How to Properly Test Thyroid Function
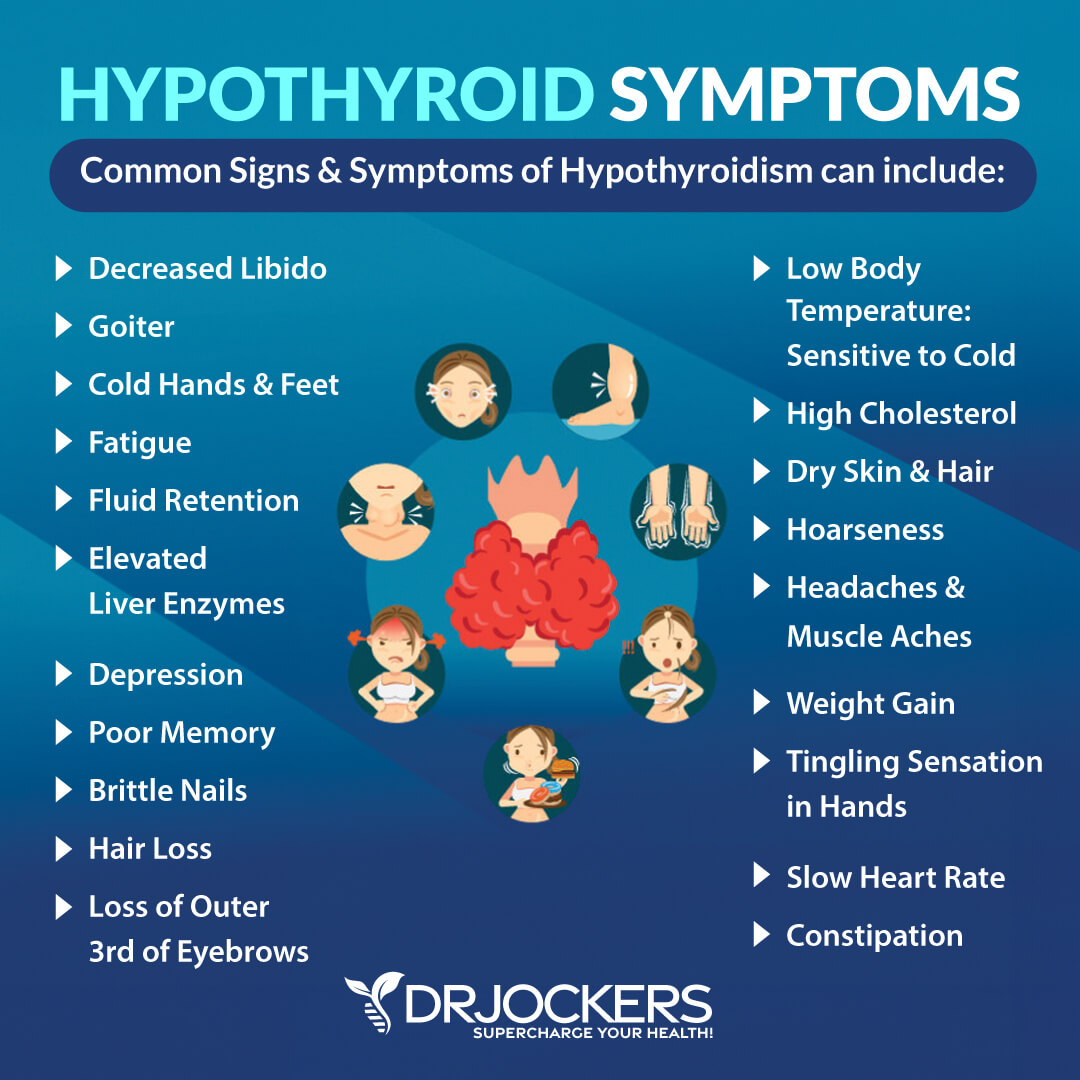
If you are not feeling your best it would be wise to test thyroid function. Hypothyroidism is one of the fastest growing health conditions we are seeing today. Lethargy, depression and weight gain are the most common symptoms (1).
It has been estimated that 27 million people in America struggle with some form of thyroid disease and up to 80 percent of hypothyroidism cases are autoimmune based (2). However, mainstream healthcare is not even testing for autoimmune indicators the majority of the time. This article will go through how to properly test thyroid function.
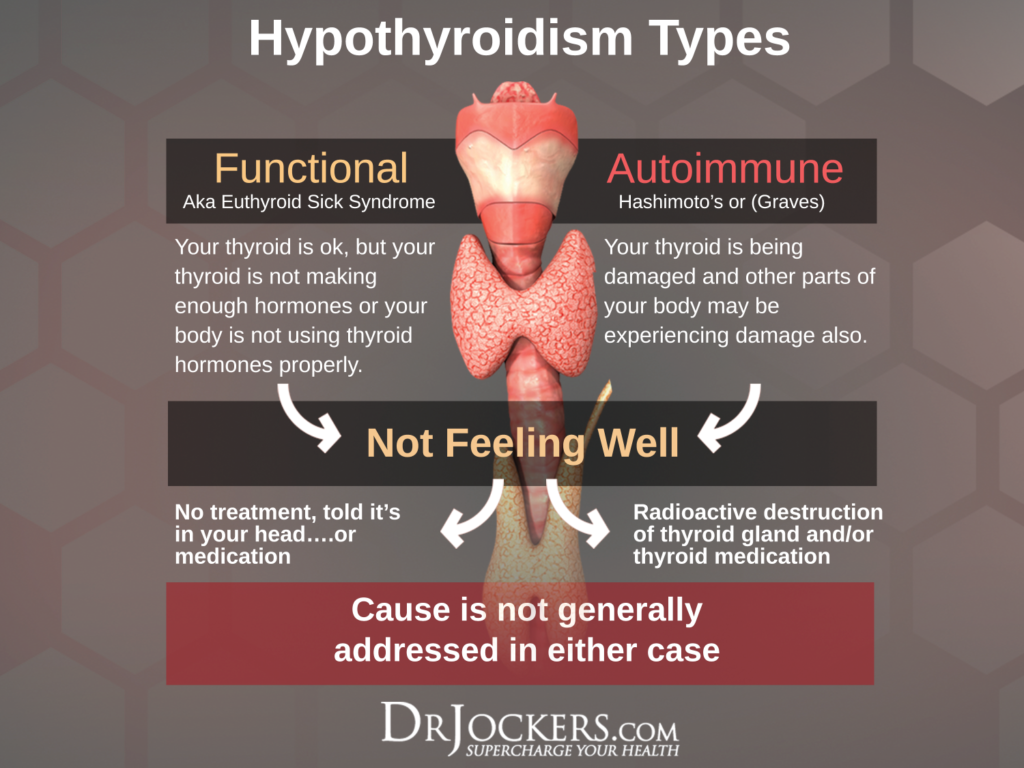
Functional vs AutoImmune Thyroid
Through personal experience, I have found that antibody (autoimmune) testing is only done upon persistent request. The causes and treatments for an autoimmune condition versus a functionally underactive thyroid are different. Therefore, having a clinician to properly test thyroid markers for these differences is extremely important if we want treatment to be the best.
My clients are exhausted with their conventional doctors and unproductive thyroid care, or lack thereof. Many of them come to our website and programs looking for answers. They wonder why nothing is changing, what triggered their thyroid problem to begin with, and what is the best course of action?
Searching for the Solution
We have to ask ourselves, why are doctors not checking every aspect of thyroid function? Furthermore, why are we not addressing the thyroid and its function in our bodies as a whole? We have been compartmentalizing healthcare for too long and it is time to take a holistic approach.
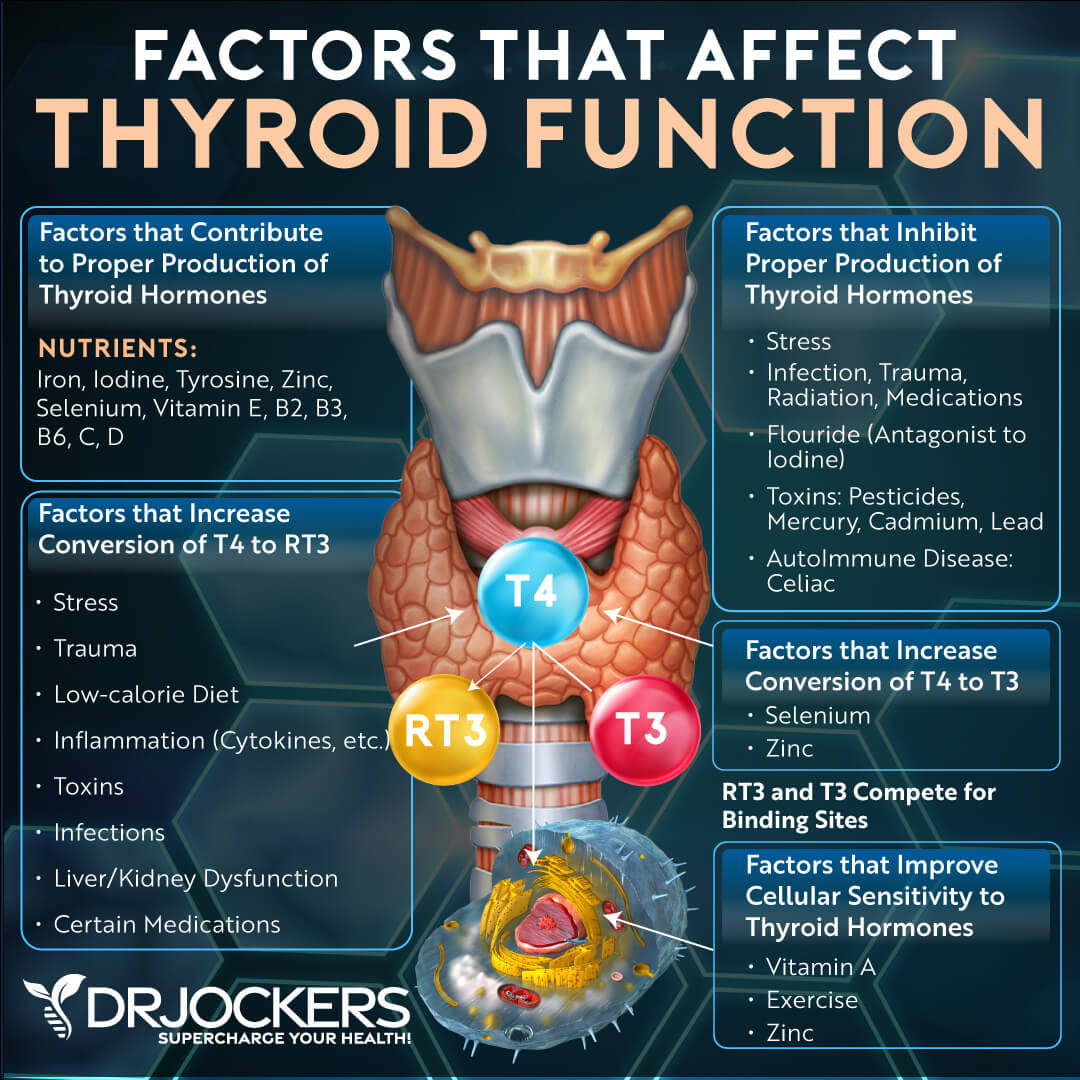
There are many areas for malfunction between the stimulation, secretion, and utilization of the active form of thyroid hormone, T3. There are many key players that perform an important role in this cascade and it is important to look at all of them in order to understand the larger picture of the patient’s thyroid function.
