 Women’s Health Guide: Overcome 7 Common Female Health Concerns
Women’s Health Guide: Overcome 7 Common Female Health Concerns
Women’s health is very important. Women go through different hormonal shifts than men. There are a number of women’s concerns that men don’t experience. Women are also at a higher risk of various symptoms and health issues, often due to the major hormonal transitions between puberty and menopause. Let’s talk about women’s health and how to overcome 7 common female health concerns.
In this article, I will go over the importance of women’s health and how it affects perimenopause. I will go over the top 7 common female health concerns. You will understand the major root cause factors of women’s health issues. I will share my top natural support strategies to support women’s health and well-being.
Women’s Health and Perimenopause
It’s no surprise to say that male and female bodies are different. Beyond the more obvious physical characteristics, there are some major hormonal differences. This means that certain health issues only affect women. Other health issues may affect women differently or put them at higher risk than men.
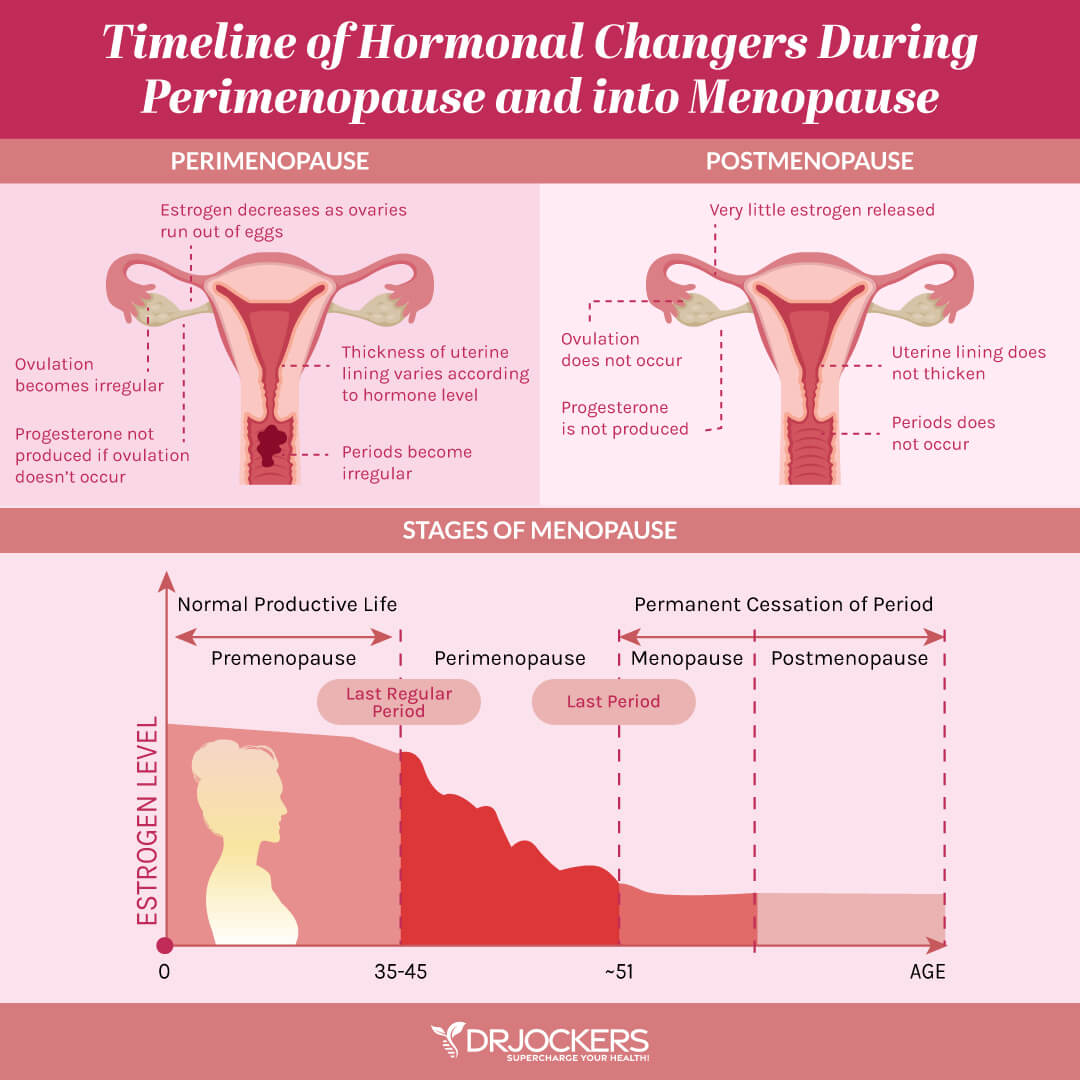
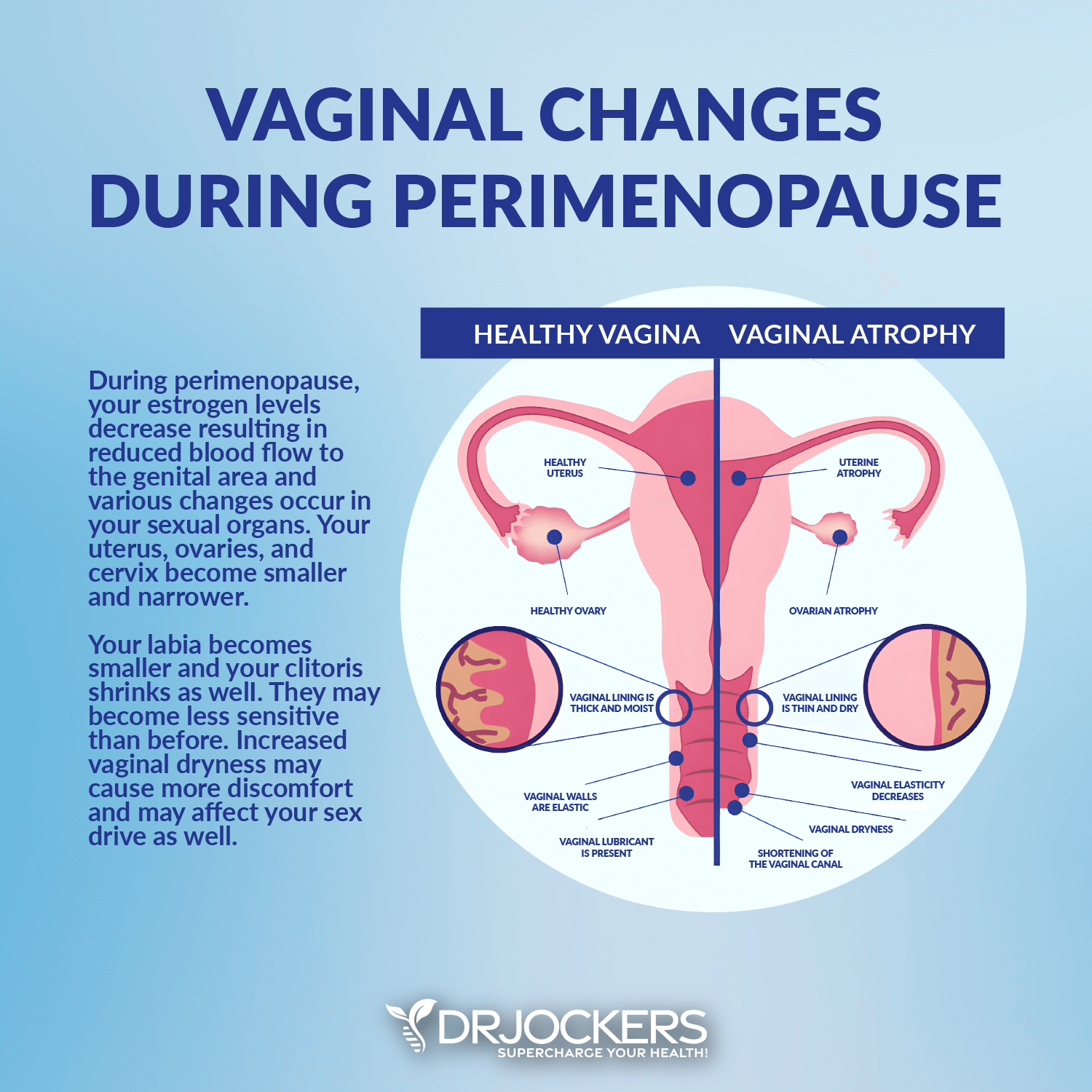
Perimenopause and menopause are times of hormonal shifts that can increase women’s health issues and symptoms. Menopause is the end of a woman’s menstrual cycle. It happens when a woman has gone for 12 months without a period without any other cause, such as amenorrhea. The average age of menopause is 51.
