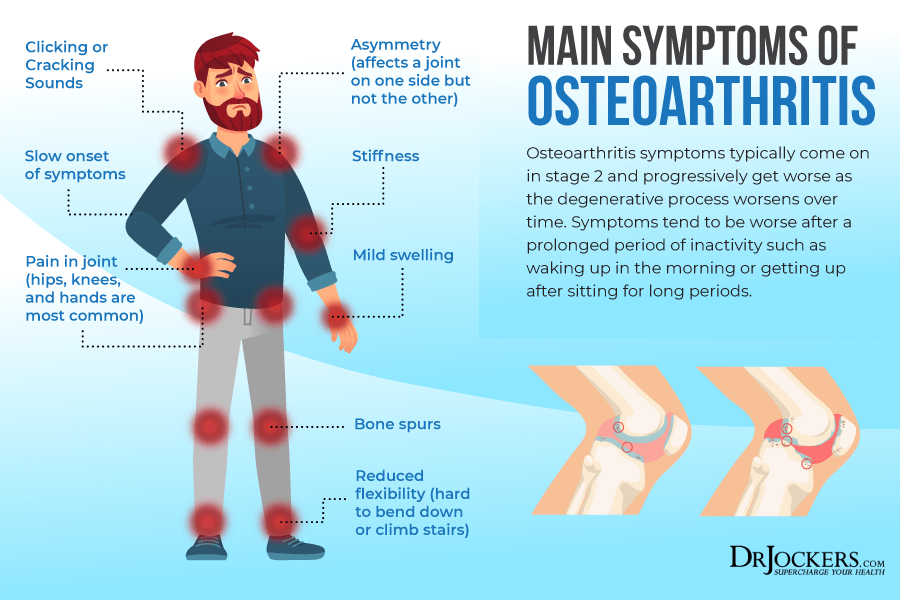
Major Symptoms of Osteoarthritis
While osteoarthritis may occur in any of your joints, the most common areas it may affect include your knees, hips, spines (usually in your lower back or at your neck), hands, and fingertips. Major symptoms of osteoarthritis may include (1):
- Pain
- Aching
- Stiffness
- Tenderness
- Discomfort
- Swelling
- Decreased motion
- Decreased flexibility
- Inflammation
Over time as osteoarthritis progresses, the pain becomes more intense. If you are experiencing joint inflammation or any symptoms of osteoarthritis, it’s important that you visit your healthcare professional for the right diagnosis. Symptoms of osteoarthritis may overlap with rheumatoid arthritis or other joint inflammation, but your treatment protocol may significantly differ depending on your diagnosis and the cause of your condition.
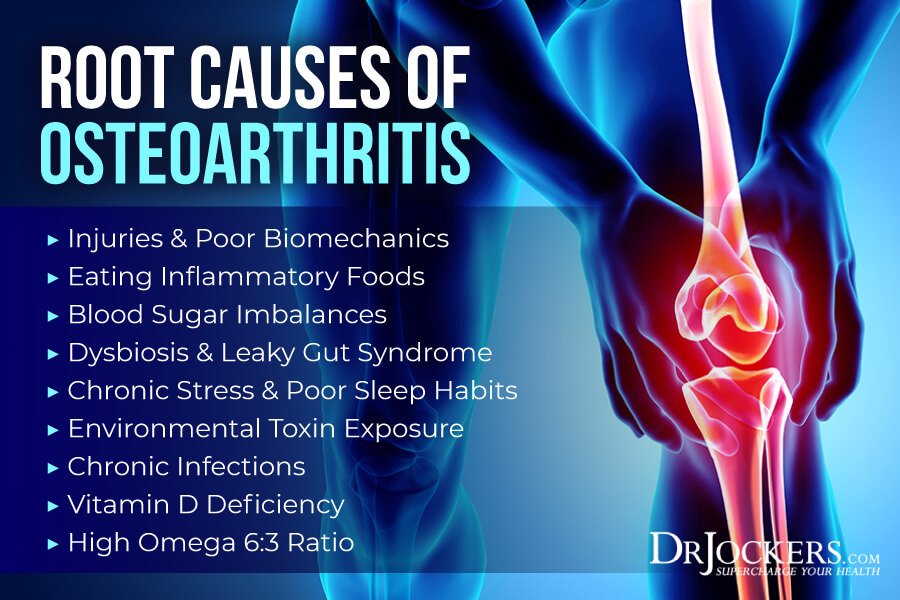
Root Causes of Osteoarthritis
You may develop osteoarthritis over time for a number of reasons. Here are the top root causes of osteoarthritis.
Injuries & Poor Biomechanics
A 2013 study published in Osteoarthritis Cartilage has found that osteoarthritis is a disease of mechanics that may develop because of mechanically induced injury to the joints that can increase inflammation and worsen any structural damage (2). The term biomechanics refers to how your body (bio) moves (mechanics).
When we talk about your biomechanics, we talk about movements that involve your joints, muscles, and nerves. Poor biomechanics makes your joints, muscles, and nerves undergo something that is not familiar, normal, or healthy to your body. It leads to irritation and aggravation that may result in pain or discomfort.
On-going and unaddressed poor biomechanics are a problem because they can result in chronic pain, joint inflammation, injuries, and osteoarthritis. Injuries to or around the joints can also lead to further joint inflammation and the development of osteoarthritis. Moreover, long-term or chronic injuries can also cause further muscle weakness, overcompensation, and poor biomechanics.
This can further feed into your issues and increases your risk of the development or worsening of osteoarthritis. Poor biomechanics, joint inflammation, muscle weakness, and osteoarthritis can turn into a vicious cycle unless your biomechanics are corrected.
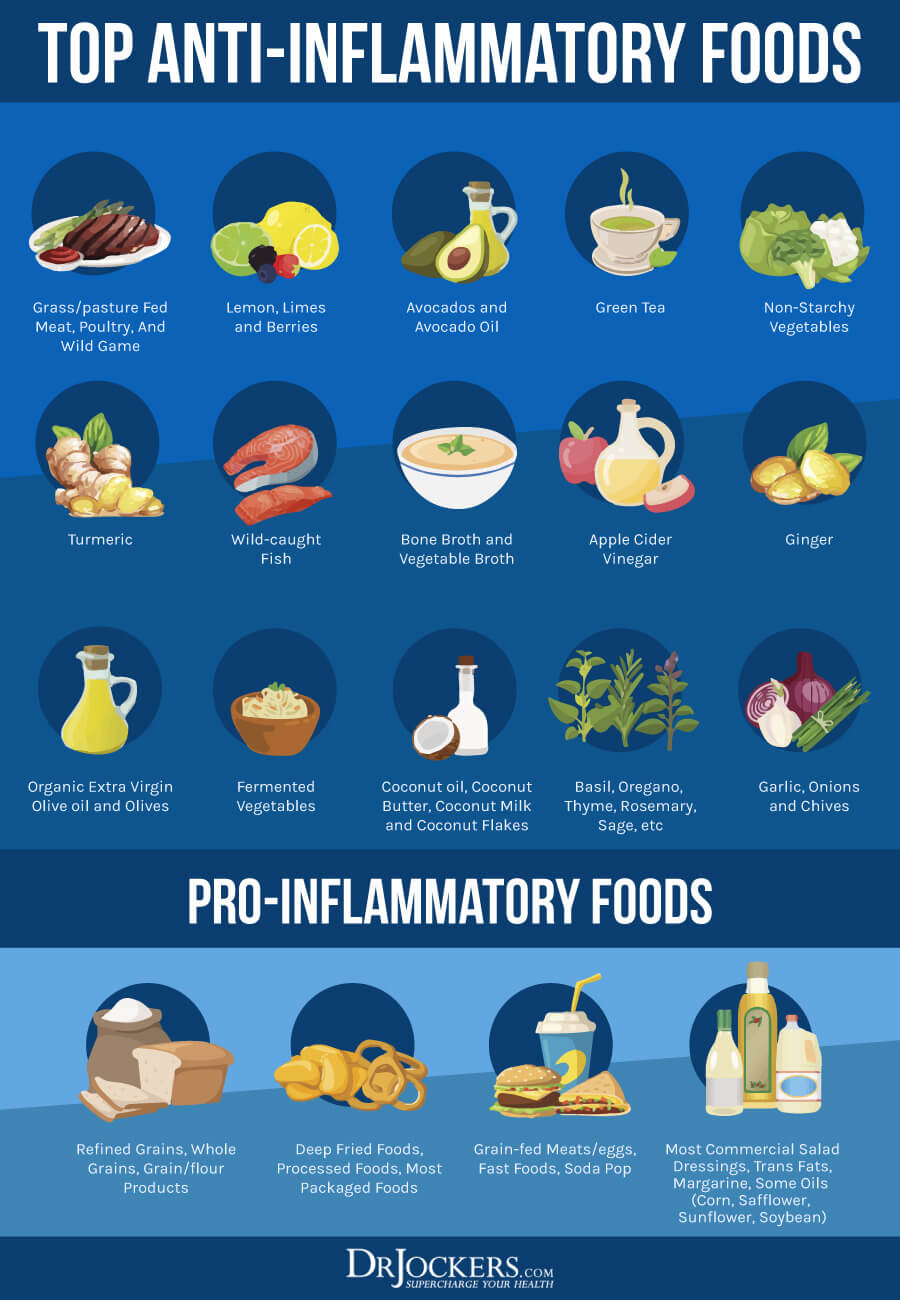
Eating Inflammatory Foods
Osteoarthritis is a degenerative joint condition that is characterized by inflammation and pain, especially in later stages. Eating too many inflammatory foods, including refined sugar, refined carbohydrates, refined oils, artificial ingredients, conventional and processed animal products, conventional dairy, junk food, highly processed foods, and food sensitivities can increase inflammation and aggravate symptoms of osteoarthritis.
A 2016 study published in Nutrition & Diabetes has found that adults between ages 20 and 30 years old who drank soft drinks sweetened with high-fructose corn syrup were more likely to develop joint inflammation than those who did not (3). According to a 2018 study published in Rheumatology diet and nutrition plays an enormous role when it comes to osteoarthritis. (4).
Eating an anti-inflammatory, whole foods diet, however, can reduce your symptoms and risk of osteoarthritis. According to this study, consuming plenty of antioxidants, polyunsaturated fatty acids (PUFAs), and vitamin D and K is absolutely critical.

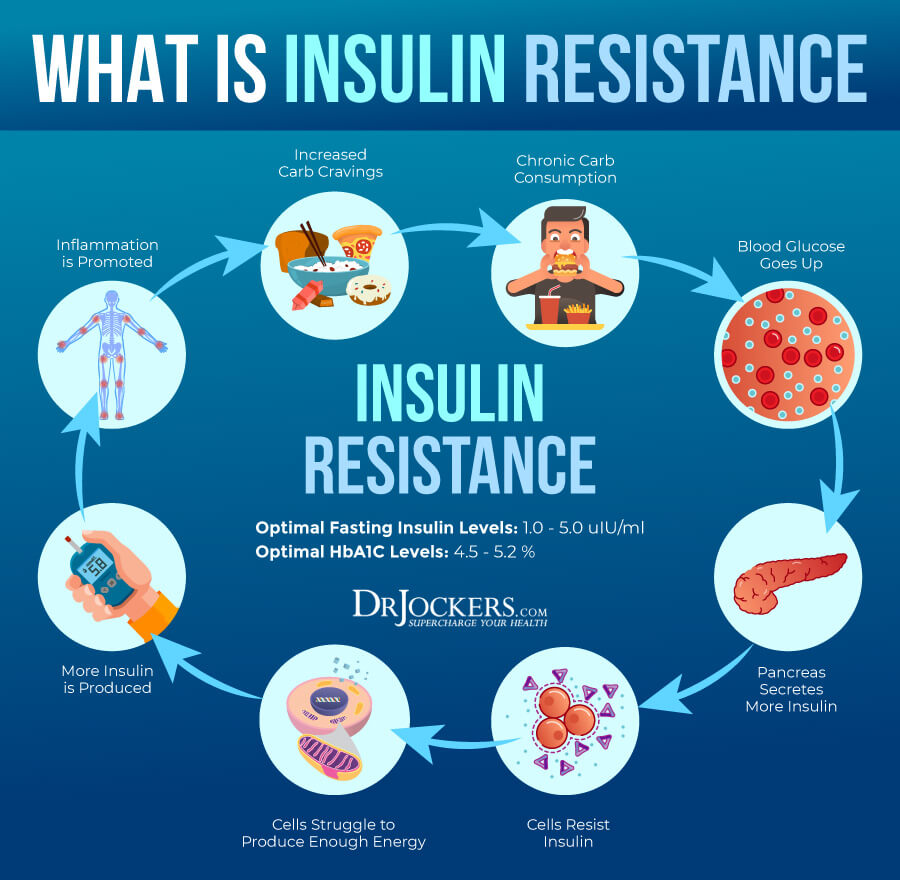
Blood Sugar Imbalances
Because blood sugar imbalances can increase inflammation in your body and trigger your symptoms of osteoarthritis. A 2018 review published in Autoimmune Reviews has found that following a conventional Western diet with too many inflammatory processed foods can increase insulin resistance and obesity and as a result also increase inflammation and contribute to joint inflammation (4).