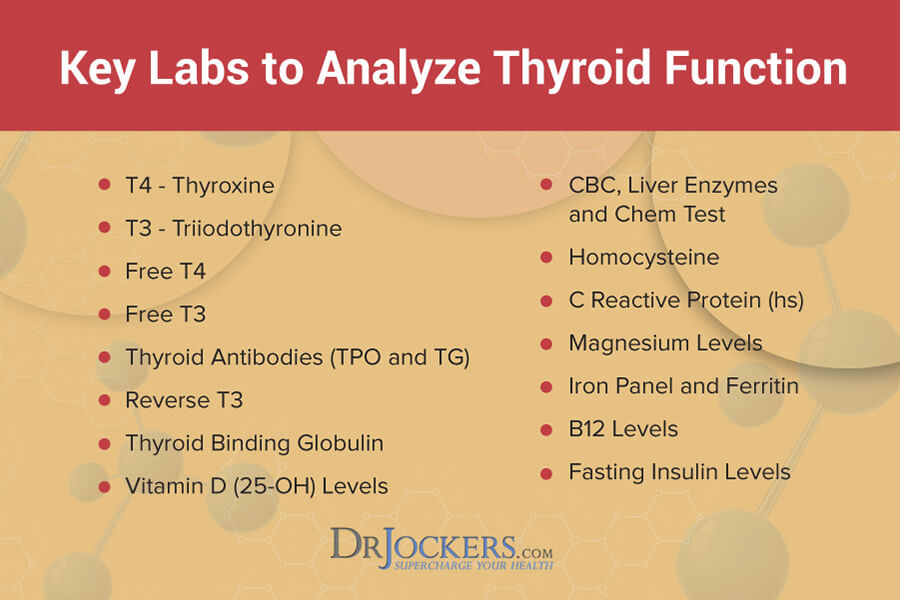
Mainstream medical doctors are only looking at thyroid stimulating hormone (TSH) and some even look at T4 and T3. While these values are important, they do not give us the necessary tools to find the underlying reason for thyroid malfunction.
In this short article, we will look at what lab values should be tested and what these values mean. There is a lot of misinformation out there on the internet so I want this to be straightforward and truthful for educational purposes.
Thyroid Testing
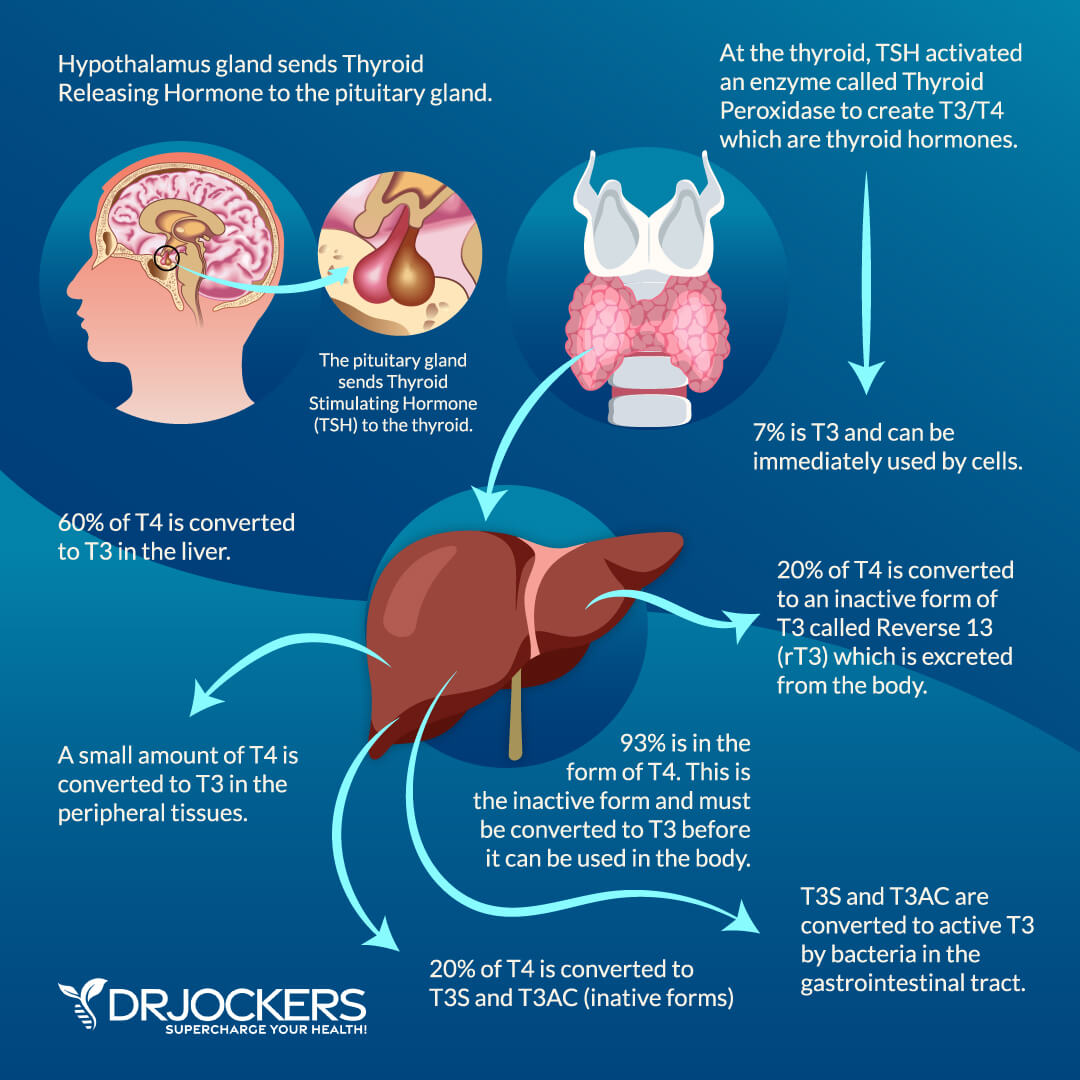
The thyroid responds to signals from the hypothalamus and pituitary in order to appropriately maintain to the body’s metabolic needs. The hypothalamus is responsible for managing hunger, thirst, sleep, hormones, body temperature and other important functions.
It is also constantly monitoring thyroid hormone levels and when more thyroid hormone is needed, it sends out a signal known as thyrotropin releasing hormone (TRH). This hormone travels to the pituitary, which is our master hormone gland, and triggers it to release thyroid stimulating hormone (TSH).
TSH is sent directly to the thyroid, which is then stimulated to produce more thyroid hormone, or T4 (6.) As mentioned before, standard thyroid testing will look at TSH and sometimes T4 and T3.
TSH
TSH levels indicate how your feedback loop between the hypothalamus, pituitary and the rest of the body is doing. It does not tell us how the thyroid itself is functioning. For example, if the body has low levels of the active thyroid hormone, the pituitary will secrete more TSH in order to try to meet the demands for more active thyroid hormone.
Therefore, a high TSH can indicate the underproduction of thyroid hormone and/or hypothyroidism. On the other hand, if the body has elevated levels of the active thyroid hormone, the pituitary will slow the secretion of TSH. Therefore, low TSH can indicate the over-production of thyroid hormones and/or hyperthyroidism.
Another cause of low TSH or elevated T3 could be that the patient is on supplemental thyroid hormone. Supplementation of T3 or natural desiccated thyroid hormone can trick the body into thinking that it has enough T3 circulating and suppress the secretion of TSH.
This may temporarily solve the problem, but symptoms usually reappear because the root cause has not been addressed. Sometimes we can still experience thyroid dysfunction with “normal” TSH levels (5). The clinical range for TSH is 0.5 – 4.5 uIU/mL and the functional range we look at for optimal health for TSH is 0.5-2.0 uIU/mL.