Perimenopause is the transitional period leading up to menopause that can last for several years to even over a decade. Most women notice symptoms of perimenopause sometimes in their 40s, but some may even notice them in the mid-30s. Perimenopause is characterized by uneven fluctuations of the estrogen hormone that lead to the lengthening or shortening of the menstrual cycle. It may lead to periods without ovulation. It can cause symptoms similar to menopause, including hot flashes, fatigue, sleep issues, and vaginal dryness.
7 Common Female Health Concerns
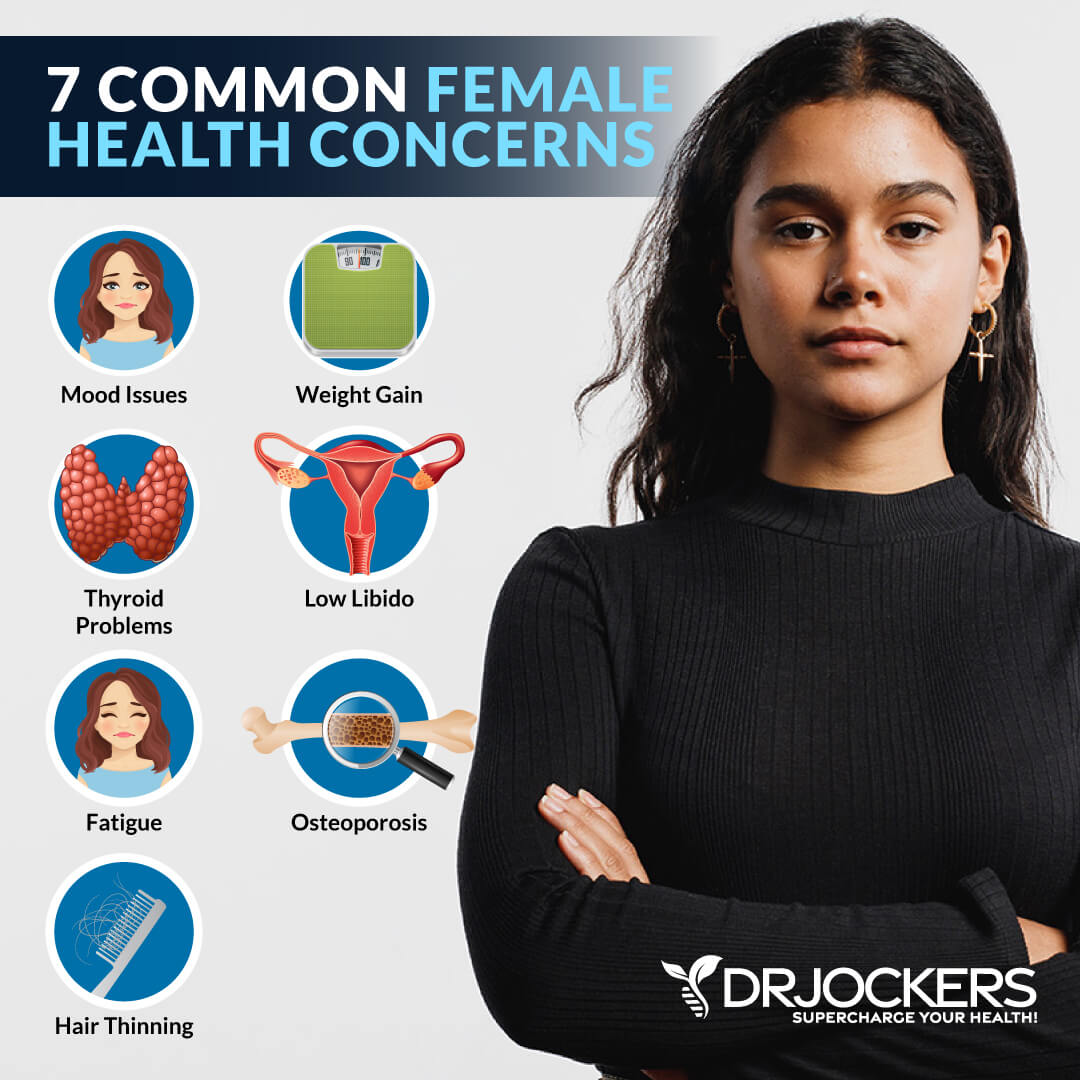
There are 7 common women’s health concerns you need to understand:
Mood Issues
Mood issues, such as anxiety and depression, are not unique to women only. However, hormonal shifts and women’s health issues can increase the risk and influence mood fluctuations. Many women, for example, experience mood shifts before menstruation or as a symptom of perimenopause or menopause. Postpartum depression and anxiety are also common concerns.
