Pancreatitis: Symptoms, Causes and Natural Support Strategies
Pancreatitis can be a debilitating condition that results in overwhelming pain and malnutrition. Chronic pancreatitis in the United States results in more than 122,000 outpatient visits and more than 56,000 hospitalizations per year. Painful flare ups bring these patients in for help. The most common causes of pancreatitis and additional flare ups include alcoholism and obstructive gallstones in the liver that block the pancreatic duct.
As a healthcare provider, I feel compelled to help these patients deal with their pain naturally and relieve the causes as best as possible. Many of these patients experience their lives being changed forever due to an inflamed pancreas and they go to the medical doctor to receive pain medication and told to consume a low fat and low salt diet. This leaves the patient severely malnourished. They may be pain free, but the effects of opioids, NSAIDs, and malnutrition make the body function decline drastically.
Unfortunately, there is currently little research done on natural ways to overcome pancreatitis. However, this article will dive into the few natural support strategies that that can improve the health of the pancreas. It is important to note that the strategies I discuss are not currently FDA approved to prevent, mitigate, treat or cure pancreatitis and should not be confused as such.
Anatomy and Physiology
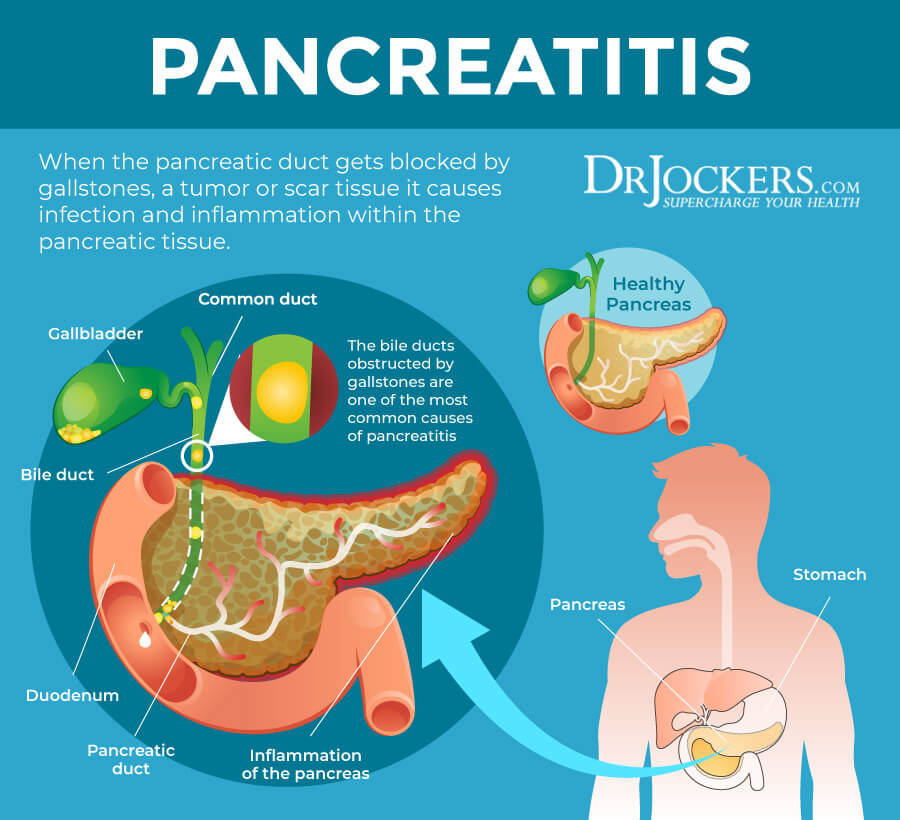
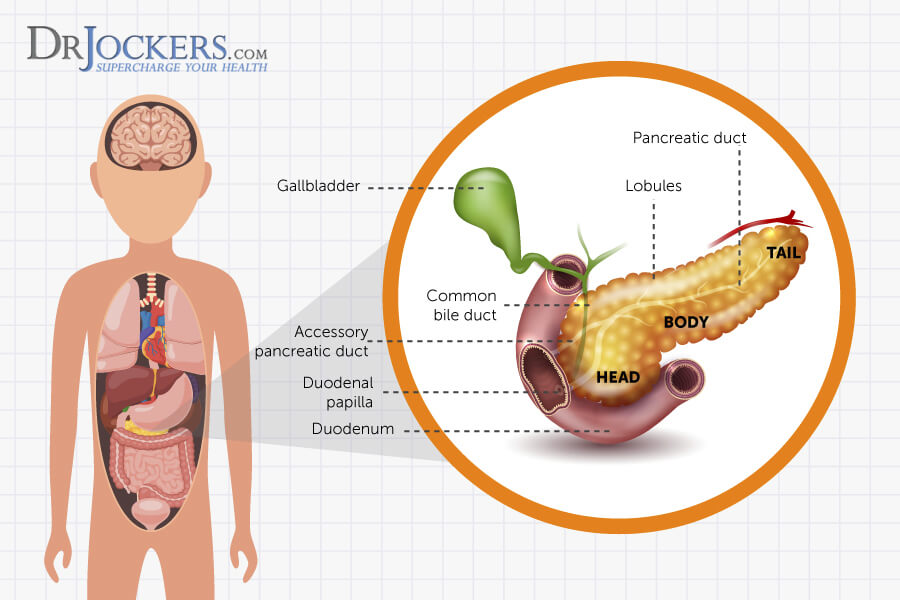
The pancreas is located in the upper abdomen close to the liver and rests just behind the stomach. It has a connecting entrance into the duodenum of the small intestine. The pancreas is known for having exocrine and endocrine functions, meaning that it secretes hormones externally and internally respectively.
The pancreas has a pancreatic duct, which runs along the middle of the pancreas and joins the common bile duct and enters the duodenum at the ampulla of Vater. This opening is surrounded by the sphincter of Oddi, which helps to control the rate at which the pancreas and gallbladder elicit secretions into the duodenum (1).
Exocrine Secretions
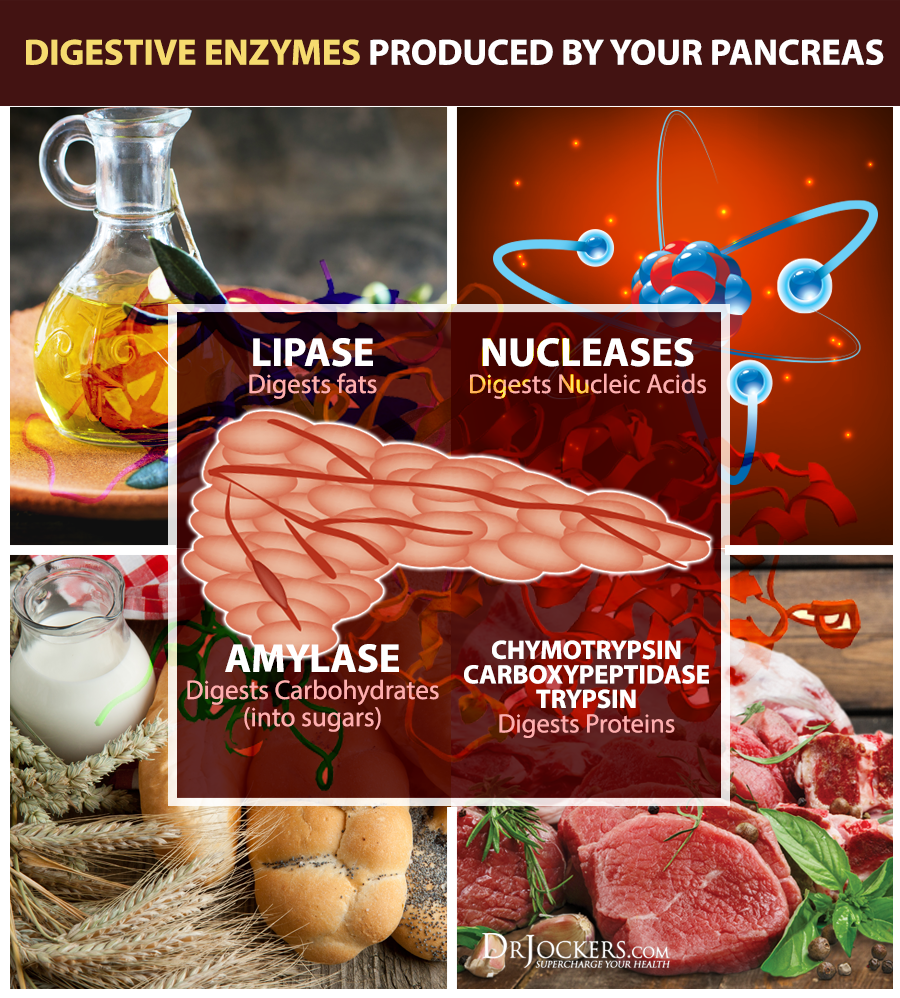
There are three main enzymes, which hare high in protein content and an electrolyte-rich fluid, secreted by the pancreas in order to digest food particles. The secretion itself is alkaline because of the high concentration of sodium bicarbonate present in the fluid.
The alkaline secretion enables the enzymes to neutralize the highly acidic gastric juice before it enters into the intestines. If the pancreas is not secreting enzymes correctly, the acidic gastric contents can go directly into the duodenum and become excruciatingly painful.
The main enzymes are:
- Amylase: Aids in carbohydrate digestion
- Trypsin: Aids in digestion of proteins
- Lipase: Aids in the digestion of fats
- Nucleases: Aids in the breakdown of Nucleic acids
Other enzymes are secreted to breakdown more complex foods, but these four are the main ones to be focused on. The secretion of these enzymes is stimulated by hormones produced in the gastrointestinal tract. Secretin is the major hormone that stimulates increased sodium bicarbonate secretion from the pancreas and the hormone released by the small intestine called CCK is the major stimulus for secretin.
Both of these are located in the cells of the duodenum. As soon as gastric juices enter into the duodenum, the pH and contents stimulate the release of these hormones that cause the pancreas and gallbladder to respond with bile and enzyme release. The vagus nerve also plays a role in exocrine pancreatic secretion (1).
Endocrine Function
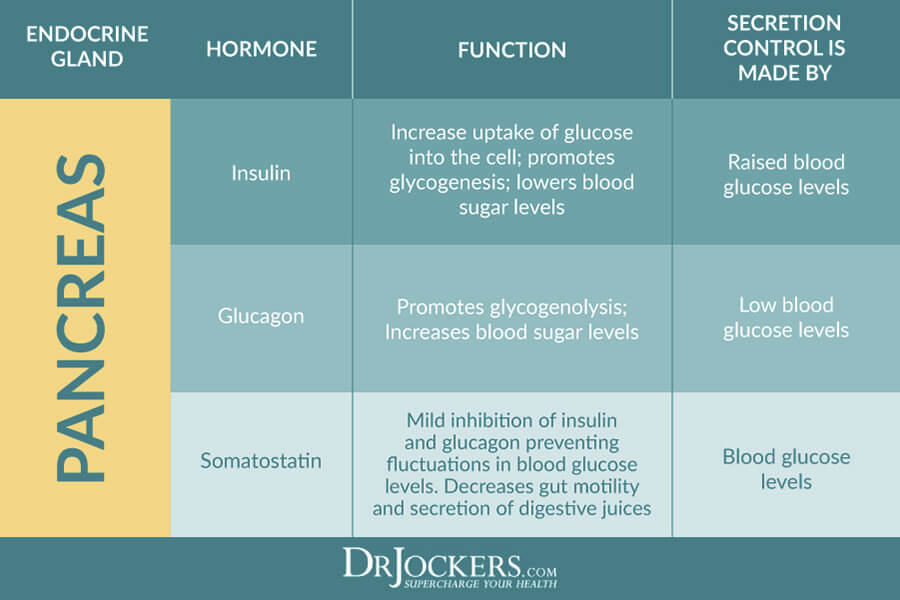
The endocrine portion of the pancreas houses cells known as the islets of Langerhans. These are composed of alpha, beta, and delta cells. Insulin is produced by the beta cells, glucagon by the alpha cells, and somatostatin by the delta cells. These are the three hormones secreted internally by the pancreas that will be focused on here.
- Insulin’s function is to lower blood glucose by stimulating the uptake of glucose into the cells. Once it is pushed into the cells, it is either used for energy or stored as glycogen for later use. Insulin also promotes the storage of fat and protein synthesis. The level of insulin secreted by the pancreas is controlled by the amount of glucose in the blood.
- Glucagon has the opposite function of insulin. It is used to raise blood glucose by converting stored glycogen into glucose in the liver. Glucagon is secreted by the pancreas when blood glucose levels decrease.
- Somatostatin interferes with the release of growth hormone from the pituitary gland and glucagon from the pancreas. Both of these factors act to raise blood glucose levels while somatostatin acts to bring it down.
Significant dysfunction of the pancreas must occur before enzyme secretion is impaired and inhibits proper digestion of fats and proteins. Normal pancreatic enzyme secretion is between 1,500-3,000 mL/day (1).
Geriatric Considerations
As the body ages, or metabolic dysfunction ensues, there is an increase in the amount of fibrous material and fatty deposition in the pancreas. The rate of pancreatic secretion is decreased, which means decreased amylase, trypsin, lipase, sodium bicarbonate and other enzymes. This could be due to delayed gastric emptying and pancreatic insufficiency.
These malfunctions can cause decreased absorption of nutrients and result in many deficiencies. Promoting dietary choices and supplements that help maintain a healthy pancreas is crucial for nutrient absorption and overall health (1).
Pancreatitis is inflammation of the pancreas caused by the release of pancreatic enzymes into pancreatic tissue, which causes hemorrhage and necrosis. Hemorrhage means that there is excessive bleeding caused by tissue damage. Necrosis is premature cell death due to injury, disease, or lack of blood supply.
Typically, enzymes are not activated until they reach the inside of the intestines where the environment is able to handle activated enzymes. Therefore, when these enzymes get congested and release into the pancreatic tissue, the enzymes begin to digest the pancreas and this is extremely painful.
Most people are aging very poorly due to a number of lifestyle factors including poor dietary habits, exposure to environmental pollutants, medication usage, insufficient sleep, economic pressure and emotional stressors. These all impact the ability of the pancreas to function normally.

Acute Pancreatitis
There are approximately 5,000 new cases of acute pancreatitis in the United States every year. This can be a deadly attack; studies show that the mortality rate associated with acute attacks alone is 10 percent.