Thyroid Synchrony
TSH also activates the enzyme necessary to create T3 and T4. This enzyme is called thyroid peroxidase (TPO) and it combines thyroglobulin, iodine and hydrogen peroxide. Through this process, the thyroid produces thyroid hormones. The end product is about 93% of the storage form of thyroid hormone, T4.
The other 7% is T3, which is the active form of thyroid hormone (3). As you can see, the thyroid does not produce a large amount of the active form of thyroid hormone. It actually produces the storage form and conversion takes place later. The liver is responsible for converting about 60% of T4 to T3 through the glucoronidation and sulfation pathways.
Any form of liver congestion or portal hypertension will interfere with the T4 to T3 conversion (4). Stress hormone function will results in another 20% being converted into a permanently inactive form of T3, known as reverse T3. Healthy gastrointestinal flora is responsible for converting the last 20% of T4 into T3 (4).
T4
The main hormone produced by the thyroid T4, which is a storage form of the hormone. It is circulated throughout the bloodstream and stored in tissues so that it’s available when needed. We also measure Free T4 since it is unbound and more readily usable by the body.
T4: 6-12 ug/dL (we like to see it around 8-10)
Free T4 (Direct): 1 – 1.5 ng/dL
If free or bound T4 is high, this tells us that the thyroid is overactive and producing too much thyroid hormone. It could also mean that the conversion of T4 to T3 is not occurring in the liver and/or the gut. If Free or bound T4 is low, this tells us that an underactive thyroid is an issue. However, it does not tell us if the problem is functional or autoimmune related. (5).
Measuring T3 Levels
When the body is in need of the active thyroid hormone, it converts storage T4 into T3. A portion of the T3 is bound to thyroid binding globulin while another portion is not bound and that is called free T3. Free T3 can attach to cell receptors and provide power for metabolic processes. If Free T3 is high, this means that the thyroid is overactive or over converting T4 to T3 levels which happens in cases of high testosterone.
If T3 is low, this means that the conversion process may be suffering. Hypothyroid symptoms can still be present even if TSH and Free T4 are within normal limits. A sluggish liver, estrogen dominance and gut dysbiosis can all cause low T3 levels. These are very common causes of an low thyroid function and there are key markers to review when you test thyroid function (5). Here are the optimal ranges for T3 levels.
T3: 100-150 ng/dL
Free T3: 3.0-4.0 pg/mL

Reverse T3
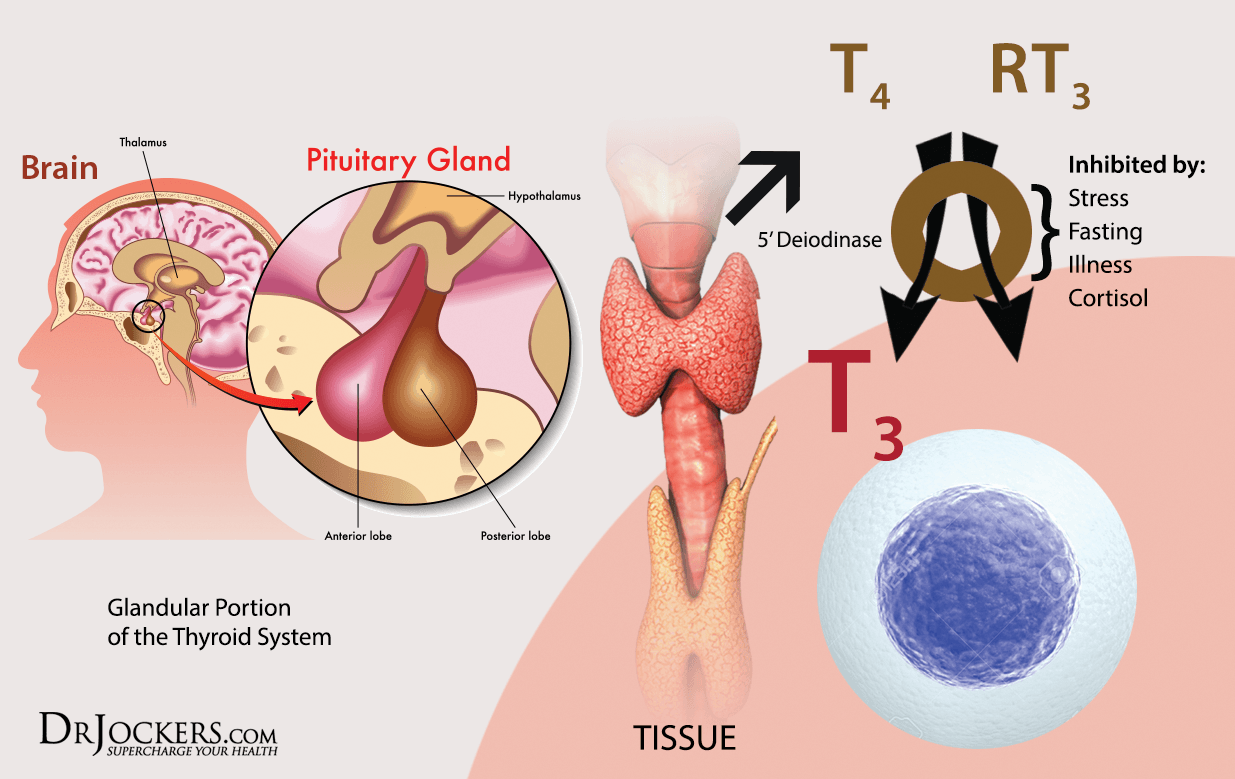
Chronically elevated levels of cortisol, in response to chronic stress, increases reverse T3 production. This mimics free T3 in the body but does not carry out the active duties for metabolic processes in the same way. This is considered a stress induced hypothyroidism. This is a very key measurement to process when you test thyroid function.
The range for rT3 is 9-24 ng/dL and high levels are associated with chronic stress, trauma or malabsorption. Low levels are very rare and not be a clinical indication of any problem but in some cases may be associated with hyperparathyroidism.
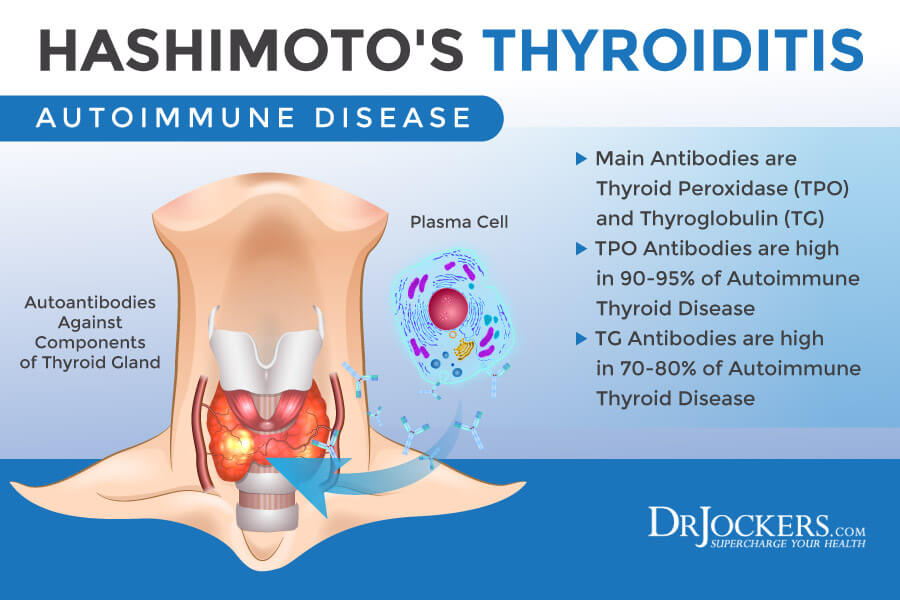
Thyroid Antibodies
Two of the most important antibodies to measure include thyroid peroxidase (TPO) and thyroglobulin antibodies (TG). Thyroid peroxidase attacks the enzyme responsible for assimilating T4. Thyroglobulin antibodies also attack thyroid tissue and impair function. These are important biomarkers to look at when you test thyroid function.
The clinical lab ranges for these antibodies are 0-34 IU/mL for TPO antibodies and 0-0.9 IU/mL for TG antibodies. If the levels for these antibodies are clinically high and the individual has a high TSH over 4.5, along with clinical symptoms, a diagnosis of Hashimoto’s Thyroiditis is made.
If the individual has high antibodies and the TSH is very low and T4 is up over 12 ug/dL along with clinical symptoms, than a diagnosis of hyperthyroidism or Graves disease is made.
