 Intestinal Permeability, Histamine, and Leaky Gut Functional Lab Markers
Intestinal Permeability, Histamine, and Leaky Gut Functional Lab Markers
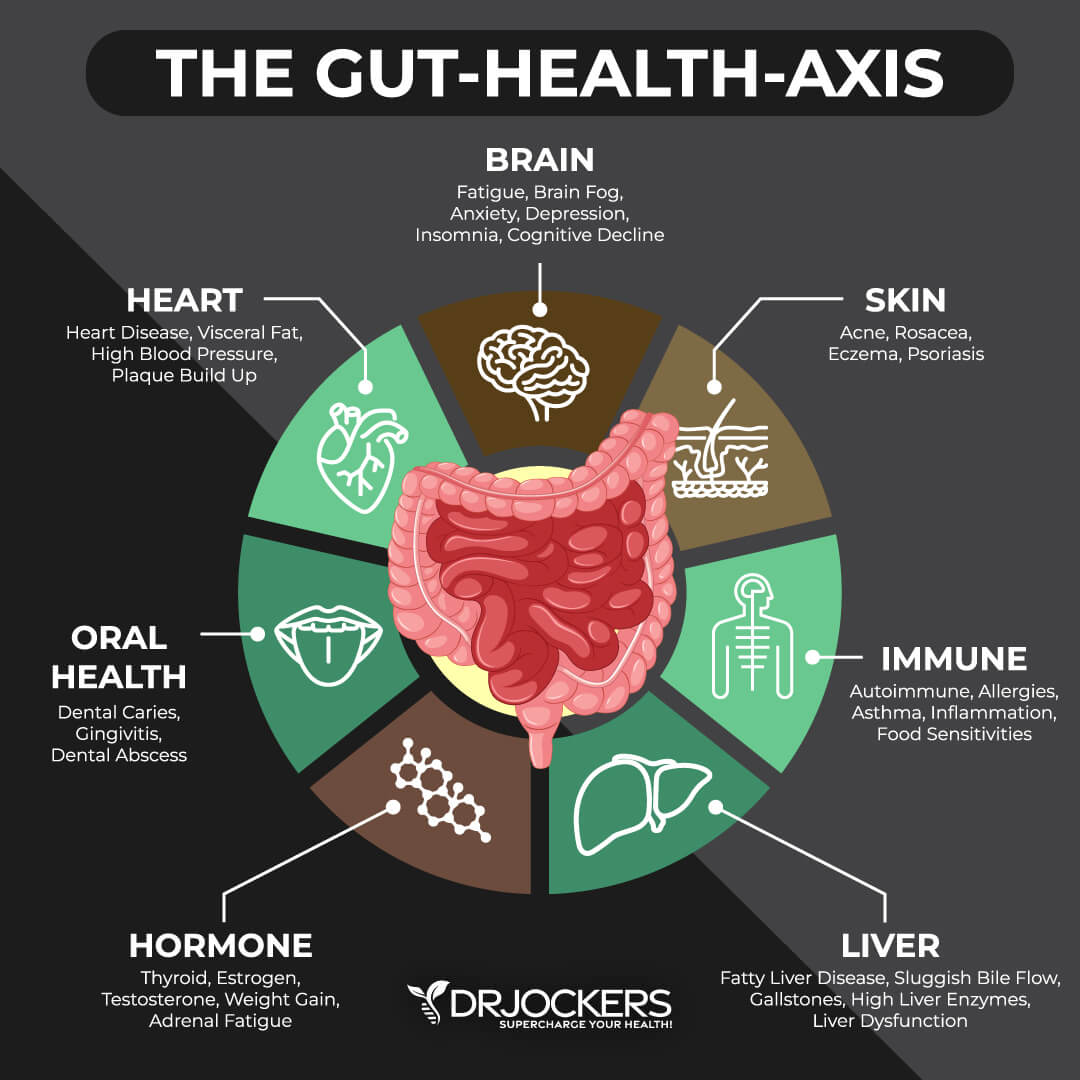
Intestinal permeability or leaky gut syndrome is an increasingly common health issue. It means that your gut lining has developed some holes that can allow undigested food particles, toxins, and microbes to pass through into your bloodstream. This can increase chronic inflammation and lead to a chronic immune response. As a result, intestinal permeability can cause histamine intolerance, chronic symptoms, autoimmunity, and other chronic health issues.
In this article, you will learn what intestinal permeability or leaky gut is. You will understand how intestinal permeability develops. You will learn about the symptoms of intestinal permeability and its connection to histamine and histamine intolerance.
I will share the most important functional lab markers, including key lab markers for intestinal permeability and histamine, GI Map gut health markers, and basic blood markers we need to look at to test for intestinal permeability and related problems. These functional lab markers can allow proper diagnosis, an effective individualized treatment protocol and recovery.
What is Intestinal Permeability “Leaky Gut”
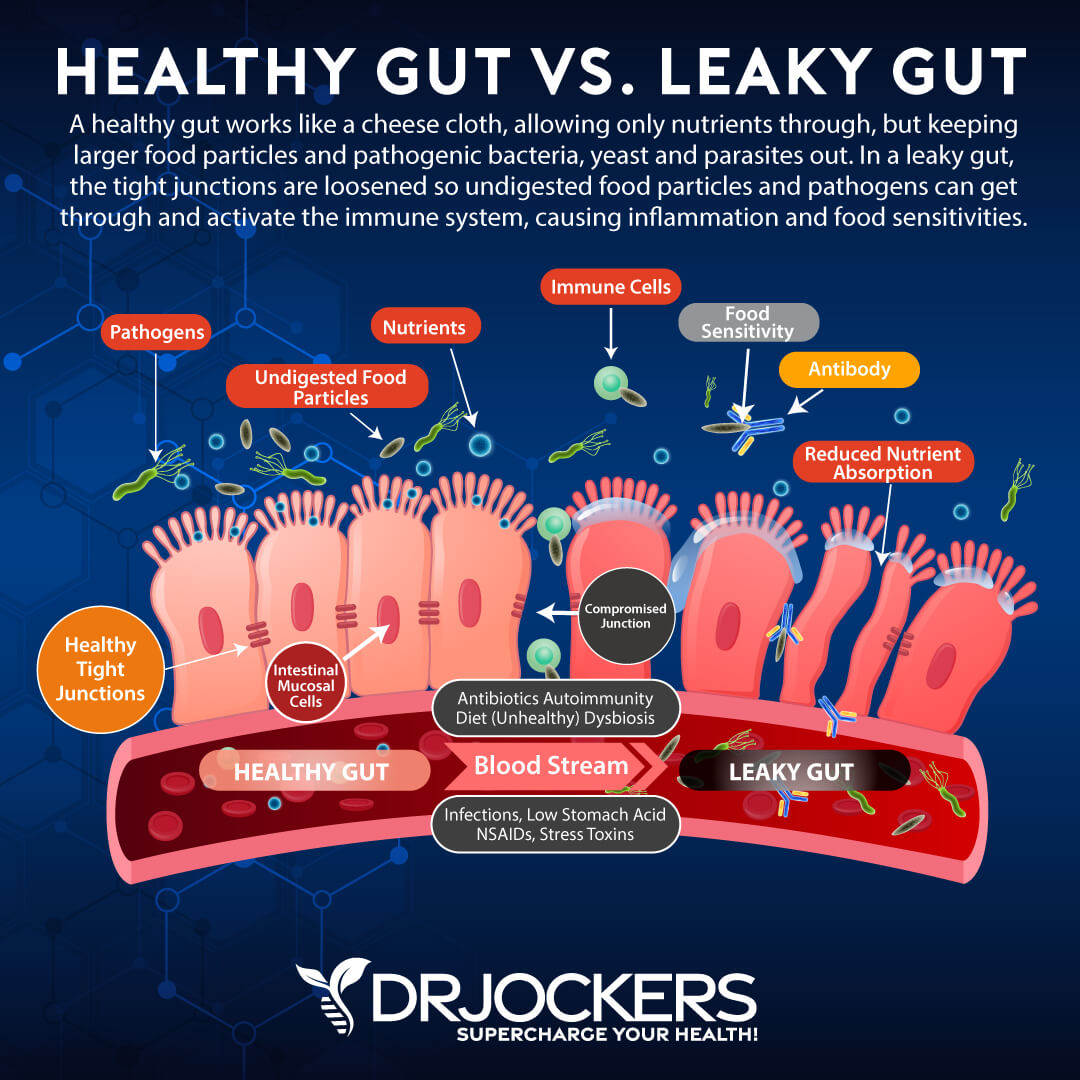
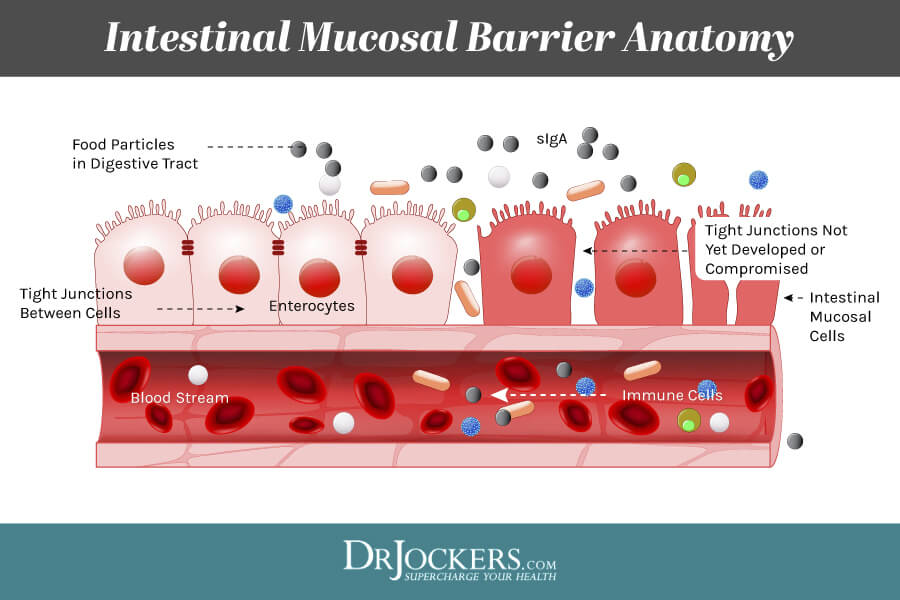
Intestinal permeability is also known as leaky gut or leaky gut syndrome. If your gut lining is healthy, it is naturally semi-permeable. This means, that your gut lining allows important micronutrients to pass through tiny junctions or holes into your bloodstream. However, these tiny gateways are very small, and undigested food particles, microbes, and toxins are unable to get through. This helps to keep your gut and the rest of your body healthy. Pathogens that can’t pass through will eventually get eliminated through urine or stool.