A 2015 study published in Clinical Geriatric Medicine has found a link between diabetes and osteoarthritis (5). At 52 percent, they found a higher prevalence of osteoarthritis in those with type 2 diabetes than in those without it. The group without type 2 diabetes had only 27 percent of the prevalence of osteoarthritis. Researchers believe that hyperglycemia and poor lipid metabolism may contribute to the breakdown of cartilage and osteoarthritis.
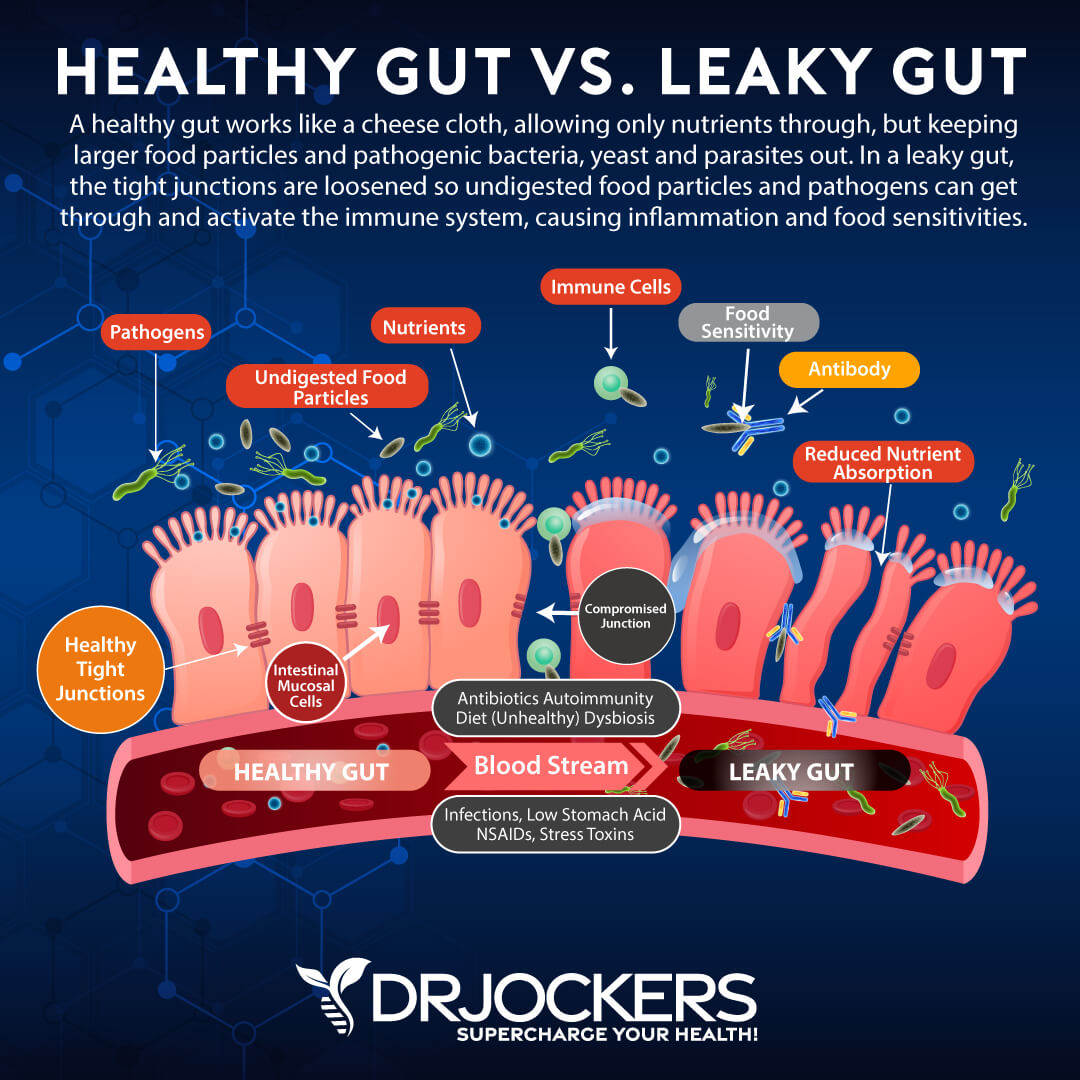
Dysbiosis & Leaky Gut Syndrome
Your gut health is one of the most important aspects of your health. If your gut microbiome is out of balance, sooner or later, it will affect other areas of your body, including your joints and bones. Gut dysbiosis means that your gut flora is out of balance and there are too many bad bacteria and other pathogens hanging out there and compromising your health.
Gut dysbiosis can become a serious issue. It increases your risk of leaky gut syndrome. In a healthy body, your gut lining has tiny openings to allow nutrients to pass into your bloodstream but stop pathogens. Leaky gut syndrome means that these holes become bigger. It is characterized by larger openings on your gut lining that allow toxins, bacteria, and large food particles to ‘leak ‘ or to get through into your bloodstream.
Both gut dysbiosis and leaky gut syndrome can increase inflammation throughout your body and may affect your joint health. A 2019 study published in Heliyon has found a correlation between gut dysbiosis and joint osteoarthritis (6).
Gut dysbiosis causes low-grade systemic inflammation that can increase the risk or symptoms of osteoarthritis, including pain, swelling, inflammation, and compromised movement. Addressing gut dysbiosis and leaky gut syndrome, recreating a gut microbiome homeostasis, and improving your gut health may reduce your symptoms and reduce your risk of osteoarthritis.
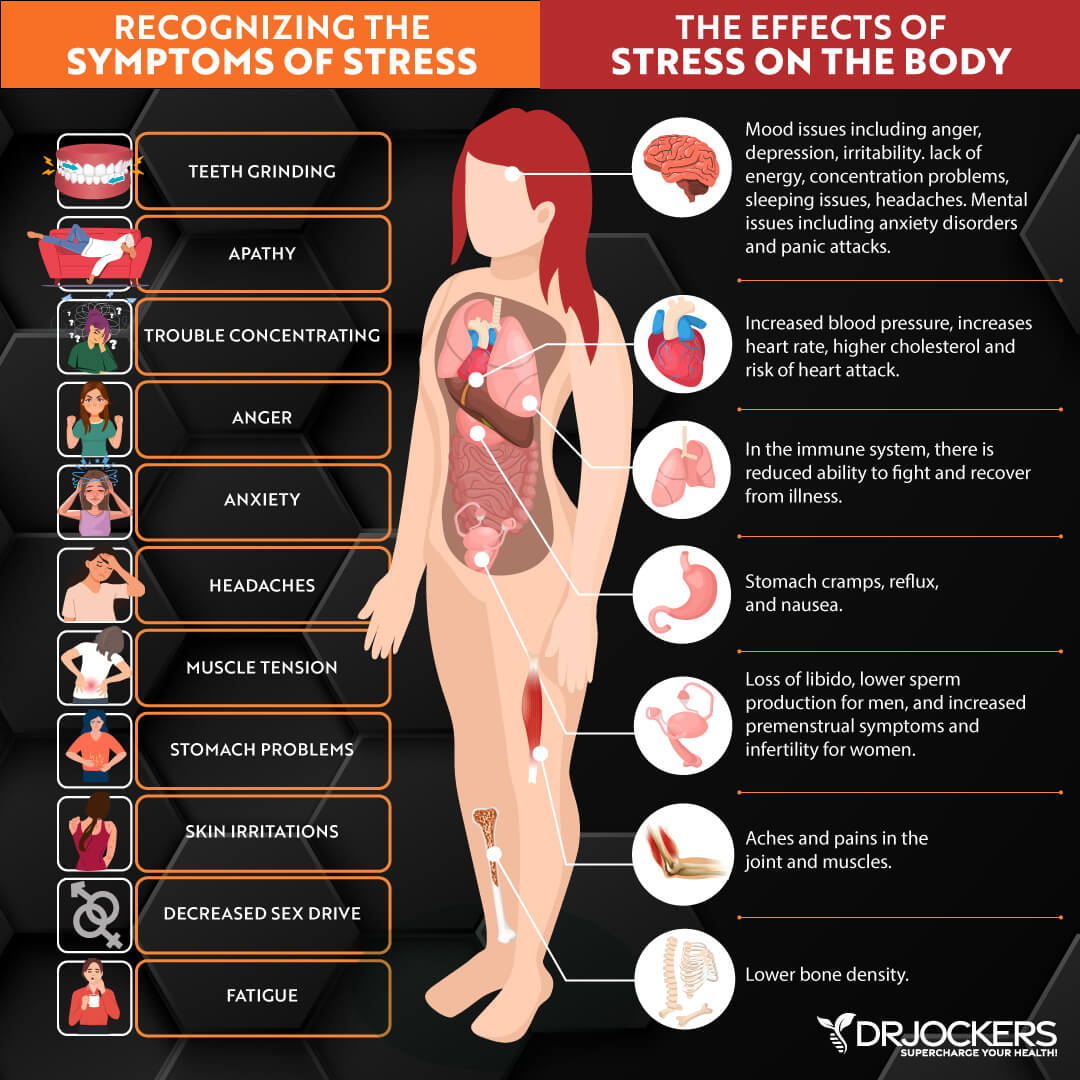
Chronic Stress & Poor Sleep Habits
Chronic stress and poor sleep are two major lifestyle factors that can increase inflammation and affect your health. Chronic stress, including emotional, mental, social, physical, and spiritual stress, can impact your immune system and set off an inflammatory response.
This inflammatory response can lead to the development or worsening symptoms of osteoarthritis. Chronic stress can result in poor sleep and insomnia. Poor sleep, on the other hand, can further aggravate chronic stress and its symptoms.
Joint inflammation, osteoarthritis, and pain can also increase your stress levels and make quality sleep more difficult contributing to the vicious cycle of stress, poor sleep, inflammation, pain, and other osteoarthritis symptoms.
The longer you are experiencing chronic stress, the more serious and destructive this chronic inflammation can become, and the worse your osteoarthritis symptoms may turn. A 2011 study published in PLoS One has found that stress management training can be beneficial for patients with joint inflammation and arthritis (7).