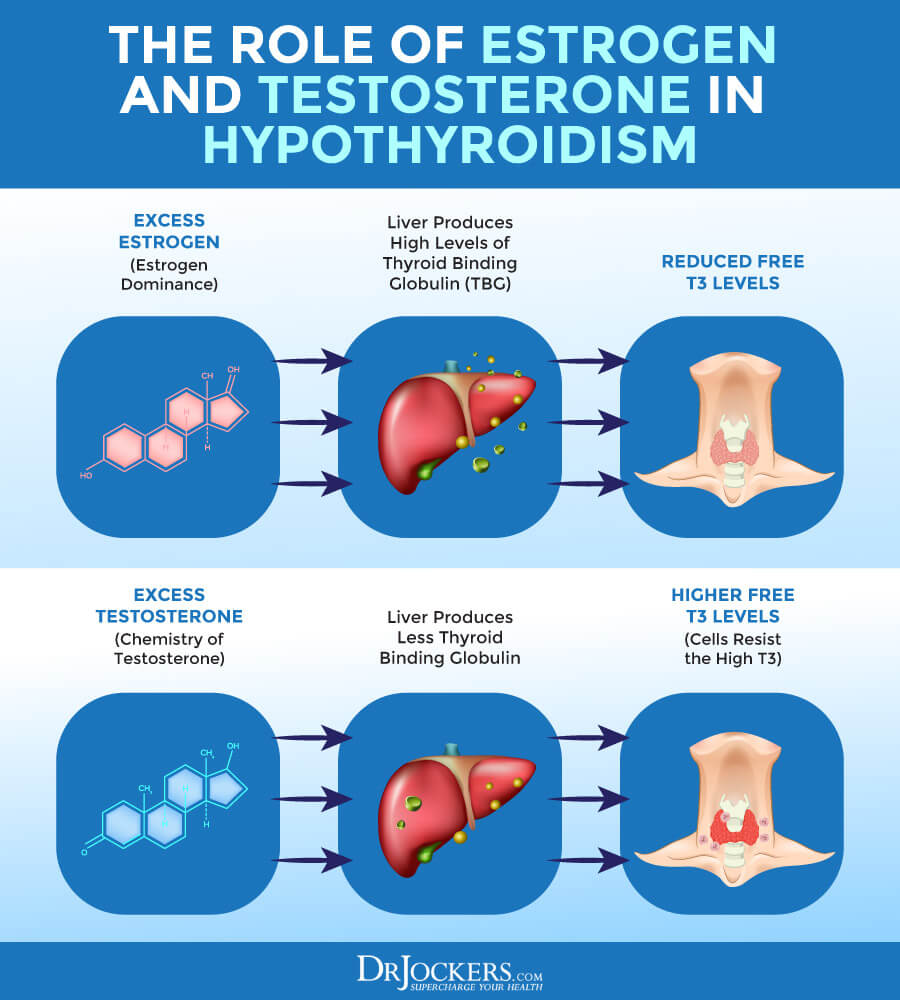
Thyroid Binding Globulin (TBG) and T3 Uptake
TBG is a binding protein that binds free thyroid hormones T4 and T3. When TBG increases it reduces free hormone levels including free T3 levels, which may cause a functional hypothyroidism.
TBG levels can increase during pregnancy, high estrogen levels and liver disease. TBG levels can decrease during hyperthyroidism, Cushing Syndrome, malnutrition, renal disease and medications (7).
The way we measure TBG levels is through T3 uptake because it is easier to measure. The optimal T3 uptake level is 28-38%. The higher percentage the more binding sites are available. This happens with high estrogen which increases TBG and lowers T3 uptake levels. High estrogen can occur with birth control pills, sluggish liver, insulin resistance and estrogen dominance. This results in lower free T4 and T3 levels.
Elevated testosterone will reduce binding sites, which will increase T3 uptake and result in higher levels of free T3. In many cases, the TSH will be normal or low, the T4 levels will be normal or low but the free T3 levels will be high with elevated testosterone. High testosterone is associated with testosterone replacement and with insulin resistance in some women which can also lead to PCOS.
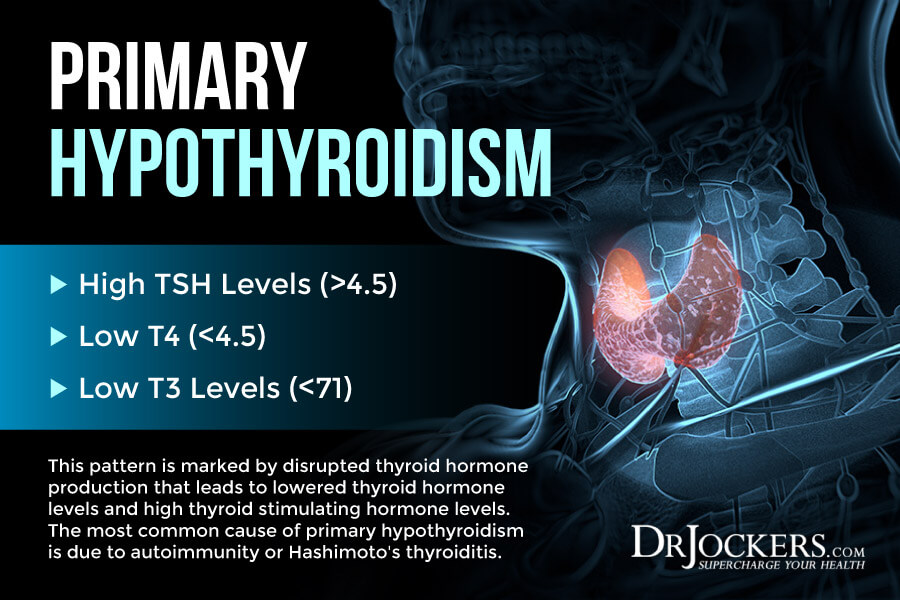
Primary Hypothyroidism:
In primary hypothyroidism, the most common lab finding is high thyroid stimulating hormone (TSH) and low T4 and T3. In this pattern, decreased thyroid hormones (T3 and T4) in the blood stimulates the hypothalamus which stimulates the pituitary gland to release TSH. TSH stimulates an enzyme in the thyroid gland called Thyroid Peroxidase to use iodine to create more T3/T4 which is released into the blood. The increase in T3/T4 stop the hypothalamus which stops the pituitary from releasing TSH which stops the production of T3/T4.
In primary hypothyroidism, the thyroid gland does not produce enough T3/T4 which means there is chronically low amounts of the hormones circulating in the blood. This causes the hypothalamus to continually send signals to the pituitary which is continually releasing larger and larger amounts of TSH.
Patients with blood test results that show high levels of TSH are prescribed synthetic thyroid hormones to increase the amounts of circulating thyroid hormones and shut down the stimulation of the hypothalamus/pituitary. This decreases the amount of TSH and “normalizes” your blood tests.
Unfortunately, most medical doctors are only familiar with primary hypothyroidism and fail to find other patterns of hypothyroidism. Here are 6 additional patterns to be aware of.
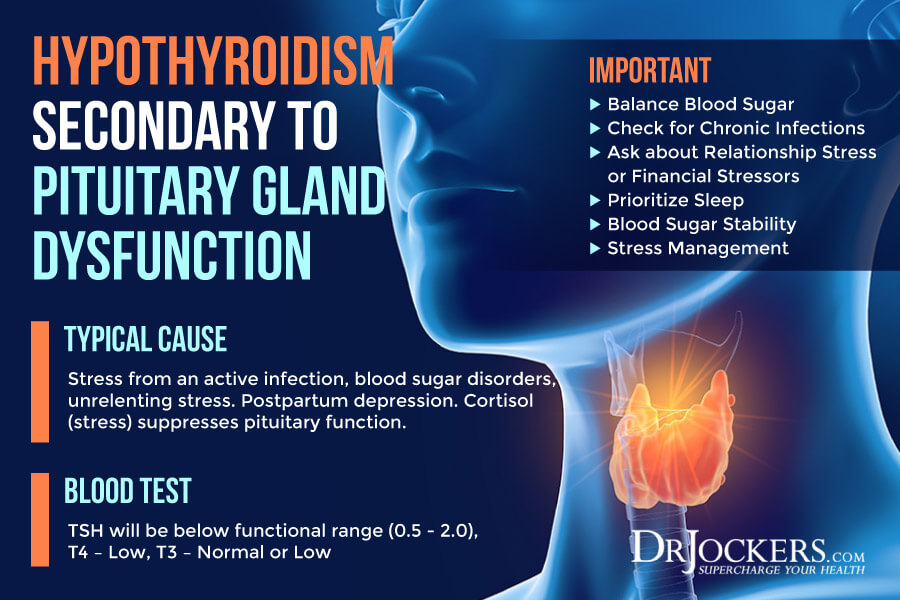
Pattern #1: Hypothyroidism Secondary to Pituitary Hypofunction
In this pattern, the pituitary gland is unable to send out enough TSH to stimulate the thyroid. A blood test would result in low levels of TSH, which would indicate either a normal working thyroid or even a hyperthyroid! Of course, the lack of TSH stimulation causes the thyroid to to either produce just enough thyroid hormone or too little thyroid hormone.
The most common cause of a suppressed pituitary is chronic stress. Constant bombardment of the pituitary gland by adrenal hormones causes the pituitary to shut down with the added side-effect of decreasing TSH output.
If the doctor only tests for TSH, he/she would assume that thyroid function was normal (which it would be if there was enough TSH) even though the patient was presenting with signs and symptoms of hypothyroidism. If prescription thyroid medication is used, it may initially help symptoms. However this is a dangerous course of treatment.
Flooding the system with thyroid hormones causes the pituitary to be suppressed even further. Larger amounts doses of hormones are prescribed and the increase of hormones in the system causes cells to become resistant to thyroid hormones (similar to pre-diabetics being insulin resistant). Eventually the pituitary/thyroid communication could be permanently lost requiring a lifelong dependence to prescription medications.
Post-partum depression is another cause of a suppressed pituitary. The stresses of pregnancy and birth can rapidly suppress the pituitary leading to symptoms of hypothyroidism.
Typical Cause: Stress from an active infection, blood sugar disorders, unrelenting stress. Cortisol (stress) suppresses pituitary function.
Blood Test: TSH will be below functional range (0.5 – 2.0), T4 – below 6, T3 – Normal
Important: Balance blood sugar, Check for chronic infections, ask about relationship stress or financial stressors. Prioritize sleep, blood sugar stability and stress management.
