
Seasonal Allergies: Symptoms, Causes and Natural Support Strategies
Seasonal allergies, often called hay fever, are symptoms that occur during specific times of the year. This usually occurs at times when outdoor molds release their spores or when plants release tiny pollen particles into the air to fertilize other plants. Allergies are an indication of a disrupted immune system. In this article, I will go over natural strategies to support your immune response.
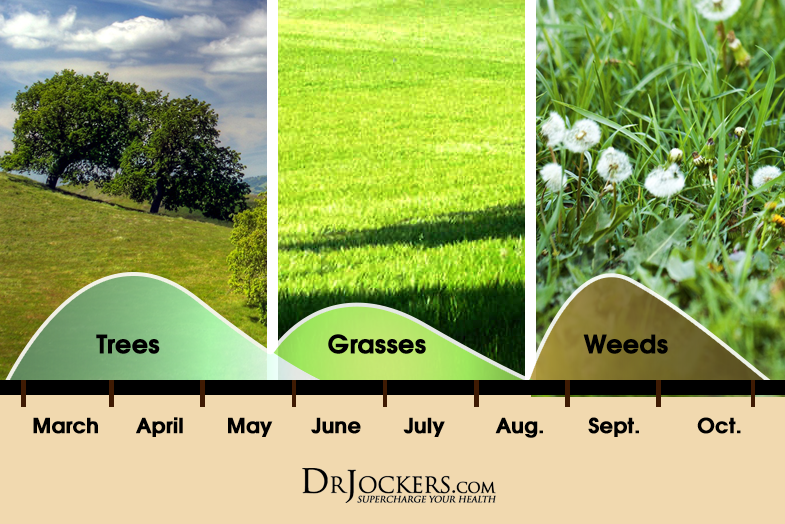
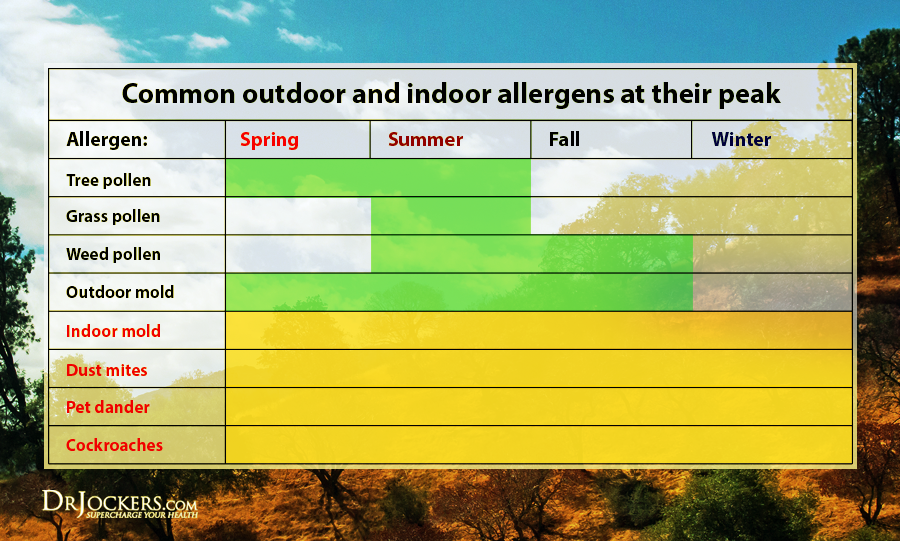
Seasonal allergies depend on what the individual is having a specific immune reaction to. In the mid-Atlantic states, tree pollination happens between February and May. Grass pollination happens in May – June and weeds from August – October. Mold spores usually increase between mid-summer through the fall. If you have stronger symptoms during one of these periods it is an indication your body is struggling with that particular particle.