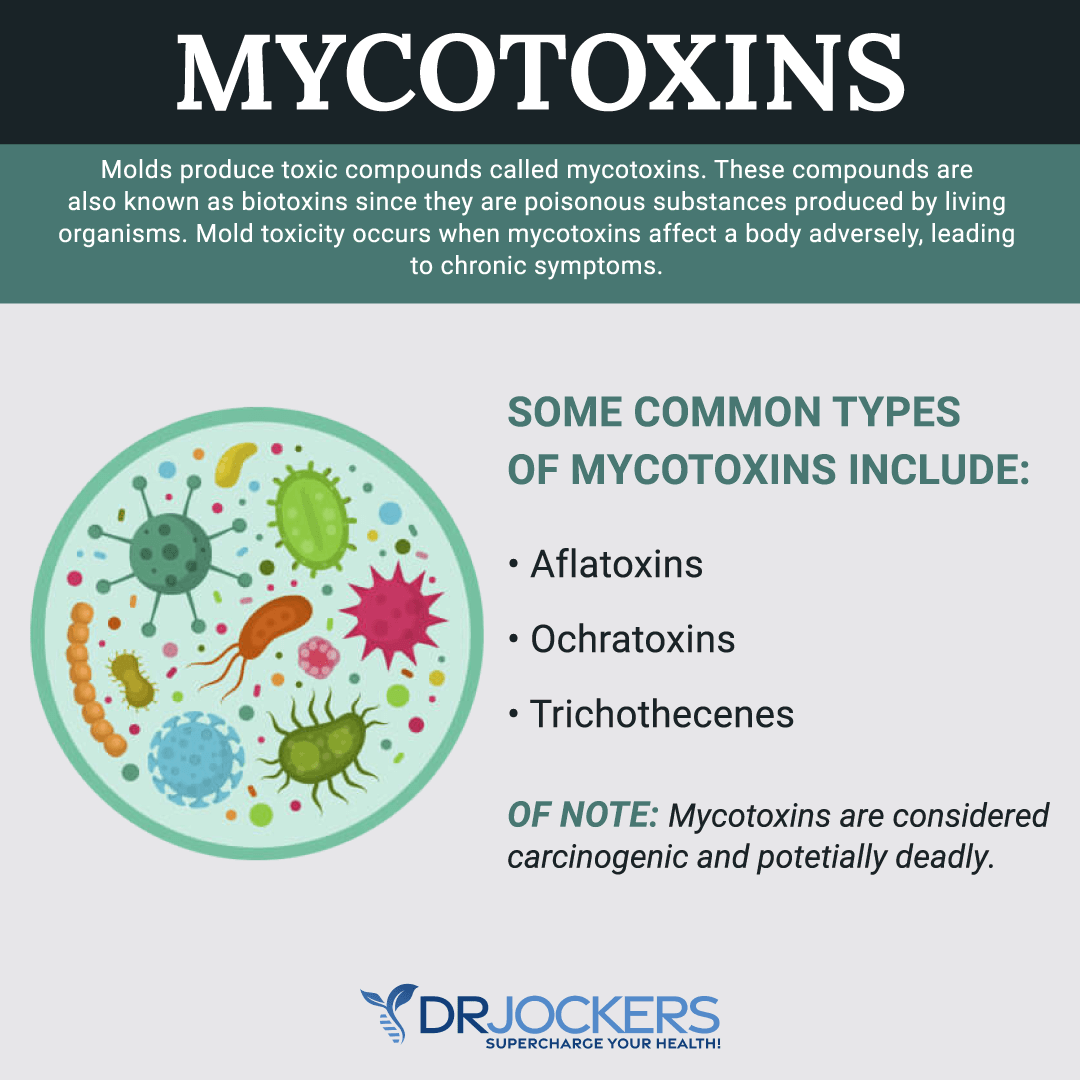
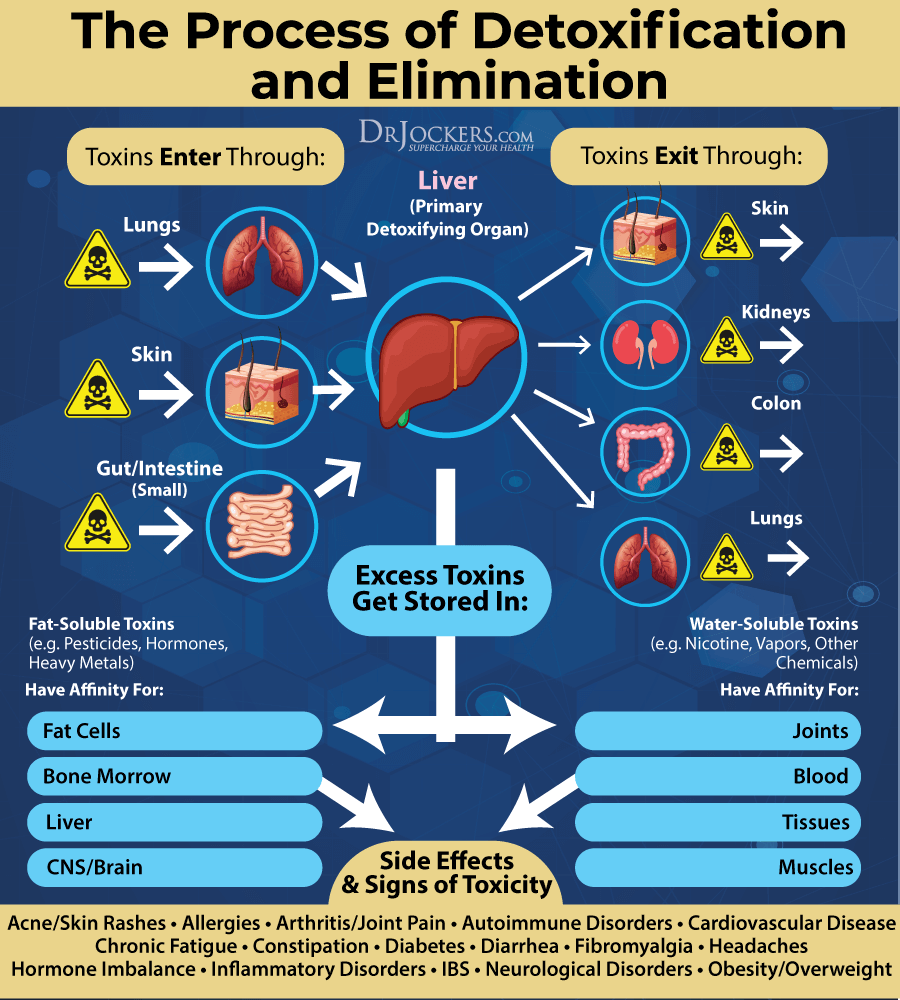
Environmental Toxin Exposure
Environmental toxins, including air pollution, tap water, mold, chemicals in conventional cleaning, body, and beauty products, plastic, and so on often go unnoticed or taken as a normal part of modern life, but they can have detrimental effects on your health.
They can increase inflammation in your body and potentially increase your risk of osteoarthritis. A 2003 study published in Clinical Rheumatology has found that mold and mycotoxins from moisture damage can trigger inflammation and joint-related symptoms (8).
Chronic Infections
Chronic infections, including oral infections, Lyme disease, and the Epstein-Barr Virus infection (EBV) can increase chronic inflammation, trigger joint inflammation, joint pain, and other musculoskeletal problems, and may increase osteoarthritis.
According to a 2013 study published in the Current Opinions in Rheumatology, has found that oral infections and periodontal diseases may be linked to rheumatoid arthritis (9). While it’s not clear if it’s the same with osteoarthritis, oral infections increase inflammation in your body that can trigger joint inflammation and worsen symptoms of osteoarthritis.
According to a 2011 study published in the Journal of American Academy of Orthopedic Surgery, joint inflammation and arthritis is a common orthopedic complication of chronic Lyme disease (10). A 2016 case report published in Rheumatology Clinical has found that EBV may contribute to inflammatory patterns, joint inflammation, and arthritis (11).
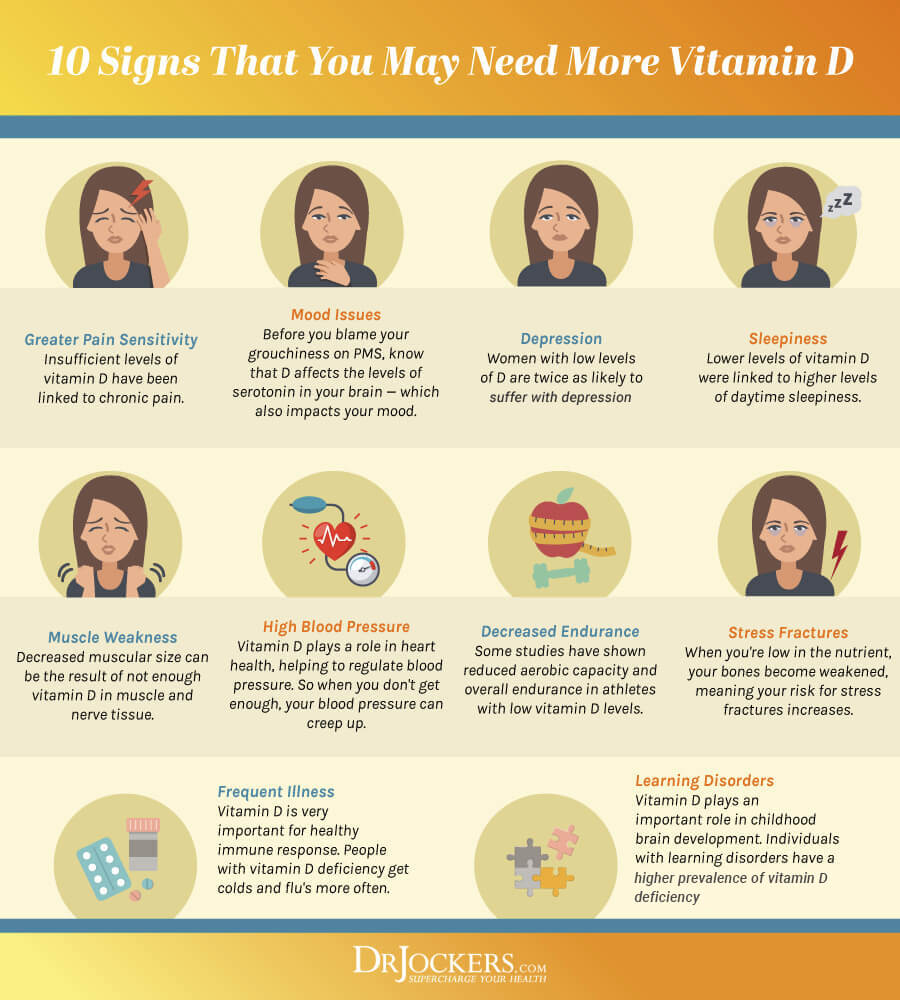
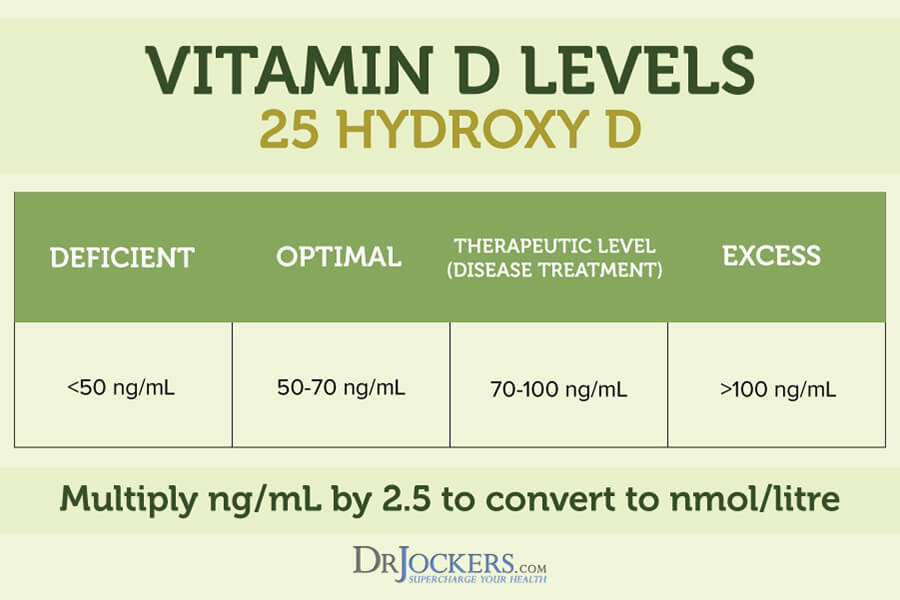
Vitamin D Deficiency
Vitamin D is a critical vitamin for a variety of health reasons, including for the health of your joints, muscles, and bones. Vitamin D deficiency is an incredibly common problem, yet it can weaken your bones that can lead to joint issues. It may also affect your immune system and increase overall inflammation, both of which can increase your risk of osteoarthritis and joint issues.