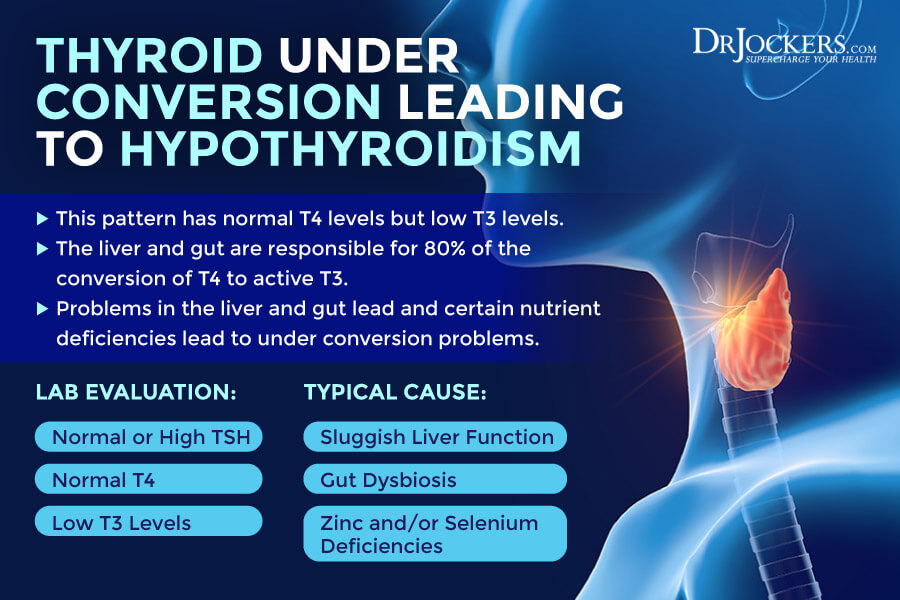
Pattern #2: Thyroid Under Conversion Leading to Hypothyroidism
In this pattern, the thyroid and the pituitary are working properly, but the conversion of T4 (inactive) to T3 (active) is hampered. This means that the cells can not use the hormones present in the blood. The properly functioning thyroid means that there is enough hormones present to make the TSH test normal.
If the doctor tested for T4 as well (which is often the second test run after the TSH test), this too would be normal. T4 is inactive, and it must go through conversion process to become T3, the active form of thyroid hormone.
After the hypothalamus stimulates the pituitary, and after the pituitary releases TSH, and after thyroid peroxidase makes T3/T4 in the thyroid, T3 and T4 is released into the blood and catches a ride on a protein called Thyroid Binding Globulin which acts as a taxi to transfer the hormones.
Roughly 93% of the thyroid hormones is in the form of T4 which is an inactive form and must be converted to T3 before the cells of the body can use it. 7% is made into T3 and can be immediately transferred to cells by thyroid binding globulin proteins.
In the liver, around 60% of the inactive T4 is converted to T3. Another 20% gets converted to reverse T3 which is inactive and excreted from the body. The last 20% is converted to T3S and T3AC which are inactive forms of T3. T3S and T3AC are then converted into the active form of T3 by bacteria located in the gastrointestinal tract. It can then be used by the cells of the body to fuel metabolism
Conversion takes place in the liver and GI tract, if these areas are sluggish it can lead to an under conversion of T4-T3. The liver is the area where 60% of the conversion takes place and is usually the site of the problem, although the gut and liver work together so you really need to address both. Other factors include stress, inflammation and zinc and selenium deficiencies.
Typical Cause: Poor diet and gut function can lead to a deficiency of nutrients responsible for adequate function of the enzymes needed for conversion. Can also be caused by zinc and/or selenium deficiencies.
Lab Evaluation: Normal TSH, Normal T4 & Free T4 Levels and Low T3 & Free T3 Levels
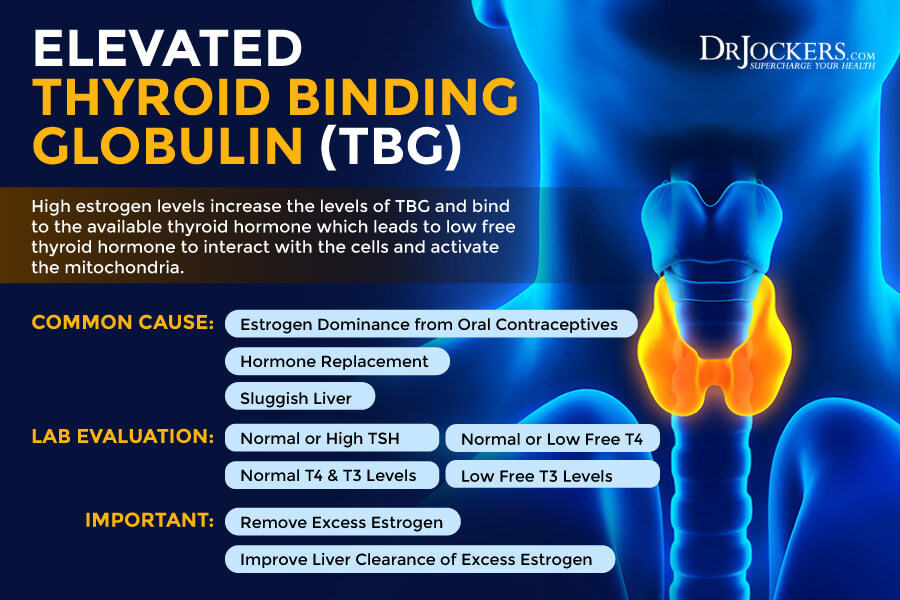
Pattern #3: Elevated Thyroid Binding Globulin leading to Hypothyroidism
Thyroid binding globulin (TBG), as stated earlier, is a protein that acts as a taxi to transport thyroid hormones through the blood. In this pattern, the pituitary, thyroid and conversion of hormones are all working properly, but there is too much TBG transporting the hormones.
Like a real taxi cab, thyroid hormones can not ever reach the destination cells if they never get out of the taxi! Any free thyroid hormone in the system quickly attaches to a TBG and simply drives around without ever getting out and entering cells.
High estrogen levels from oral contraceptives, hormone replacement therapy, our food supply, or hormone creams increase the level of TBG. TSH levels are still normal due to the circulating hormones.
Common Cause: Estrogen dominance from oral contraceptives, hormone replacement or sluggish liver.
Lab Evaluation: Normal or High TSH, Normal T4 & T3 Levels and Normal or Low Free T4 & Low Free T3 Levels
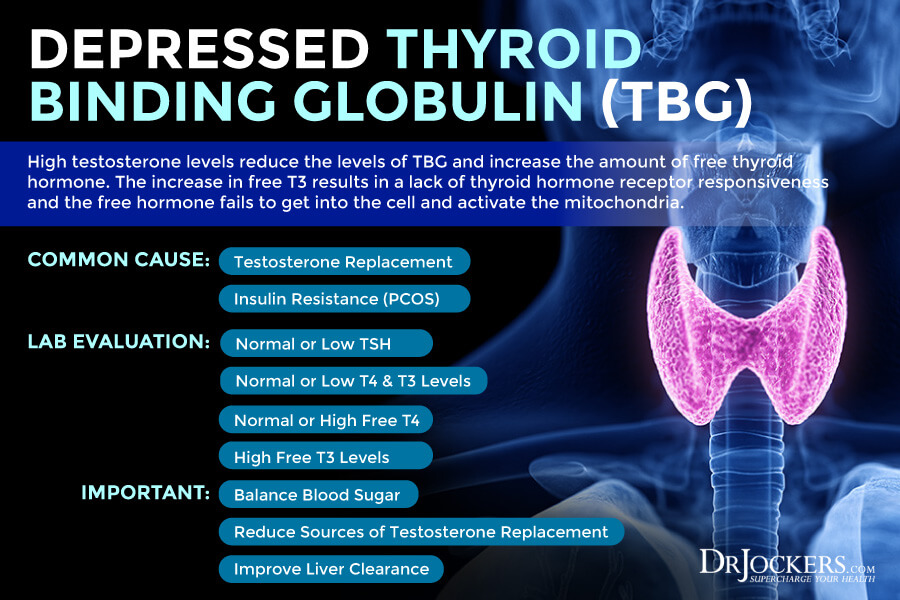
Pattern #4: Depressed Thyroid Binding Globulin leading to Hypothyroidism
This is a pattern associated with High Testosterone. High Testosterone reduces thyroid binding hormone levels making more free hormones available.
The thyroid and pituitary are again working properly, but this time there is too much T4 converted to T3 (remember roughly 20% of T4 is converted into reverse T3 which is inactive and excreted). High levels of testosterone is the cause which also has the added effect of decreasing the amount of thyroid binding globulin (TBG: the taxi that carries the thyroid hormones).
The high levels of T3 in conjunction with low TBG causes cells to become resistant to T3. They close the doors and do not allow anymore T3 into the cells. TSH levels will be normal even though the patient is showing signs of hypothyroidism.
This pattern is similar to insulin resistance. In fact, patients with thyroid over conversion often also present with insulin resistance and polycystic ovary syndrome (PCOS) which is also caused by increased testosterone levels. Managing blood sugar is extremely important. Since there is already too much T3, prescription thyroid medication will not help in this pattern.
Lab Evaluation: Normal or Low TSH, Normal or Low T4 & T3 Levels, Normal or High Free T4 & High Free T3 Levels
Common Causes: Testosterone replacement or insulin resistance.