Pollen and Spring Allergies:
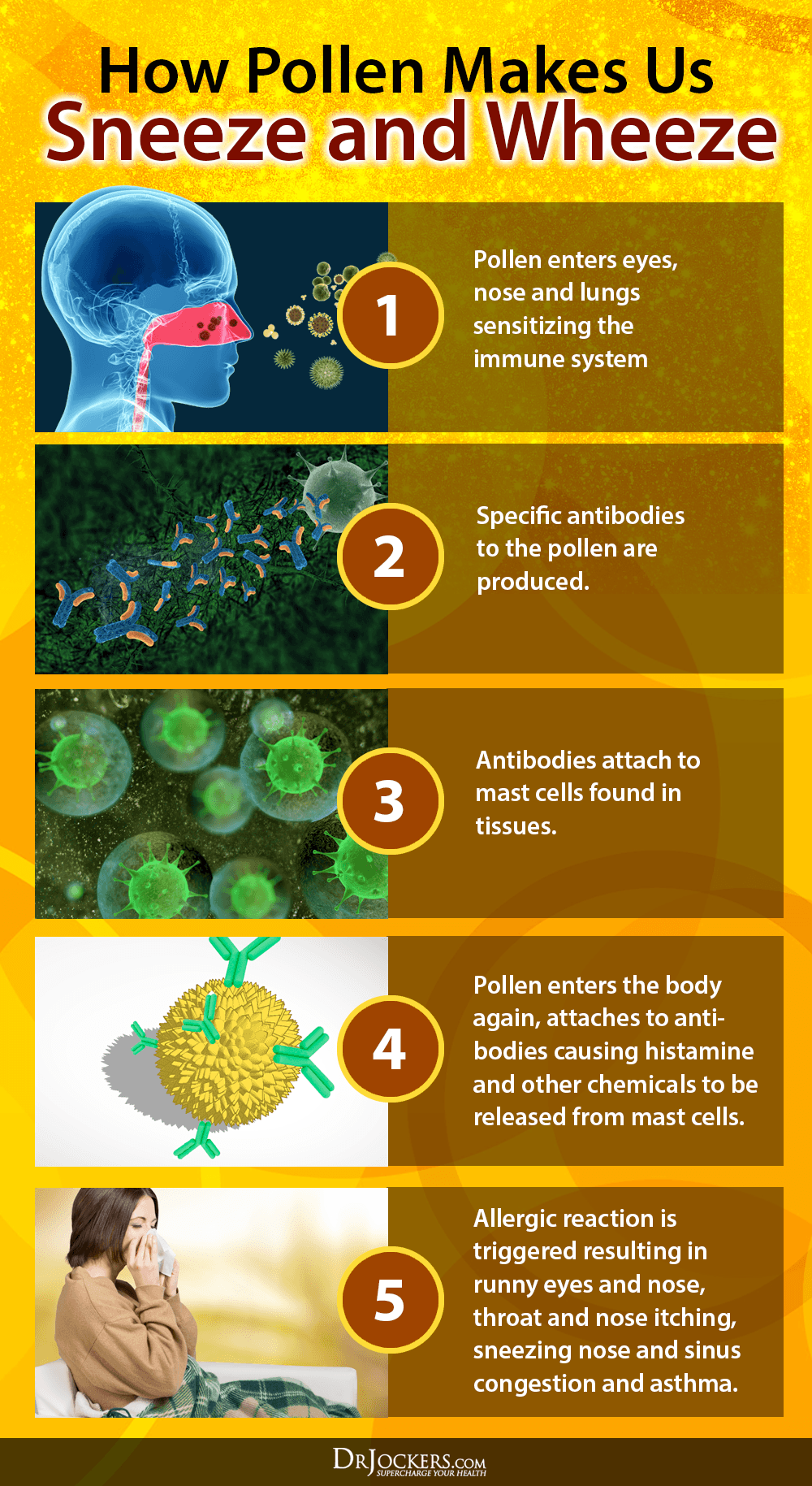
Pollens are tiny, egg-shaped powdery grains released from flowering plants, which are carried by the wind or insects and serve to cross-pollinate other plants of the same type for reproductive purposes. When pollen is present in the air, it can land in a person’s eyes, nose, lungs, and skin to set up an allergic reaction that can cause the following symptoms:
Pollen can travel long distances and the levels in the air can vary from day to day. The pollen level can be quite different in various areas of a particular city or region. Levels of pollen tend to be highest from early morning to mid-morning, from 5AM to 10AM.
Spring allergies are a result of pollen from trees, which can start pollinating anytime from January to April, depending on the climate and location. Trees that are known to cause severe allergies include oak, olive, elm, birch, ash, hickory, poplar, sycamore, maple, cypress, and walnut. In certain areas of the world, some weeds will also pollinate in the springtime.
Summer Allergies:
Grass pollen is typically the main cause of late spring and early summer allergies. Grass pollen is highest at these times, although grass may cause allergies through much of the year if someone is mowing the lawn or lying in the grass. Contact with grass can result in itching and hives in some people who are allergic to grass pollen.
Grasses can be divided into two major classes — northern and southern grasses. Northern grasses are common in colder climates and include timothy, rye, orchard, sweet vernal, red top, and blue grasses. Southern grasses are present in warmer climates, with Bermuda grass being the major grass in this category.