The problem occurs inflammatory foods, infections, toxins, chronic stress, and other harmful external factors compromise the health of your gut lining. Ongoing exposure to these factors can seriously damage your gut lining and break apart these tiny passageways creating bigger holes. When bigger holes develop, your gut lining becomes permeable and you develop intestinal permeability or leaky gut syndrome.
If you have intestinal permeability, it means that not only important micronutrients can pass through into your bloodstream, but the holes are big enough for undigested food particles, toxins, microbes, and pathogens to easily move through.
Needless to say, these particles shouldn’t be passing into your bloodstream. By getting in there, they can cause serious damage. Intestinal permeability can increase chronic inflammation and compromise your immune system. It can lead to an ongoing chronic immune response to these foreign substances, which increases the risk of chronic symptoms, autoimmunity, and other health problems.
An increasing number of scientific evidence suggests that intestinal permeability is a major cause of many chronic health issues and needs to be taken seriously. A 2012 review published in Clinical Reviews in Allergy and Immunology and a 2017 review published in Frontiers in Immunology have both found that intestinal permeability can increase the risk of intestinal permeability (1, 2). A 2021 study published in PLoS One has found that intestinal permeability may also increase the risk of metabolic health issues (3).
How Does Intestinal Permeability Develop
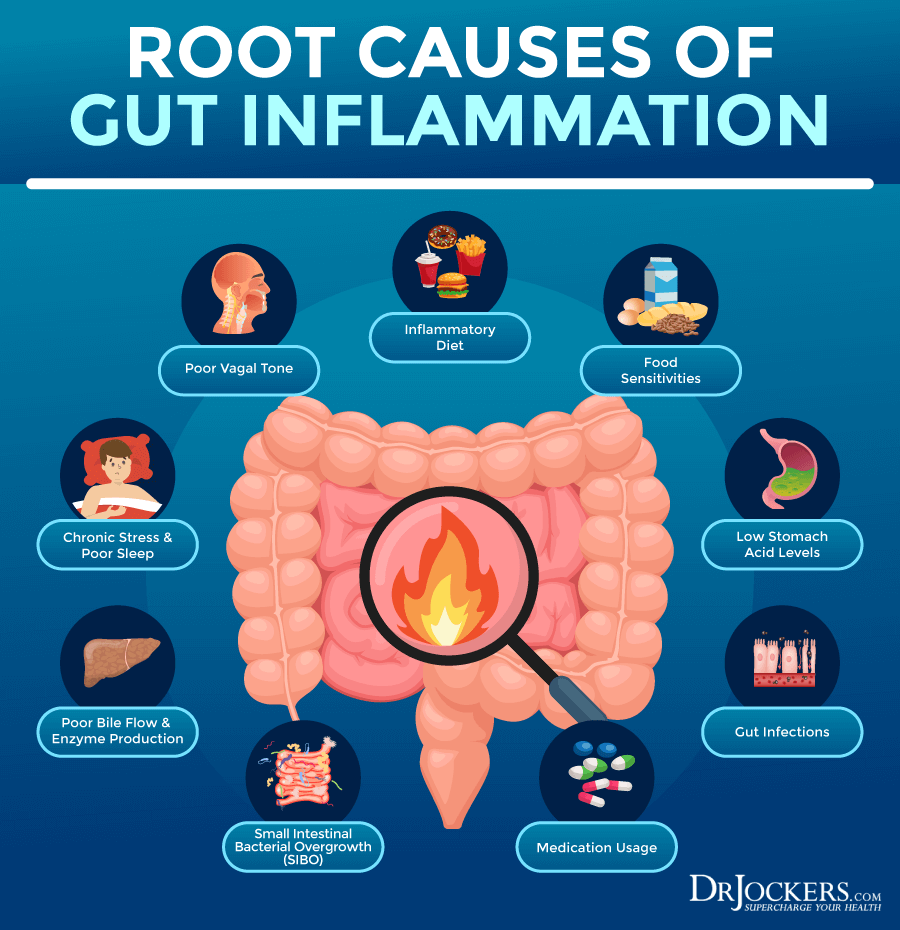
Intestinal permeability develops over time due to chronic exposure to a number of unhealthy factors, including inflammation foods, infections, toxins, medications, and stress.
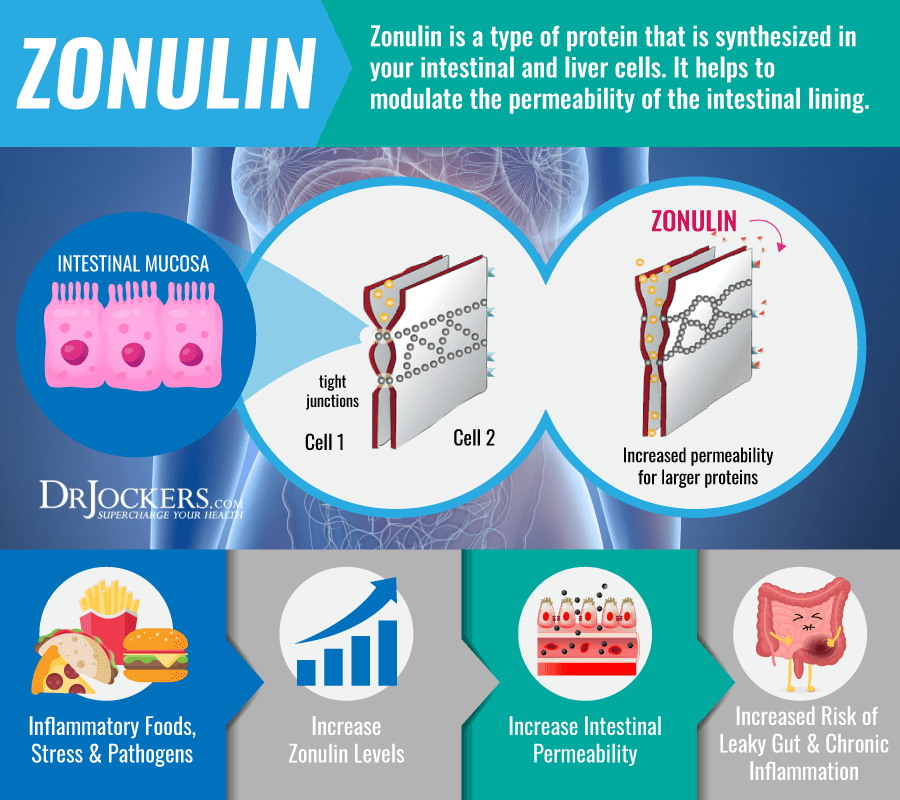
Inflammatory foods, including refined sugar, refined oil, gluten, dairy, artificial ingredients, food sensitivities, and high-histamine foods, are among the number one causes of intestinal permeability. A 2012 study published in the Annals of New York Academy of Sciences has found that zonulin, released by gluten, for example, plays a role in the development of intestinal permeability and consequent autoimmunity (4).
Gut infections, including small intestinal bacterial overgrowth (SIBO), candida overgrowth, bacterial overgrowth, intestinal parasites, and viral infections can all compromise your gut health and increase your risk of intestinal permeability. For example, a 2014 review published in Autoimmune Diseases has found that the Epstein Barr Virus (EBV) often plays a role in intestinal permeability, gut problems, and autoimmunity (5).
Environmental toxins, including pesticides, chemicals, mercury, and BPA from plastic, and certain medications, including antibiotics, anti-acids, non-steroidal anti-inflammatory drugs (NSAIDs), and steroids, may also increase your risk of intestinal permeability. A 2017 review published in Frontiers in Immunology has found that toxins play a role in the increased risk of intestinal permeability (2).
Lastly, chronic stress, including emotional, psychological, and physical stress can increase your risk of intestinal permeability. A 2019 review published in Current Opinions in Behavioral Sciences has found that stress and depression can increase inflammation, gut imbalances, and intestinal permeability (6).