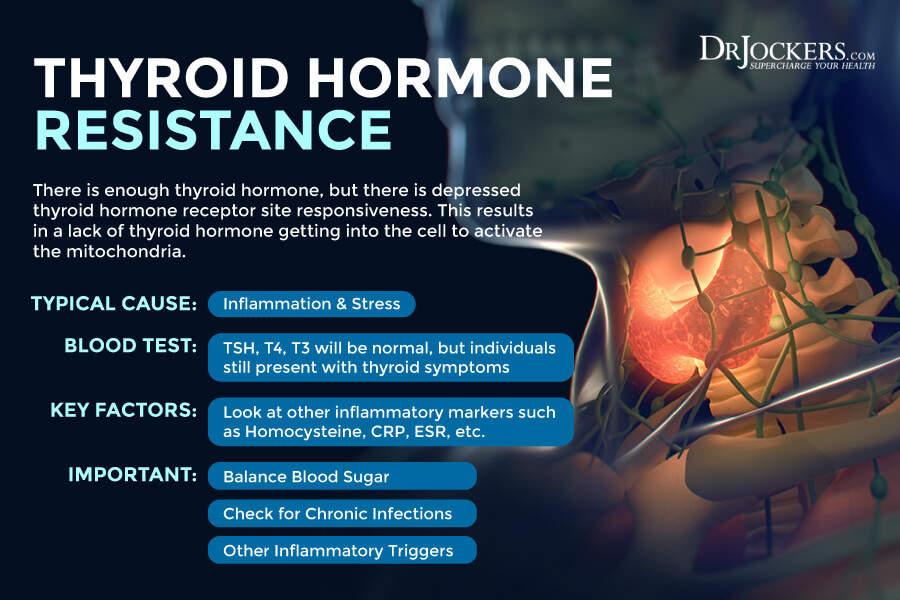
Pattern #5: Thyroid Hormone Resistance leading to Hypothyroidism
In this pattern, there is depressed thyroid receptor site responsiveness. This means that the proper amount of free hormones are in the blood stream but they aren’t getting into the cells where they are needed.
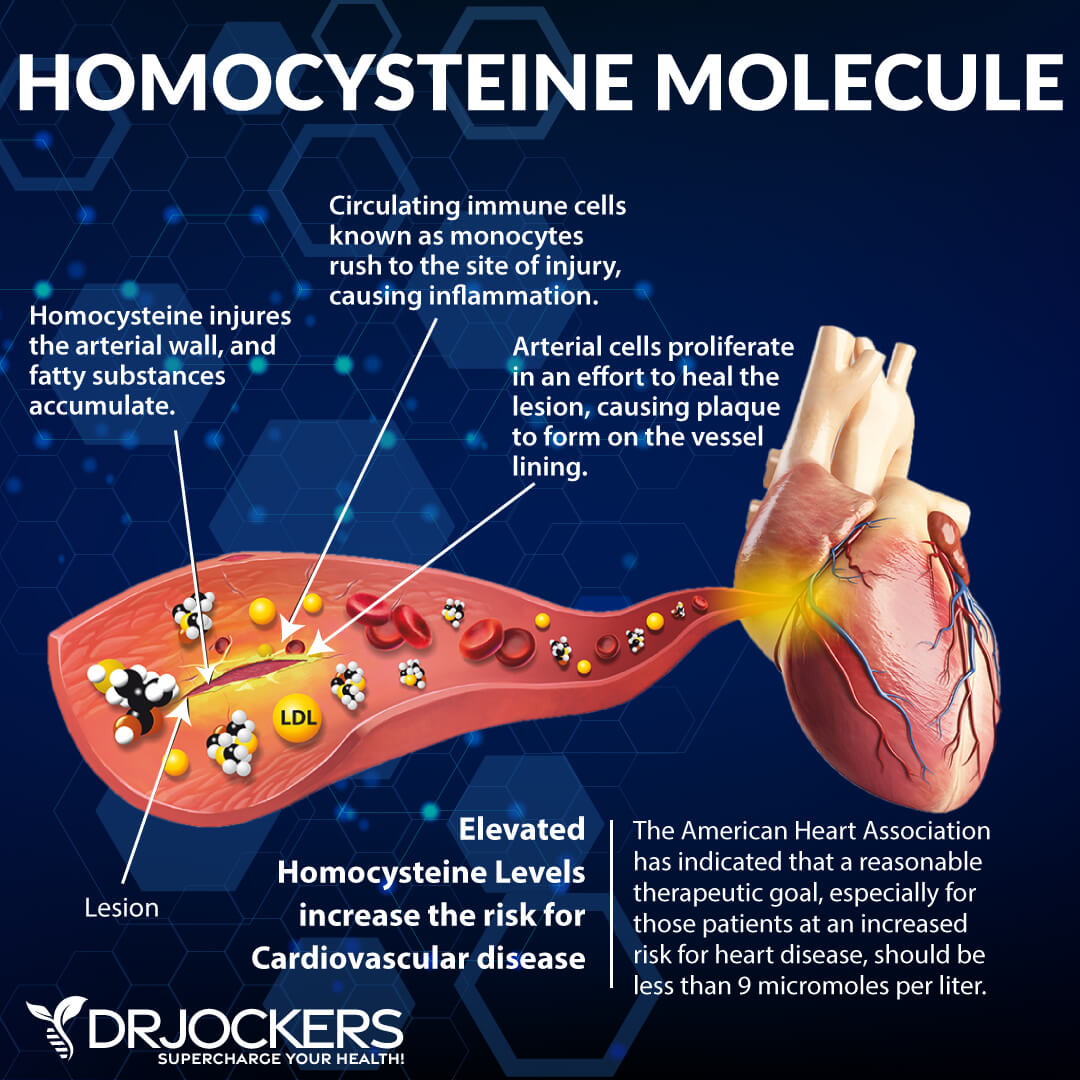
Chronic stress or elevated homocysteine levels can cause thyroid resistance similar to what happens in thyroid over-conversion. In this pattern it is not too much T3, but too much inflammation or cortisol which causes the resistance. TSH levels are again normal and prescription thyroid medication would not have much effect.
Blood Test: TSH, T4, T3 will be normal, but individuals still present with thyroid symptoms
Typical Cause: Stress & Inflammation
Important: Careful examination of immune related disorders and managing stress
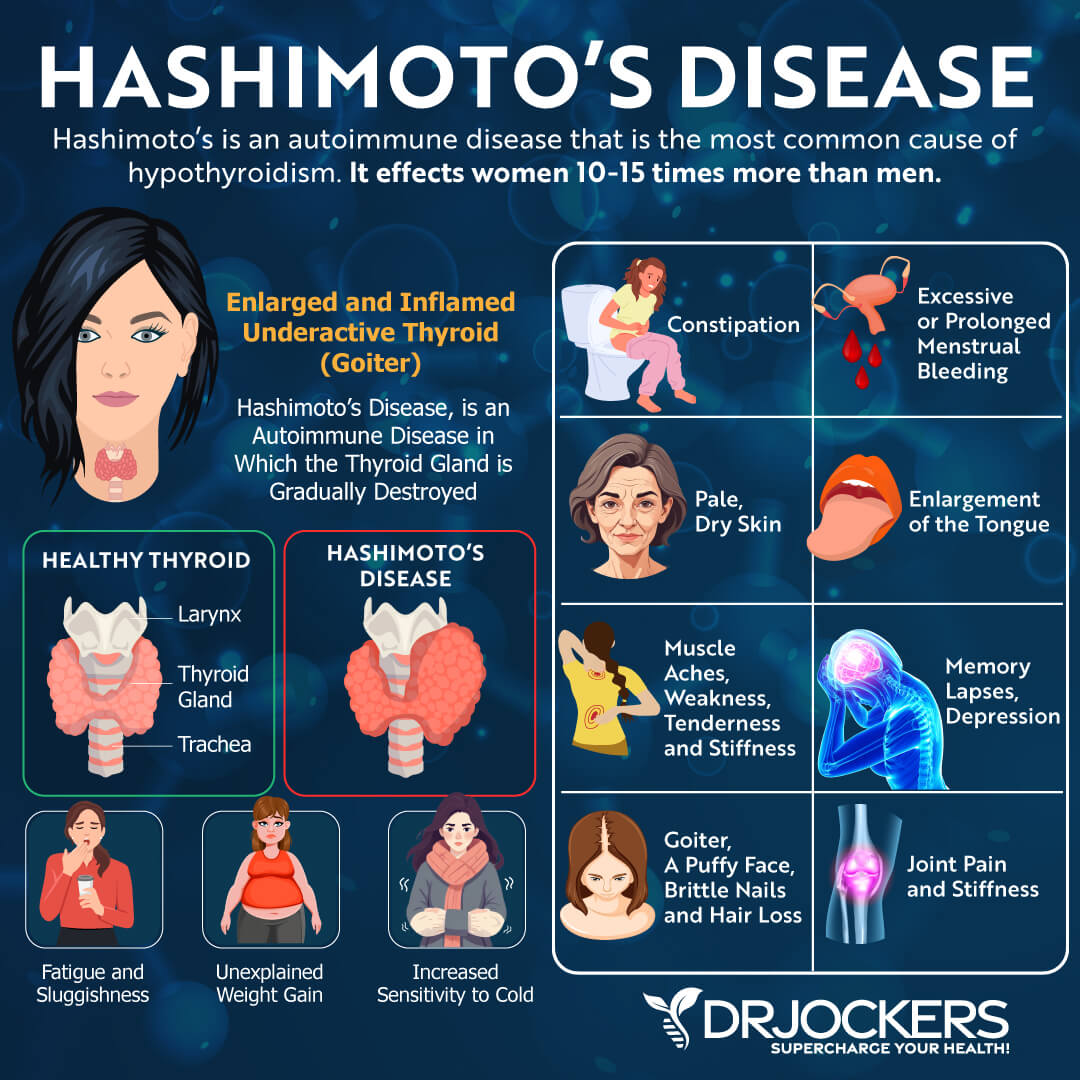
Pattern #6: Autoimmunity Leading to Hypothyroidism
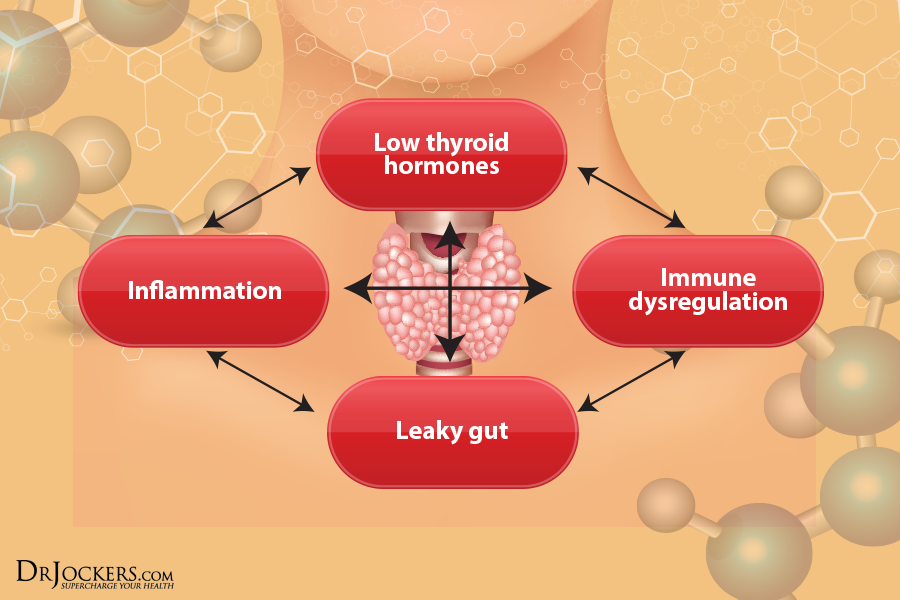
This is the most common cause of primary hypothyroidism and is called Hashimoto’s thyroiditis. In this pattern, the immune system recognizes and flags the thyroid proteins as a threat and develops memory cells to destroy thyroid tissue.