Fall Allergies:
Weed pollen is the main cause of seasonal allergies in the late summer and early fall. Depending on the area of North America, these weeds include ragweed, sagebrush, pigweed, tumbleweed (Russian thistle), and cocklebur. In certain areas of the world, some trees can pollinate in the fall as well.
Other common allergens include indoor molds, dust mites, pet dander, and cockroaches. These 4 can occur all year long and won’t typically change with the seasons. It is good to identify which of these are your major allergens so you minimize your exposure to them.
MalCoordinated Immunity:
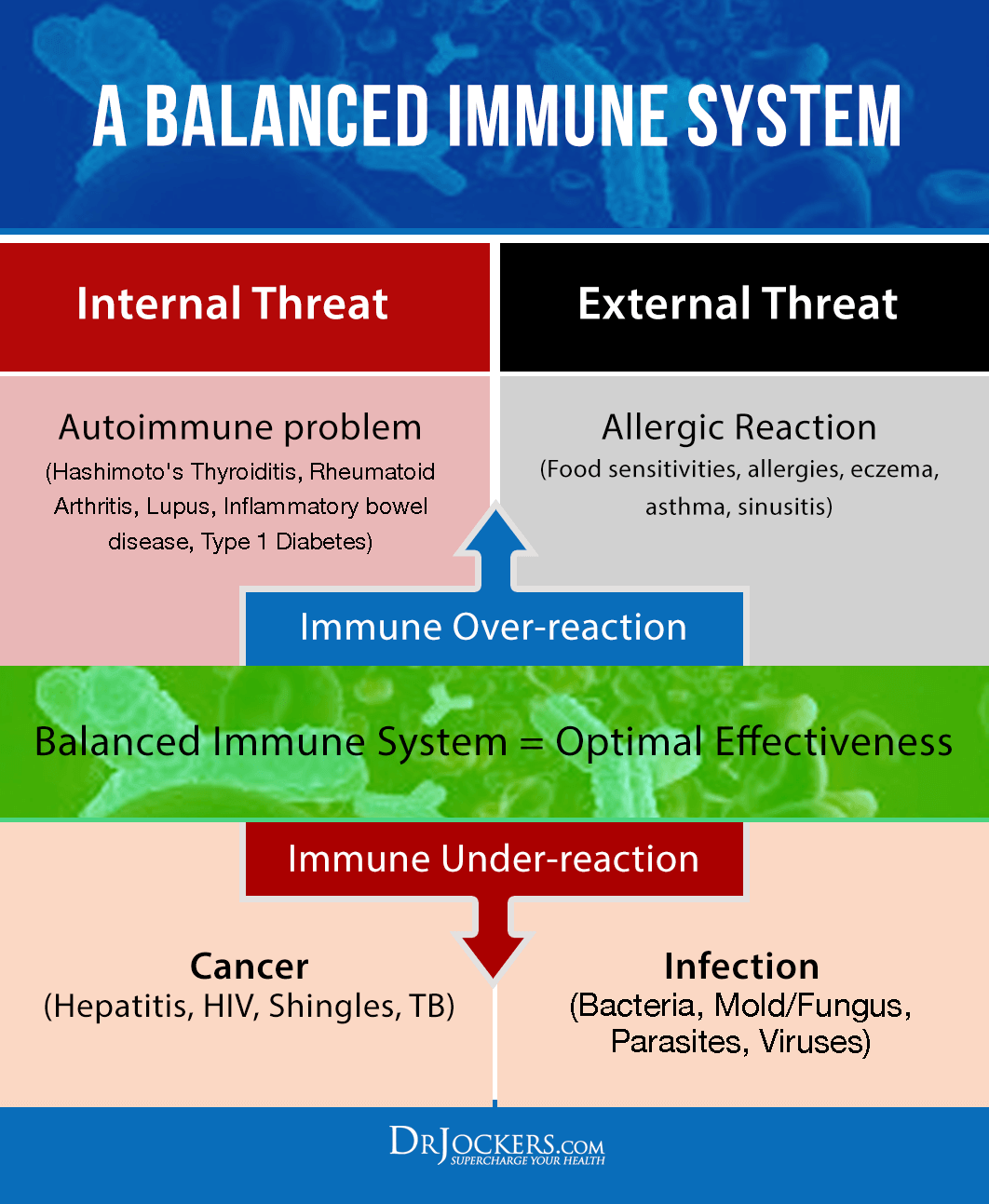
Allergies occur when the immune system is malcoordinated. This can occur from some major bodily stressor that interferes with the natural maturity and function of the immune system.