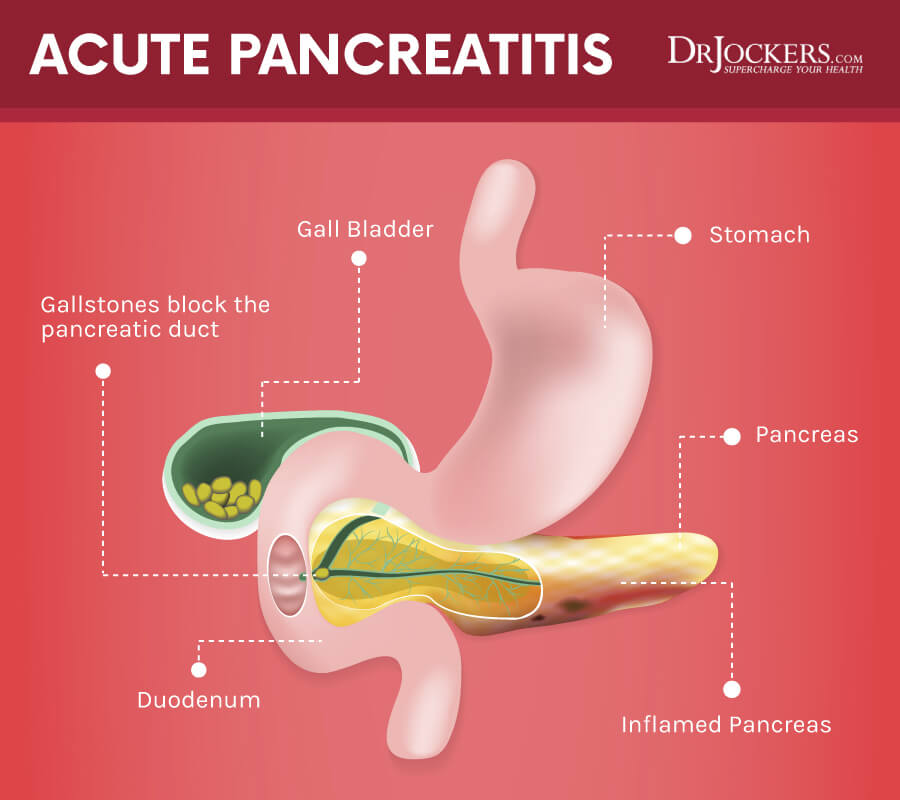
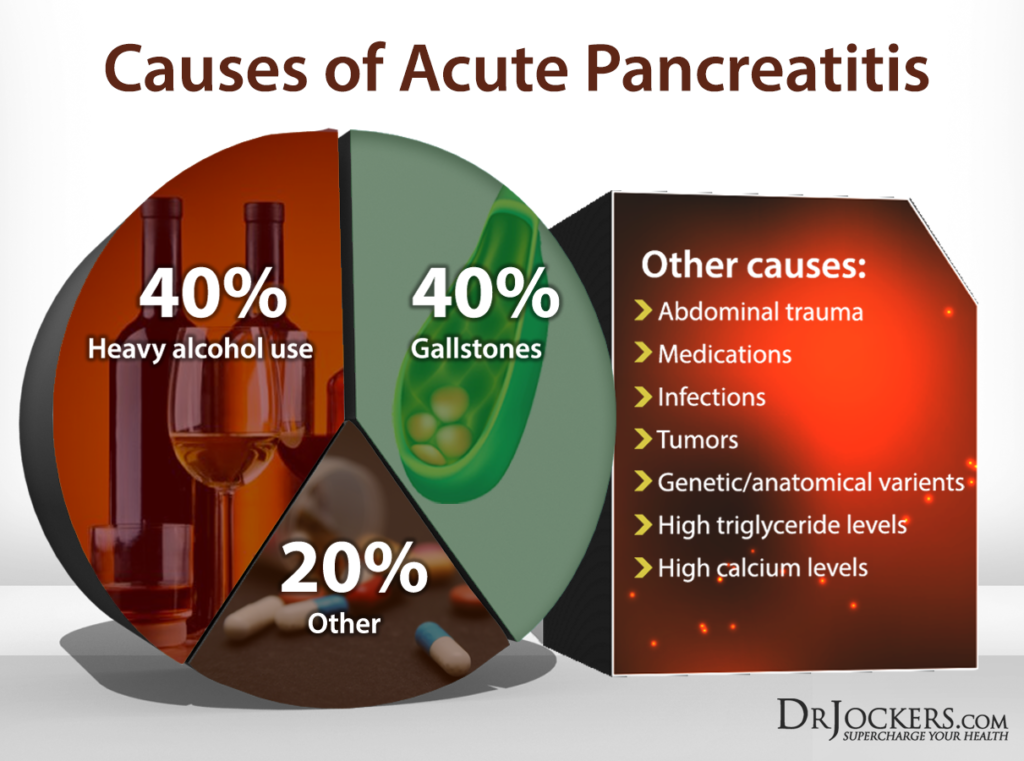
The etiology is not completely clear but alcoholism and gallstones are the primary risk factors for acute pancreatitis, but there are still 20 percent of cases where the cause is unclear. Gallstones can obstruct the pancreatic duct or cause bile reflux, which can activate enzymes in the pancreatic duct system and cause auto digestion, inflammation, swelling, and pain in the pancreas.
Alcohol causes the duodenum of the small intestines to become edematous, or retain water. This causes an increase in pressure and spasm of the sphincter of Oddi and this can obstruct pancreatic enzyme flow. In addition, alcohol actually stimulates the production of more pancreatic enzymes so this just adds more pressure and swelling to the connection point of the pancreas and duodenum
Other causes include tissue ischemia related to trauma or surgery, pancreatic tumors, third-trimester of pregnancy, infections, elevated calcium levels, and hyperlipidemia. Medications that have associated with the disorder include thiazide diuretics, estrogen, steroids, salicylates, and NSAIDs (2).
Symptoms of Acute Pancreatitis
- Epigastric pain radiating to the back (often induced by a fatty meal or excessive alcohol intake)
- Nausea and vomiting
- Abdominal distention and rigidity
- Elevated heart rate
- Elevated temperature
Acute pancreatitis is a medical emergency and help should be sought immediately. The damage done by digestive enzymes on the pancreas can quickly escalate into bleeding internally, dying tissue, edema, pressure in the abdominal cavity, congestion and failure of other organs and lactic acidosis.
Treatment for acute pancreatitis is typically eliminating the cause, hydration and reintroducing food once the inflammation has gone away (2).
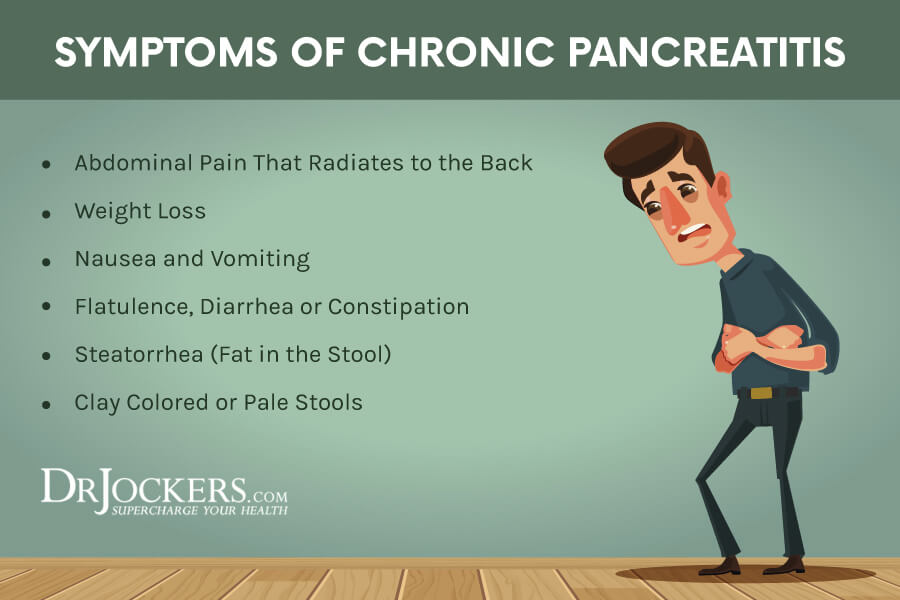
Chronic Pancreatitis
Causes of chronic pancreatitis are less clear because they typically do not have classic manifestations of the disease. However, these patients do suffer from long-term effects such as hormone imbalances, enzyme deficiency, chronic pain, and nutritional imbalances. Common characteristics of chronic pancreatitis include chronic inflammation, fibrosis and dysfunction of pancreatic tissue.
Currently, it is deemed by the medical field as irreversible and will eventually lead to pancreatic insufficiency. Alcoholism and malnutrition are the most common risk factors. Approximately 10-20 percent of cases have no identified cause. A genetic link has been made to a specific gene mutation associated with cystic fibrosis in these cases. Cystic fibrosis patients are likely to develop chronic pancreatitis as well.
When chronic pancreatitis is related to alcoholism, the concentration of insoluble proteins increases in the pancreatic secretions. This results in the calcification of the proteins and plug formation that blocks the pancreatic ducts and the flow of juices (2).
Other cases may be related to a stricture or stone that is blocking pancreatic outflow, which is known as obstructive pancreatitis. Recurrent episodes of inflammation will eventually lead to fibrotic changes to the tissues and loss of exocrine function, which leads to malabsorption and pancreatic insufficiency. When endocrine function is disrupted, diabetes may ensue.
The Problems with Modern Medicine
Treatment for chronic pancreatitis typically evolves around pain management and aiding nutrition absorption. Surgery is also an option.
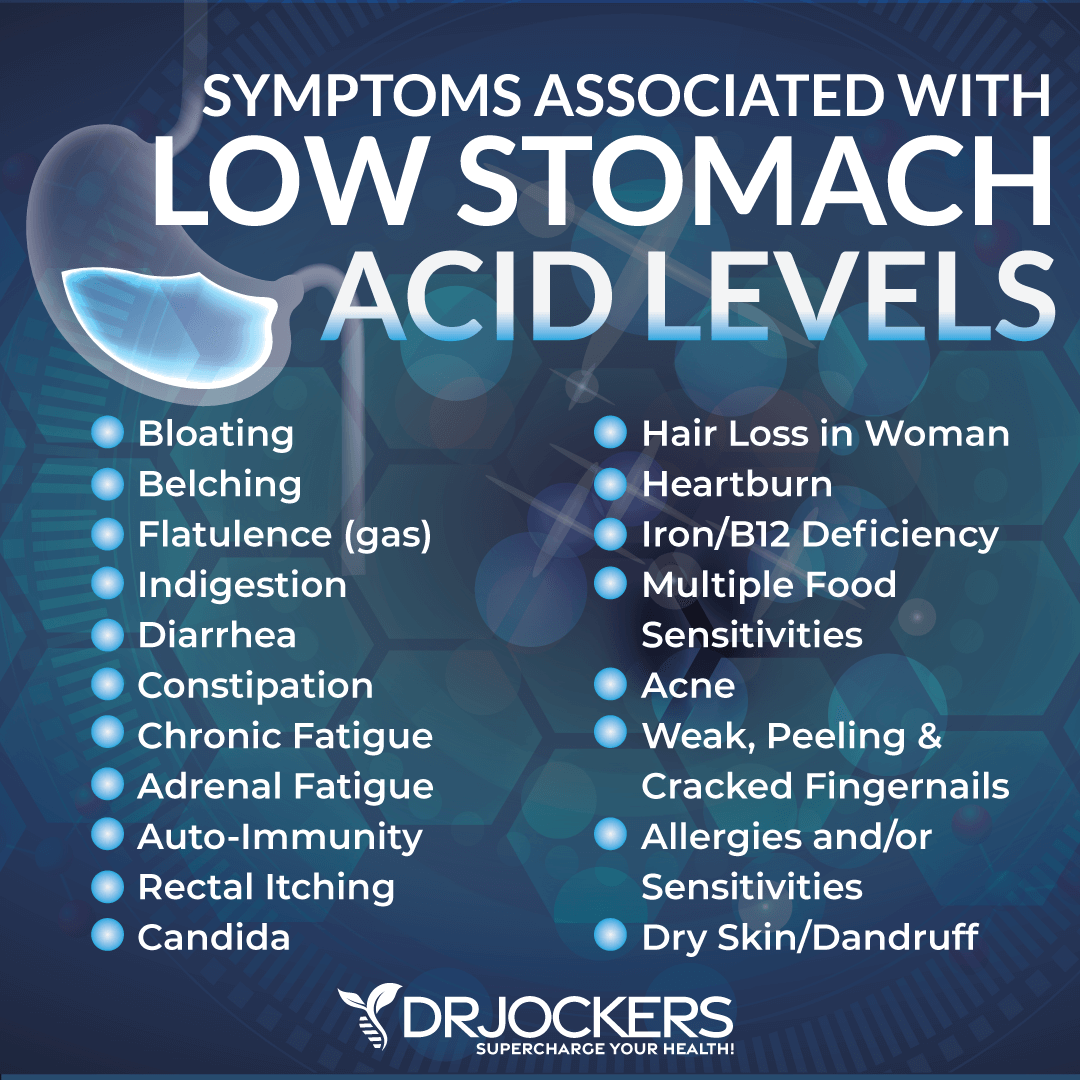
Patients are typically given opioids to control pain, which can worsen constipation. Non-steroidal anti-inflammatory medications (NSAIDs) are very common to give for inflammation. Most people believe NSAIDs are harmless. However, studies show that they damage the stomach lining, which leads to reduced protein absorption and a much greater increase for food allergens and stomach ulcers.
Pancreatic enzyme supplements are usually given to help with absorption. H2- blockers and proton pump inhibitors are typically given to neutralize or decrease gastric secretions, which further worsens the ability for the body to digest and absorb nutrients. This also slows gastric motility and can worsen constipation. This also puts the patient at risk for developing infections due to the sterilizing effects of stomach acid (2).
Low stomach acid levels are associated with increased risk of developing small intestinal bacterial overgrowth (SIBO), Candida overgrowth, B12, iron and zinc deficiencies. In addition, many individuals with low stomach acid develop protein malabsorption and leaky gut syndrome.
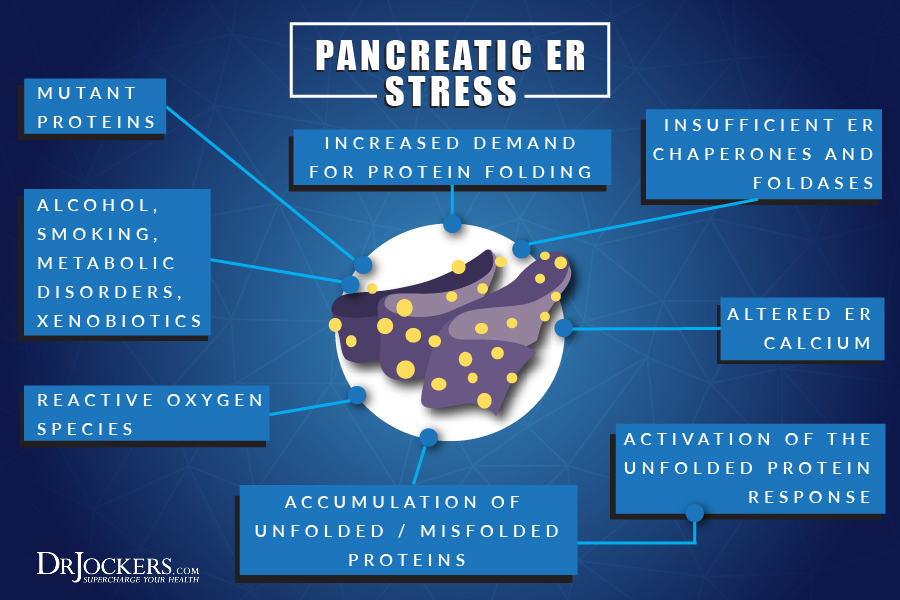
Endoplasmic Reticulum Involvement
There is little research to support the pathogenesis of pancreatitis but a new study has revealed that endoplasmic reticulum stress and calcium signaling could play a big role in this chronic disease. This finding has suggested the need for more research in this area (2). The endoplasmic reticulum is important organelle in human cells that plays a major role in producing, processing, and transporting proteins and lipids.
It produces transmembrane proteins and lipids for its membrane and other cell components such as lysosomes, secretory vesicles, the Golgi apparatus, and the cell membrane. Without this functioning properly, proteins and lipids cannot be transported and processed properly in order to form different structures that are needed. Damage to the endoplasmic reticulum has been found as contributing factor in many chronic diseases and is now recognized as a contributing factor to chronic pancreatitis.
Acute pancreatitis is caused by toxins that induce acinar cell calcium overload, zymogen activation, cytokine release and cell death, yet is without specific drug therapy. Mitochondrial dysfunction has been implicated but the mechanism not established.