Symptoms of Intestinal Permeability
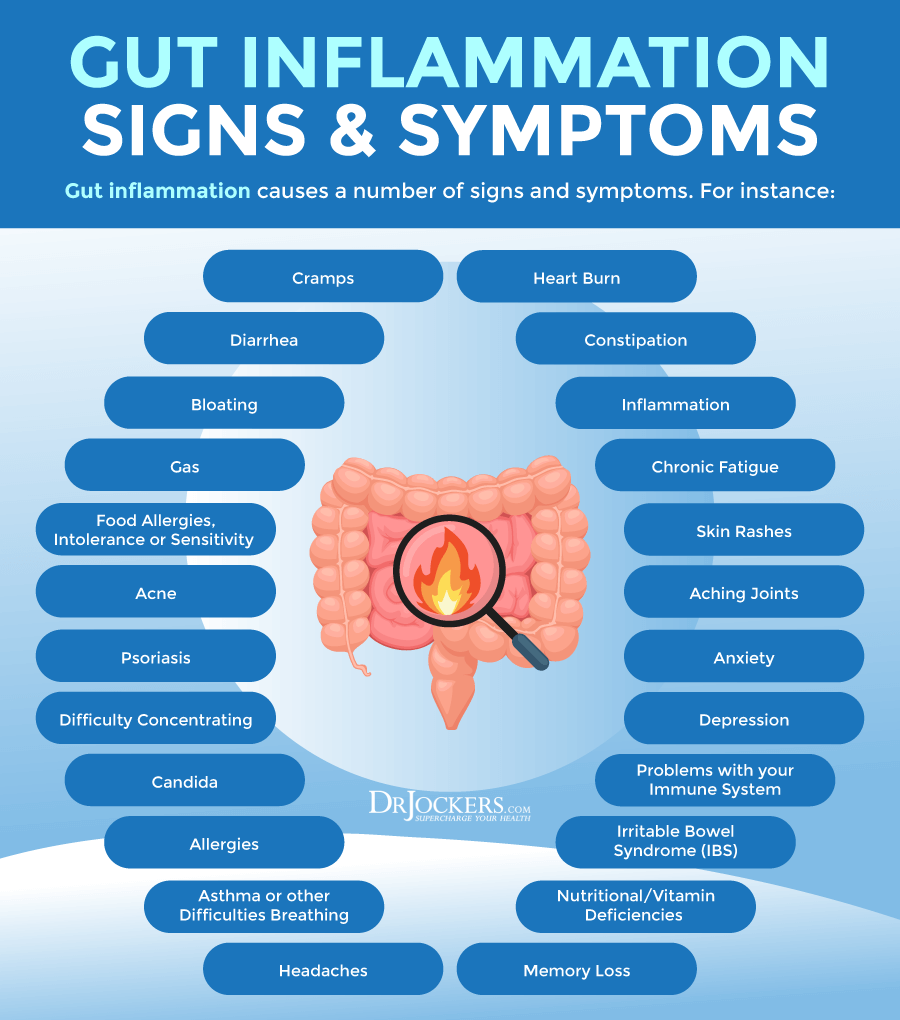
Signs and symptoms of intestinal permeability may include:
- Digestive issues, including bloating, gas, constipation, diarrhea, nausea, or irritable bowel syndrome (IBS)
- Food allergies, food sensitivities, or food intolerances
- Skin problems, including acne, rashes, eczema, or rosacea
- Fatigue
- Insomnia or other sleep issues
- Brain fog, difficulties concentrating, memory troubles
- Mood imbalances, including anxiety and depression
- Headaches or migraines
- Chronic muscle or joint pain
- Getting sick often, slow recovery from illness, and other signs of poor immune health
- Seasonal allergies or asthma
- Hormonal imbalances, including irregular periods, PMS, or polycystic ovarian syndrome (PCOS)
- Autoimmune diseases, such as Celiac disease, Chron’s disease, rheumatoid arthritis, Hashimoto’s thyroiditis, lupus, or psoriasis
- Fibromyalgia
- Chronic fatigue syndrome
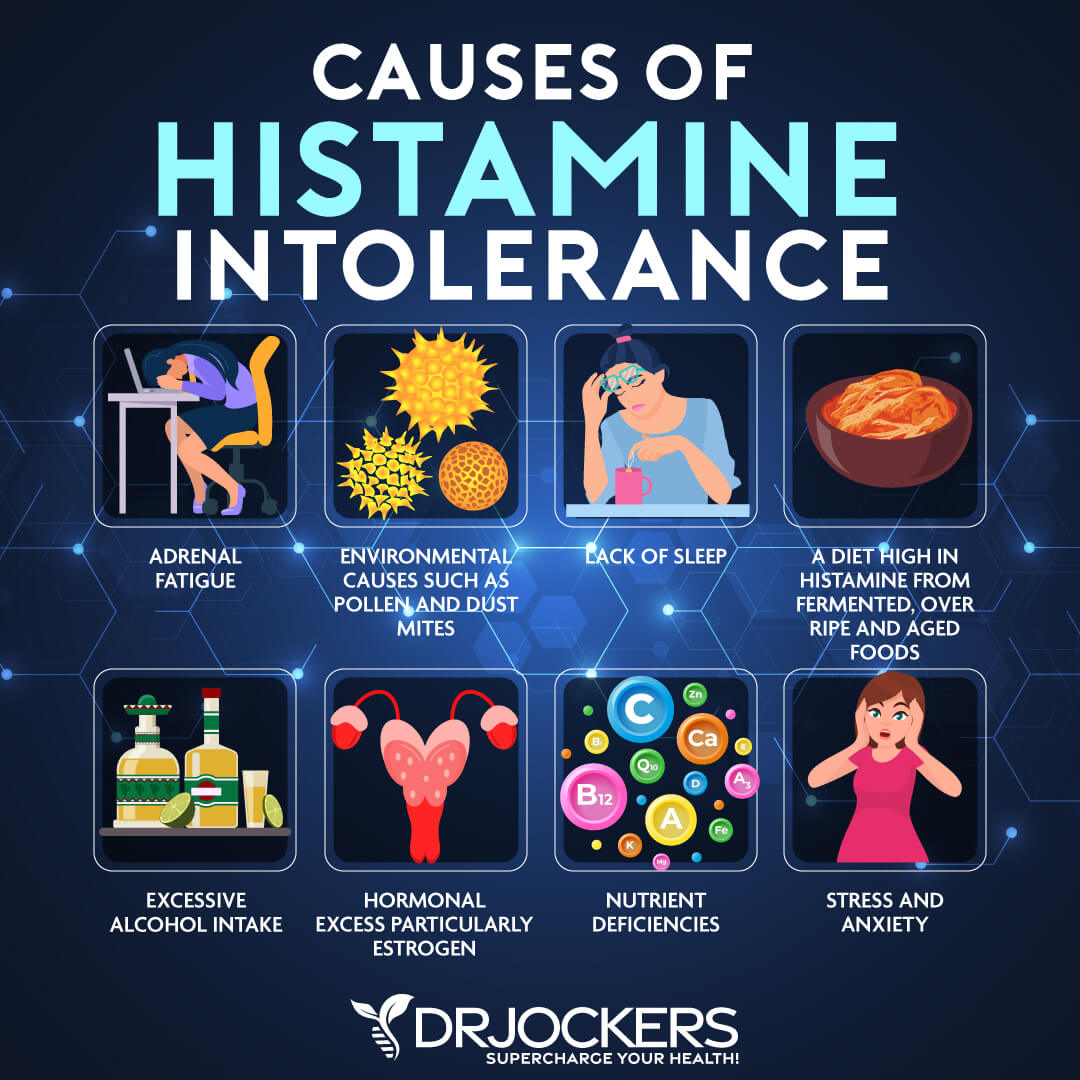
Intestinal Permeability and Histamine Intolerance
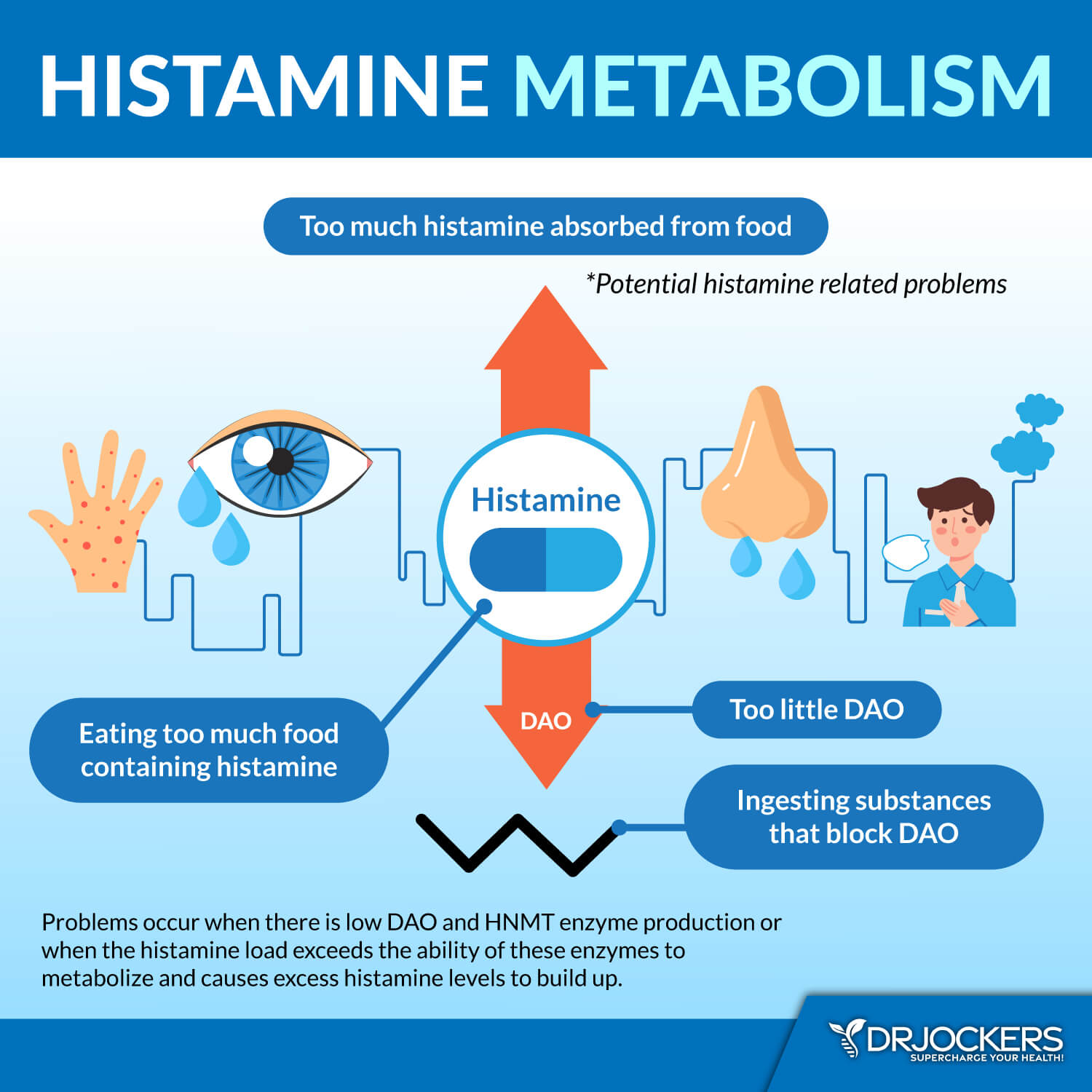
Intestinal permeability can also increase your risk of developing histamine intolerance and symptoms of histamine intolerance in several ways, including inflammation, bacterial overgrowth, and a deficit of the diamine oxidase (DAO) enzyme.