Due to environmental challenges early in life, many individuals never develop a normal immune response and are prone to allergic reactions throughout their lives. Others encounter some sort of an immune insult during their life that throws their immune system out of control.
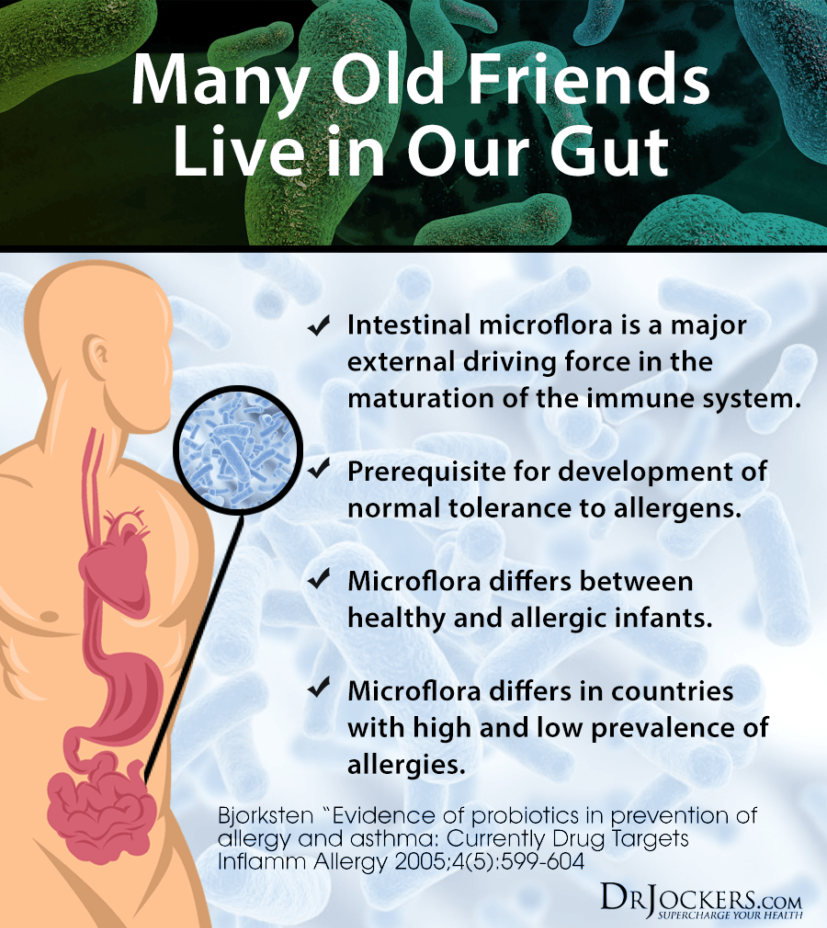
One of the most common issues is an altered gut microflora. The gut microflora is responsible for 70% of our body’s innate immune response (1, 2, 3). The natural makeup should help the body recognize between safe environmental particles (pollen, dust, weeds, etc.) and unsafe environmental particles (bad bacteria, bad yeast, and viruses).
When the gut microflora is altered early in life it can create an immune malcoordination where the immune system is oversensitive to safe environmental particles. This may lead to seasonal allergies in some and autoimmunity and/or chronic inflammatory conditions such as asthma in others (4, 5, 6).
Environmental Insults to Immunity:
The main things that insult the body’s microflora include the mother’s microflora at birth, caesarian delivery, genetically modified foods in mom and baby’s diet, breastfeeding vs formula feeding, vaccinations, physical trauma to the child, and antibiotic usage.
Some of the most common and controllable issues include a poor diet early in life and the use of antibiotics both for medical reasons and in food products. Most commercial farms give antibiotics to their animals which then end up in our meat and dairy. These antibiotics throw off our microflora balance and disrupt the immune system.