Root Causes of Pancreatitis
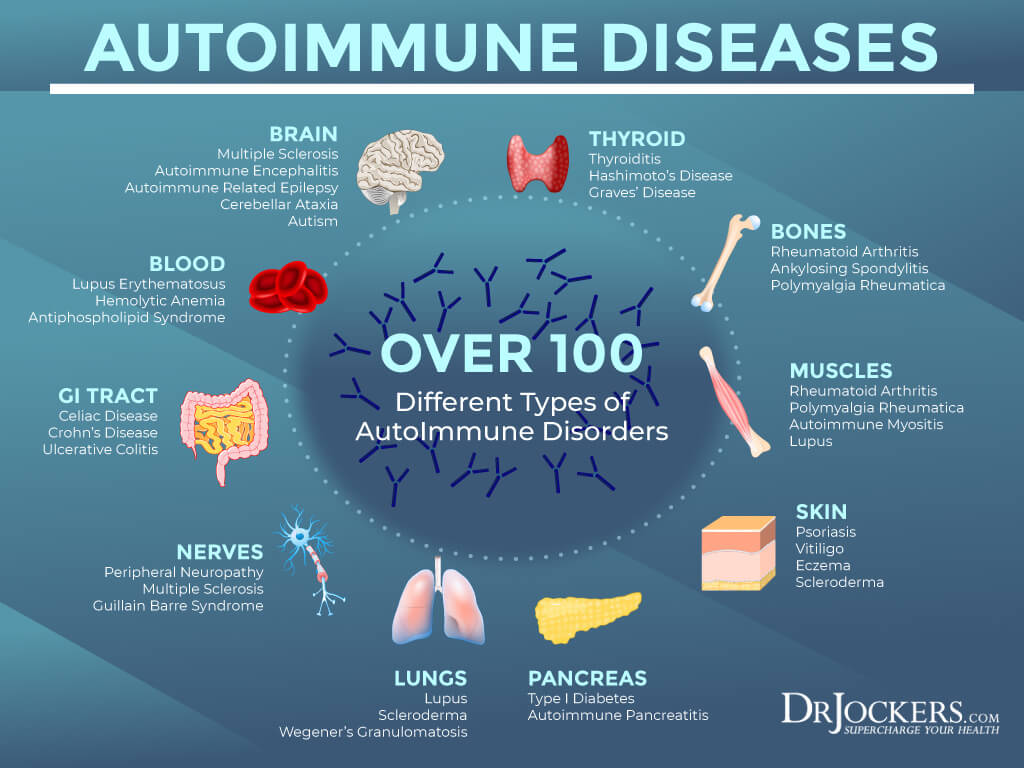
There are several root causes of pancreatitis that you need to be aware of, including autoimmunity, gallstones, alcohol and medications, pancreatic cancer, abdominal surgery or injury, infections, and gut dysbiosis.
Autoimmunity
Autoimmunity means that your immune system is mistakenly attacking its own cell. Autoimmunity may manifest itself as autoimmune pancreatitis. A 2009 article published in the North American Journal of Medical Sciences explains that autoimmune pancreatitis was first introduced as a medical condition with a name in 1995 (3).
There are two types of autoimmune pancreatitis: type 1 and 2. Type 1 affects the pancreas and other organs, including the liver, bile ducts, kidneys, salivary glands, and lymph nodes. It is often mistaken for pancreatic cancer because of its overlapping signs and symptoms. Type two only affects your pancreas and is often linked to irritable bowel disease (IBS).
Besides autoimmune pancreatitis, other autoimmune conditions may also affect pancreatic health and increase your risk of pancreatitis. Lupus, Sjögren’s syndrome, rheumatic arthritis, primary biliary cirrhosis, and primary sclerosing cholangitis (PSC) may also increase your risk or cause pancreatitis.
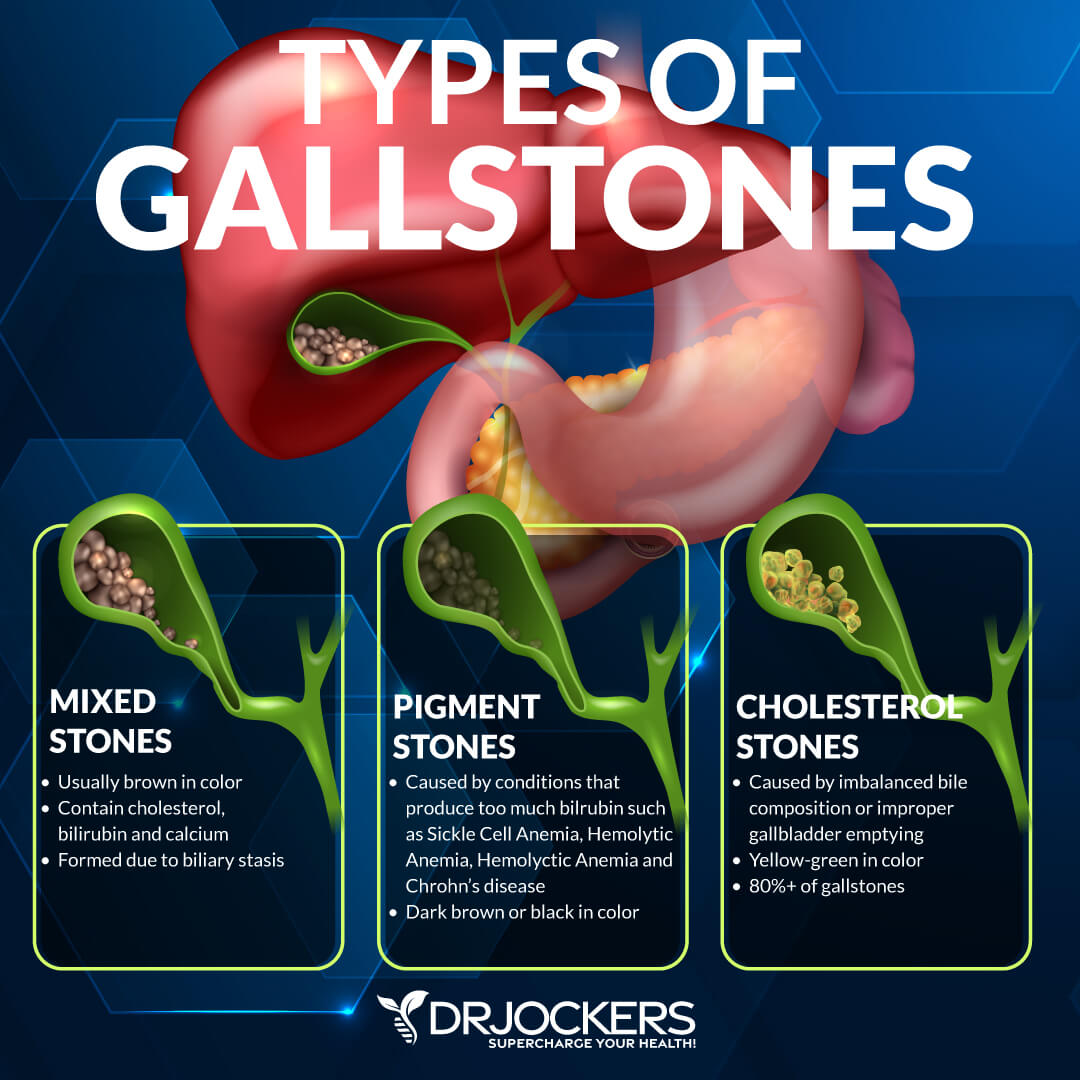
Gallstones
Gallstones are hardened deposits of bile that can form in your gallbladder. They can also increase your risk of pancreatitis. Gallstones pass through the bile duct moving towards the small intestine, but they can get stuck.
You may develop gallstone pancreatitis when the gallstones end up blocking your pancreatic duct. This leads to bile backflow and pancreatic injury. This can cause inflammation, abdominal pain, nausea, vomiting, chills, fever, and jaundice. It is a severe medical issue that can lead to serious complications if left untreated (4).
Alcohol and Medications
Heavy alcohol consumption and alcoholism can cause pancreatitis. According to a 2010 study published in the Journal of Gastroenterology Hepatology, your pancreatic acinar cells are responsible for metabolizing alcohol into toxic byproducts. These byproducts can damage your pancreatic ducts, promote inflammation, and lead to acute or chronic pancreatitis (5).
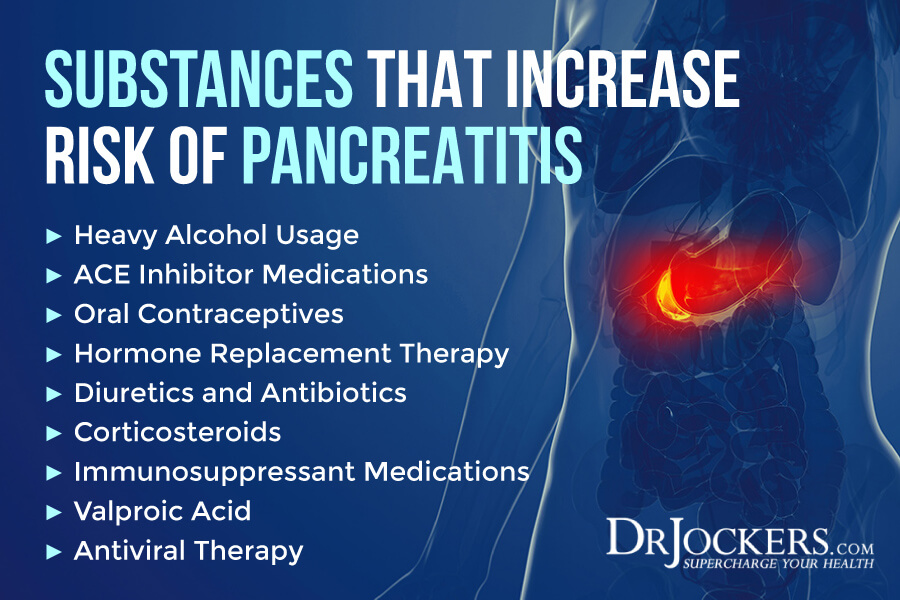
Certain medications can also increase your risk and cause pancreatitis. According to a 2015 review published in The Ochsner Journal, medications are responsible for between 1 and 2 percent of pancreatitis incidents (6).
Angiotensin-converting enzyme (ACE) inhibitors, statins, oral contraceptives, hormone replacement therapy, diuretic, highly active antiretroviral therapy, valproic acid, oral hypoglycemic agents, antibiotics, corticosteroids, immunosuppressant medications, and certain medications for high blood pressure may increase the risk of acute pancreatitis.
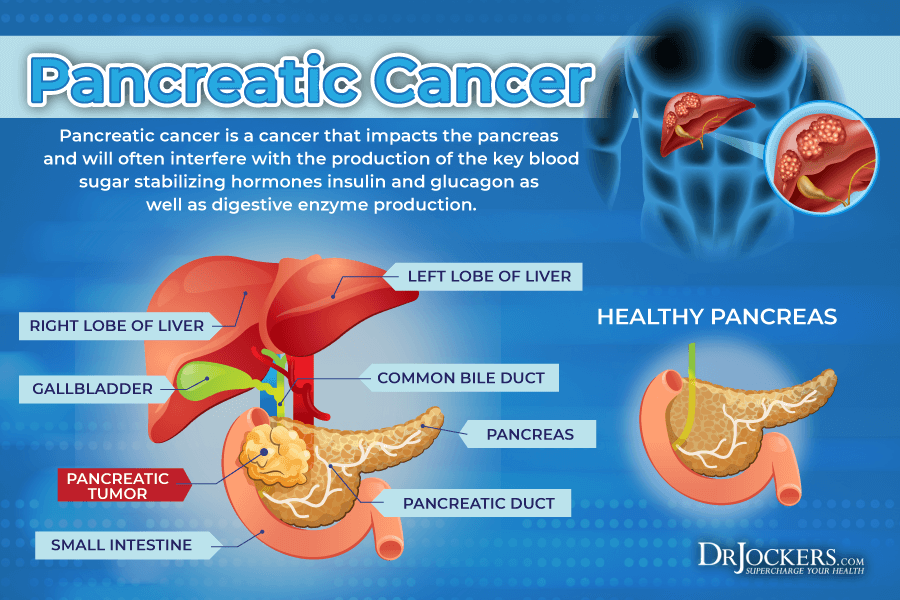
Pancreatic Cancer
Pancreatic cancer is uncontrolled cancerous cell growth that affects your pancreas. According to the American Cancer Society, pancreatic cancer affects about 55,440 people each year, and it is responsible for about 3 percent of all cancers in the United States (7).
It may also result in pancreatitis. According to a 2017 study published by Medicine (Baltimore), acute pancreatitis may be a rare manifestation or early sign of pancreatic cancer (8).
Abdominal Surgery or Injury
Abdominal surgeries or injuries can also result in pancreatitis. According to a 2013 review published in the World Journal of Gastroenterology, pancreatic trauma can result in post-traumatic pancreatitis, which without timely diagnosis and treatment can be fatal (9). A 2018 study published in Academic Forensic Pathology has found that gunshots and stab wounds are responsible for about 20 to 30 percent of pancreatitis cases from penetrating trauma, with firearms being the most common reason (10).
According to a 1961 study published in Archives in Surgery, infections, anesthesia, hemorrhage, and faulty surgical techniques can increase the risk of postoperative acute pancreatitis (11). A 2000 study published in The Journal of the American College of Surgeons has found that though it’s rare, acute pancreatitis may develop after abdominal vascular surgery (12).
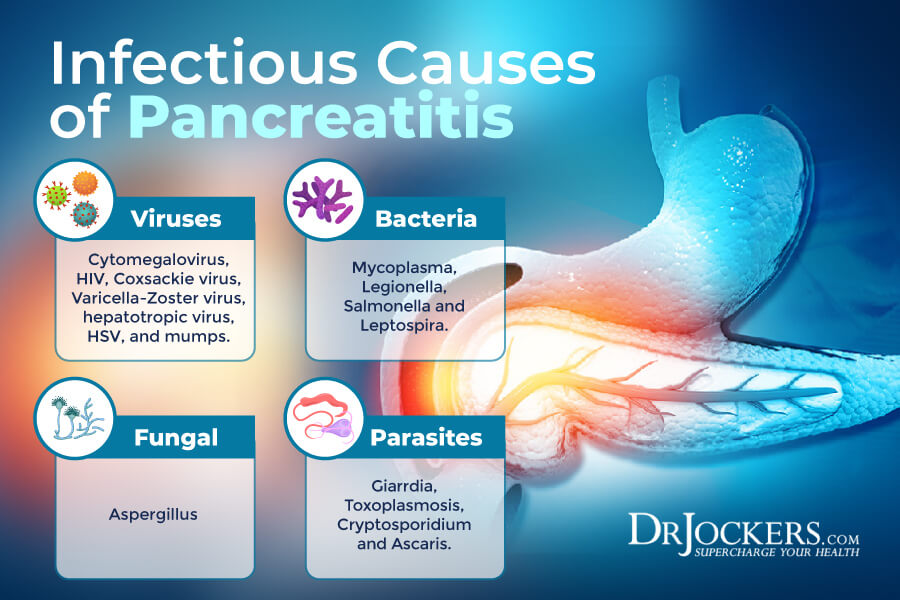
Infections
Viral and parasitic infections may also increase the risk of pancreatitis. According to a 2017 review published in Gastroenterology Research, in the 10 percent of acute pancreatitis cases, microorganisms and infections are the cause (13).
According to the researchers, the most common pathogens that may cause acute pancreatitis include “viruses (hepatotropic virus, Coxsackie virus, cytomegalovirus (CMV), human immunodeficiency virus (HIV), herpes simplex virus (HSV), mumps, varicella-zoster virus, and other viruses); bacteria (mycoplasma, legionella, salmonella, and leptospira); fungi (aspergillus); and parasites (toxoplasmosis, cryptosporidium, and ascaris)” (13).