According to a 2017 study published in the Orthopedic Journal of Sports Medicine, low vitamin D levels have been associated with articular cartilage problems and osteoarthritis (12). A 2015 study, on the other hand, has found that taking vitamin D may help to prevent articular cartilage erosion and osteoarthritis (13).
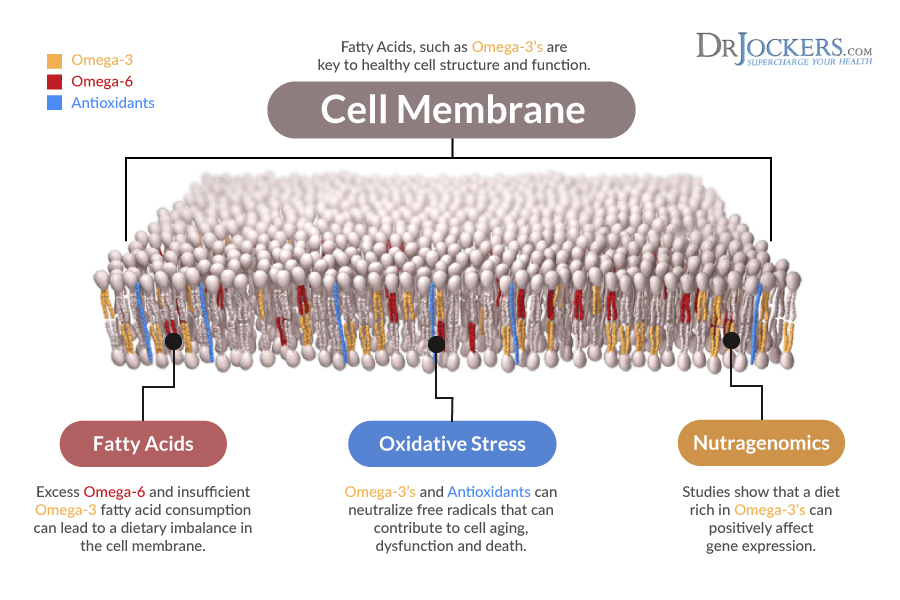
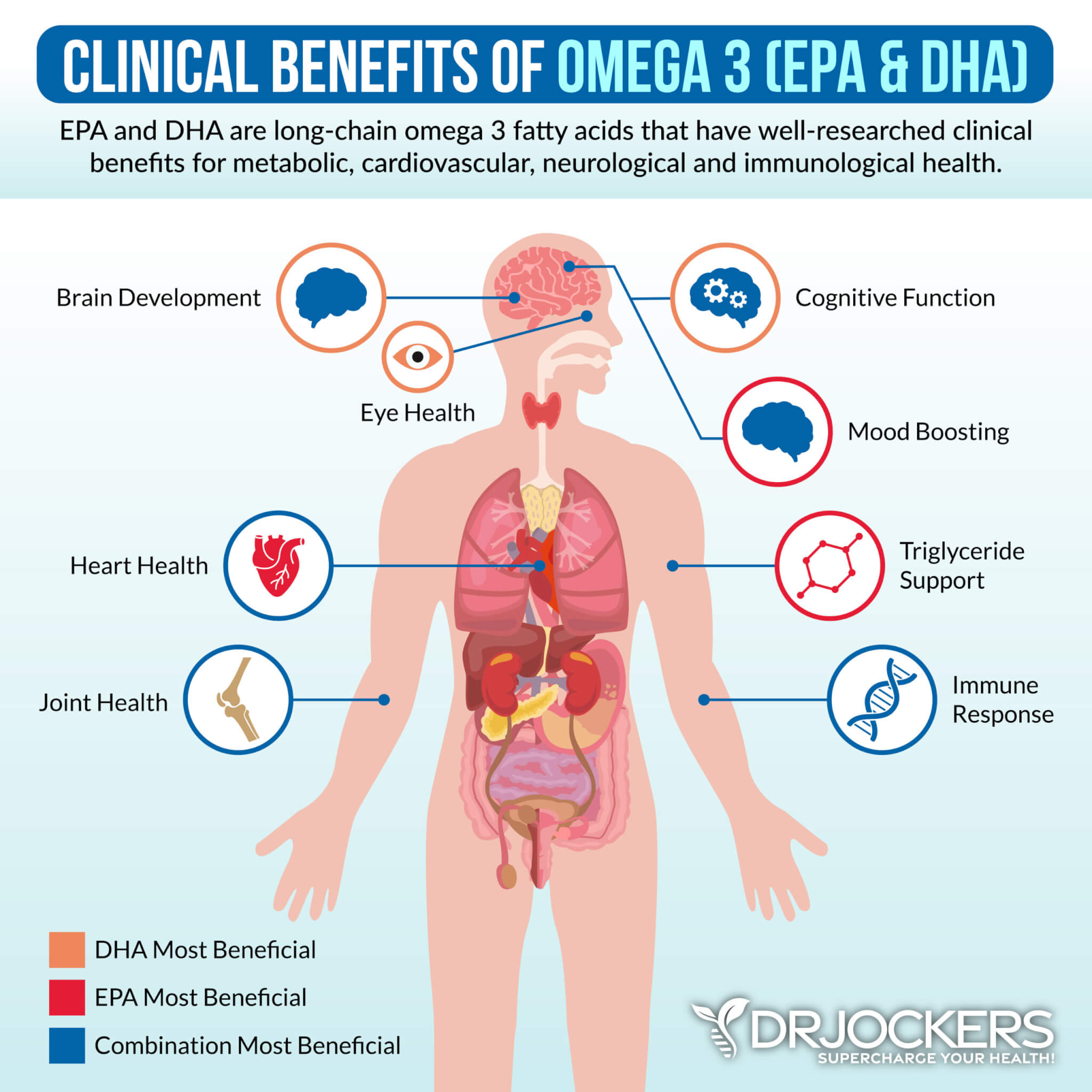
High Omega 6:3 Ratio
Fats often get a bad rap. However, fats are incredibly important for your health. However, what kind of fats you eat and in what ratio matters. Omega-3 and omega-6 fatty acids are polyunsaturated fatty acids that have many (poly) double bonds.
Omega-3 fatty acids have anti-inflammatory while omega-6 fatty acids have pro-inflammatory effects on your body. Let’s be clear, your body needs both of them for health and well-being. Inflammation protects you from injuries and infections and is necessary for your survival. However, inflammation becomes a problem when it turns into chronic inflammation.
Having a high omega 6:3 ratio with too much omega-6s is a problem and can lead to chronic inflammation. The healthy ratio should be between 1:1 and 4:1. The problem is that most people have a much higher ratio and increased chronic inflammation.
A 2018 study published in the Clinical Journal of Pain has found that high omega 6:3 ratios have been associated with inflammation, pain, and function issues in the knee joints (14). On the other hand, according to a 2018 study published in Open Heart, a low omega 4:3 ratio can help to reduce inflammation, hence it may help to reduce inflammation and symptoms related to osteoarthritis (15).
Natural Support Strategies
Aging is inevitable, osteoarthritis is not. Your body doesn’t have to develop osteoarthritis and if you already have osteoarthritis, your condition doesn’t have to worsen and your symptoms don’t have to become debilitation. With the help of some simple natural support strategies, you may improve your joint health. Here is what I recommend:
Anti-Inflammatory Nutrition Plan
Studies, including a 2016 study published in Nutrition & Diabetes and a 2018 study published in Rheumatology have found that eating an inflammatory diet can contribute to the development and symptoms of osteoarthritis while eating an anti-inflammatory and nutrient-rich diet can help (3, 4). I recommend that you follow an anti-inflammatory nutrition plan for your joint health.
Eliminate all refined sugar, refined oil, conventional and processed meat and dairy, artificial ingredients, processed foods, and junk food. Eat a diet rich in anti-inflammatory foods, including greens, vegetables, mushrooms, low glycemic index fruits, herbs, spices, sprouts, nuts, seeds, grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game.
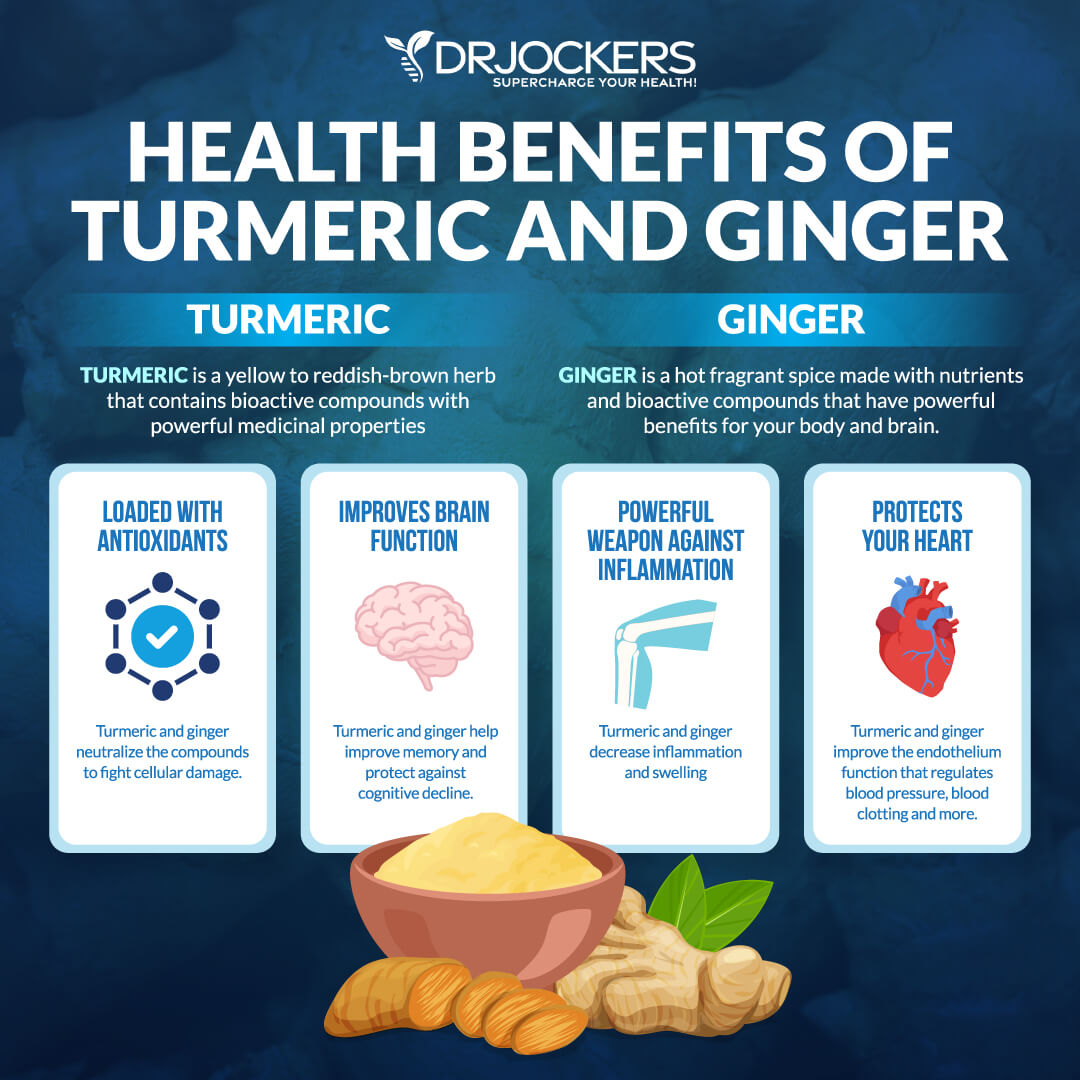
Make sure that you eat plenty of anti-inflammatory herbs, including ginger and turmeric, and omega-3-rich foods, such as fish, seafood, flax seeds, chia seeds, and hemp seeds. Also look to get a lot of healthy fats from avocados, olives, olive oil and coconut oil.