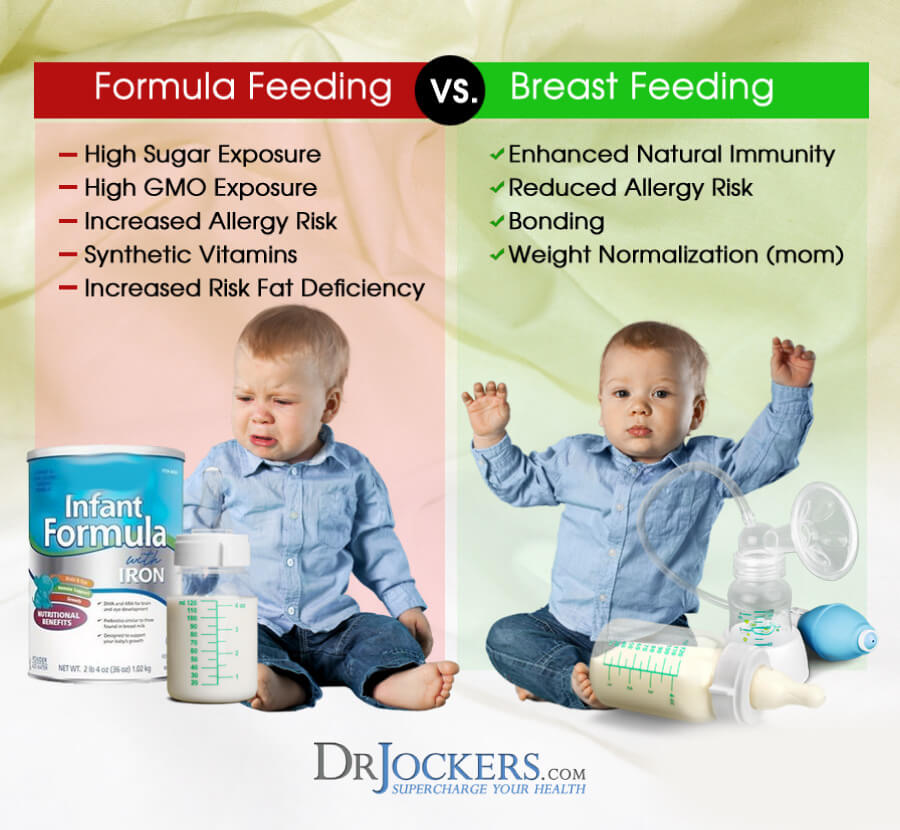
When mom and child are consuming genetically modified foods that are high in environmental chemicals it alters the microflora balance (7, 8). The use of processed infant formulas also contributes to the development of an altered and unhealthy microbiome in the child (9).
Vitamin D, Probiotics and Omega 3’s:
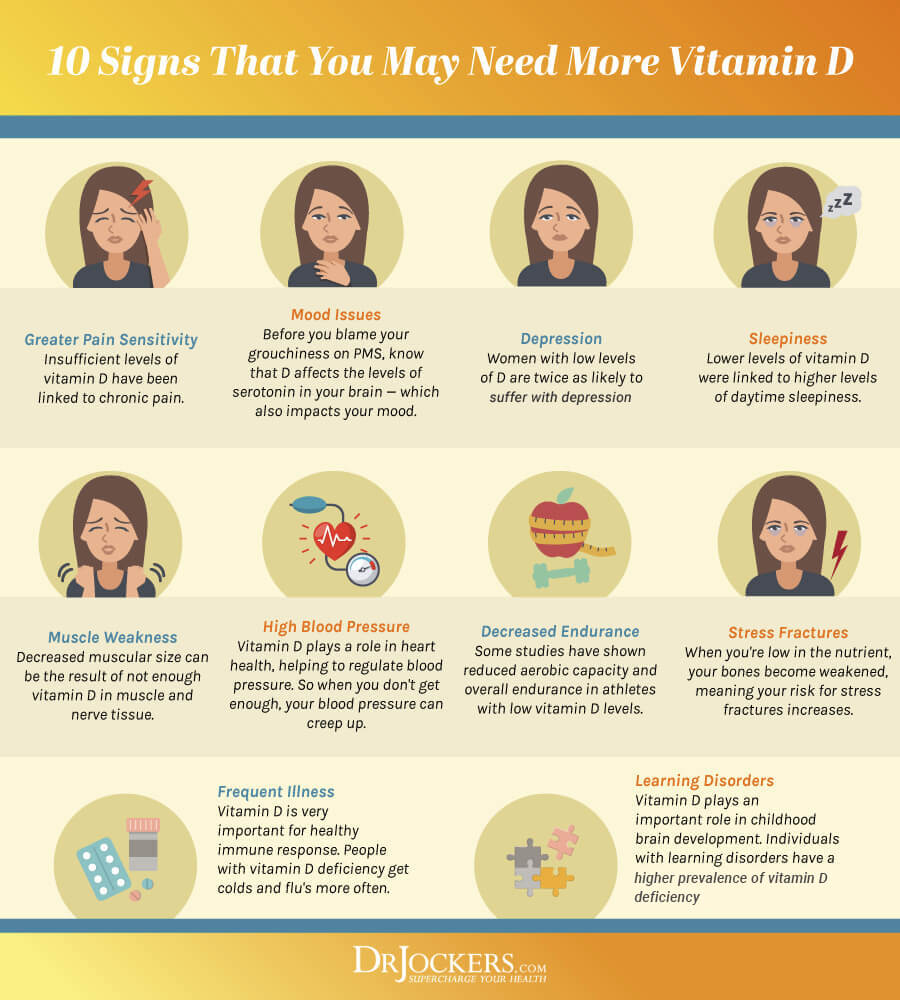
There are some great strategies a family could take to ensure that children will develop early in life with a healthy immune response. Mom should begin by optimizing her vitamin D3 levels to 60-100 ng/ml. Most often this requires supplementation of 5,000-10,000 IU daily along with a small amount of vitamin K2.