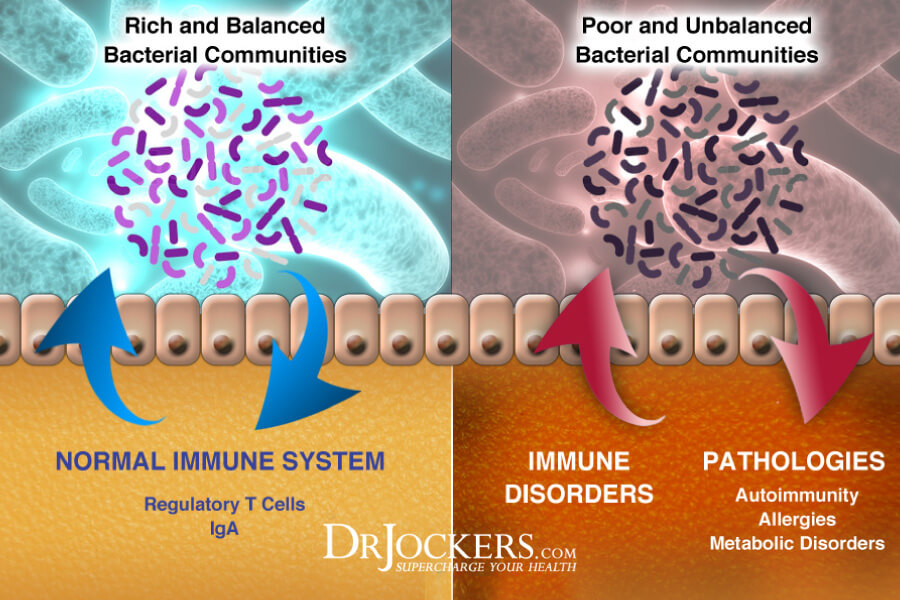
Gut Dysbiosis
Gut dysbiosis means that your microbiome is out of balance and there are too many bad bacteria and too few beneficial bacteria in your gut. Gut dysbiosis can increase the risk of chronic inflammation, digestive complaints, and all kinds of acute and chronic health issues, including pancreatitis.
A 2015 study published in Pancreas has found that gut dysbiosis can increase inflammation which can result in the progression of acute pancreatitis (14). A 2021 review published in Frontiers in Immunology has also found that gut dysbiosis can lead to chronic pancreatic inflammation and autoimmune pancreatitis (15).
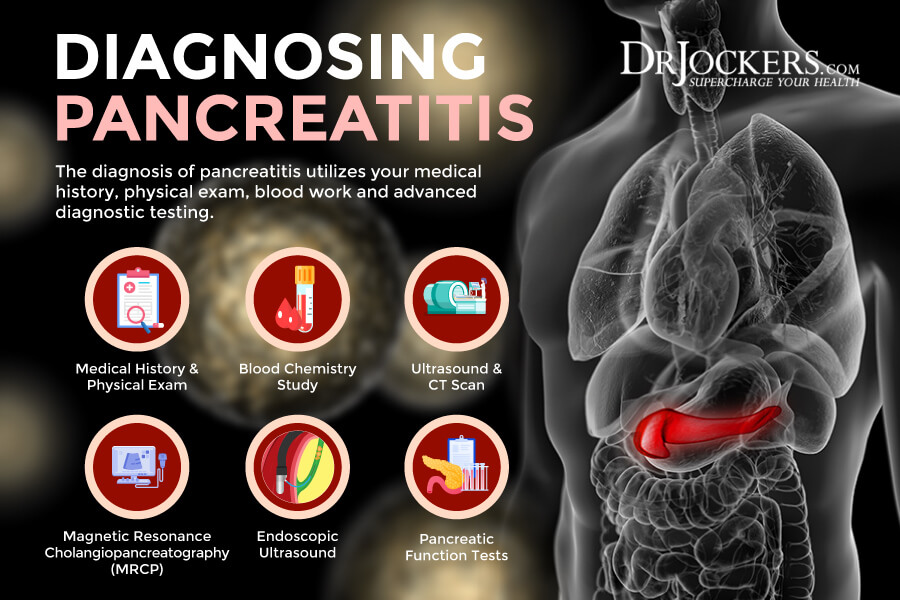
Diagnosis Pancreatitis
To diagnose pancreatitis, your doctor will go over your medical and family history, including medications you may be taking. They will ask about your symptoms, perform a physical exam, and check for abdominal pain and tenderness (16).
If there is a concern for pancreatitis or other issues, they may order some lab tests and diagnostic imaging, including (16):
- Blood test for high blood glucose
- Blood test for high amylase and lipase levels, which are digestive enzymes created by your pancreas
- Blood tests for lipid or blood fat levels
- Blood tests for inflammation levels, including inflammation of the pancreas, gallbladder, bile ducts, and liver
- Blood test to check for signs of pancreatic cancer
- Stool samples to check for fat malabsorption
- Ultrasound to look for gallstones
- Computer tomography (CT) scan to check for pancreatitis or pancreatic cancer
- Magnetic resonance cholangiopancreatography (MRCP) to look at your pancreas, bile ducts, and gallbladder checking for causes of pancreatitis
- Endoscopic ultrasound (EUS) to look at your pancreas and bile ducts for abnormalities
- Pancreatic Function Test (PFT) to see how well your pancreas respond to a hormone created by your small intestine, called secretin.
 Conventional Treatment Options
Conventional Treatment Options
Treatment for acute or chronic pancreatitis may involve intravenous (IV) fluid for dehydration, pain medication and antibiotics (IV or by mouth), a low-fat diet, or in more severe cases, nutrition through IV or a feeding tube (17).
In many cases, acute pancreatitis is mild and can resolve with the help of treatment within a few days. In more severe cases, it may require more serious treatments, including (17):
- Cholecystectomy surgery may be used to remove the gallbladder if the reason behind your acute pancreatitis is gallstones.
- If there is an abscess or infected, painful, or bleeding pseudocyst, your doctor will drain fluid from your abdomen to reduce symptoms. They may also remove any damaged areas of your pancreas.
- Endoscopic cholangiopancreatography (ERCP) may be used to take care of any narrowing or blockage in your pancreatic or bile duct.
Chronic pancreatitis can be more complex to treat. It may include lifestyle changes, supplements, and other options. Your doctor may recommend (17):
- Medicines and digestive enzymes can support digestion and address the malabsorption of vitamins. If you have malabsorption difficulties, vitamin A, D, E, K, as well as, vitamin B12 shots may be recommended.
- Chronic pancreatitis can increase your risk of diabetes. If you develop diabetes, an eating plan for diabetes, blood glucose monitoring, regular check-ups, and in some cases, medication will be recommended.
- Surgery may be recommended to relieve any pressure or address any blockage in the pancreatic duct or to remove the affected area of your pancreas. In some cases, the entire pancreas will need to be removed followed by islet auto-transplantation. Normally, your pancreas creates insulin. However, after this surgery, doctors transplant islets from your pancreas to your liver. This way, the islets can still create insulin.
- In some cases, nerve block shots may be recommended to numb the nerves that carry pain messages from your pancreas. This may help to break up and remove any gallstones.
Furthermore, your doctor will likely recommend to stop drinking alcohol, stop smoking, and lose weight if you are overweight or obese. Removing alcohol and cigarettes can reduce pancreatitis, reduce the risk of chronic pancreatitis, and improve the symptoms of chronic pancreatitis. Weight loss and maintaining a healthy weight can reduce the risk of gallstones and support pancreatic function (17).
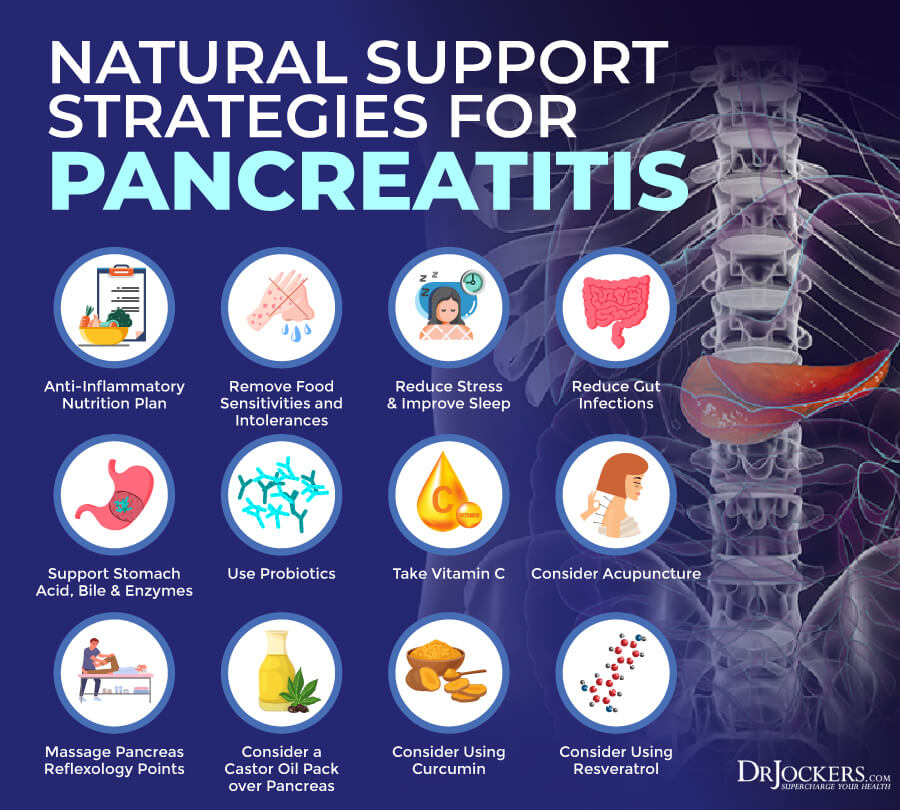
Natural Support Strategies
You may improve your health and reduce your risks and symptoms of pancreatitis with the help of some simple natural support strategies. Here is what I recommend:
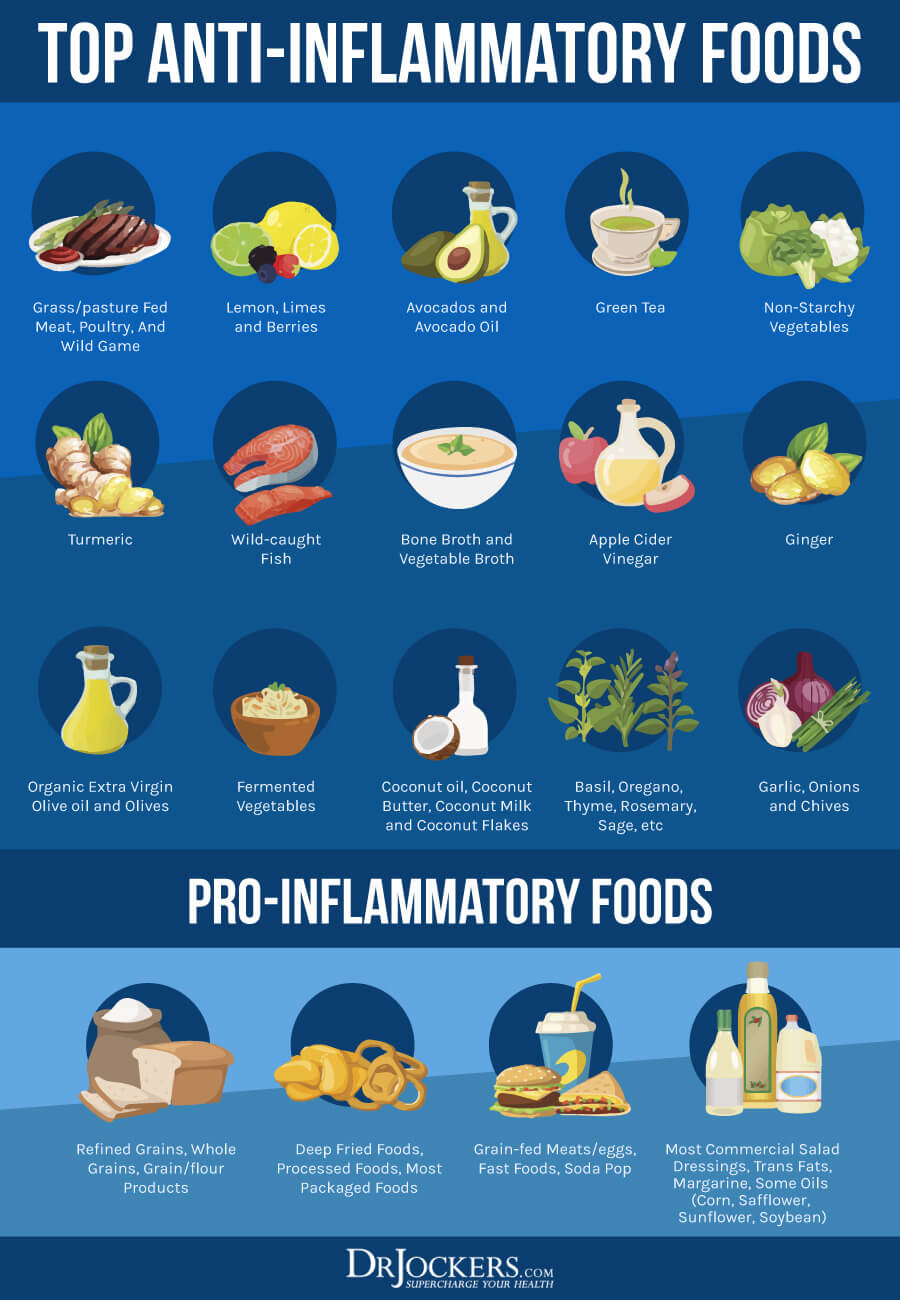
Anti-Inflammatory Nutrition Plan
Pancreatitis is driven by inflammation. An anti-inflammatory nutrition plan can help to improve chronic pancreatitis and reduce the risk of acute pancreatitis. I recommend that you remove any inflammatory foods from your diet, including refined sugar, refined oils, artificial ingredients, additives, deep-fried foods, junk food, and highly processed foods.
Eating a low-salt and low-fat vegetarian diet has been shown to decrease painful attacks (18). However, this does not provide the beneficial nutrients of fats and proteins and would leave the patient malnourished. Fats are a vital part of our diets for blood sugar stabilization, decreased disease, hormone production, cell production and protection, decreased inflammation, and overall function. A diet without quality fats is detrimental to our health.
A 2018 review published in Frontiers in Immunology has found that healthy nutrition and omega-3 fatty acids, probiotics, glutamine, and vitamins A, C, E, and D may help to reduce the risk of acute pancreatitis and its complications (19). I recommend eating lots of greens, vegetables, herbs, low-glycemic index fruits, fermented foods, grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game. I recommend consuming healthy fats, including avocadoes, olives, olive oil, coconut oil, pasture-raised butter and ghee, wild-caught fatty fish, nuts, and seeds.