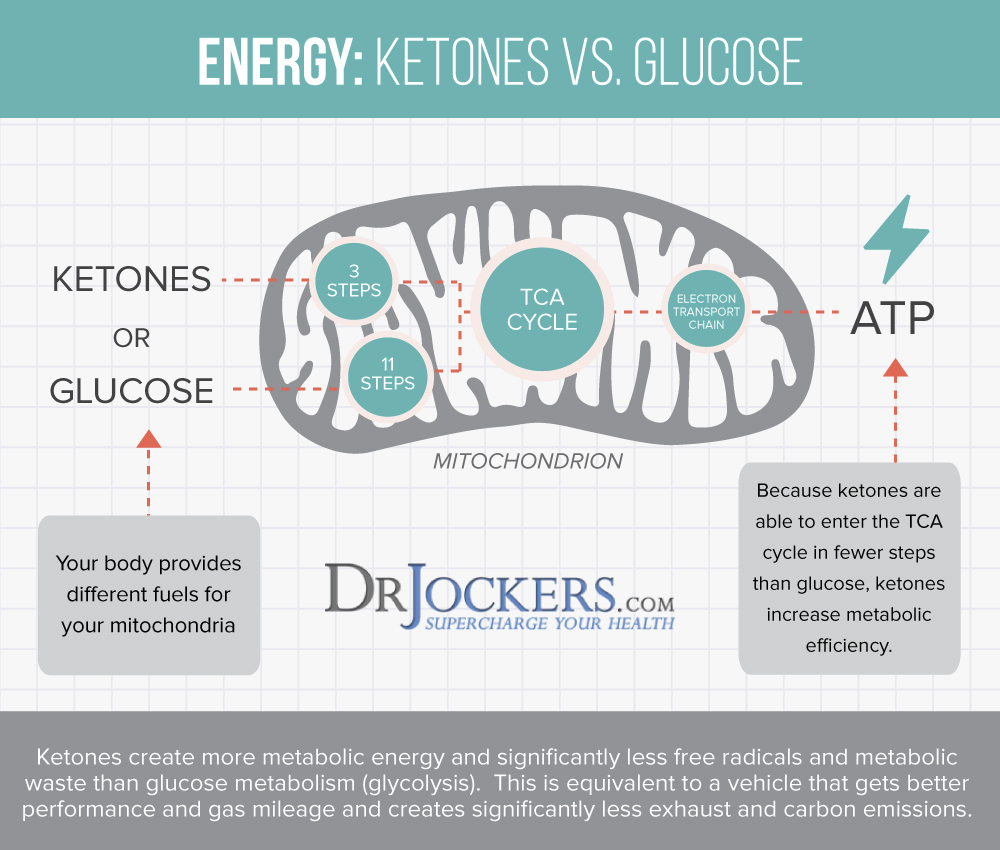
Consider Getting into Ketosis
Getting into ketosis is a smart way to reduce inflammation and improve your joint health. Under regular circumstances, your body relies on glucose (sugar) for energy. Eating a low-carb ketogenic diet, fasting, or being deprived of glucose or food otherwise means that your body will be deprived of dietary glucose and have to start using fat for energy instead. Through this process, your body experiences ketosis and becomes fat-adapted, which means that it also becomes much more efficient than when relying on glucose.
A 2020 study published in Pain Medicine has found that eating a low carbohydrate diet, such as a ketogenic diet, can reduce pain in people with knee joint inflammation (16). Ketosis offers similar health benefits as intermittent fasting, including cellular autophagy, reduced inflammation, improved blood sugar levels, and reduced risk of chronic disease.
It’s not surprising that the top two ways to achieve ketosis are fasting and a ketogenic diet. I recommend that you combine a ketogenic diet with intermittent fasting for optimal joint and health benefits. Here is a helpful article on how to follow a real food keto diet.
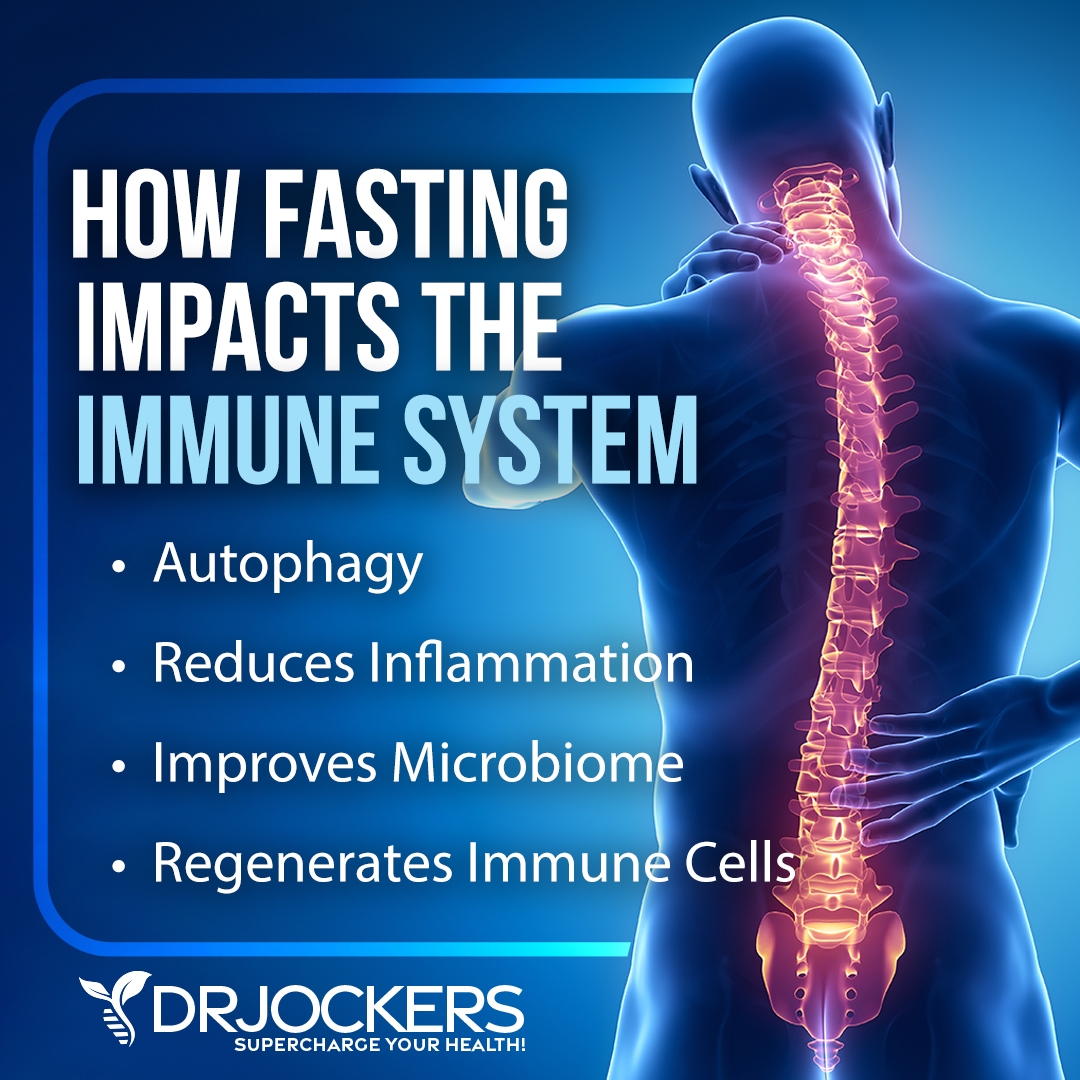
Intermittent Fasting
Intermittent fasting is a great way to achieve ketosis and support your health. It is a way of eating when you are cycling between periods of fasting or feasting within one day. It has similar benefits to a ketogenic diet and may help to reduce inflammation, pain, insulin resistance, and the risk of chronic disease. According to a 2019 study published in Nutrients, intermittent fasting during Ramadan had a positive impact on joint inflammation (17).
If you are new to intermittent fasting or any fasting, I recommend starting with a Simple Fast of 12 hours of fasting, including your overnight sleep. For example, if you eat dinner at 6 pm, stop eating after 12 hours, and you will be ready to eat again at 6 am the next day. I recommend that you increase your fasting period gradually.
After a week, you may want to extend your fasting window to 14 hours and eventually to 16 hours. You will notice that delaying breakfast until 7 am, 8 am, or even 10 am will come naturally to you over time. Most people feel the best with 16 hours of fasting a day, however, it’s important that you listen to your body and do what offers the most benefits to you.
Reduce Stress & Prioritize Good Sleep
Stress and poor sleep can contribute to chronic inflammation and symptoms of osteoarthritis, while a 2011 study published in PLoS One has found that stress management training can be helpful for those with arthritis (7). To reduce chronic stress, I recommend a variety of stress reduction practices, including meditation, breathwork, guided visualization, muscle relaxation strategies, gratitude, journaling and prayer.
I recommend that you spend plenty of time in nature, engage in uplifting activities, try new hobbies that make you happy and calm. Seek out a supportive community, spend time with friends and family that lift you up, and make sure to have some dedicated me-time as well. Laugh and smile more.
Prioritize good sleep by making sure that you sleep 7 to 9 hours a night. Develop a relaxing bedtime routine and follow a regular sleep schedule that supports your body’s circadian rhythms. Avoid electronics, food, caffeine, alcohol, and stress close to bedtime, but engage in relaxing activities.
Along with my stress reduction strategies I mentioned earlier, reading, crossword puzzles, board games, coloring, healing baths, listening to calming music, loving conversation, and sipping on herbal tea may be helpful ideas. Make sure that your bedroom is a safe sanctuary with a supportive bed and comfortable bedding and pillows.

Regular Movement & Exercise
Living a sedentary lifestyle can contribute to chronic stress and chronic inflammation, which can lead to or aggravate osteoarthritis. (7). I recommend that you stay active throughout the day and exercise regularly. Start your day with some movement, such as stretching, a few yoga moves, a short walk outside, or a trampoline session.
Stay active throughout the day as much as you can by getting up from your desk regularly to stretch out or move, taking the stairs instead of the elevation, going for a walk during lunch, walking or biking instead of driving short distances, playing with your kids or pets, or having a dance session in your living room.
Make sure to listen to your body and not overdo it. If you are at later stages of osteoarthritis, you may have to opt for low impact and joint-friendly workouts only and make strength-training a priority. A 2013 study published in Osteoarthritis Cartilage has found that poor biomechanics can contribute to poor biomechanics (2). Improving your biomechanics, using the right form, and strengthening your body is important, and working with a physical therapist or trainer well-versed in osteoarthritis and joint health may be a helpful idea.