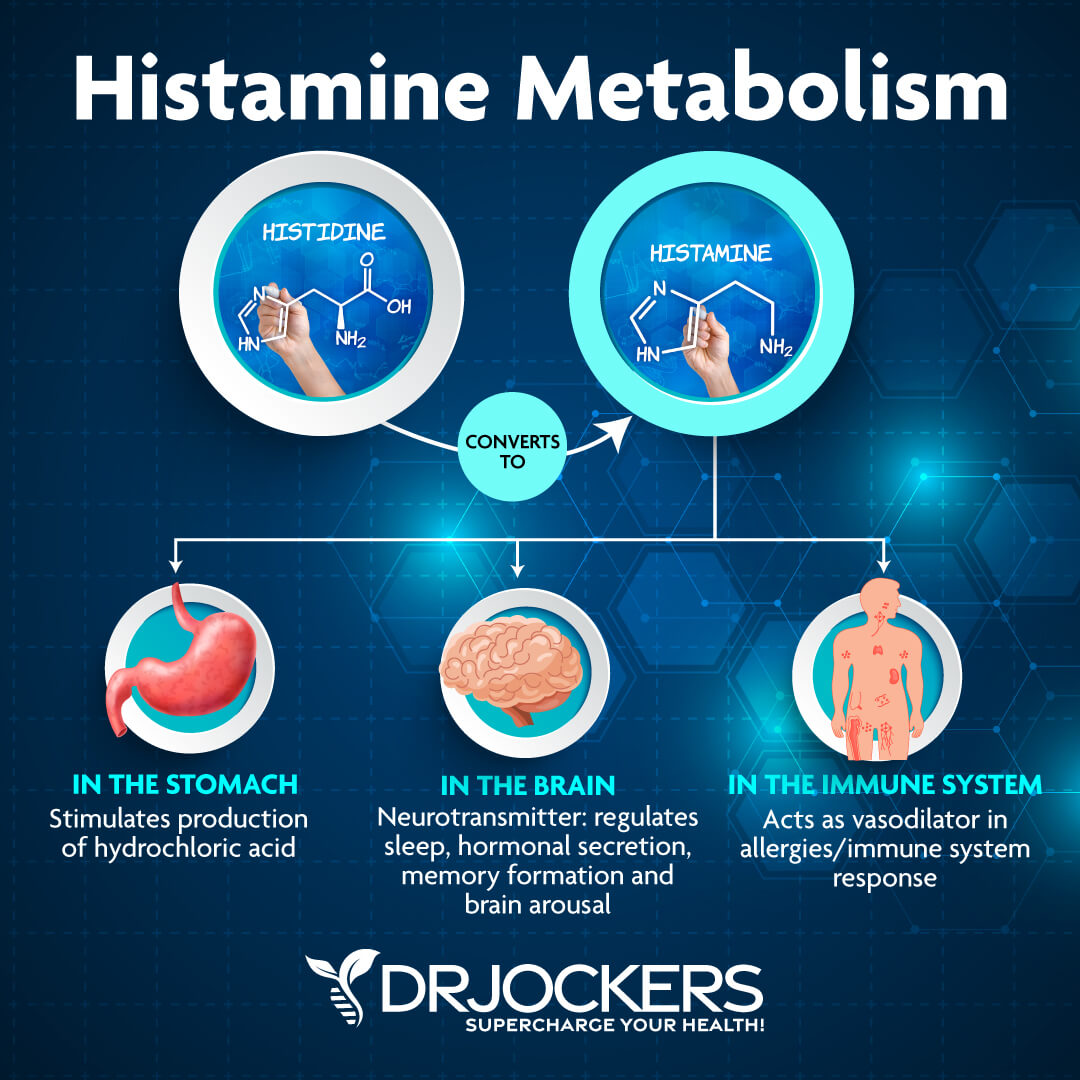
Histamine is an important chemical produced by your body. It helps your body to get rid of allergens through an immune response, support digestion by triggering the release of stomach acid, and support brain, mental, and overall health by communicating with your brain.
While histamine is essential, if you have too much of it, it can become a problem, since your body won’t be able to handle it and break it all down. Too much histamine in your body means that you have histamine intolerance, which can lead to a number of uncomfortable symptoms, including skin issues, digestive problems, migraines, anxiety, and more, as well as, contribute to other chronic health issues.
As 2018 study published in Mediators of Inflammation and a 2013 study published in the British Journal of Pharmacology explains, histamine plays a role in the modulation of the immune and inflammatory response in inflammation (7, 8). If you have intestinal permeability, it means that foreign pathogens and larger food particles can pass into your bloodstream.
Intestinal Permeability and Excess Histamine
Intestinal permeability is also a sign that there is something off in your gut, and there is likely a gut microbiome imbalance. Such gut imbalance can increase the risk of bacterial overgrowth.
Bacterial overgrowth, of course, increases chronic inflammation and gut health issues. However, according to a 2016 research published in Integrative Medicine (Encinitas), certain bacteria, especially L. casei and L. bulgaricus, also increase histamine production (8).
Lastly, intestinal permeability and other gut health issues can also increase the risk of a deficiency in the diamine oxidase (DAO) enzyme. The DAO enzyme is an important enzyme that’s critical for the breakdown of excess histamine and keeping your histamine levels at bay.
Not having enough DAO enzymes means that your body won’t be able to deal with the excess histamine increasing the risk of histamine intolerance. A 2019 study published in Food Science and Biotechnology has found that supplementing with DAO enzymes can improve histamine intolerance (10).
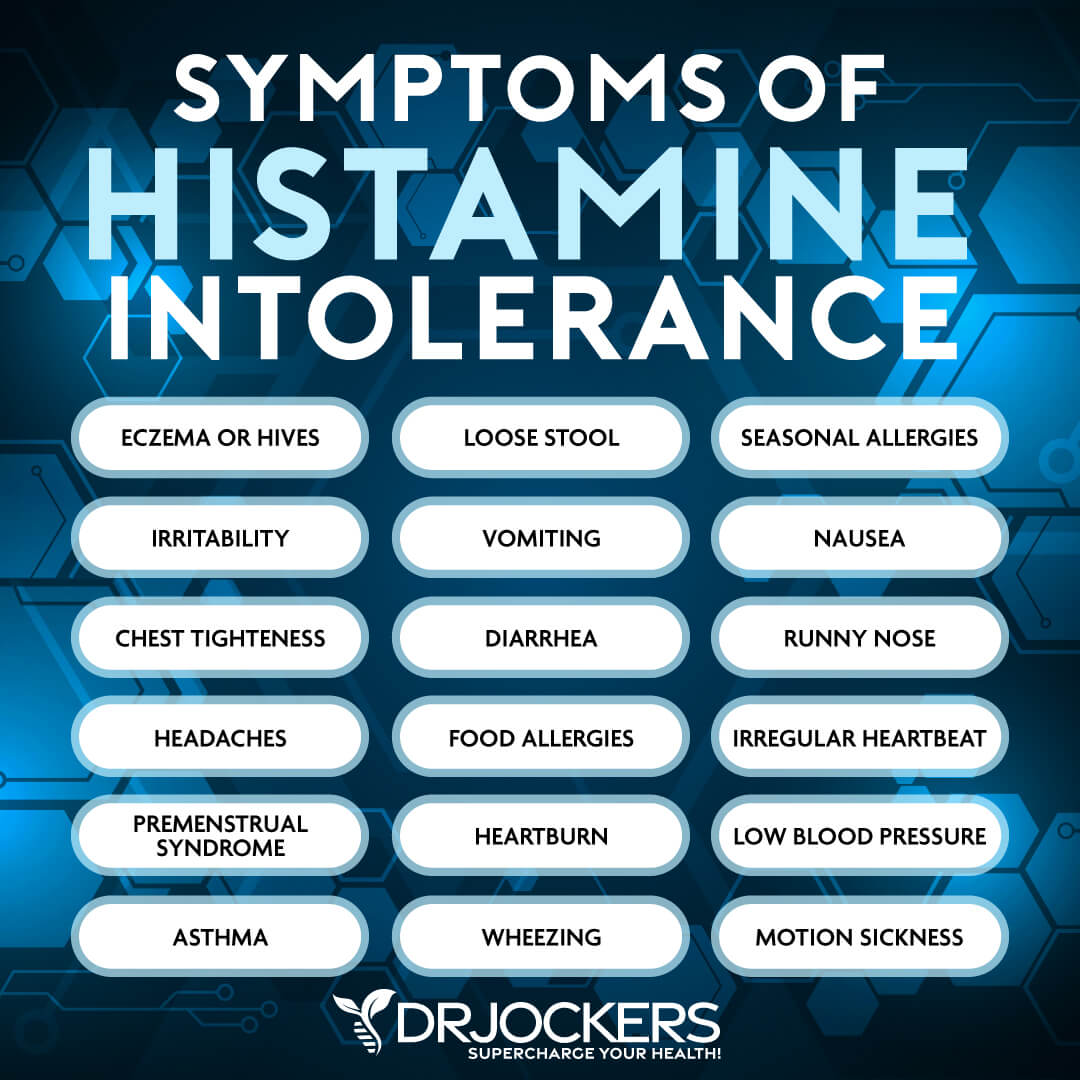
Symptoms of Histamine Intolerance:
Symptoms of histamine intolerance may include:
- Congestion or runny nose
- Headaches or migraines
- Diarrhea or constipation
- Hives, eczema, rashes, psoriasis, and other skin problems
- Flushing
- Allergies or asthma attacks
- Crawling sensation on skin or scalp
- Vertigo
- Tachycardia
- Low blood pressure
- Hypertension
- Anxiety
- Abnormal menstrual cycle or PMS
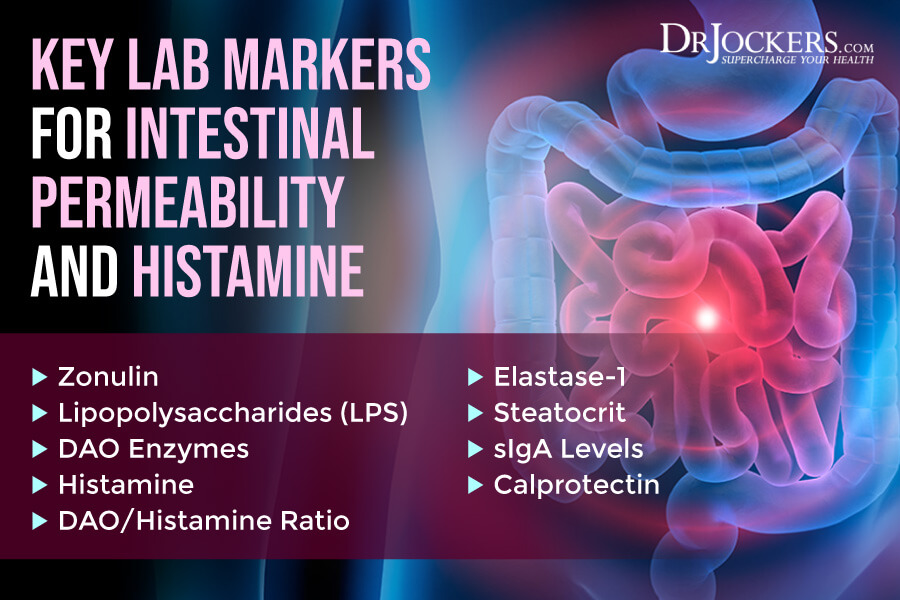
Key Lab Markers for Intestinal Permeability and Histamine
To check for intestinal permeability and histamine, I recommend looking at the following key lab markers.
Zonulin
Zonulin is a type of protein that is synthesized in your intestinal and liver cells. It helps to modulate the permeability of the intestinal lining. Checking your zonulin levels can help to detect or determine the risk of intestinal permeability.
A 2012 review published in Clinical Gastroenterology and Hepatology has found that zonulin can play a role in intestinal permeability and it should be considered both as a diagnostic tool and for its therapeutic implications (11). A 2016 review has also found that zonulin plays a role in regulating the function and health of the intestinal barrier and can play a role in the development of chronic inflammatory diseases (12).