Remove Food Sensitivities and Intolerances
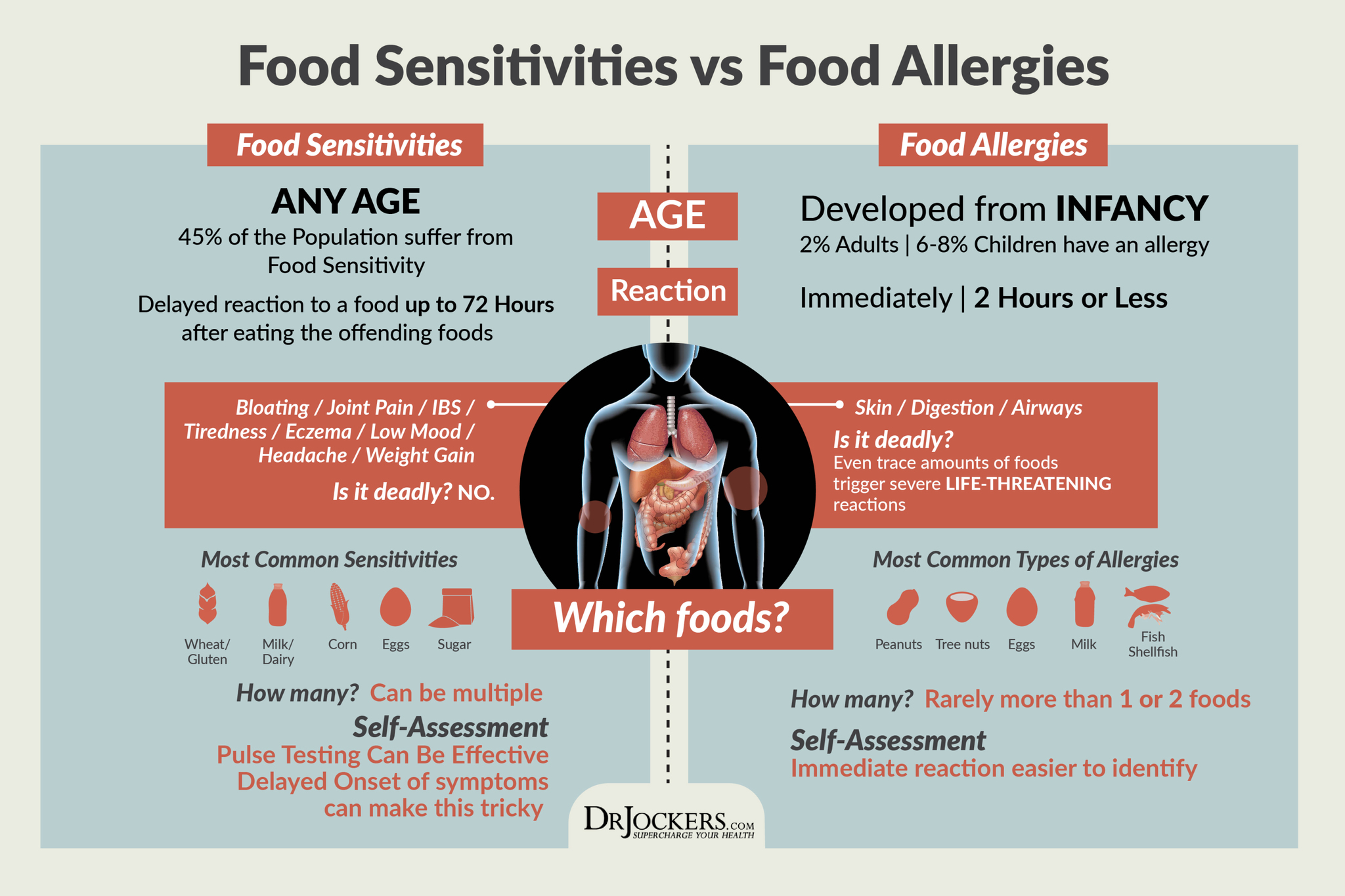
Food sensitivities and food intolerances can cause chronic inflammation and increase your risk of pancreatitis. According to a 2017 study published in Digestive Disease and Sciences, certain foods, especially milk, eggs, mustard, fish, bananas, and kiwi can trigger acute pancreatitis (20). Food sensitivities and intolerances can also cause or worsen symptoms of chronic pancreatitis.
Common food sensitivities include gluten, dairy, soy, corn, shellfish, fish, wheat, tree nuts, and sugar. However, you can be sensitive to any food, including those that may be healthy for most people. I recommend figuring out your food intolerances.
Blood tests can be a good place to start, however, they cannot test for all foods and false results are common. Muscle response and pulse testing can help you find some further answers by tapping into your body’s wisdom. An elimination diet is possibly the best method to find all your sensitivities and triggers. You can find information on all these methods by searching my website.
Once you find your food sensitivities and intolerances, I recommend that you remove these foods from your diet. Since food sensitivities can change over time, I recommend performing these tests every year or if new symptoms or health issues occur.
Reduce Stress and Improve Sleep
Chronic stress and poor sleep can increase chronic inflammation, which can increase your risk of all kinds of health issues, including pancreatitis. A 2014 study published in the World Journal of Gastroenterology has found that chronic physical or mental stress or a combination of both can contribute to acute pancreatitis (21). Another 2014 study published in Aging Cell has found that sleep deprivation can negatively impact pancreatic health (22). Reducing chronic stress and improving your sleep is, therefore, critical for pancreatic health and function.
Reduce stressful activities and situations in your life as much as possible. For example, instead of checking the news or scrolling social media all day long, designate one specific time for this during the day. Unfollow social media accounts, blogs, and other sources that increase your stress and don’t add anything to your life. Learn to respond to stress better. Practice gratitude, mindfulness, positive thinking, and kindness.
Meditation, breathwork, guided relaxation, visualization, prayer, and spiritual practices are great tools to center yourself, relax your body, and calm your mind. Journaling can help to release any frustration on paper, spot any cognitive patterns you may want to change and reflect. Coloring, crocheting, arts, and crafts can help to relax and calm your mind.
Reducing stress throughout the day is critical for restful sleep. However, there are some strategies that you can use to wind down in the evening and sleep better. Avoid alcohol, sugar, caffeine, and heavy foods in the evening. Use blue-light blocking glasses when using electronics and avoid electronics altogether at least two hours before bedtime.
Engage in relaxing activities, such as taking a healing bath, sipping on herbal tea, reading, coloring, doing crossword puzzles, engaging in calm conversations and family time, reflecting on the day, or spiritual practices. Invest in a supportive bed, mattress, bedding, and pillows. Try blackout curtains and eye masks to support your sleep.

Reduce Gut Infections
A 2017 review published in Gastroenterology Research, in the 10 percent of acute pancreatitis cases, gut infections are the cause (13). These gut infections may include viral, bacterial, fungal, and parasitic infections. Eating a healthy, anti-inflammatory, and gut-friendly diet is absolutely critical. Supporting your microbiome with fermented foods and probiotics improves your gut health (19).
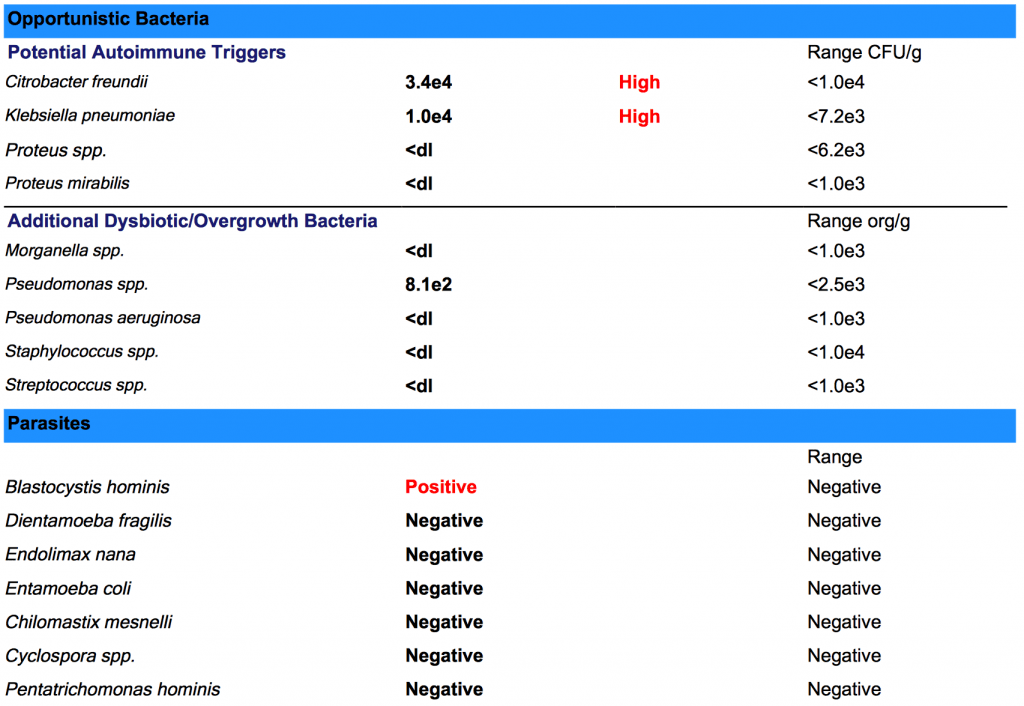
In addition to a gut-friendly diet and probiotics, supplementation for your specific gut infections may be beneficial. I recommend testing for gut infections with a GI Map Stool Test or another high-quality stool testing that can help to identify what underlying gut infections may be causing your health issues.
Mimosa pudica seed is a great option for parasites. Oregano oil, garlic, olive leaf extract, Pau d’arco, berberine, and grapefruit seeds extracts are some other herbs that help to reduce and remove gut infections. I recommend that you work with a functional medicine professional who can guide you with a personalized protocol. My team and I would be happy to support your journey. To learn more about the GI-MAP™ DNA Stool Analysis, click here.
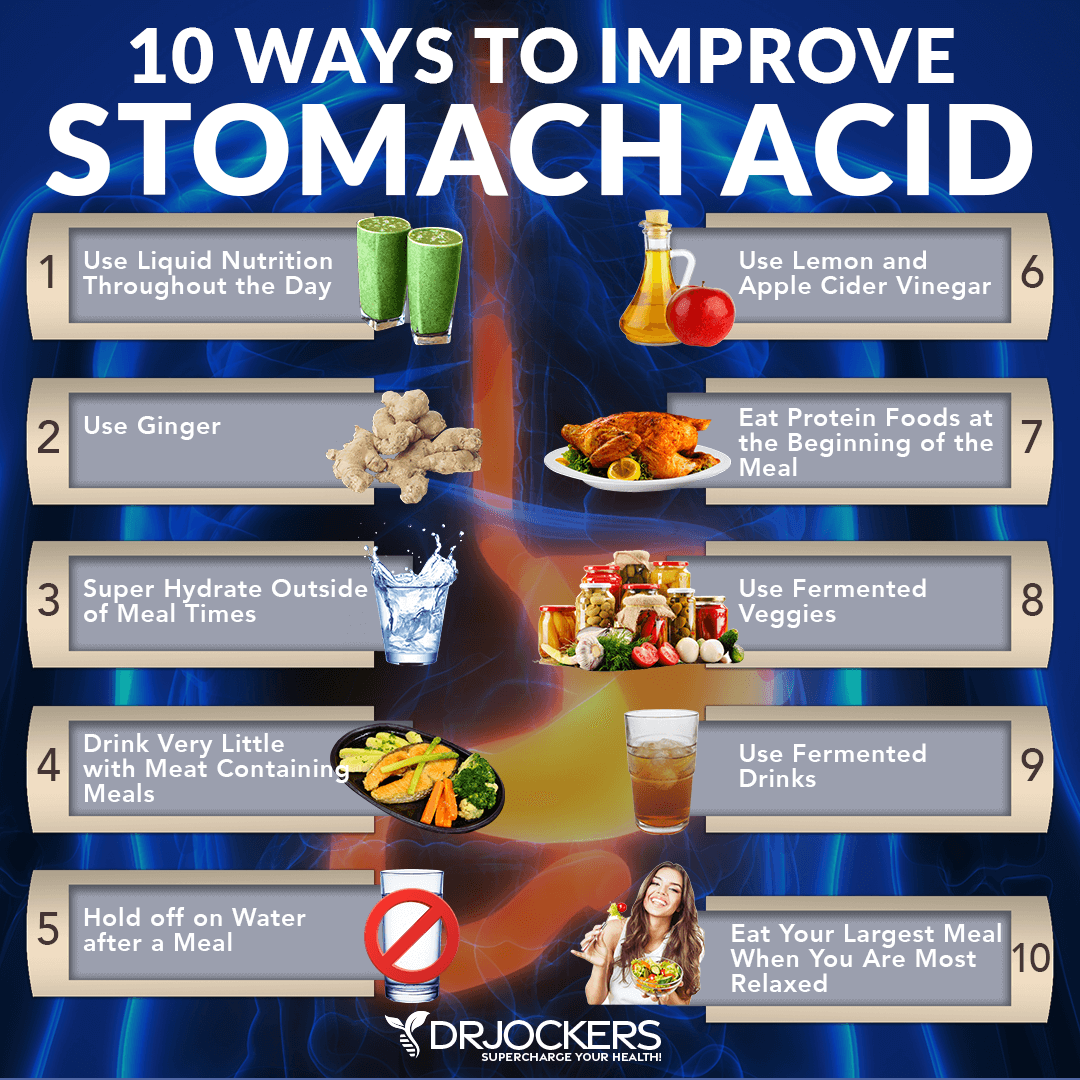
Support Stomach Acid, Bile & Digestive Enzymes
You may also benefit from supporting your stomach acid levels and bile flow, and taking digestive enzymes. According to a 2000 study published in the British Journal of Clinical Pharmacology, acid-suppressing medications can increase the risk of acute pancreatitis (23). As a 2009 study published in the Saudi Journal of Gastroenterology explains, blockage in the bile duct by gallstones may cause acute biliary pancreatitis (24).
Pancreatitis can often cause malabsorption and malnutrition and these issues can also cause or further trigger pancreatitis making vitamin supplementation often necessary (19). A 2016 study published in Current Drug Metabolism has found that using pancreatic enzymes may help to improve pancreatitis (25).
To support your stomach acid levels, I recommend the following:
- Use Liquid Nutrition Throughout the Day: Try to make sure that at least half of your meals are in a liquid form, such as a protein shake or green smoothie. Protein shakes are pre-metabolized and very easy to digest and do not depend upon HCL production. If you have low HCL, it may be helpful to drink one to two protein shakes daily to support amino acid absorption, reduce extra stress on your digestion, and support healthy stomach acid levels.
- Use Ginger: Ginger is one of the best things for improving digestive juices. I recommend drinking 2 to 3 cups of ginger tea each day. You can put ginger essential oil in water (2 to 3 drops in 8 oz of water), juice a ½ inch of fresh ginger root in a green juice each day, and use ground ginger on your foods. You can also add fermented ginger to your diet, which is common in Asian dishes such as kimchi.
- Super Hydrate Outside of Meal Times: Good hydration can help activate bowel motility and push contents through the digestive system, which will reduce microbial fermentation and toxicity in the body. This can help to support your stomach acid levels.
- Drink Very Little With Meat Containing Meals: When you are eating meat or any sort of heavier food, you should stop drinking water or other liquids at least 30 minutes before the meal, except if you need to take a supplement with 2 ounces of water. Holding off water during these meals will reduce any potential dilution of the gastric juices and allow for better digestion.
- Hold Off On Water After a Meal: To allow for optimal digestion, I also recommend not drinking water or other liquids until at least 30 minutes after a meal. This allows for proper stomach acid activity, sterilization, and protein metabolism.
- Use Lemon and Apple Cider Vinegar: Squeezing fresh lemon or using lemon juice or apple cider vinegar on your meat and vegetables helps to pre-metabolize the food and support better digestion and nutrient absorption. You can either marinate foods in a lemon or ACV base or just add them as a dressing right before consuming them.
- Eat Protein Foods at the Beginning of the Meal: The stomach will begin churning out its stomach acid when you start eating, especially when consuming protein. While it’s culturally common to eat a salad before their protein dish, this is not great for your HCL production. It is a much better idea to eat your protein with the salad or vegetables instead of after.
- Use Fermented Veggies: Fermented foods such as sauerkraut, kimchi, pickles, pickled ginger, and other fermented vegetables all contain organic acids, enzymes, and probiotics which help to improve digestive juice secretions. I recommend using one of these with all of your heavier meals and especially any meal with protein.
- Use Fermented Drinks: Fermented drinks such as apple cider vinegar, coconut kefir, and kombucha offer anti-microbial benefits and help to reduce the bacterial load, especially the bacteria in the stomach such as H Pylori. Keeping H Pylori levels down is critical for the body to be able to produce enough stomach acid.