She should also boost her microbial friends by eating raw fruits & vegetables, fermented foods, and taking probiotic supplements. This will help nourish her microbiome and provide the proper immune control for a healthy child.
She should stabilize her omega 6 to omega 3 fatty acid ratios by eating grass-fed meats and wild-caught fish and purified fish oil supplements. She should completely avoid processed foods and foods cooked with inferior vegetable oils.
Breast Fed Babies and Allergies
The newborn baby should be exclusively breastfed for at least the first 6 months and ideally the first 12-18 months. Mother’s milk provides valuable immunoglobins early in life that play an enormous role in supporting the infant’s immune system as it matures (10).
Mother’s milk is also a rich source of medium-chain saturated fats such as lauric acid that help feed and strengthen immune cells. Mother’s milk provides IgA and probiotics which inoculate the baby’s gut and give it a defense against dangerous intestinal microbes that can cause damage to the gut lining (11).
Vaccinations Increase Risk of Allergies:
Vaccinated children are much more susceptible to allergies. In fact, a 2010 study found that 40% of vaccinated children reported having at least one allergy whereas less than 10% of children who were not vaccinated reported an allergy. The same study showed that almost 11% of vaccinated children have seasonal allergies whereas only 2.5% of non-vaccinated children have this condition (12).
Vaccines act to strengthen the adapted or acquired part of our immune system led by antibody formation. Within this system, there are the Th1 and Th2 branches. Vaccines are thought to over stimulate the Th2 branch of the adapted immune system creating an immune imbalance that leads to hyperinflammatory conditions that may prelude allergies for certain individuals (13).
 Nutrition and Seasonal Allergies:
Nutrition and Seasonal Allergies:
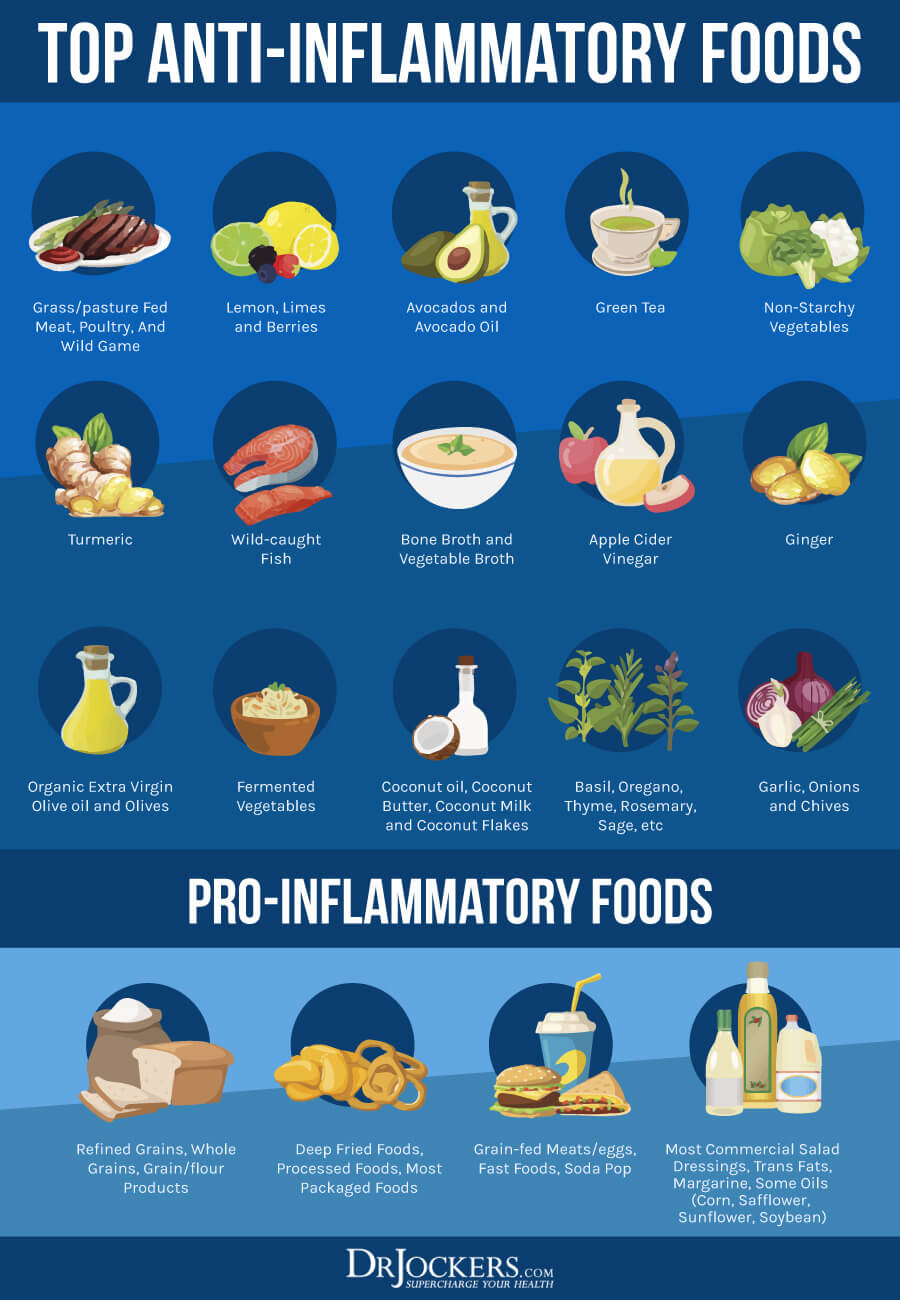
Beating allergies includes an anti-inflammatory diet and lifestyle. This is done by rebuilding the intestinal wall with probiotics and fermented foods. De-inflaming the body by avoiding inflammatory foods and consuming whole foods rich in omega-3 fatty acids and antioxidants.
The most common foods that should be avoided include gluten, dairy, peanuts, soy, corn, sugar & vegetable oils (corn, soy, cottonseed, canola, peanut). The diet should be rich in chlorophyll-rich veggies and bioflavonoid-rich fruits and veggies such as onions, lemons, limes, grapefruit, berries, and herbs of all kinds.