An elevation in TPO or TG antibodies is an early warning sign that this is occurring. Overtime, if the thyroid destruction continues, the thyroid will be unable to produce enough T4 and then the hypothalamic-pituitary-thyroid axis will ramp up with higher levels of TSH to try to signal for the production of more thyroid hormone.
Blood Test: Positive Antibodies to TPO or TG. High TSH and low T4 and T3 levels.
Typical Cause: Immune Dysregulation – not a thyroid disorder
Important: Manage immune system/barrier system – manage triggers, heal/seal the gut, restore immune integrity.
Additional Labs to Help Support Thyroid Health
There are some additional labs that look at key nutrients and inflammatory markers associated with thyroid health. These are specialized labs you can ask your doctor to run or work with a functional health coach to get these fun and evaluated for you.
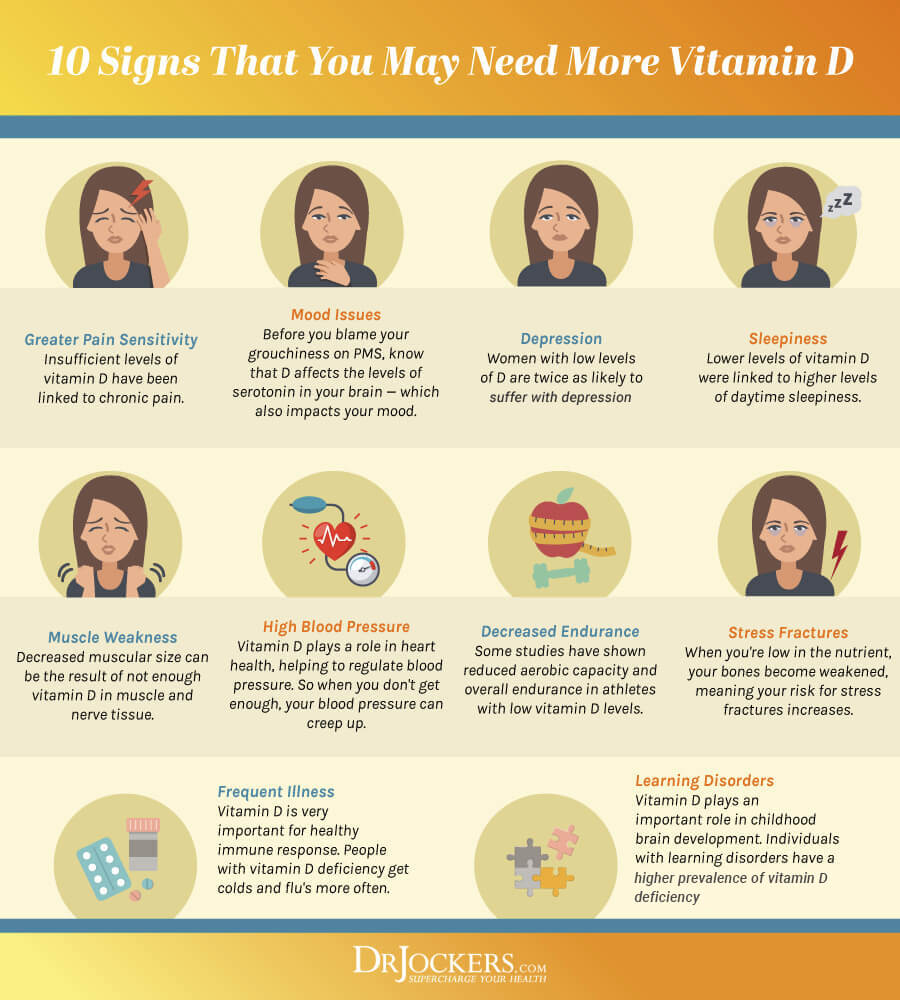
Vitamin D (25-OH) Levels
Low vitamin D3 is associated with thyroid disorders and should be addressed. Vitamin D levels play a very important role in immune regulation, calming down autoimmunity and keeping inflammation levels under control (8).
The test you are looking for is the 25-OH vitamin D3 and the optimal levels are between 50-100 ng/ml. Getting regular sun exposure and supplementing with vitamin D3 at 1,000 IU per 25 lbs. of body weight (taken with food) is the best way to improve and optimize your levels.
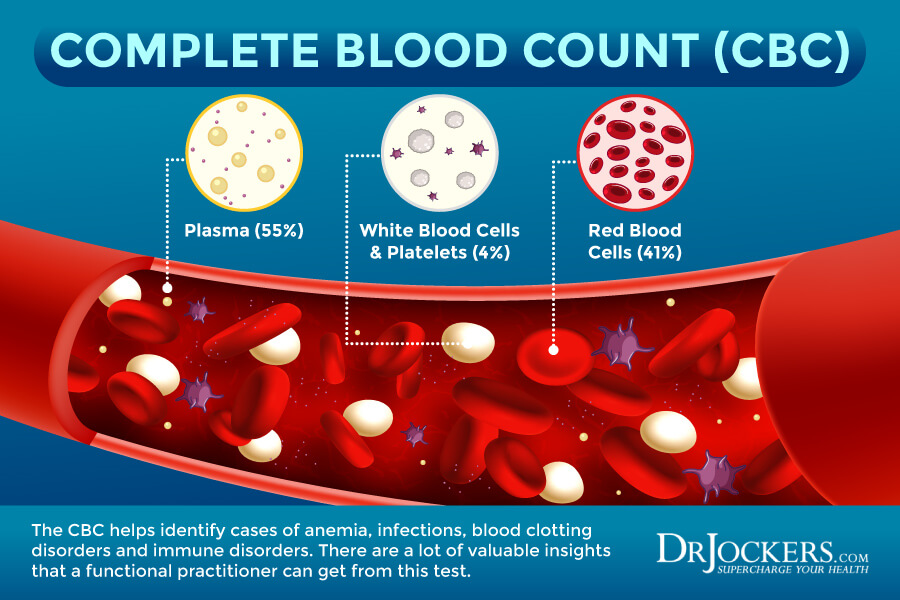
CBC & Chem Test
A complete blood count will look in detail at red blood cell counts, iron stores and white blood cell levels. Both iron-deficient and B12 deficient anemia are a common finding with thyroid disorders. This portion of the test will also check for liver function.
As mentioned before, 60% of T4 to T3 conversion takes place in the liver so we want to check for adequate liver function. Finally, this test looks at kidney health, digestive health and blood sugar regulation.
Homocysteine:
Elevated homocysteine levels is an indicator of poor methylation function, which also complicates thyroid function (9). Homocysteine is an inflammatory byproduct of the metabolism of the amino acid methionine. Optimal levels of homocysteine are between 6-9 mmol/L. If your levels are elevated it is a sign of poor methylation and inflammation.
Certain nutrients such as vitamin B2, B6, folate and B12 as well as magnesium and zinc are key for optimal homocysteine levels. These same nutrients are important for healthy thyroid function.
CRP-hs
C Reactive Protein (CRP) reveals the inflammatory status of the body. Increased inflammation impedes the T4-T3 conversion. I like to test this in order to assess what the inflammatory load is on the body and how that may be impacting the thyroid.
The best test for CRP is the high sensitivity reading or Hs-CRP which is more accurate than standard CRP testing because it breaks it into .01 measurements. Optimal levels are under 1.0 mg/L.
Magnesium
Lowered magnesium is a common deficiency and will also effect thyroid function (10). Magnesium is critical for over 300 function in the body including the production of cellular energy. It is also very important for blood sugar stability and healthy adrenal-pituitary and hypothalamic function.