A 2020 review published in F1000 Research has found the same results (13). According to the discussion, zonulin-mediated intestinal permeability can increase the risk of chronic inflammatory diseases, including autoimmune diseases, such as Celiac disease, type 1 diabetes, multiple sclerosis, inflammatory bowel diseases (IBDs), and ankylosing spondylitis, metabolic disorders, such as obesity, gestational diabetes, hyperlipidemia, insulin resistance, and non-alcoholic fatty liver disease, intestinal diseases, such as irritable bowel syndrome (IBS), non-celiac gluten sensitivity, and environmental enteric dysfunction, certain cancers, such as glioma and hepatocellular carcinoma, and neuroinflammatory conditions, such as autism spectrum disorder, schizophrenia, major depressive disorder, and chronic fatigue syndrome.
According to a 2017 study published in Practical Laboratory Medicine, the normal median concentration of fecal zonulin is around 61 ng/mL (+/- 46 ng/mL) making 15 to 107 ng/mL the normal range (14). Normal serum zonulin levels are a median of 34 ng/mL (+/= 14 ng/mL) making 20 to 48 ng/mL normal. High zonulin levels may indicate intestinal permeability, intestinal inflammation, and gut health issues.
Lipopolysaccharides (LPS)
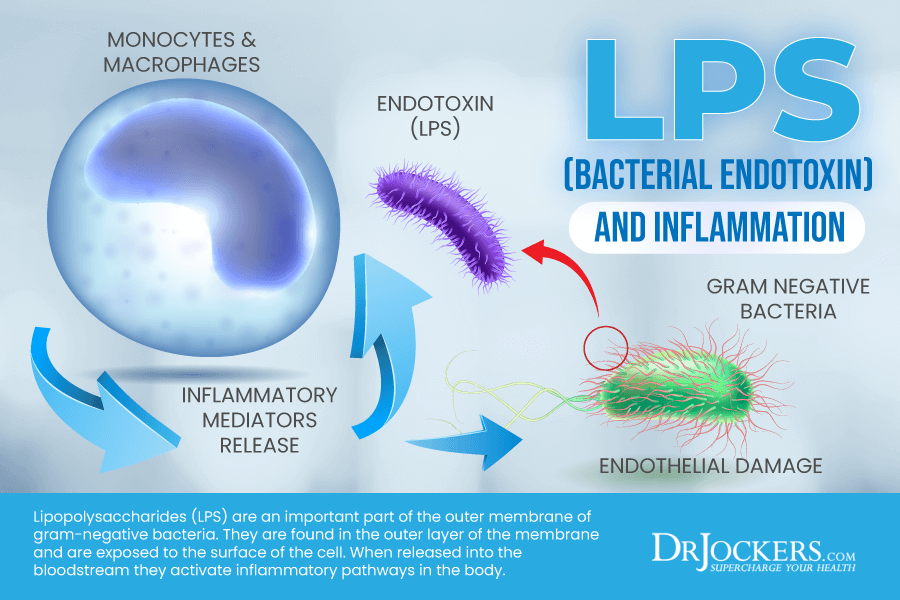
Lipopolysaccharides (LPS) are an important part of the outer membrane of gram-negative bacteria. They are found in the outer layer of the membrane and are exposed to the surface of the cell. They help to support and stabilize membrane structure.
According to a 2020 review published in the Journal of the Endocrine Society, LPS can cause changes in the intestinal lining which may lead to the development of various diseases (15). A 2017 review published in the American Journal of Pathology has found that high LPS levels can increase intestinal permeability and related gut issues, such as Crohn’s disease (16). According to a 2018 review published in the European Journal of Microbiology and Immunology, normal levels of LPS are very low at 5 picogram per mL blood or below (17).
DAO
As you’ve learned earlier, the DAO enzyme is an important enzyme that’s critical for the breakdown of excess histamine and keeping your histamine levels at bay. Not having enough DAO enzymes means that your body won’t be able to break down all the excess histamine, which may lead to histamine intolerance.
A 2016 study published in the International Journal of Immunopathology and Pharmacology has found that people with histamine intolerance tend to have lower levels of serum DAO enzymes (18). A 2018 study published in Allergy has found that reduced DAO enzyme levels are linked to higher histamine levels and histamine intolerance (19). According to a 2013 scientific paper published in the Allergo Journal, healthy DAO plasma levels may range between 15 and 50 U/ml, however, during pregnancy, they may increase up to 500-fold (20).
Histamine
As you’ve learned, histamine is an important chemical for your immune response, fighting allergies, your digestion, and brain health. However, if you have too much histamine or histamine intolerance, it becomes a problem. Checking your histamine levels is important to detect histamine intolerance which may be related to intestinal permeability as well.
A 2021 study published in Nutrients has found that histamine intolerance may actually be connected to your gut (21). Poor gut health and certain medication can reduce DAO enzyme activity and lead to histamine intolerance. Another 2021 review publish Nutrients has found that histamine intolerance is connected to low intestinal DAO enzyme levels (22). According to a 2007 review published in The American Journal of Clinical Nutrition, normal histamine levels are between 0.3 and 1.0 ng/mL (23).
DAO/Histamine Ratio
We also have to take a look at your DAO/histamine ratio. This ratio helps detect subtle imbalances between histamine and DAO levels. Even if the DAO enzyme level is normal when histamine is high, symptoms can occur. A low ratio indicates that there may not be enough of the DAO enzyme relative to the amount of histamine in your body.
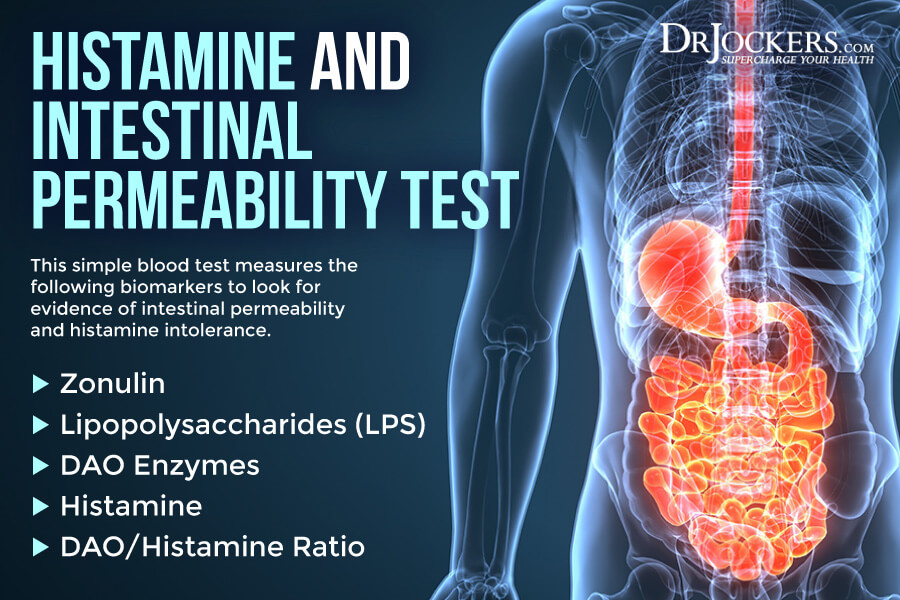
Histamine and Intestinal Permeability Test
To test for these levels, I recommend the Histamine and Intestinal Permeability Test. This is a comprehensive test that tests for histamine, DAO, the DAO: Histamine ratio, Zonulin, and Lipopolysaccharide (LPS). With the help of this test, you can find out if you have histamine intolerance and look for signs and risk factors of intestinal permeability.
GI MAP Test Markers
The GI Map Stool Analysis is my favorite gut test to look for dysbiotic flora, bacterial, parasitic, and viral pathogens, potential autoimmune triggers, and all intestinal health markers.
This is the best and most comprehensive gut test I have found and it helps me tremendously to identify the root cause of my patient’s health issues and help them to repair their bodies and regain their health naturally. Here are the markers I recommend looking at with the help of the GI Map Stool Analysis to check for intestinal permeability.
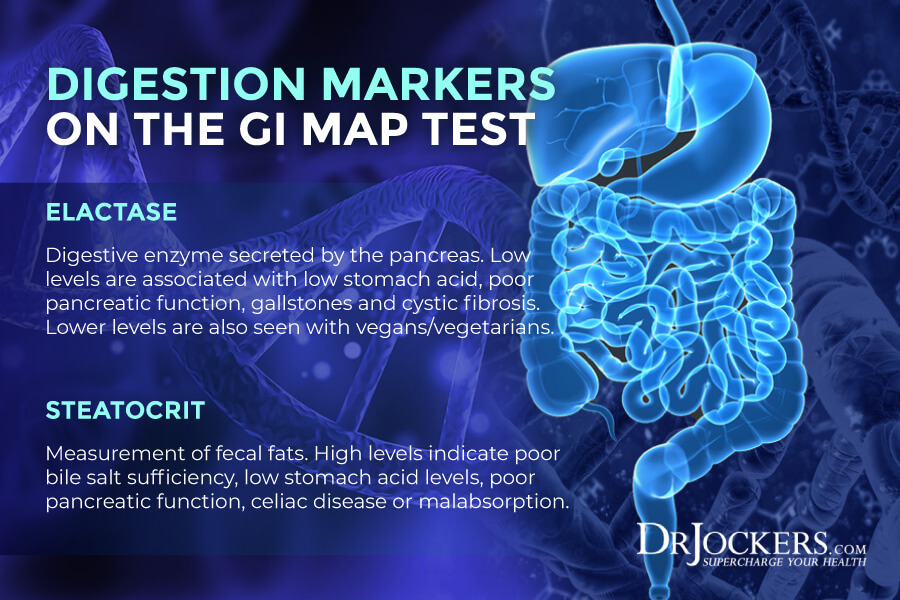
Low Elastase-1
This gut health test looks at Pancreatic Elastase 1 levels, which is a digestive enzyme secreted by your pancreas. A 2007 study published in the Journal of Gastroenterology has found that looking at elastase 1 and fecal calprotectin levels can help look for pancreatic issues and find a possible connection between pancreatic problems and intestinal inflammation (23).
Normal elastase-1 levels are below 200 mcg elastate/g. Low levels have been associated with poor pancreatic function, gallstones, cystic fibrosis, and hypochlorhydria. Low levels are more common among vegans and vegetarians (25).
High Steatocrit
The GI map also checks for steatocrit levels, which is a measure the amount of fat in feces. A 2016 research published in Ecology and Evolution has found that fecal steatocrit levels are a good indication of intestinal health (26).
Normal steatocrit levels are between 0 and 14.9 percent. High levels of steatocrit indicate fat malabsoprtion, which may be due to intestinal issues (25). It is also a potential marker for low stomach acid, poor bile flow, reduced pancreatic lipase and potentially poor liver health.