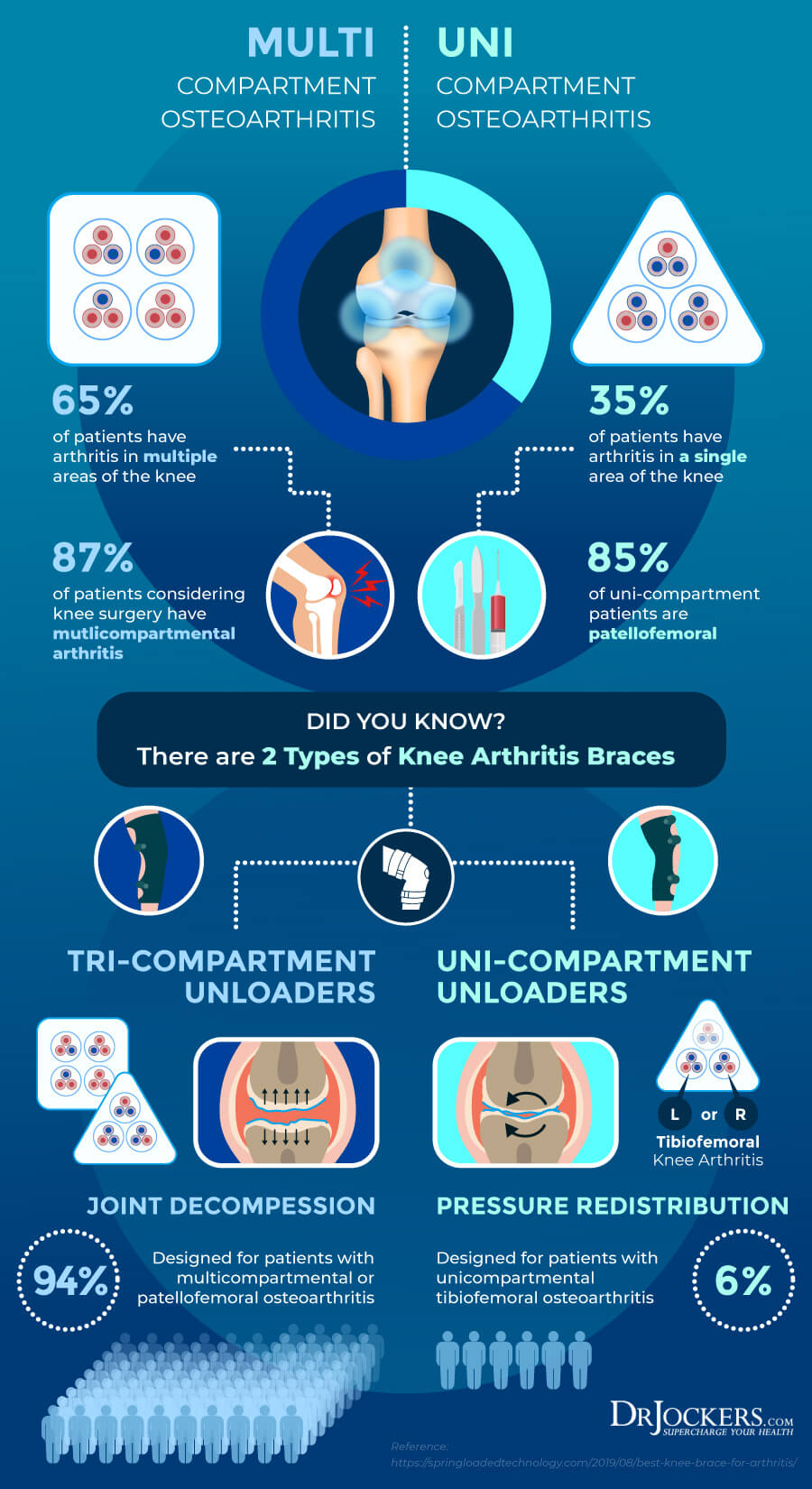
Wearing Braces to Support Inflamed Joints
Wearing braces to support inflamed joints is often recommended as non-surgical treatment option for osteoarthritis. The benefits of braces have been shown by various studies, including a 2016 observational study published in the International Journal of Rheumatic Diseases (33).
Braces can help to enhance stability by shifting the weight away from the inflamed areas to reduce pain. They help to lower swelling through compression and reducing pressure and discomfort. The extra support provided by braces may also increase your confidence in completing daily tasks and becoming more active again.
Depending on the affected area, the severity of your symptoms, and personal preference, your doctor will recommend a brace that’s right for you. Braces may be made of plastic, metal, or other hard materials, or synthetic rubber, foam, or other soft materials depending on your needs.
Different braces have different functions. Prophylactic braces can protect athletes and active individuals from injury. Functional or supportive braces help with existing injuries. Rehabilitative braces help to heal by limiting movement. Unloaders or offloaders reduce pressure and are the most common braces for those with osteoarthritis.
You can get braces to protect just about any joint or body part, including braces for your ankles, back, knees, shoulders, and wrists with a variety of options for each joint. An unloader knee brace can help to reduce pressure and keep your knee from wobbling. A hinged knee brace offers stability and helps with movement.
A drop-lock hinged knee brace can help after surgery or an injury. While you can find braces at medical supply stores, pharmacies, and online, it is usually best to seek recommendations from an orthopedic doctor or physical therapist and get custom made braces if possible or necessary.
Heal Your Gut & Improve Your Microbiome
Your gut and microbiome health can have a serious impact on joint health. According to a 2019 study published in Heliyon, there is a link between gut dysbiosis, chronic inflammation, and osteoarthritis (6). Healing your gut and improving your microbiome is an essential step for joint health. I recommend that you support your microbiome by eating plenty of prebiotic- and probiotic-rich foods, taking daily probiotics.
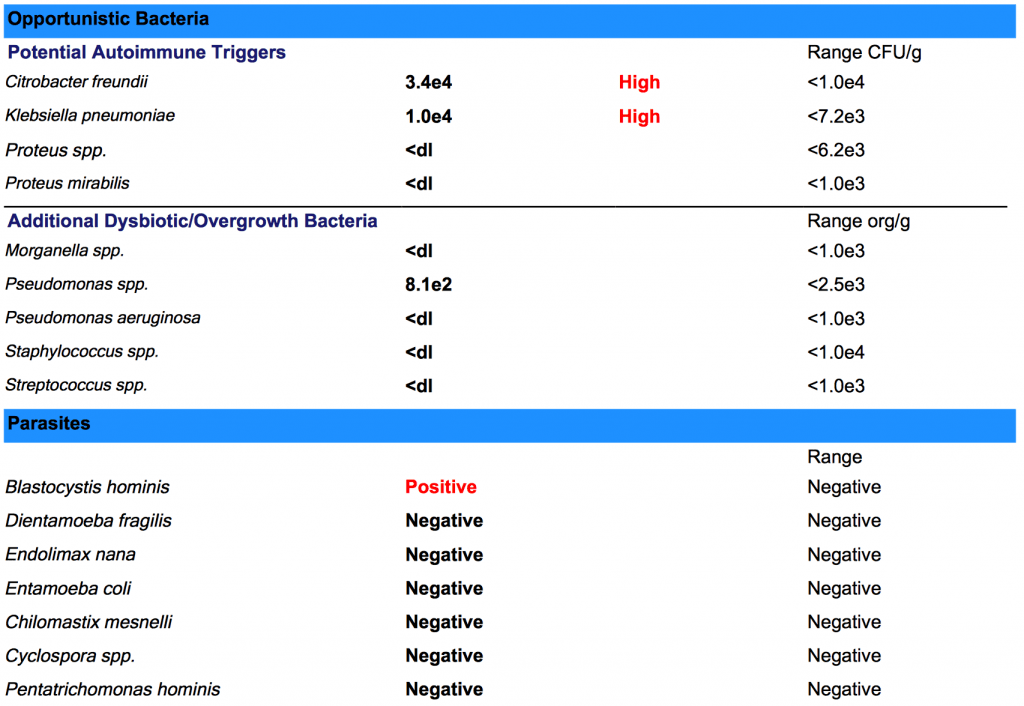
Take digestive enzyme supplements before meals to improve your digestion. If you are dealing with any chronic gut infections or other chronic infections, talk to a functional health doctor, like me, to help you address them through appropriate herbal supplementation and diet. Testing for gut infections and microbiome imbalances using a lab such as the GI MAP may be a helpful idea to identify the root cause of your health issues and develop an effective treatment plan.
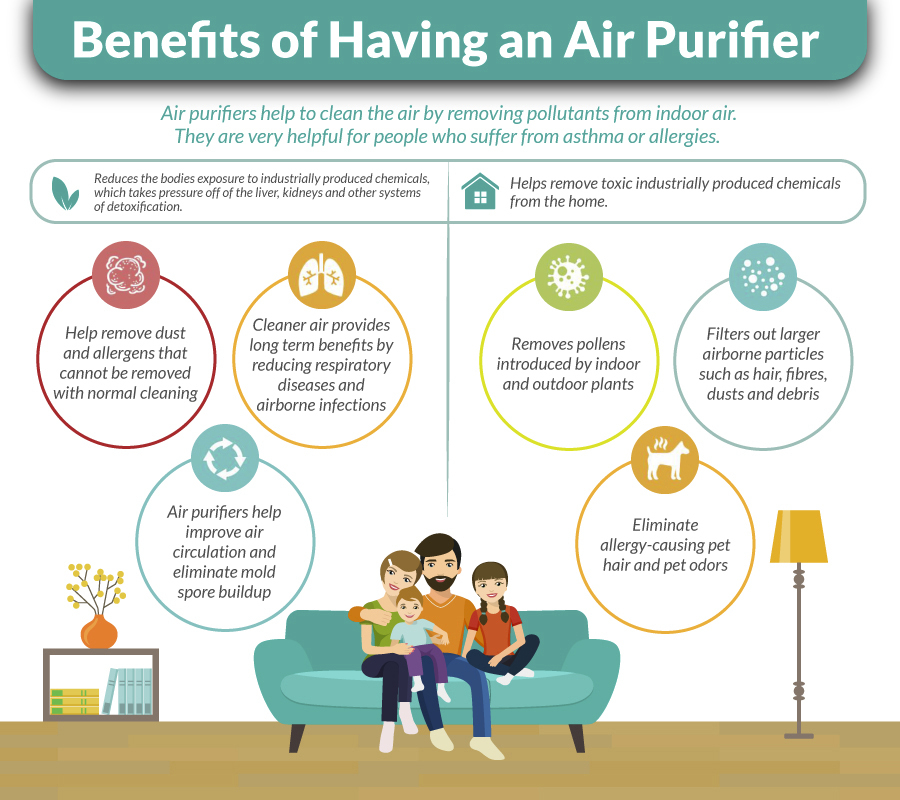
Improve Air & Water Quality
Environmental toxins can lead to inflammation and increase your symptoms of osteoarthritis. For example, according to a 2003 study published in Clinical Rheumatology, mold exposure may trigger joint-related symptoms (8). Reducing toxins from your air and water is critical.
Having a high-quality air filtration system can help to remove mold, allergens, microbes, and toxins from your air and improve your indoor air quality. A high-quality water purification and filtration system can help to remove toxins and chemicals from your tap water making sure that you have safe drinking water. Reduce or eliminate the use of plastics and opt for glasses, mason jars, ceramic mugs, glass bottles, and stainless-steel bottles instead.
Open up Detoxification Pathways
Environmental toxins can make symptoms of osteoarthritis worse (8). Opening up and improving your detoxification pathways is an important strategy to reduce inflammation and symptoms. Improve your body’s ability to detoxify through urine by drinking plenty of water. Increase detoxification through the skin and sweating by exercising and using infrared sauna therapy regularly.
Try bioactive carbons such as fulvic and humic acids and activated charcoal to help pull out toxins from your body to be eliminated through bowel movements. If you don’t have regular bowel movements, you may try some herbal intestinal mover supplements with aloe vera, ginger, cascara sagrada bark, black walnut hulls, garlic, fennel seed, cayenne, wormwood, senna seed, and barberry root that support digestion and healthy bowel movements. Support lymphatic health and detoxification through daily dry brushing and rebounding.
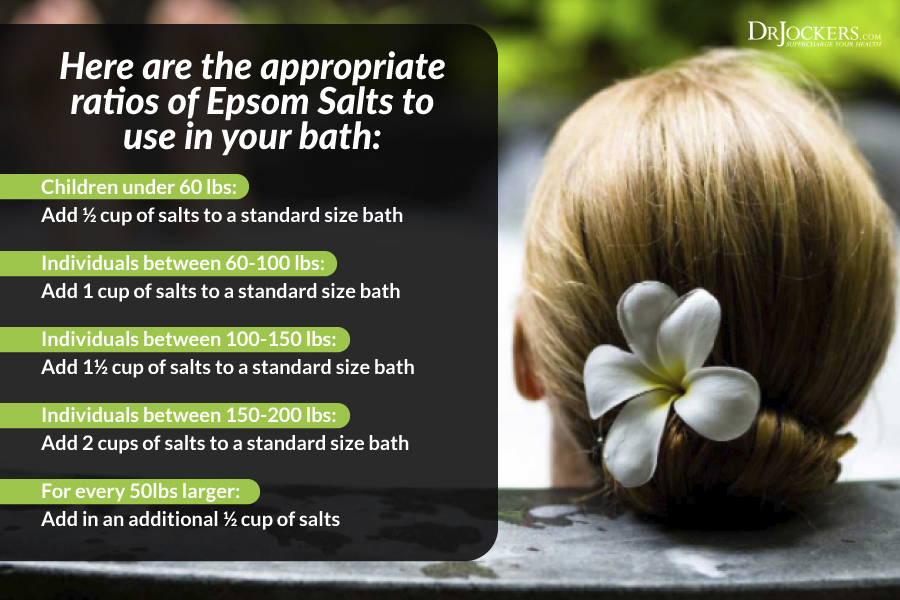
Do Epsom Salt Baths
Taking regular Epsom salt baths can also support your detoxification pathways to reduce symptoms from toxicity (8). Epsom salt baths are also used to reduce muscle tension and pain in the joints.