A magnesium deficiency can lead to chronic inflammation and increased pituitary gland stress that alters proper TSH production. I always want to look at magnesium levels when I test thyroid function. Optimal levels are over 2.0 mg/dL
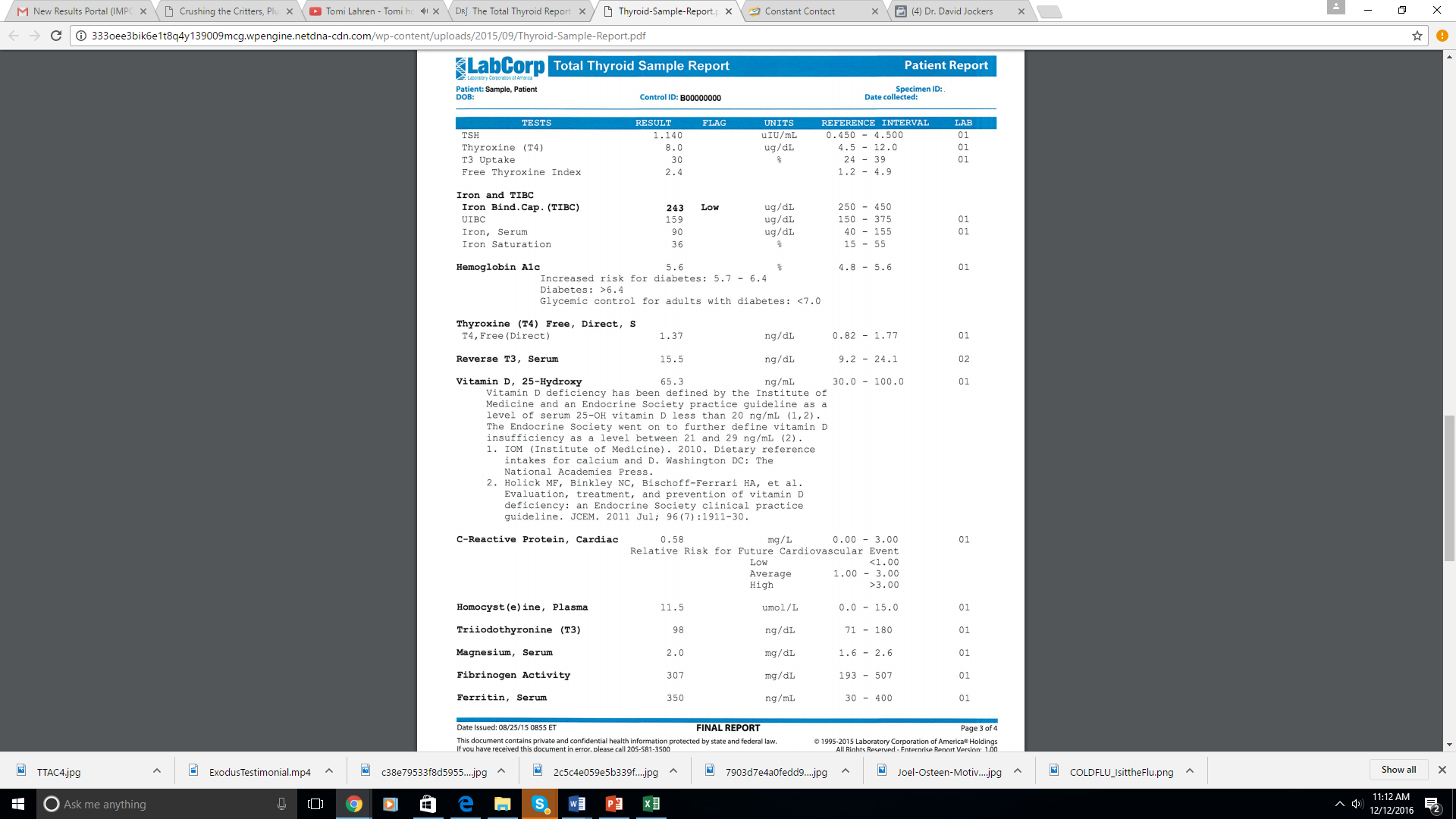
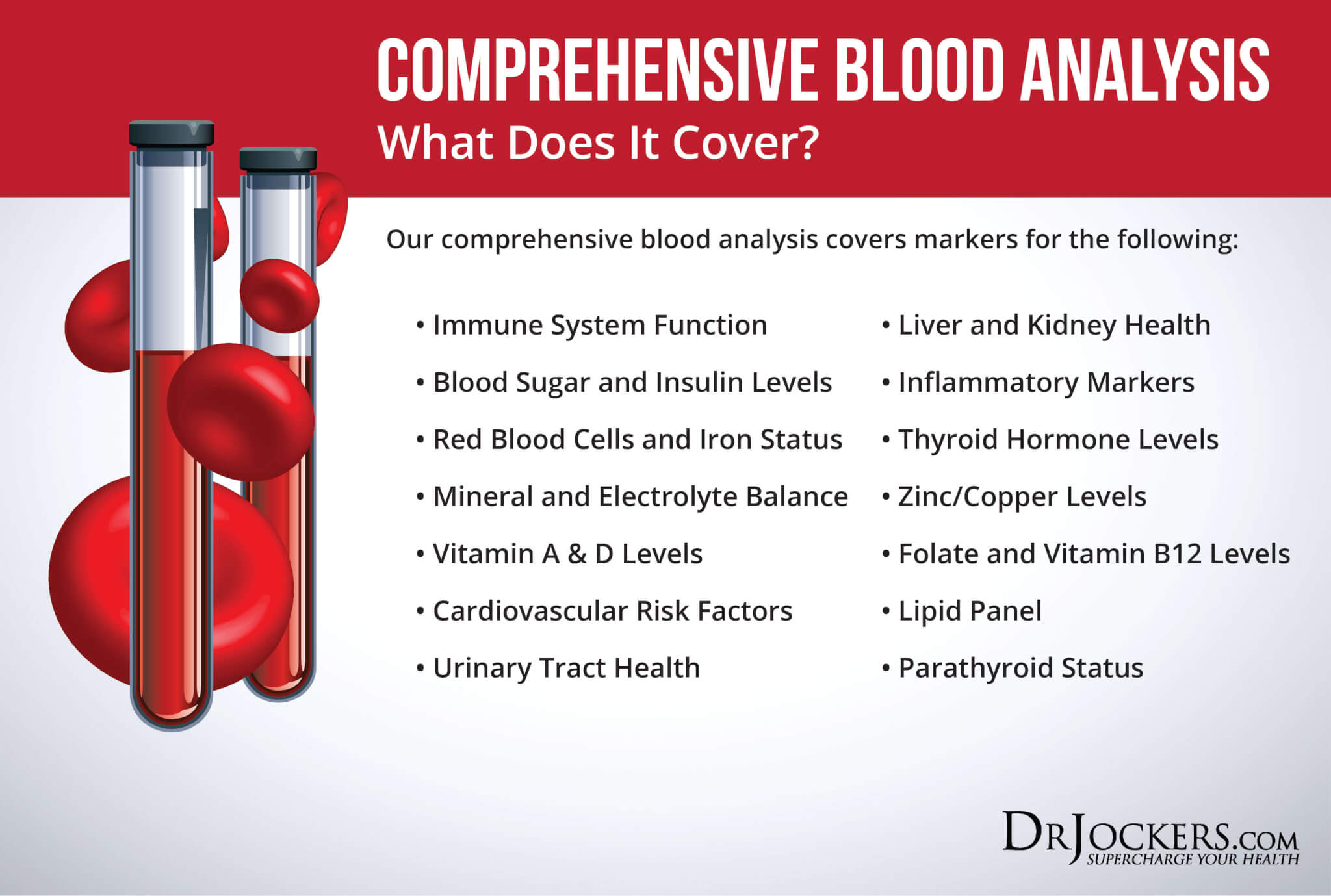
Comprehensive Blood Analysis
Taking a standard thyroid hormone, such as Synthroid or Armour Thyroid, does not address the underlying cause. If thyroid problems are related to antibody, thyroid binding globulin or reverse T3 production, taking additional medications or hormones can actually promote more thyroid and hormonal disruptions.
When we suspect a thyroid problem, we recommend our Comprehensive Blood Analysis which has all the testing we discussed in this article. We sincerely hope that you find the solution to your thyroid problem and would be more than happy to help you through the process!
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!



As a certified clinical nutritionist, I have to say this is very well and clearly presented. Thanks for getting the word out concerning thyroid function and testing.
Thank you so much Crystal!
So how do we get the proper test? Can we ask our doctor to peform this test? In my experience it is not that easy ….
Yes, you can order the test here or download the sample copy and bring it to your doctor to order: https://drjockers.com/complete-thyroid-report/
If we suspect we suffer from a malfunctioning thyroid but all tests appear “normal” is there something we can do, other than RX medication, to improve the fuction of our thyroid?
I would recommend seeing a functional doctor, because most likely the tests are not normal…just not pathological. You may have functional imbalances. You can email our functional diagnostic nutritionist Haley at nutrition@drjockers.com and she can help.
I live in the UK,and wonder how I can get these special tests done here.
You should try to request them from your general physician or look for a functional medicine doctor in your area.
When my last daughter was born 12 years ago I was told my pituitary glad wasn’t working at all but my thyroid was working fine…I still do not believe this…I would love to test them and find out what is going on in my body and possibly heal with diet…I don’t know if you can help ?
Yes Jennifer, this is the lab test you would want to get. https://drjockers.com/complete-thyroid-report/