A 2011 study published in the Journal of Psychiatric Research has found that anxiety, depression, and bulimia nervosa are more common in women than men (1). A 2017 review published in Focus has found that anxiety disorders may be more prevalent in women due to a combination of hormonal differences and hormonal shifts, stressors, including trauma more prevalent in women than men, and remunerative cognitive style coping with emotional distress (2).
A 2019 study published in Frontiers in Psychology has found that estradiol fluctuations during the menopausal transition can increase sensitivity to stress and cause symptoms of depression (3).
Weight Gain
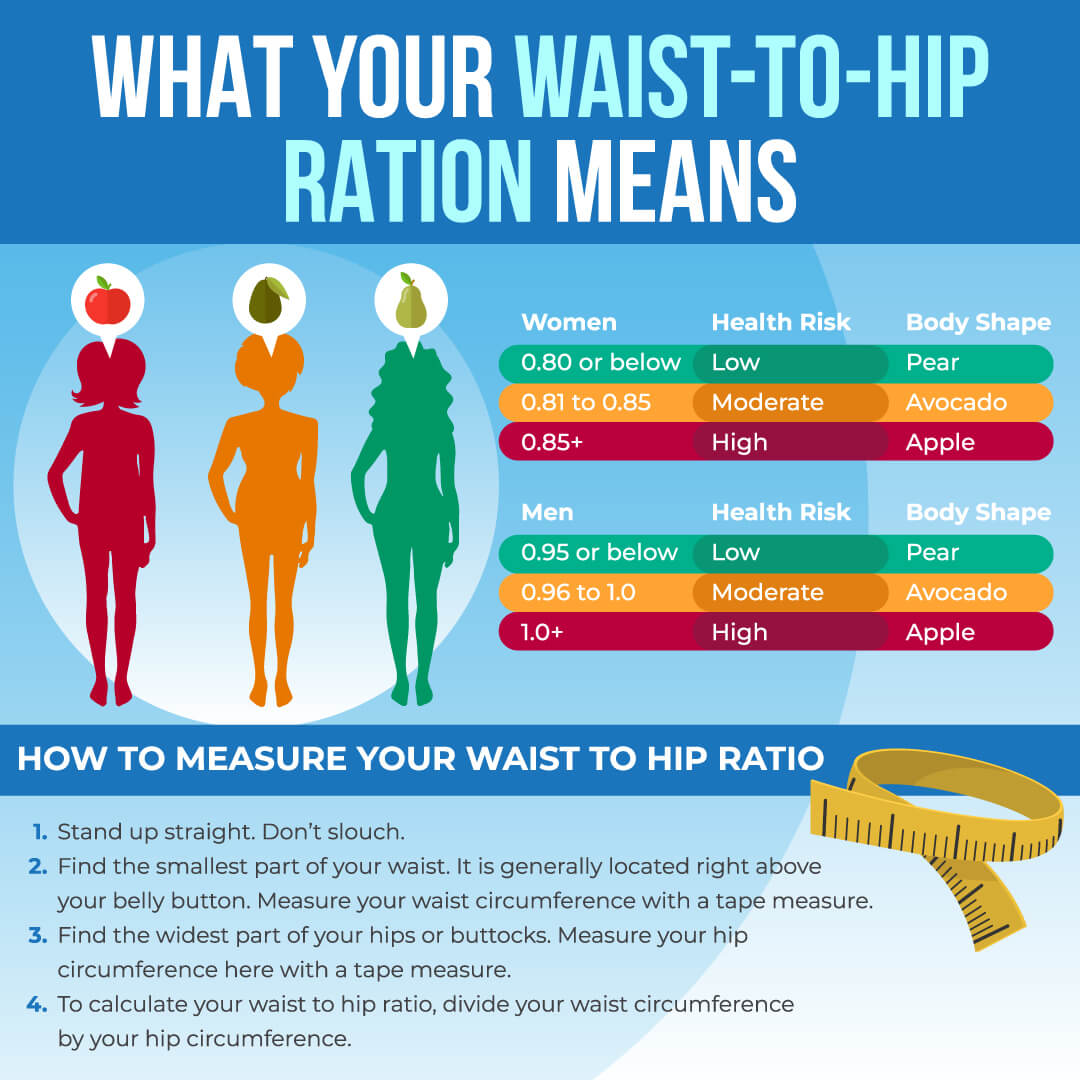