The diet should also be rich in healthy immune-enhancing fats such as coconut oil, grass-fed butter or ghee, olives, olive oil, and avocados. Sustainably raised animal products such as grass-fed beef and lamb, organic poultry, and wild-caught fish should be consumed regularly on this nutrition plan.
5 Key Supplements To Support The Immune System:
These supplements are some of the very best to support the immune system and reduce hypersensitivity. They are not FDA-approved to prevent, mitigate, treat, or cure allergies and should not be confused as such. However, they are very good for promoting a healthy immune response.
1. Vitamin D3: Vitamin D3 is crucial for immune coordination in the body. Low levels of vitamin D3 are associated with chronic inflammation and allergies (14). I recommend getting high-quality sun exposure regularly or supplementing with 1,000 IU of vitamin D3 with 4.5 mcg of K2 per 25 lbs. of body weight daily.
2. Probiotics: Probiotics play an important role in the gut microbiome and immune coordination. There are studies have shown that supplemental probiotics are very effective at reducing allergy symptoms (15). Some people find great relief by using probiotics.
3. Quercetin & BioFlavonoids: Quercetin, dihydroquercetin (DHQ) and rutin are active bioflavonoids that modulate an exaggerated immune response. Bioflavonoids work synergistically with other antioxidants to protect tissues from the negative effects of oxidation and inflammation often observed during hyperimmune reactions (16).
4. Bromelain: Bromelain is an enzyme complex extracted from the stem and fruit of the pineapple. Its modulation of the inflammatory response is thought to exert a beneficial effect in combating hypersensitive immune reactions (17) Studies identified its positive effects on controlling edema, tissue permeability, and vasodilation (18). Bromelain is also found to enhance the absorption of quercetin (19).
5. Stinging Nettle: Stinging nettle leaf has been found to regulate a variety of inflammatory activities associated with hyperimmune response, including mast-cell degranulation, prostaglandin formation, and histamine action (20, 21)
We have a supplement called Allergy Defense that combines vitamin C, quercetin, stinging nettle, bromelain, and bioflavonoids to help the immune system deal with seasonal challenges. Again, this supplement is not FDA-approved to prevent, mitigate, treat, or cure seasonal allergies but it can be used to help support the immune system.