Abnormal sIgA
Part of the test is an immune response test (secretory IgA or sIgA and anti-gliadin IgA). According to a 2011 study published in Mucosal Immunology, this test can tell a lot about mucosal health and immune health (27). Poor levels may indicate intestinal issues, IBS, IBDs, or food sensitivities as well.
Normal sIgA levels are 5.2 +/- 0.94 ug/mL (28). Low fecal sIgA may indicate a suppressed gut immune system, chronic dysbiosis, antigen exposure, protein malnutrition, immunocompromised state, or chronic stress. High fecal sIgA may indicate acute infections, acute stress, food sensitivities, or chronic dysbiosis. High anti-gliadin IgA may indicate an immune response to gluten (25).
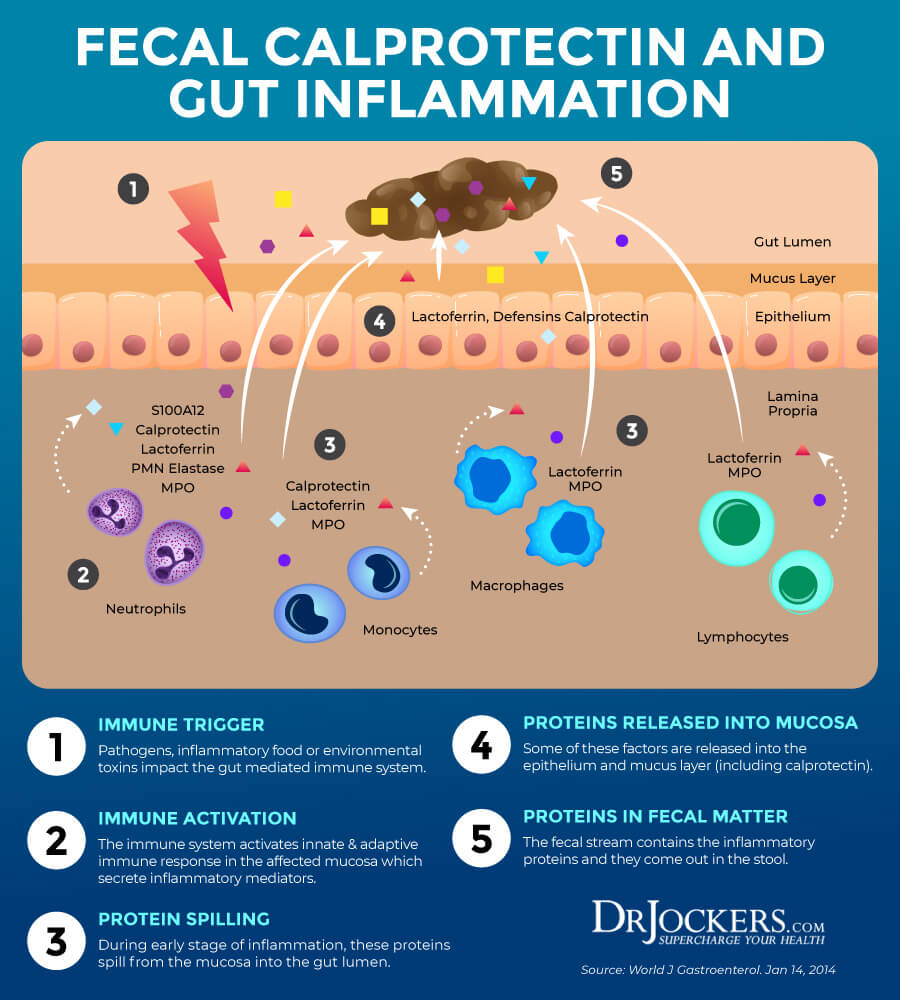
High Calprotectin
The test also checks for certain markers of inflammation. Calprotectin levels look for intestinal inflammation.
According to a 2007 study published in the Journal of Gastroenterology, that looking at elastase 1 and fecal calprotectin levels can help look for pancreatic issues and find a possible connection between pancreatic problems and intestinal inflammation (23). According to a 2011 study published in Clinical Gastroenterology and Hepatology, this test is very important for the diagnosis of irritable bowel disease (29).
Normal calprotectin levels are between 10 to 50 or 60 μg/mg (30). High levels may indicate inflammatory bowel disease and help us to differentiate from irritable bowel syndrome. Food allergens, polyps, infections, diverticulitis, and colorectal cancer may also cause high calprotectin levels (25).
Basic Blood Testing Markers
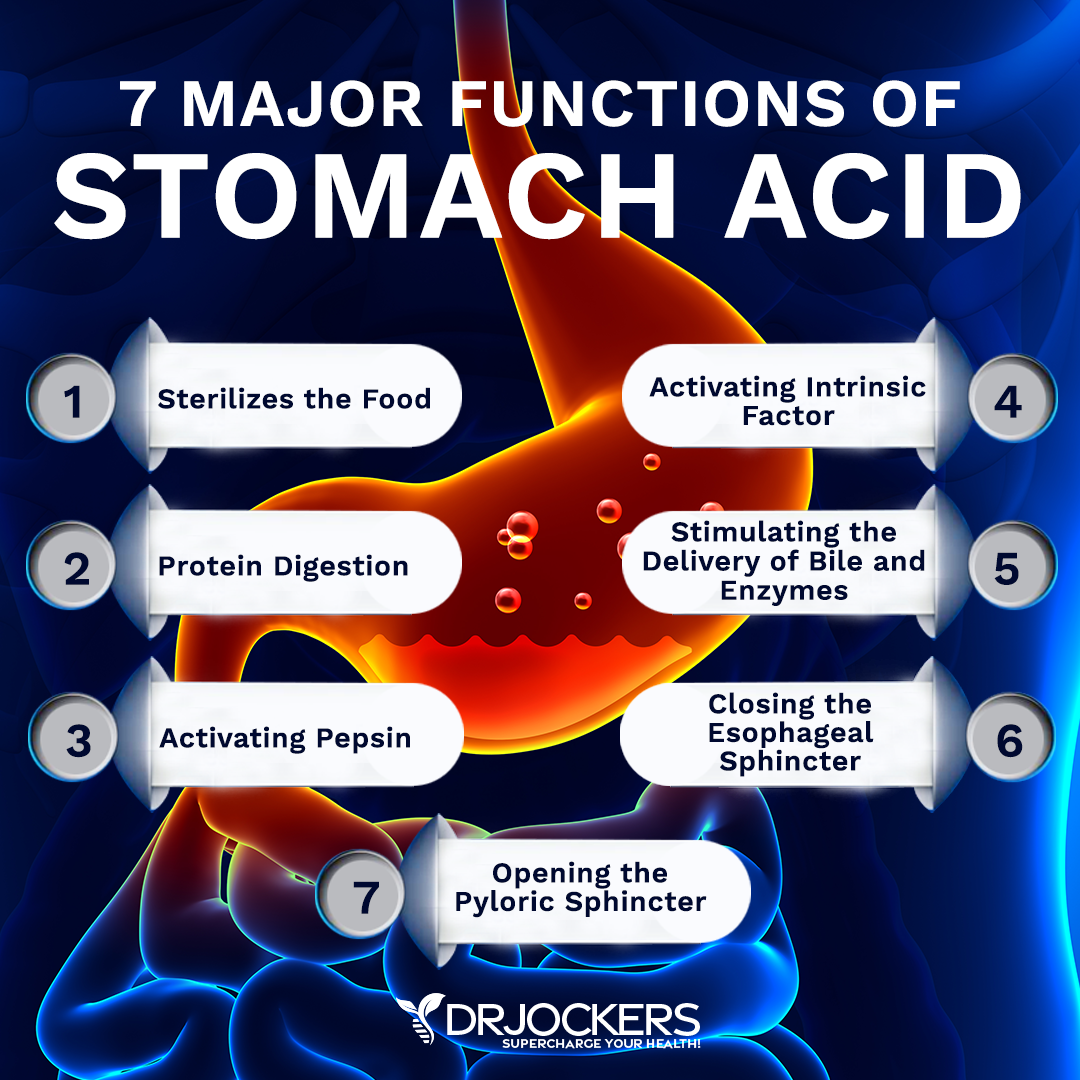
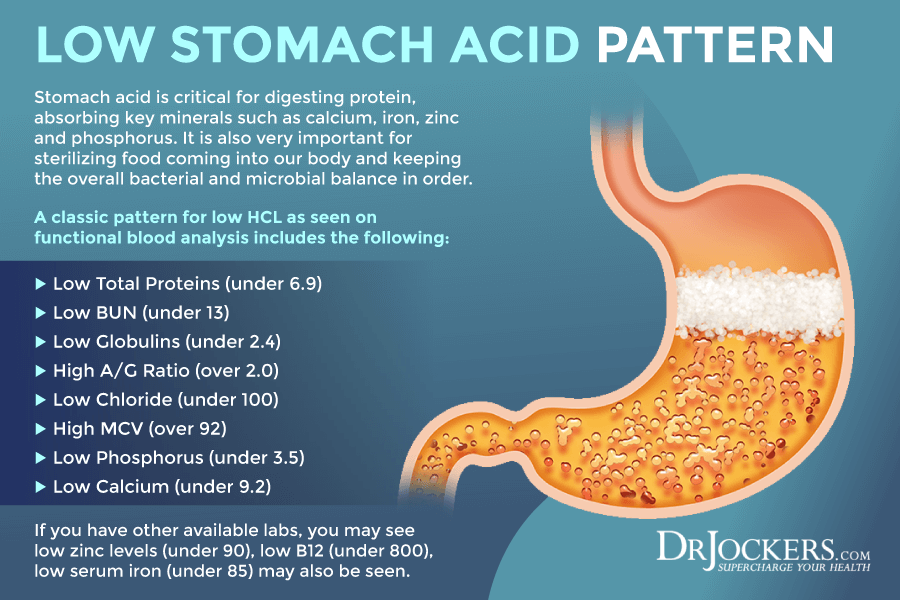
I recommend looking at some basic blood testing markers to look at stomach acid, malabsorption, and other digestive issues. Stomach acid (HCL) is essential for digesting protein, absorbing key minerals such as calcium, iron, zinc, and phosphorus. It is also necessary for sterilizing food coming into our bodies and keeping the overall bacterial and microbial balance in order.
As people age or if they have certain infections, stressors, or other health problems, they lose the ability to produce enough HCL to properly absorb nutrients and keep their microbiome in balance. When this happens, it can cause a wide variety of health problems.
A classic pattern for low HCL as seen on functional blood analysis includes the following: Low total proteins (under 6.9), low BUN (under 13), low globulins (under 2.4) and high A/G Ratio (over 2.0), low chloride (under 100), high MCV (over 92). If you have other available labs, you may see low zinc levels (under 90), low B12 (under 800), low serum iron (under 85) may also be seen. Let’s look at these markers.