Weight gain is another health concern that happens to both men and women. However, weight gain in women is often connected to hormonal changes and is a common women’s health concern during and after perimenopause and menopause.
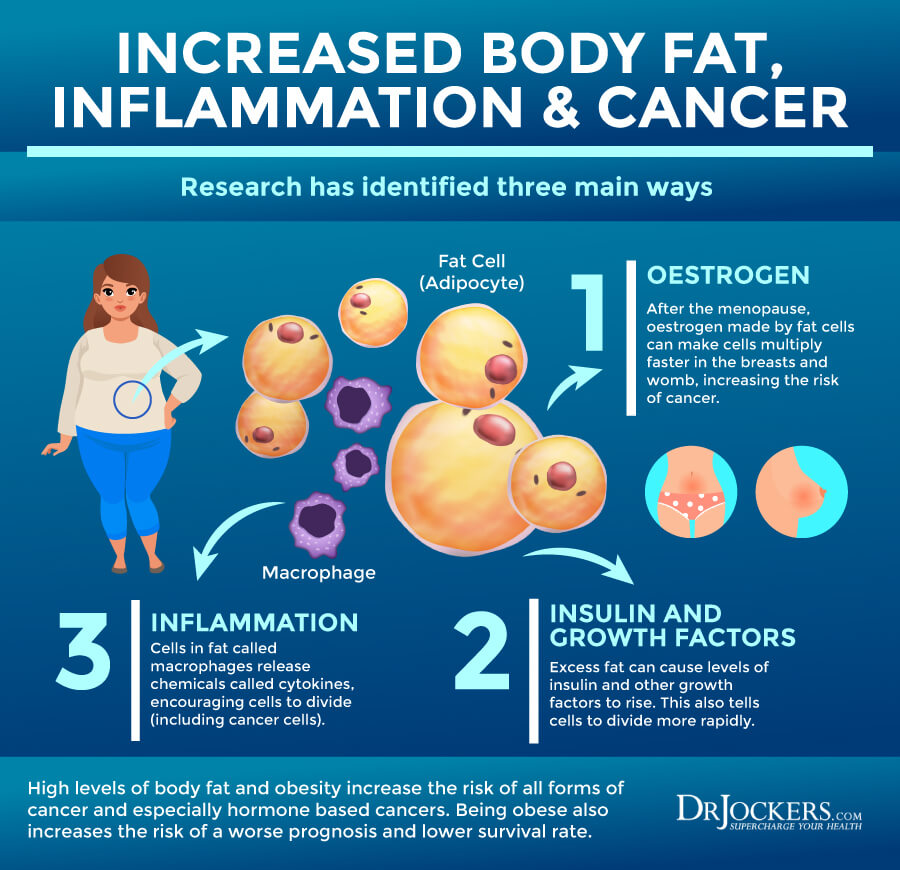
A 2014 study published in Biomedical Research International has found that reduced estrogen levels due to menopause can increase the risk of abdominal fat and obesity (4). A 2017 review published in Concise Review for Clinicians has found that weight gain in women is common during midlife and can increase the risk of various health issues, including cardiovascular disease, hypertension, hyperlipidemia, and blood sugar issues (5).