- Eat Your Largest Meal When You Are Most Relaxed: Your body needs to activate the parasympathetic nervous system to produce enough stomach acids. If you are busy and on the go, you will be in fight or flight sympathetic mode. If you struggle with low stomach acid, this fight or flight state will not allow your body to produce anywhere near enough. Relaxing before the meal is important to improve stomach acid production.
To support bile flow, gallbladder health, and live function I recommend using the following foods and herbs: apple cider vinegar (ACV), artichokes, lemon, lime, parsley, cucumber, celery, mint cilantro, radishes, milk thistle, dandelion greens, turmeric, ginger, sauerkraut, green tea.
Additionally, you may benefit from a kidney and liver support herbal supplement, activated coconut charcoal for detoxification, and a bile flow support supplement with dandelion, guggul extract, choline, taurine, and methionine. Moreover, I also recommend taking digestive enzymes with every meal to support digestion and absorption.
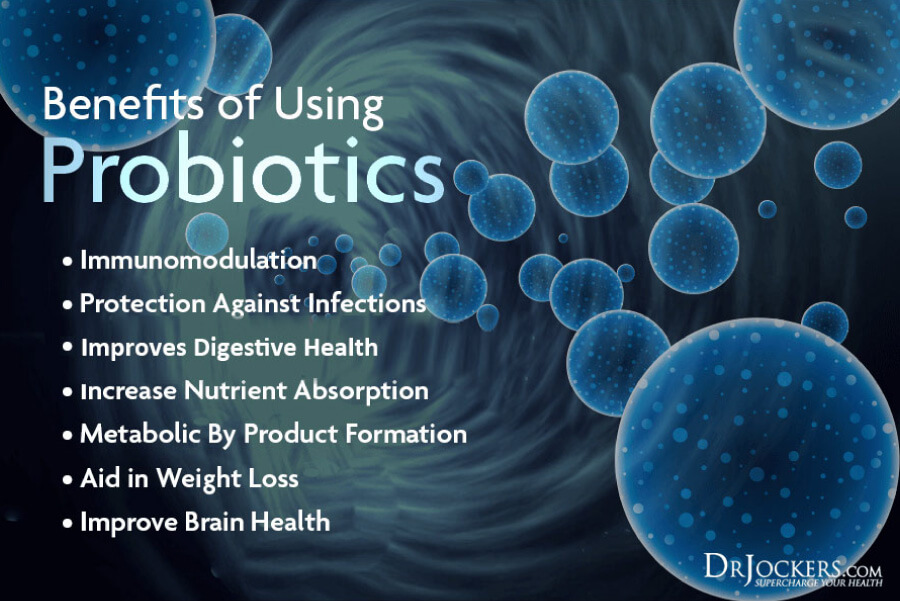
Use Probiotics
Gut dysbiosis is one of the main possible causes of pancreatitis (14,5). Taking probiotics may help to improve your microbiome thus support your pancreatic health as well. A 2008 study published in the American Journal of Physiology, Gastrointestinal and Liver Physiology has found that taking probiotics can reduce oxidative stress and support pancreatic glutathione biosynthesis in acute pancreatitis (26). A 2021 randomized, double-blind, placebo-controlled trial has also found that probiotics may help to reduce the length of hospital stay in acute pancreatitis patients (27).
To support your pancreatic health, I recommend that you eat probiotic-rich fermented foods, including sauerkraut, fermented vegetables, kimchi, pickles, coconut kefir, and kombucha. Even more importantly, I recommend that you take a high-quality daily probiotic supplement.
Take Vitamin C
Vitamin C is an important vitamin that is critical for your immune system. People with pancreatitis often struggle with malabsorption of nutrients and vitamin deficiencies (19). They may benefit from supplementation, including vitamin C supplementation.
A 2003 study published in the World Journal of Gastroenterology, taking a high-quality, high-dose vitamin C intravenously for 5 days can improve acute pancreatitis (28). To support your pancreas, I recommend eating foods rich in vitamin C, including lemon, lime, other citrus, strawberries, black currants, peppers, Brussels sprout, and broccoli.

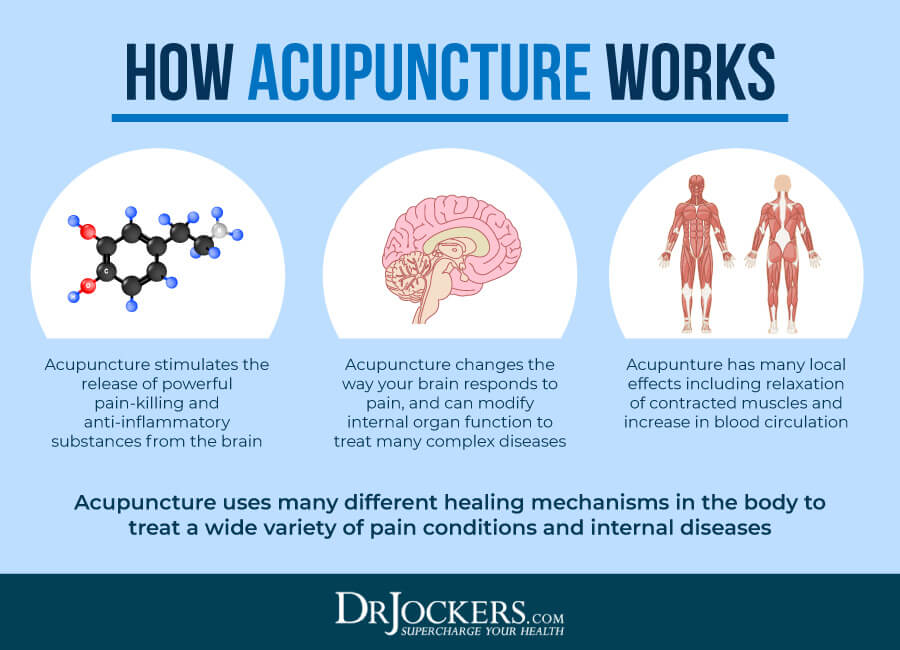
Consider Acupuncture
Acupuncture is a form of alternative medicine and part of Traditional Chinese Medicine (TCM). It uses thin needles on specific points of your body to recreate healthy energy flow within your body, reduce symptoms, and improve your health.
According to a 2017 randomized controlled trial, acupuncture may help to reduce pain in patients with chronic pancreatitis (29). A 2019 systematic review and meta-analysis has found that acupuncture may also benefit acute pancreatitis patients (30). If you are dealing with pancreatitis, you may benefit from seeing an acupuncture clinic.
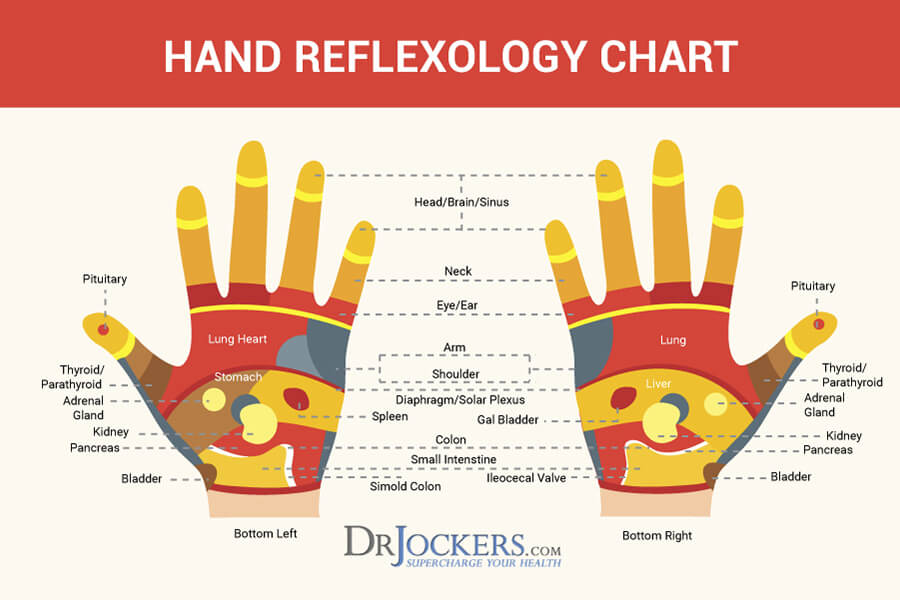
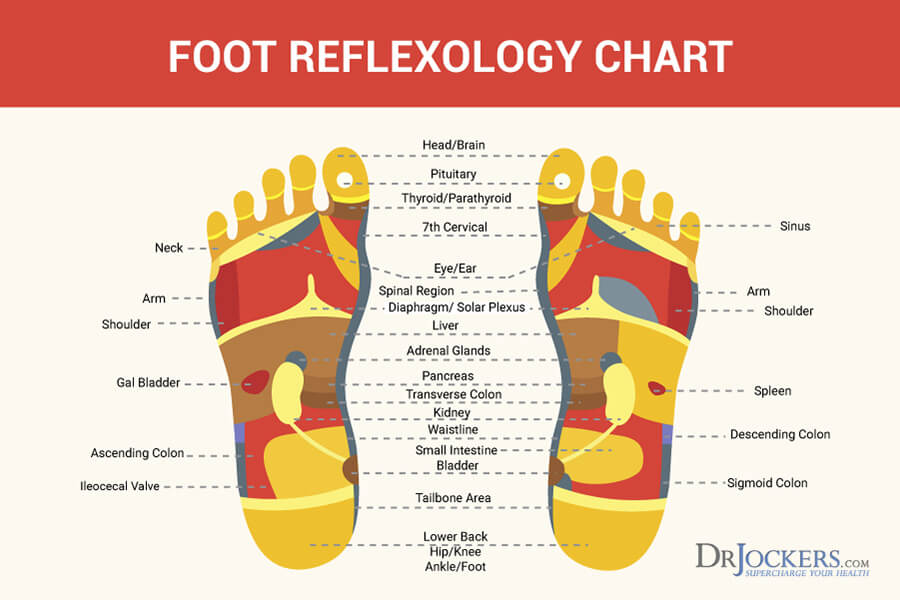
Massage Pancreas Reflexology Points
Reflexology uses specific points in your feet and hands only that correlate with certain organs in your body. According to a 2015 paper published in the Journal of Traditional and Complementary Medicine, reflexology may be beneficial for chronic health conditions and may help to support your overall health and wellness (31).
You may also perform this yourself. You may benefit from massaging pancreas reflexology. Reflexology points for your pancreas are located on the outside section of the middle of your arch and the lower section of the middle of your hands.
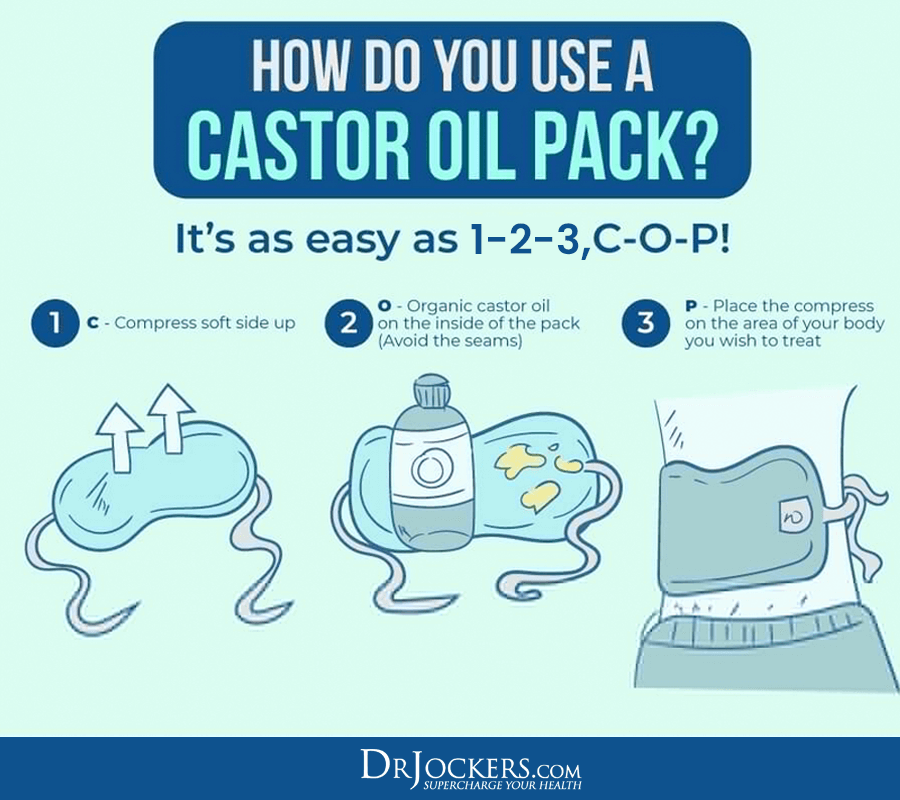
Consider Using a Castor Oil Pack Over Pancreas
Castor oil has been used for a long-time to help to detoxify the body. Castor oil packs are often used for liver detoxification. However, if you have pancreatitis, using castor oil packs may also feel good and improve your symptoms. All you need is a bottle of castor oil, a 12 by 12-inch wool cloth, a clear plastic wrap, a dish towel, and a hot water bottle.
Squirt some castor oil on the wool cloth until it’s soaked through but not dripping wet. Microwave the cloth for about 30 seconds. It can get very hot very quickly, so make sure not to overheat it. Wrap the castor oil cloth with some clear plastic wrap.
Apply this castor oil pack over your pancreas where your pain is, place a dish towel over it. To keep it warm, place a warm water bottle over it. Leave the castor oil pack on for 30 to 60 minutes. Repeat this daily.
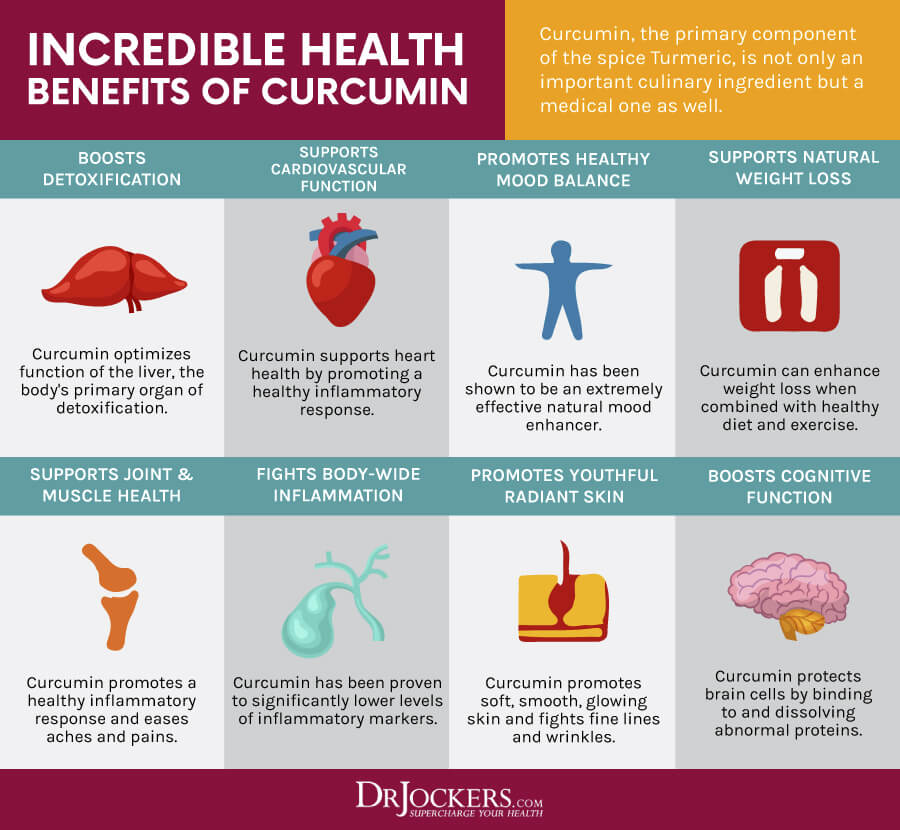
Consider Using Curcumin
Curcumin is the active compound of the spice, turmeric. Turmeric is well-research for its anti-inflammatory properties that may also benefit your pancreatic health. According to a 2018 study, curcumin may help to reduce inflammation in severe acute pancreatitis cases (32). A 2019 study published in Molecular Medicine Reports has also found that curcumin may support pancreatic health and benefit those with acute pancreatitis (33).