Low Total Proteins
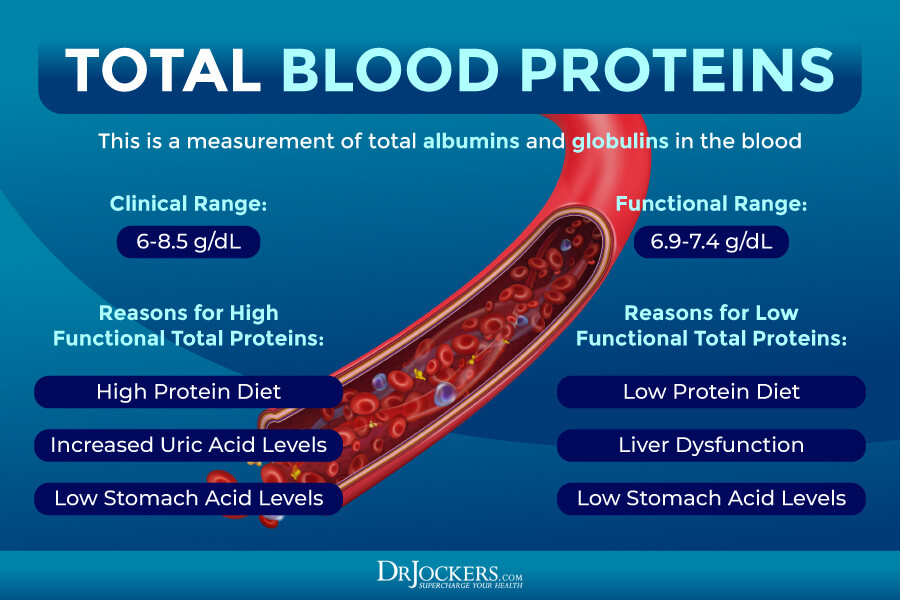
One of the markers we need to look at is your total protein. According to a 1968 study published in Gut diet, including eating too much or too little protein can affect stomach acidity (31). Total protein, not surprisingly, measures the total protein levels in your blood.
Serum proteins are separated into albumin and globulins, albumin being the one at the highest concentration. Too much or too little protein in your diet can often cause elevated or low levels of total protein. Uric acid and HCL levels can also affect your total protein count.
The optimal range for total is 6.9 to 7.4 g/dL. High levels may indicate a high protein diet, increased uric acid, or low HCL. Low levels under 6. 9. may indicate a low protein diet, liver dysfunction, or low HCL. Low HCL is commonly caused by an H pylori infection, gut inflammation, dysglycemia, or hypothyroidism.
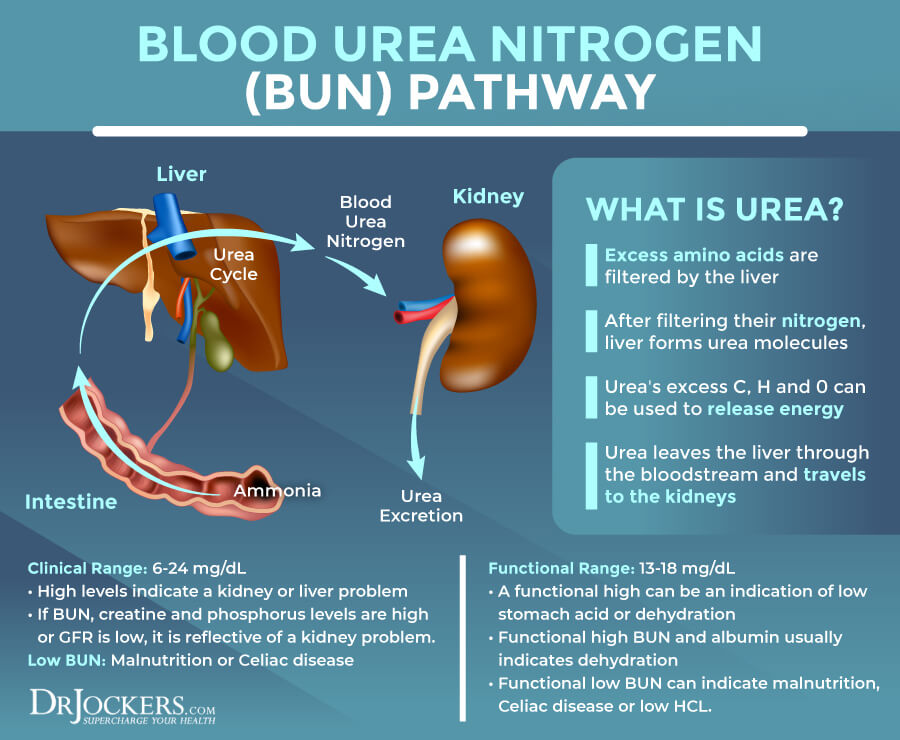
Abnormal BUN
Blood urea nitrogen (BUN) is formed in the liver. It is the final step of protein metabolism. It is a waste product that your kidneys remove from your blood. High levels often indicate problems with kidney function. A 2015study published in the World Journal of Gastroenterology has found that high BUN levels (over 21) can play a role in upper gastrointestinal bleeding (32).
The clinical range for BUN is 6 to 24 mg/dL The optimal range is 13 to 18 mg/dL. High levels can be a kidney problem or high functional range levels often indicate low stomach acid or dehydration. If the BUN levels are and your creatinine and phosphorus levels are high, it usually means kidney problems, while if only the BUN levels are high, it may be due to dehydration or low HCL.
High BUN and high albumin usually mean dehydration. Low levels under 13 may mean low HCL. Low levels can be too much hydration. Low BUN can also mean malnutrition, Celiac disease, or low HCL.
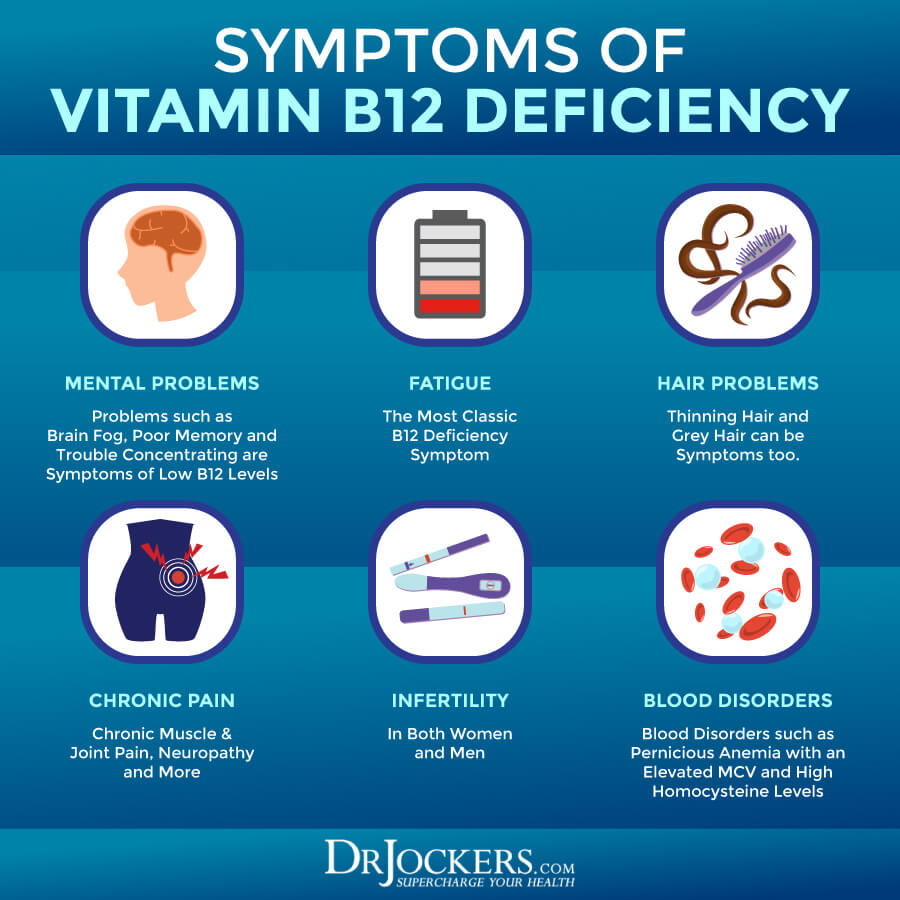
High or Low MCV
MCV stands for the mean corpuscular volume and is the average volume of a red blood cell. Iron deficiency, vitamin deficiencies, and red blood cell problems often cause unhealthy MCV levels. Poor MCV can be linked to gut health issues as well. A 2019 study published in the Annals of Surgical Oncology has found that high MCV may be correlated with poor outcomes for gastroesophageal adenocarcinoma (33).
Optimal levels of MCV are between 85 and 92 fl. Low MCV is related to a microcytic, or iron deficient, red blood cell. High MCV, over 92, is related to a megaloblastic, or a B vitamin deficient, red blood cell. If the MCV is flagged high it is typically a B12 or folate deficiency. If the MCV is flagged low it is typically an iron deficiency. Both of these can be related to poor absorption from low stomach acid levels.
Low Chloride
Chloride is another essential electrolyte that affects fluid and pH balance. It is also a critical element in the development of HCL stomach acid. However, according to a 2021 article published by StatPearls Publishing, HCL is essential for digestion and taking care of pathogens from undigested food (34). Adrenal stress and adrenal failure is often behind low chloride levels, while stress, insulin resistance, or aspirin use are common culprits of higher levels.
The optimal range for chloride is 100 to 106 mmol/L. Elevated levels of chloride may be a sign of adrenal stress, high salt diets, kidney problems, or too much aspirin. Low levels of chloride, under 100, may indicate adrenal fatigue, low HCL, or kidney issues.