I recommend setting aside 40 minutes for an Epsom salt bath since it takes about 20 minutes to pull out toxins and 20 minutes to absorb the minerals in the water. Just simply mix Epsom salts with your bath water using the following guidelines then relax with a good book or music or just your thoughts:
- Children under 60 lbs: Add ½ cup of salts to a standard size bath.
- Individuals between 60-100 lbs: Add 1 cup of salts to a standard size bath.
- Individuals between 100-150 lbs: Add 1½ cup of salts to a standard size bath.
- Individuals between 150-200 lbs: Add 2 cups of salts to a standard size bath.
- For every 50lbs larger: Add in an additional ½ cup of salts.
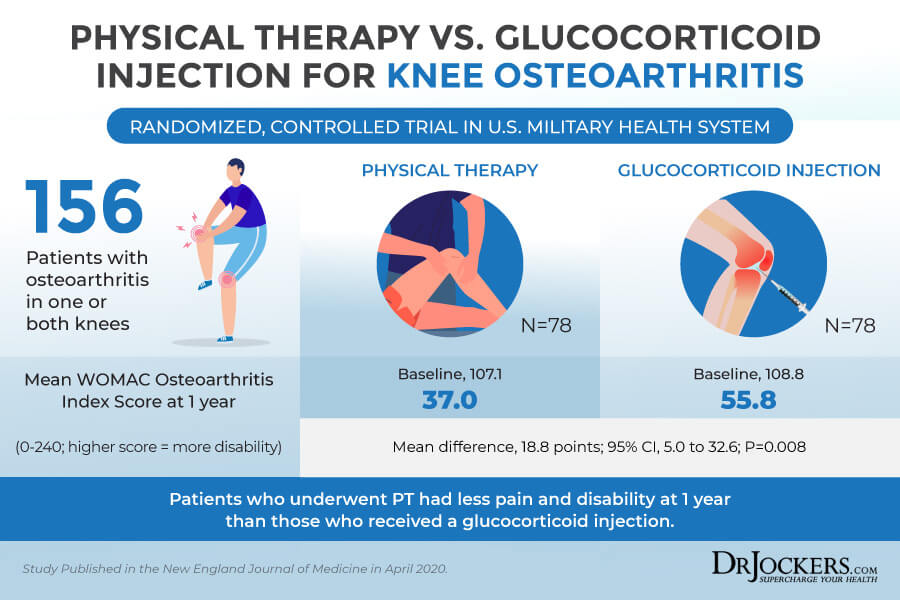
Consider Chiropractic, Massage & Physical Therapy
As you know from a 2013 study published in Osteoarthritis Cartilage I mentioned earlier, poor biomechanics and injuries can contribute to joint issues and the development of osteoarthritis (2). Chiropractic, massage, and physical therapy may all play a role in improving your symptoms and your joint health. These therapies offer different benefits and can work hand in hand.
A chiropractor is a bodywork therapist who works with your spine and joints and can help to relieve joint pain and help to move your back into alignment. A massage therapist works with your muscles directly and can help to release muscle tension that may contribute to or develop because of joint inflammation. Massage therapy can also reduce stress and tension that may contribute to inflammation and increase symptoms.
A physical therapist can help to improve your biomechanics through exercise and strengthening strategies. They can teach you strategies on how to strengthen your body, have a better posture, and use a proper form when exercising or moving. Physical therapy can help you to keep the benefits you receive from chiropractic work and massage therapy long-term. Physical therapy can also reduce the risk of injuries. A 2020 study in the New England Journal of Medicine showed that patients with osteoarthritis in one or both knees who went through physical therapy had significantly less pain and disability than those who got a steroid shot for pain relief.
Optimize Vitamin D Levels
Vitamin D deficiency may not only play a role in osteoarthritis, but a 2017 study published in the International Journal of Molecular Sciences has found that vitamin D can play an important role in reducing inflammation and pain management (12, 13, 18). A 2015 study published in Pain Therapy has also found that vitamin D supplementation may lower chronic pain which is a common characteristic of osteoarthritis (19).
Optimal levels of vitamin D should be between 50 and 100 ng/ml. Spending time outside in the sun and eating vitamin D-rich foods such as oily fish, liver, and egg yolk is important to increase your vitamin D levels, however, sunshine and food are usually not enough for optimal vitamin D levels. I recommend taking a daily vitamin D supplement with vitamin K2 to improve absorption.
Use Omega 3 Fatty Acids
You’ve learned from a 2018 study published in the Clinical Journal of Pain and a 2018 study published in Open Heart that good omega 3 and 6 ratio is critical for reducing joint inflammation (14, 15). A 2007 meta-analysis published in Pain has found that only 3 to 4 months of supplementation with omega-3 fatty acids can help to reduce inflammatory joint pain (20).
According to a 2020 study published in the Mediterranean Journal of Rheumatology, omega-3 fatty acids can benefit autoimmune joint inflammation (21). I recommend that you eat plenty of omega-3 rich foods, including fish, seafood, walnuts, flax seeds, chia seeds, and hemp seeds. Additionally, I recommend supplementing with a high-quality omega-3 fish oil supplement on a daily basis.
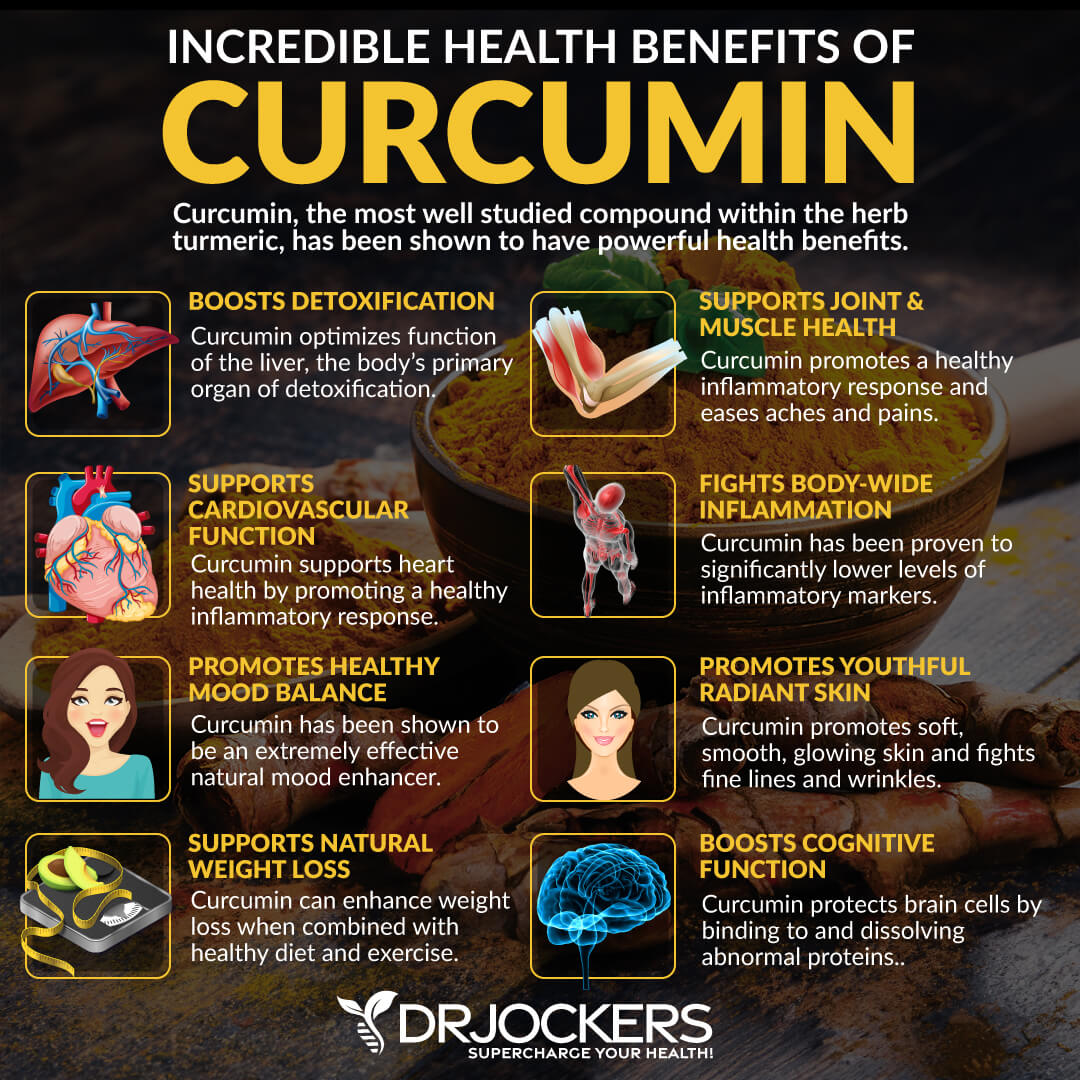
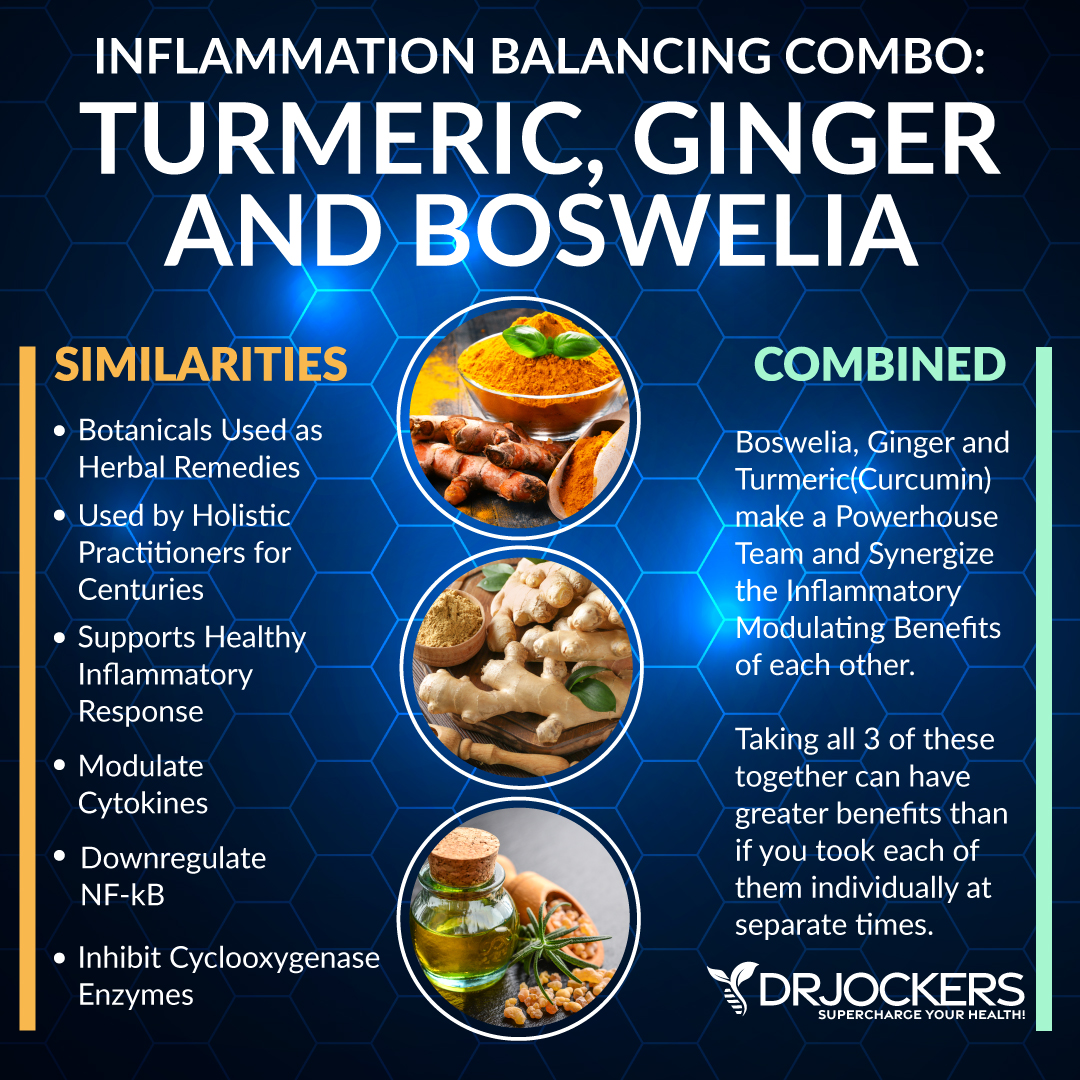
Use Anti-Inflammatory Herbs
Along with an anti-inflammatory diet and lifestyle, I recommend using anti-inflammatory herbs, such as turmeric, ginger, and boswellia to improve your joint health. You may use turmeric and ginger in your cooking, smoothies, juices, dressings, and teas; however, I recommend that you use these herbs in the form of supplements as well.