I recommend that you take a curcumin supplement daily. Additionally, I also recommend using turmeric regularly in your cooking, including your curries, soups, vegetable dishes, dressings, smoothies, and juices.
Consider Using Resveratrol
Resveratrol is a polyphenol found in the skin of red grapes, berries, pistachio, and cacao. It offers anti-inflammatory and antioxidant properties that may benefit your pancreatic health. A 2018 study published in Molecular Nutrition & Food Nutrition has found that resveratrol may be a potentially effective therapeutic agent for chronic pancreatitis (34). According to a 2021 comprehensive review published in Biomedicine and Pharmacotherapy, resveratrol may offer some antioxidant and anti-inflammatory benefits for acute pancreatitis (35).
I recommend eating foods rich in resveratrol and taking a daily resveratrol supplement. You can find supplements for inflammation that include both resveratrol and curcumin.

Final Thoughts
Pancreatitis can be a debilitating condition that results in overwhelming pain and malnutrition. Treatment often involves medication, dietary restrictions, and often even surgery. Yet, there are natural support strategies that can support your pancreatic and overall health. I recommend that you follow the natural support strategies outlined in this article to improve your health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and thrive in life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!




Please if you have lists of food or beverages to avoid I would love to see them . I am recuperating form a severe bout of pancreatitis and need gallbladder removable .
Hey Joyce, so sorry to hear this! I would recommend sticking with liquid foods – vegetable juices, fermented drinks like coconut water kefir and protein shakes with coconut milk and a healthy protein powder.
Thank you for great article, if you please clarify, liquid fast – can it be BLENDED , NOT JUICED, greens /kale, parsley, cilantro, lemon, OR fiber is not beneficial in this case
Good question All. It can be a little of both!
Did you have your gallbladder out then? Just curious if you know what your triglycerides were at the time of the pancreatitis?
so for chronic pancreatitis what would be recomended
Yes, follow the steps in this article Omar!
Do you know what your triglycerides are at the times of pancreatitis?
mine can run up to 2500 when I have an attack. it is painful
Interesting info about pancreatitis. I’m actually concerned I’m going through a bout as I text. I had it 10 years ago & had my gallbladder removed. I do not drink at all so that’s not an issue. I’ve had double hip replacements and am on heavy opiates that I don’t take as prescribed (I take less) 10mg oxycodone 4x daily 20mg OxyContin 2x daily. I’ve had 2&1/2 electrolyte drinks and 7 saltines in 2&1/2 days I’m getting worried but starting to feel human.
Sorry to hear this Kathy. Strong medications such as what you are taking can cause this!
I had my gall bladder remobed one year ago. I believe I am suffering from Sphincter of Oddi Dysfunction. Is this the protocol I should follow? I have also looked into the FODMAPS diet, and using mineral salts to alkalize the bile. What are your thoughts? Thank you.
Hey Brianna, I am so sorry to hear about this! Yes, I would recommend following this protocol in the article. You can also see if you are having trouble with the higher FODMAP foods and doing mineral salts is a very good idea!
Dear Dr. Jockeys, you don’t mention the enzymes essential for metabolizing meat and dairy. I consume raw milk kefir and grass fed organic meat. Does your product work in digesting these?
Glenda,
Yes SuperDZYME will help in digesting both of those. It is going to be mainly protease and lactase that will be responsible for breaking meat and dairy down but there are others that are involved. It provides very thorough digestive support for different types of foods.
Hi I would like to know the best thing for my son to.use for recurrent bouts of pancreatitis….hes suffered with this since being 8 years old and gets severe pain and vomiting which lands up with him being hospitalize, these attacks come on at least once a month your advice would be much appreciated
Hey Donna I’m so sorry to hear about what you and your son are going through. I would start with the recommendations in this article.
Also, you can email nutrition@drjockers.com for direct guidance on this!
Do you know what his triglyceride levels are at these times? Please look up FCS (familial chylomicronemia syndrome and it’s support group on FB if they were high.
Good day! Can this help my brother recover from pancreas cancer stage 4 according to d doctor. Pllleeaase help.
Hi Jilda so sorry to hear about this! The strategies in this article will help support the pancreas and promote healing.
Good morning. This probably a very silly question, but is it possible to have gallstones if your gallbladder was removed years ago?
Hey Mary good question, it is possible for gallstones to form in the bile duct but it is very rare!
My father had them in the duct very scary!
Dr. Jockers I saw you in an interview with Ty Bolinger on the TTAC. Received some great information.
I am wasting away from an autoimmune disorder. So I am taking Hydrazine Sulfate and I
can note the stability in my weight, and not so much weight loss now. Will Hydrazine Sulfate
help my pancreas?
Hey Theartis, I have not heard anything about hydrazine sulfate and the pancreas.
For the past 6 years I have had pancreatitis it was bad because I was bleeding internally and they stopped it but i also had a very bad gallbladder that released infected gall stones which lodged them selves in my pancreas and cause allot of problem then I had major surgery and have since healed but every once am in a while I get bouts of pancreatitis and end up In the hospital. I stopped drinking and tried a better lifestyle but I still end up going to the hospital. Can you send some light on why this is still happening.
Hey Jen I’m so sorry to hear about this! There could be a lot of factors involved here. Have you worked with a Functional Medicine Practitioner before? If not, you may benefit from going through some lab work and really figuring out how to support your body in your specific case. I’d say start with the strategies outlined above and email nutrition@drjockers.com if you want to dive deeper with this!
What diet would you recommend for gastroparesis, My mother was just given this diagnoses after months of suffering and I would like to keep her as healthy as possible given her circumstances?
Hey Randee,
So sorry to hear about this!
I would suggest a healing diet:
https://drjockers.com/5-benefits-healing-diet/
She may also benefit from a Gut Healing protocol and certain supplementation. Get in contact with nutrition@drjockers.com and we can make a more individualized plan!
I got diverticulitis and would like to know what can I do to heal naturally. Thank you in advance
Hey Julia, we have some great information on this here https://drjockers.com/4-steps-to-heal-diverticulitis-naturally/
Hi doctor,
I’m 38 and have been suffering from pancreatitis since 2003 due to increased rate of triglycerides, last time the rate was as high as 23. I have been on diet and medication ( lipanthyl/ befizal) yet I have several episodes that leaves me in the hospital bed most times. Pls how can you be of help to me, I’m giving up on the treatment I’m receiving, I need to try something else more efficient to reduce the rate of triglycerides. What would you recomnend?
Thanks!
Thanks for the great info. I’m interested to know how your enzyme supplements stack up against ones available by prescription? Also, somebody mentioned mineral salts. Do you have any information about what these do and which ones are useful? I don’t understand the recommendation for a low salt diet. I find that the balance of stomach acid is a problem – too much burns due to the lack of alkalising fluid entering the duodenum and too little results in undigested food. Thanks again.
It is my understanding the enzymes available by prescription contain a more narrow range of enzymes targeted towards protein, starches, and fats. The enzymes in my line are a very broad range of enzymes that can break down many different nutritional compounds. Mineral salts AKA Himalayan or Grey salt are naturally higher in trace minerals than conventional salts and healthier in general. Also we do not recommend a low salt diet, but this is often a solution given by doctors.
I have been having pain in my leftside,after I eat.I dont have a gallblader.I think it could be pancreastic,My level are up 3 points.Should I be on emzymes?
My husband has been sick for 10 months now and no one knows how to help him. At our local hospital they did three surgeries trying to fix what was wrong and he still hurts in the same spot. He is having to go to the Mayo Clinic in Minnesota for help and we live in Alabama! He has all the symptoms of pancreatitis, he hurts severely in his upper abdomen and it radiates to his back. He is nauseous most of the time and he can’t eat hardly anything. Thank you for all the helpful info….
Hey Lydia, have your worked with a functional medicine practitioner or functional nutrition practitioner? There could be underlying issues that have not been detected.
i had acute pancreas 10 yrs ago. as of date i have no pain but my sugar levels are fluctuated (High and Low). I am on insulin . Suggest me what food to be taken to improve my pancreas condition
Hey Ravi, follow the strategies in this article. We also have a great supplement called insulin manager that may help balance your blood sugar: https://store.drjockers.com/products/insulin-manager
Hello Dr. My recent amylase blood level was 718! I have had numerous invasive tests with all negative results, however occasionally I have mild pancreatitis flare ups with mild pain cramping etc…. Drs. started me on enzyme therapy but I didnt want to take them long term. How will your Super C or another help me. Thanks
Hey Deborah, Enzymes and Vitamin C can be helpful along with the other strategies outlined in this article.
Blessings!
I had an acute case of pancreatitis we think was caused by lisinopril, my former blood pressure medicine. I started taking it at the end of September. By mid October I started having painful attacks of what I thought was the absolute worst indigestion ever. Interestingly, my white blood cell count was elevated but we thought that was a sinus problem. Each episode was worse than the previous and by January, I was in the hospital. CT scan confirmed pancreatitis. Ultrasound ruled out gall bladder issues. I don’t drink but maybe six drinks in a year and generally eat fat but not excessively. At the point I landed in the hospital, I suspected it was the medicine and thankfully, the gastroenterologist believed me. I found some similar case studies that supported it. The hospital switched my bp med to Amlodipine. That was the fifth of January. I was released on Jan 8th and have not had another attack of pancreatitis since. I don’t think it’s a super common cause of pancreatitis but if you’ve recently started lisinopril and suddenly have really horrible pain on the left that goes to your back, head to the ER and advocate for yourself. My main doctor in the hospital didn’t believe me, I think.
I had an awful bout of what i assumed to be sinusitis after cleaning an old store room out late in my last pregnancy. Several weeks after delivery, i realised i had a “knot” just under my left ribs. When i sit or bend certain ways i can feel my ribs slipping over it. Usually it is not painful but sometimes it burns and the skin just above it has a burning itch. I rarely ever get heartburn, though i have noticed over the last couple of years it has slightly increased in frequency. I broke my tailbone 6 weeks into my first pregnancy, then subsequently traumatised it twice more within 2 months. I have frequent pain focused in the (back) hips and my “bowl” in the front- i.e. front and back, not localised to only left side and its well below the pancreas. I do have frequent nausea but again assumed it was because of pcos and possibly endometriosis. Would a severely enlarged pancreas show through, or is this maybe another organ? I am still breastfeeding, so i am concerned about what safe dx i can go through. Both echinacea tea and colloidal silver seem to help the “flare” but the knot remains. I am trying one last time to drink the echinacea tea daily (im awful with regimens) to see if i can get rid of it completely, but i need a backup plan and more insight. Any help would be greatly appreciated.
Hey Teila, it is possible but hard to say for sure. You may want to consider working with one of our health coaches to put a personalized plan together!
Hi Dr. – Great article. Is it good to take bovine pancreas supplement while having pancreatitis. My blood sugar is normal. Thank you.
John
Hey John, I would recommend following the strategies in this article.
I’m just wondering if it is safe. I’m looking in to your supplements for sure. They sound great.
So are your enzymes similar to what Drs prescribe? My mother is 70 was diagnosed with Chronic Pancreatitis last year she got better after taking the creon for a while but since Sept she’s been in pretty rough shape. Drs seem to just blow her off send her to pain management and not try to see if there is anything else going on. So I’m looking to see what else I can do to possibly help her live a better life then what she is loving right now.
Hey Jessica, they are super high quality and potency and I get great results with them!
Is there any way I can get rid of my diabetes? Hi I’m 31 and very lean, active, healthy eating person. I was diagnosed with diabetes. My doctor says it was a virus that attacked my pancreas. My triglycerides are back to normal and im on a strict diet. Thank you for this article it is very helpful!
Hey Mateja, Sorry to hear about this! I can’t tell you in black and white, but there could be some helpful strategies. Start with these articles:
https://drjockers.com/diabetes/
https://drjockers.com/chronic-inflammatory-conditions/
If you want, you can send an email to michael@drjockers.com to get started on a one-on-one coaching plan.
I was diagnosed first of November with acute pancreatitis. They have me on a no fat, low protein, low carb (pasta and bread), no sugar diet because I am also borderline diabetic. The pain is much better especially after adding digestive enzymes, however, I am exhausted all the time. Losing weight is the only side benefit of this.
Is there anything I can do to regain some amount of energy?
This sounds like a malnutrition diet Sharla. I would suggest adding in some healthy fats and moderate amounts of protein throughout the day even if in multiple small meals. Using MCT oil can be very helpful as well!
Hi Doctor,
Thank you for this great article. I was wondering if you would recommend a Ketogenic Diet for someone with autoimmune pancreatitis?
Thank you.
Yes that could be helpful Lea! I would recommend using digestive enzymes, MCT oils, and powerful anti-inflammatory supplements during this time such as ProOmega CRP: https://store.drjockers.com/products/pro-omega-crp
I have pancreas swelling but iam from kashmir what medicine required
I would follow the recommendations in this article Kamran.
Thank you for such a great article with proper resources listed! I had my first bad pancreatic attack last October and have normal lipase levels now. I still get some pain after certain meals, my question is we are able to eat MCT oil? That would be great. Also, would you advise someone with acute pancreatitis to do the Keto diet?
Again, thank you!!!
Hey Tada,
Yes MCT oils can be helpful as I outlined above in this article. Also, a ketogenic diet can be helpful but you will also want to take a look a the tips in this article: https://drjockers.com/autoimmune-nutrition-plan/
I am loving this article ! I take care of nonverbal DD young man . I am sure that this is what is going on with him now. He has epilepsy and so we have no choice but to give those meds . I am wondering about the enzymes for him . The meds cause major constipation . He has lost a considerable amount of weight. He is unable to communicate pain but I can tell he is in pain which causes more seizures. Would love to know your thoughts.
Hey Tammy, it is hard to give much guidance on this but magnesium may provide some benefits: https://store.drjockers.com/collections/top-sellers/products/brain-calm-magnesium
I was told two days ago that my pancreas was inflamed. I have had zero pain.
I stopped drinking alcohol on December 25th of last year and lost weight by avoiding overeating.
I am now going through a 3-day fast before I start a new eating regiment and all I am consuming is water and herbal teas along with lemon and apple cider vinegar water.
You talk about pain but as you know I have had zero pain and I believe my wrong and drinking alcohol behavior changes might have to do with this.
Will intermittent fasts, which aid with inflammation of the entire body, be something to help control future pancreas inflammation?
Anything specific recommendations for someone with no pain?
Hey Elliot, great to hear about the lifestyle change. Yes, doing intermittent fasts and liquid nutrition is one of the very best ways to reduce inflammation. I would also recommend a healing diet: https://drjockers.com/healing-diet/
We believe birth control pills were the main caused, My wife was diagnose with Pancreatitis back in December 2017 from one high episode of 825 Lipase her level has successfully doped to normal 28 but her Amylase is at 112 normal ranges from 3-100. At times she has a bit of discomfort and pain but we have decided not to take any medication at all. He weight was 129 and she is currently at a 119 how can I work on getting her Amylase back to normal and for her weight to increase as well as maintain pain levels in a balance.
Thanks in advance I love my wife dearly and will like to help her in any way.
You will want to follow the “Strategies for Pancreatitis Management” recommendations in the article above Shanika!