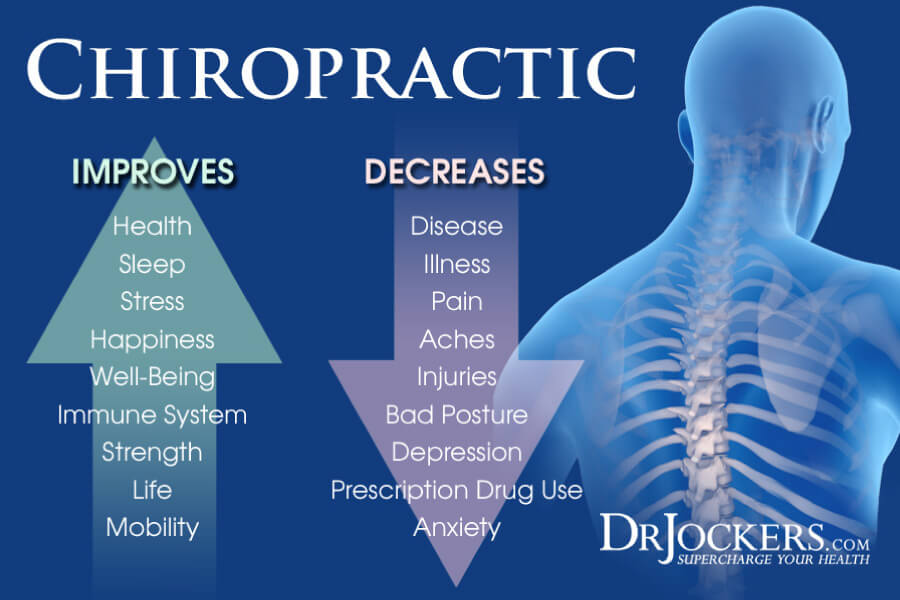
Chiropractic Care and Immunity:
Physical trauma to the upper cervical spine can impact the developing immune system of an infant or child. This form of trauma could include a slip or fall, a car accident, bad sleeping habits, or poor posture. This leads to an upper cervical (neck) subluxation that puts pressure on the brain stem. Upper cervical subluxations lead to malcoordinated immunity and allergic reactions in many individuals (22, 23, 24).
Chiropractic care to remove upper cervical subluxations and restore proper structural and neurological function to the spine and nervous system is especially critical. This includes very specific adjustments applied to release pressure on the brain stem region and specific exercises to maintain this correction and improve postural abnormalities.






Please Docter did using allergy definse effect person with liver or diebetic problem
Yes, Ghania, the Allergy defense is safe for people with diabetes or liver problems. It will actually help them to heal from these conditions.
I have a 9 year old with allergies: mostly runny/stuffy nose, sneezing, and itchy eyes. If I can only purchase one, which of your supplements would be best for him? The D3/K2 or the Allergy Defense?
Thank you.
Hi Jane, Adequate vitamin D levels are essential to immunity and brain development in children. The optimal source of vitamin D3 is from regular sunlight exposure. Allergy Defense combines a unique formulation designed to support the immune system in combating those very symptoms due to known seasonal allergies. However, it is always best to consult with a functional health practitioner that will help you customize a specific plan for your child and understand the root cause of the allergies. This article can help: https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/
My roommate gets a headache and a skin rash (dermatitis) that flares up that she thinks is from mold from the house we live in. Other people have lived here, no issues. We are going to test for mold…but what else in the house can be causing this…radon?
Also, what can she eat specifically or do to boost her immune system to fight (lets assume its mold)? Is it the same products listed above to fight allergies? The nettle and the probiotics, and D3 etc?
And is there anyway medically that it can be proven that its mold that is making her sick? A skin sample? A blood sample (everybody has mold in their blood tho). Scrape her skin dermatitis and send it to a lab….anything?
Thank you,
Rich
Hey Rich, I am so sorry to hear that she is experiencing these health problems. This article offers specific information on mold allergens including symptoms, detection and a protocol recommendation.
Hi doctor , you suggest to eat fermented food to boost the immune system but these are high in histamine , is it ok to eat these kind of foods with seasonal allergies ?
Great question Sara! Some people with seasonal allergies do great with fermented foods while others really need a low histamine diet. You just have to try it out and see if you feel better or not.