You may find individual supplements for each, however, there are inflammation defense supplements that include all three for optimal benefits and convenience.
Turmeric (Curcumin)
Curcumin is the active ingredient of one of the most researched anti-inflammatory herbs, turmeric. A 2016 systematic review and meta-analysis of randomized clinical trials published in the Journal of Medicinal Foods has found that turmeric extracts and curcumin may reduce the symptoms of joint inflammation and osteoarthritis (22).
A 2016 review published in Drug Design, Development, and Therapy has also found that curcumin has anti-inflammatory benefits for joint inflammation (23).
Ginger
Ginger offers similar health benefits to turmeric, which is not surprising since this anti-inflammatory herb is similar to and comes from the same family as turmeric. According to a 2001 study published in Arthritis Rheumatology, ginger extract has shown positive benefits for knee joint pain in osteoarthritis patients (24).
A 2015 systematic review published in Nutrition Journal has also found that ginger has anti-inflammatory benefits that may benefit osteoarthritis (25). Moreover, according to a 2013 comparative study published in the International Journal of Rheumatic Disease, using ginger and turmeric together have combined anti-inflammatory benefits for joint inflammation (26).
Boswellia
Boswellia is a plant that produces Indian frankincense and offers anti-inflammatory benefits and may be helpful for osteoarthritis symptoms. A 2019 randomized, double-blind, placebo-controlled pilot trial published in Phytotherapy Research has found that boswellia extract can be beneficial in the management of osteoarthritis in the knee (27).
A 2020 systematic review and meta-analysis published in BMC Complementary Medicine and Therapies, has also found that boswellia may be beneficial for joint pain and inflammation in osteoarthritis (28).
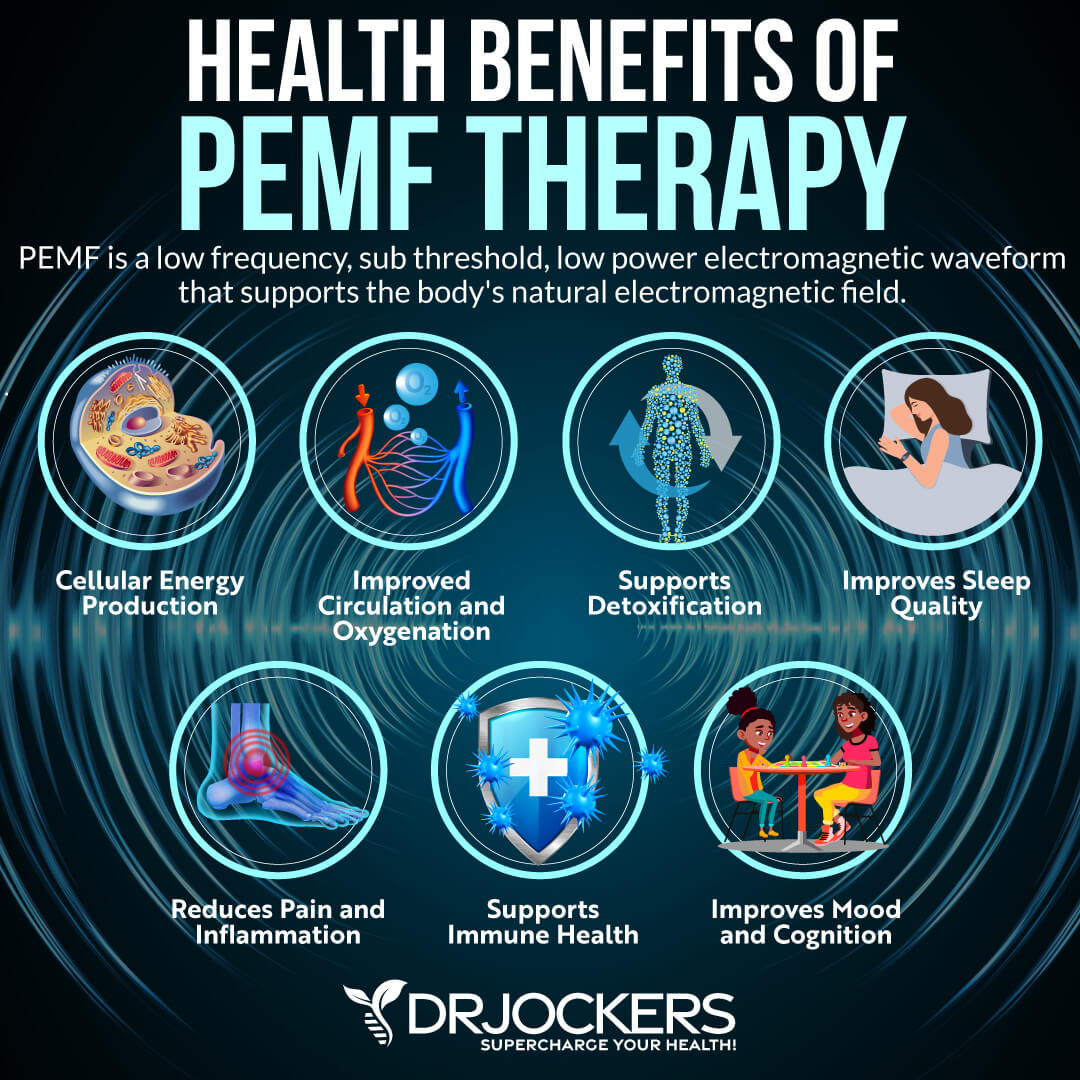
Consider Using PEMF Therapy
Pulsed electromagnetic field or PEMF therapy has been described and used dating back to thousands of years. PEMF is basically a battery charger for your body. A healthy cell in your body is at about -20 to -25 millivolts voltage and below -15 they start to get dysfunctional and can’t bounce back.
PEMF therapy introduces a mild electrical current into your damaged cells to increase blood flow, release inflammation, reduce pain, improve cellular and tissue healing, re-establish healthy cell interaction, and increase energy.
A 2013 study published in the Clinical Interventions in Aging has found that PEMF therapy may improve pain, stiffness, and pain in elderly with osteoarthritis (29). A 2018 meta-analysis published in BMJ Journals has also found that PEMF therapy may be beneficial for osteoarthritis (30).
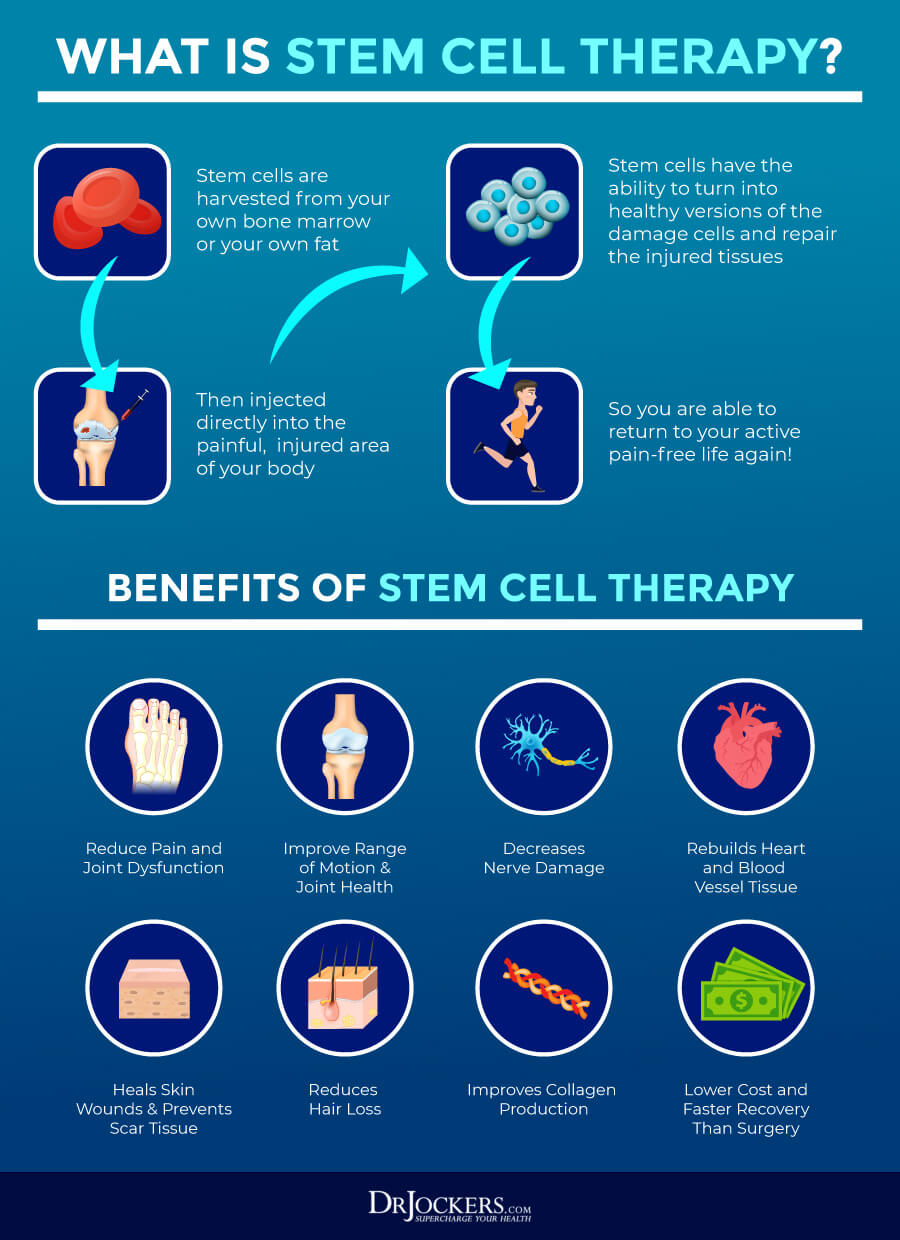
Consider Stem Cell Therapy
Stem cells are cells in your body that unlike other cells, don’t have a specific purpose or function. They are undifferential cells or raw materials. They have the ability to turn into any cell with specialized function as they need, including blood cells, brain cells, muscle cells, and bone cells.
They can divide into new stem-cells through self-renewal or other specialized cells through differentiation. Both self-renewal and differentiation can occur inside your body or in a science lab provided the right conditions.
The benefits of stem cells and stem cell therapy has been long studied. According to a 2018 systematic review published in Osteoarthritis Cartilage, stem cell therapy may be beneficial for osteoarthritis, however, more evidence and long-term follow-ups are needed (31).
Another 2018 comprehensive review published in Pain Physician has found that though the evidence is limited and more studies are needed, stem cell therapy may be beneficial for the treatment of knee osteoarthritis (32). You may learn about stem cells and stem cell therapy and many of the other natural support strategies in more detail by searching my website.
Final Thoughts
Osteoarthritis is the most common form of arthritis that affects about 32.5 million people in the United States. Osteoarthritis or degenerative joint disease is characterized by the breakdown of your joints, cartilage, and bones that may cause pain, swelling, inflammation, and loss of movement.
You don’t have to experience the often-debilitating symptoms of osteoarthritis. You can improve your joint health naturally. Try my simple natural support strategies, including diet and lifestyle changes and appropriate supplementation to support your joints, improve your health, and regain your vitality.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!




Do you have any knowledge of anyone who has reversed stage 4 osteoarthritis?