My Father in law is currently suffering from acute necrotising pancreas. He was on ventilator and per doc there is leakage of blood, and internal organ failure. Would it possible if I share the report with you in an email and so that you can help me to understand how critical he is and what enzyme can be prescribed
Are vegetarian digestive enzymes as good as .creon!? How can one improve the quality and condition of ones pancreas? And can a gallstone in the duct be dissolved or removed to get back to normal function! Thank you Wendy Mason?
Hey Wendy! Following the strategies above will be great for your pancreas. Also, here is a good article on gallstones: https://drjockers.com/beat-gallstones-naturally/
Hello my name is Brandy and I was admitted into the hospital on June 27th with the acute pancreatitis my lipase was 11000 and some that’s when I decided I had acute pancreatitis as of today which is July the second my lipase is 2059 I’m still here in the hospital so all my other enzymes are normal except for my potassium is 1.0 can you give me some information on what I need to do from your article I’m still in a little pain but the pain has decreased but my stomach is still bloated but I’m still on every 4 hours but I’ve been trying to get off of that but I still needed at times so I want to know if your program will help me and will I be able to recover from this thank you
I made a few errors. The Dr said I had acute pancreatitis
My potassium level is 0.1 low.
Hey Bernadine, following the strategies outlined above can help ensure this does not happen again!
I am happy to find this website and all the comments. I would like to ask a question to Dr Jockers but I’m techno challenged. Where and how can I write my questions to Dr Jockers?
Right here Donna! Or at drjockers@drjockers.com
I have been diagnosed with chronic pancreatitis with enlarged pancreatic ducts and tissue damage. I am not diabetic, do not drink and have a healthy diet. I found an article stating that the cause could be an overactive parathyroid gland which I had removed around 15 years ago. The doctor said it’s been there for many years without symptoms. I cannot eat very much especially proteins. I have done liquids for 3 days and am better for a couple of days then inflammation again. All the doctors I’ve seen are into very invasive tests etc. What I also found is the doctors keep looking to find things but have no treatments if they do not find cancer.
Is there any light at the end of this tunnel?
Its all an investigative process Donna! For lab recommendations email nutrition@drjockers.com
My son took the drug Amnestine (Accutane) for acne in college 9 years ago. He has had GI issues for years. We believe it the drug dries up mucus membranes and causes pancreatic insufficiency. He has pancreatic insufficiency, I should say. He has to take many enzymes including Creon, and Ox Bile. Recently someone suggested to take bitters and keep using bitters as in time they may stimulate the pancreas enough. I would like to know if anyone has healed their pancreas after using Accutane. There are so many kids out there that have been damaged in this way. It’s all over the internet if you google the right thing. What I am unable to find is if you can heal and how. How do you heal from this? He is 28 now and it breaks my heart what he’s been through. He takes so many supplements to keep his health up, cooks his own very healthy food, manages his stress etc. and still has random constipation or diarrhea which drain him. Who wants to be on all these pills at 28? I can’t tell you the money we have spent to try to get to the bottom of this! Thanks for any advice!
Hey Alisa, there could definitely be a lot going on here! Have you worked with a functional nutrition/medicine practitioner to look at hormones, gut health, inflammation, food sensitivities, etc? If not, I would recommend reaching out to Michael here: https://drjockers.com/michael-fdn-p/
WOWOWOWOWOW, I have only briefly skimmed your article but so far it is the MOST inclusive article I have seen on pancreatitis signs & symptoms & diet. Although diagnosed at the ER with very mild acute Pancreatitis the more I read the more it seems I had a chronic attack and all the previous thoracic shoulder pains I’ve continued to have since my gallbladder was removed were possibly really pancreatitis attacks. Before leaving on my cruise I will be sure to review this article THROUGHLY.
Thanks for sharing that Dee! Blessings!
Article was really useful and very brief.
I am 46years old male chronic pancreatitis patient under gone with Surgery (Frey’s Procedure) in 2015 and I would like to hear from you and opinion for my current complications. Can I reach through any email id ?.
Thanks in advance
comments by dr jokers are not helpful.
Hi doc,I always have lain at my left side kf my adomen,I dont know if its pancreatitis or what.Also I git this headache like I am into anesthesia for quiet some months now,I am wondering it this gwo symptons are connected,please help.
So sorry to hear this! Yes they may be related!
In your nutrition plan, you only specify a few fruits. What about the rest of the common fruits, which are to be avoided? Acute pancreatitis here, no diabetes. Thank you.
We try to avoid the high sugar fruits.
But for example, mango looks very high in sugar content compared to many other fruits, and its on your list.
Yes in general, we try to avoid too much sugar from fruit.
Age 57, Gallbladder removed at at 23 (stopped functioning). Alcohol problem from age 12- 25..social drinker ever since. Pain in same area as gallbladder, feels very similar. Pain increasingly getting more frequent and worse if I have about two drinks, sometimes with no drinks. I have recently stopped drinking alcohol all together now. Lipase and amylase levels checked regularly (usually up) for past five years (since sister’s death pancreatic cancer age 57). Liver enzymes are fine. I am waiting for a specialist’s consult and possible ERCP. Hard to stick to a diet as have numerous food allergies and sensitivities.
Questions: Can years of food allergies and sensitivities cause these types of issues? I certainly know alcohol can.
What are the genetics risks of developing pancreatic cancer and is it increased with years of pancreatitis flare ups? Thanks in advance
So sorry to hear that Dee and yes years of poor gut function, food sensitivities and infections can absolutely be the root cause for gallbladder and pancreas issues.
Hi Dr Jockers
Got to say this is the most informative info I’ve found online. I was first admitted in hospital last October gallstone and gallbladder out. 2 weeks later back in pancraetis then a ultrasound showed a benign cyst on pancreas which I had to let grow for six week. Then had a stent put in unfortunately stent got logged in my stomach but my cyst had decreased dramatically in size.
I always still get pains and niggles in my back I’m sure the cyst as grown back as its where it was before is this gonna cause another flare up please is there anything can do.
I look forward to your response
Thankyou Nicola
Hi Nicola, I am sorry to hear that you are suffering with this pain. Following the recommendations in this article can help you create a customized plan unique to your circumstances: https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/
Thank you for the very informative article. I have been diagnosed with hereditary (genetic) pancreatitis after gall bladder removal surgery. I have done bunch of research related to pancreatitis and would like to share some of my findings :
1) Probiotics can be dangerous and cause flare ups for people with pancreatitis (I personally experienced a few just because of sauerkraut and kimchi)
https://nutritionfacts.org/video/culture-shock-questioning-the-efficacy-and-safety-of-probiotics/
2) Hot Turmeric tea with a pinch of black pepper is my survival drink (black pepper shoots up the absorption of the turmeric).
3) Narcotic pain killers (morphine, hydrocodon) cause in my case spasm of the sphincter of Oddi which feels very similar to pancreatitis but lasts shorter period of time. However, when in the hospital stay for acute pancreatitis, narcotic pain killers extended my misery and lengths of stay.
4) Plant Based Diet significantly improved my condition and overall health.
Probiotic yogurts and low fat dairy work in my case(acute pancreatitis). I’m from Eastern Europe, my only doctor from the ER recommended to never, from now own, eat anything that includes cabbage, raw or otherwise. I don’t know if its based on any studies, but from talking with other patients, it seems like a general rule in my country, if you suffer from pancreatitis, give up cabbage.
Hi Daniel, It is always best to follow the recommendations of your trusted physician who knows your symptoms well and health history. Cooked cruciferous vegetables are packed with anti-inflammatory nutrients, however, it is best to avoid any foods that trigger complications.
I forgot to say, I take 1-2 pills a day of curcumin (turmeric extract) which is a strong antioxidant and anti inflammatory. I’ll try the turmeric tea with pepper, I enjoy the tea much more than taking pills(of any kind).
Hi Daniel, That is great to hear! Yes, please let us know if you enjoy the tea.
Dr. Jockers, thank you for all that you do to help heal the hurting. I do have a question about my ER experience three days ago. First off I pride myself in the fact that all my adult life I’ve been into eating healthy and being into alternative health and healing. I just moved into a new home and was without a kitchen for one month, and for one month I’ve eaten out every meal and made bad choices. After a lunch at the local pizza place I returned home feeling sluggish, and after one hour I was on my way to the ER. I had all the signs of acute pancreatitis, and after being given a ultrasound I was told that I had passed a gallstone as a valve appeared to be dilated. A blood test revealed a lipase level of 8000. I was admitted and was told that if I could tolerate a clear liquid lunch the following day I could be released. So after lunch, there was no more pain and I was released with instructions to stay on clear liquid diet and followup with my Primary Doctor. Since I just moved and can’t get into a doctor, just wondering what you think about the 8000 level and what appears to be a lackadaisical attitude with such a high level?
Hey Flo, I am sorry to hear this. Inflammation due to gallstones are a primary risk factor for acute pancreatitis and elevated lipase levels. This article offers tips on how to limit the inflammation, reduce and flush out gallstones: https://drjockers.com/beat-gallstones-naturally/
Hello Doctor,
You are doing great service by answering questions from patients.
I am a 38 year old male from India with no history of acute pancreatitis. For the last two years, since I was travelling a lot, had to eat outside food. I am non-alcoholic, non-smoking. On 1st May 2019, I had a severe stomach ache, went to ER and it was diagnosed as acute pancreatitis. My lipase level was 8000. After liquid diet for 3 days, I was discharged. I was following a low fat diet since then. On 10th June 2019, i had a hearty high fat meat diet and that night, my pancreas flared up. MRCP showed a pancreatic duct stricture near the head of pancreas. Otherwise the pancreas was healthy and normal size. No gallbladder stones. My doctor conducted ERCP and placed a plastic stent to clear up the stricture. Now i am on a low fat diet eating home cooked meals only. There is no pain now.
Questions
1. Could the first attack created the stricture or could it have been present before itself (getting formed over the years)
2. Both the times, i had the acute pancreatitis, it was after an heavy meat meal. Should I completely avoid meat from now on?
3. What are the chances that the strictures form again if I am on a low fat diet.
4. Could the first attack be due to stress and high fat diet that I was eating.
Thanks
Hey Sudhakar, I’m sorry to hear this. It sounds like there is a lot going on. I would recommend that you work with a functional health practitioner who will get to the root cause of your problems and customize a specific plan for you! This article can help: https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/
Dear Dr. Jockers, Thank you so much for all the information you share. I am a 68 year old female – 2 year survivor of Endometrial cancer. Still cancer free. I have been doing the Keto diet and receive holistic therapy still – 75 grams of IV Vitamin 2x a month. I have a cyst in the head of the pancreas – non cancer, however, as of recently I have started to get chronic diarrhea. I normally take 2 digestive enzymes with each meal as recommended by my practitioner but doesn’t seem to help and I am concerned this cyst is the cause. My question is … in general are there any protocols for shrinking cysts????
Hey Denise, It is important to determine the underlying cause of the cyst. I recommend working with a functional medicine practitioner to guide you on testing and supplements which may be helpful.
I Got 2 Acute Pancreatitis Attack in a year, I am on soft diet and still feel some pain sometimes, got my blood test level of Lipase and Amylase serum still elevated to 450 Lipase and 250 Amylase, both time all other tests are normal but to diagnose we went for EUS and it diagnose Microlithiasis in Gall Bladder, what do you suggest next?
So sorry to hear this! Follow this article https://drjockers.com/25-ways-improve-gallbladder-health/
Hi Dr. Jockers
Trying to help my son in law. he has been admitted to the ER with Pancreatitis 3 times last year. I was giving him some advice encouraging him to start a Ketogenic diet which has done wonders for me in the past 10 years.
However, my research has led me to suggesting that a Ketogenic diet might worsen his condition. We know that diabetes type 2 is 100% reversible by greatly reducing carbohydrates, eating moderate protein and increasing your fat intake to upwards of 70% of your total caloric intake.
However, the higher fat intake might be detrimental to his pancreatitis. I would like him to consider your diet regimen but with a higher intake of carbohydrates won’t this keep him on his diabetes meds?
So if I could ask a couple of specific questions to maybe guide me in the right direction to help him.
1. Will your diet regimen be detrimental to his diabetes?
2. If he starts your regimen, will his pancreatitis flares stop after a while and if so could he then start to add more fats and protein gradually until he is full blown ketogenic?
3. By not being on a high fat diet initially, which controls satiety and hunger making it much easier for compliance, how much MCT oil can be added to your daily diet regimen to control hunger while he heals his pancreas?
Thank you
Hey Mark, it is hard to answer these questions with full accuracy without a thorough health analysis and lab testing. I would encourage you to work with one of our health coaches who can better understand his case and customize a plan for him. https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/
I have pancreatic insuffioncy. I am on Creon. This is working well. Is this safe?
Glad you are doing better. Creon is safe but some people do have side effects. Be sure to discuss this with your physician.
Thanks! What are the side affects as my doctors (functional & traditional) states there are none (unless they were from a sick pig). I have tried supplemental enzymes with no luck. How about the ones you support?
Now they found (MRI) a lesion on the body of my pancreases. They state it is probably a cyst but can not rule out a tumor. We are looking at next steps. I do have oral herpes and have had 2 bouts on shingles and Covid 19. The last bout of shingles was pretty rough and I was put on some anti viral med, for about 3 months (which this article stated all could be reason for pancreatic issues). We have tested for the shingles/herpes virus several times and my blood works shows that I still have the virus active in me, but I don’t have symptoms. I do have break throughs in my face with some pretty painful nerve pain in my jaw, nose, eye and temple (always on my right side of face). My functional doctor has me on L-Lysine for these symptoms. I don’t want to go back on the anti viral meds. again as she wants me to do this for about 6 months as I believe my kidneys (and maybe my pancreas) took a hit on this med.. I have gotten my kidney numbers back up to 78 where they were 111.
Thoughts please?
Thanks so much for your time!!!
I’ve had chronic pancreatitis for about five years. It’s reasonably well maintained with betaine Hcl, pepsin and bitter herbs, though I at times have flares. The flares coincide with decreased gut motility (bananas are often the culprit!) or exercises that compress the abdomen, particularly those involved with raising my right leg. I also think there is a spinal connection, as I recently had a flare after several weeks of using Dr. Sinett’s Backbridge to correct poor shoulder posture, but it is impossible for me to say for certain. I’ve started eating pineapple with meals that have larger portions of animal protein, and will start using a digestive enzyme very soon. I landed here wondering whether reflexology might help. Thank you for that and all the other information you provide on this topic.
The one comment that I wish to make regards alcohol as a cause of pancreatitis. I’m fully aware of the way alcohol is metabolized and the toxic byproducts that ensue. But when my dog developed pancreatitis (now well managed with a low fat diet) our veterinarian stated that it was VERY common in older dogs. Since dogs have basically zero alcohol consumption, if alcohol CAUSES pancreatitis, then pancreatitis should be nearly non-existent in pets (personally, I feel alcohol is the perfect blame-the-victim defense of allopathic medicine). I stopped drinking several months ago due to undesirable cardiac effects (from heart issues [caused by a bicycle crash in 2010] that developed in 2018, the year before my first pancreatitis flare). I suspect the health crisis caused by my heart issues led to my pancreatic issues. And six years later I’m slowly clawing back the health that I lost during that period.
Personally, I suspect that pancreatitis is yet another disease of circulatory dysfunction, caused by widespread endothelial damage (seed oils would be my prime suspect in the case of my dog and myself). If so, increased Omega 3s and supplementation to increase nitric oxide production could be beneficial, and there is some anecdotal evidence to suggest the latter is.
I developed a spastic colon a year or two after learning about my pancreatitis. Something in my routine had started to significantly improve that last month, but I’m struggling to parse things to determine what created the benefit. Right now, I’m thinking if I can solve the spastic colon issue, I’ll be on my way to also resolving the pancreatitis. The two seem connected.