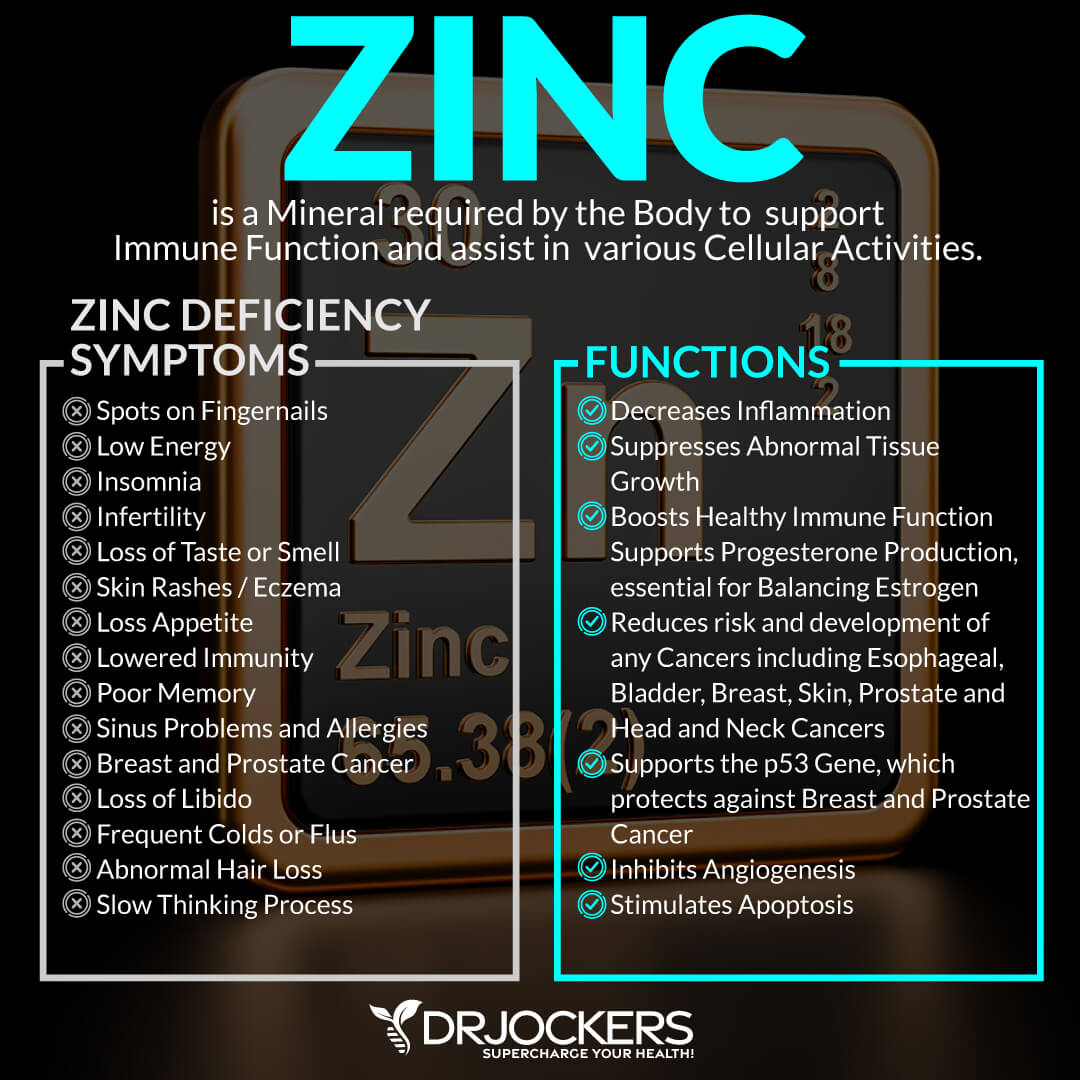
Low Zinc, B12 & Iron
Zinc is an important mineral that helps to reduce inflammation, improve immune health, and support overall health. A 2016 study published in the Middle East Journal of Digestive Diseases has found that zinc supplementation may help to improve acid reflux and heartburn (35). A 2001 study has found that zinc supplementation may help to reduce intestinal permeability in those with Crohn’s disease (36).
Vitamin B12 is important for brain and mental health, bone health, energy, heart health, and reduced risk of anemia. A 2016 study published in the Journal of Nutrition and Healthy Aging has found that gastric acid inhibitor medications for acid reflux and heartburn may cause deficiency in vitamin B12 (37). A 2014 review published in Cell Metabolism has found that vitamin B12 may serve as an important modulator for the gut microbiome (38).
Iron is essential for growth and development, energy, hormonal health, and other areas of your health. A 2004 study published in The American Journal of Clinical Nutrition has found that lower gastric acid output related to an H. pylori infection may cause problems with iron absorption, which may lead to iron deficiency (38). A 2018 review published in Pharmaceuticals (Basel) has found that iron deficiency can cause gut microbiome issues, however, high or unabsorbed iron can too (39).
Normal plasma zinc is 90-135 ug/dL. Normal serum vitamin B12 level between 800 pg/mL and 1500 pg/mL. The lab range for serum iron is 27-159 ug/dL while the functional range is 85-130 ug/dL. Low zinc levels, under 90, low B12, under 800, low serum iron, under 85, may indicate low HCL levels and gut health issues.
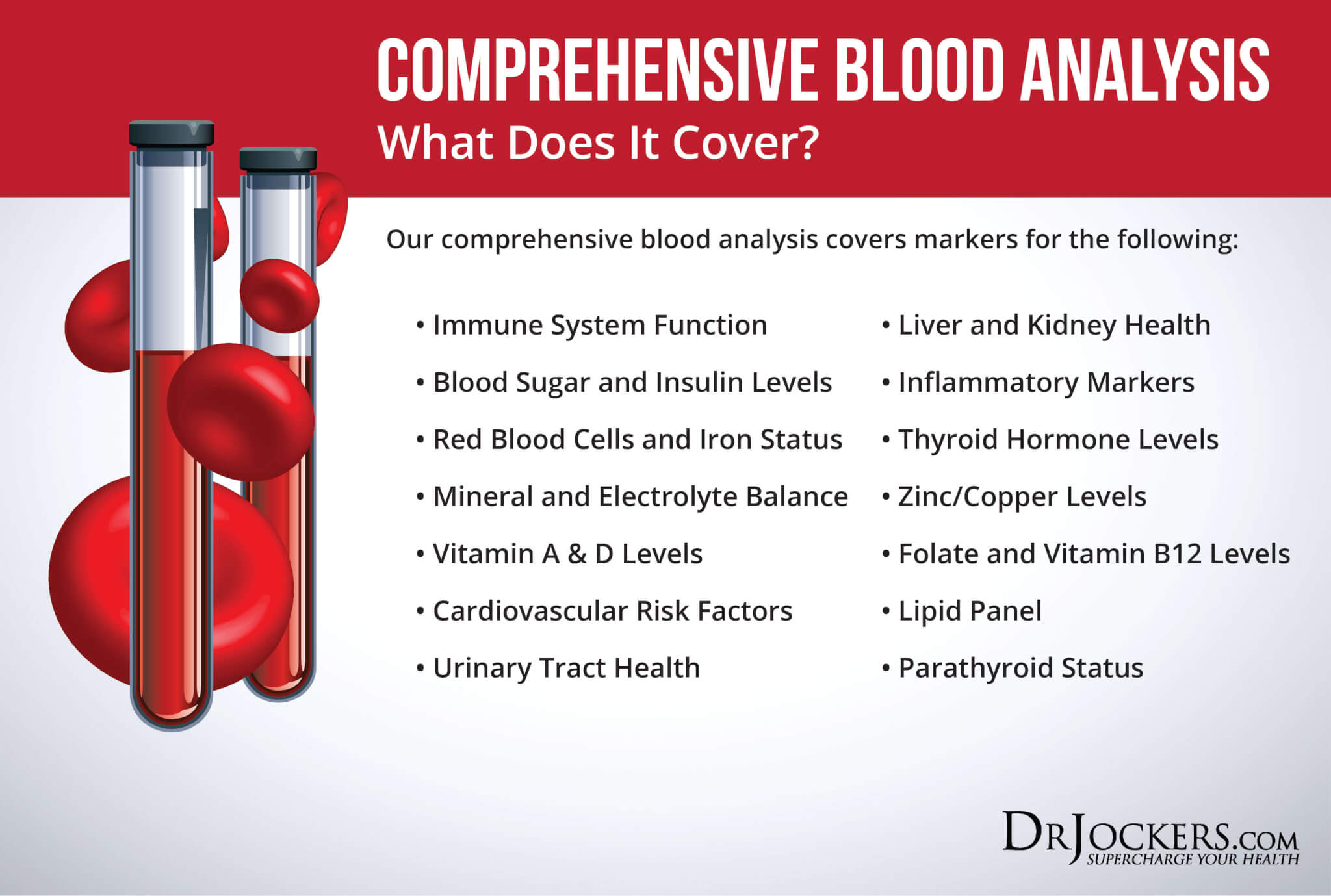
Comprehensive Blood Analysis
To look at the optimal ranges of these markers, I recommend and regularly use a Comprehensive Blood Analysis (CBA). This blood analysis is a very detailed blood test that looks at all of these markers of inflammation and other health functions.
This test is more sophisticated than most conventional doctors run. It examines all parameters for inflammation, blood sugar levels, insulin levels, immune system function, thyroid function, parathyroid hormone levels, mineral and electrolyte balance, zinc and copper ratio, vitamin A and D levels, folate and vitamin B12 levels, a complete metabolic panel, complete blood count, liver function, kidney function, urinary tract health, nutrient deficiencies, and more.
I recommend getting the Comprehensive Blood Analysis done regularly both as a preventative measure and to monitor your inflammation levels and progress if you are on a treatment plan. Remember, our team is always happy to help to understand your results and create a personalized treatment protocol to regain your health and well-being naturally.
Final Thoughts
Intestinal permeability means that your gut lining has developed some holes that can allow undigested food particles, toxins, and microbes to pass through into your bloodstream. This can increase chronic inflammation and lead to a chronic immune response. Intestinal permeability can cause histamine intolerance, chronic symptoms, autoimmunity, and other chronic health issues.
If you have symptoms of intestinal permeability or histamine intolerance, I recommend that we look at some key lab markers for intestinal permeability and histamine, GI Map Stool Test, and Comprehensive Blood Analysis. These functional lab markers can support a proper diagnosis and can also allow an individual treatment protocol to regain your health and wellness naturally.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and thrive in life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!





Hello,
My name is Irene from Canada. I have been doing Mimosa Seed and Intestinal Remover along with charcoal for parasites and leaky gut. I have incorporated a high quality collegen to plug up leaky gut. I have endured histamine reactions and have suffered facial acne for 5 years. I always try to fix this but it is up and down 🙁 Now that I have recently done your products and collegen 2x daily including no sugar and grains. What number one product or thing can I incorporate in my last week of parasite killing? I am doing pumpkin seeds daily. I have on a fixed budget and would really appreciate a really good leaky gut sealer to really make head way. I am 64 and I will take full responsibility of no testing at this time. I know I have leaky gut so I want to go for that solution first as this time. Thank you for your recommendation and time to help me. Irene I am reading your article on leaky gut these next few days. Blessings to all at drjockers.com
Sorry to hear this! I would reach out to our functional health coaches so they can help customize a plan for you: https://drjockers.com/long-distance-coaching/