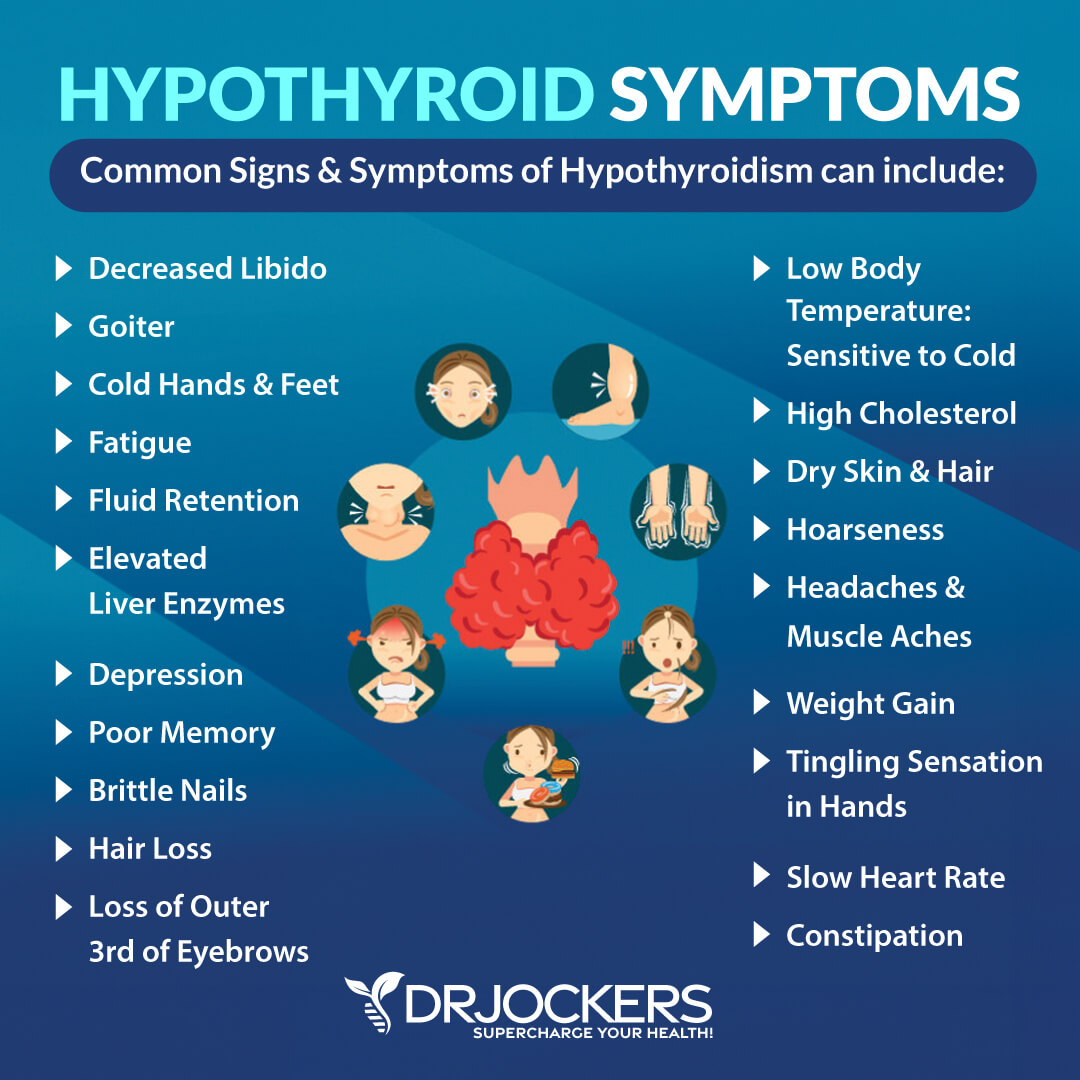
Thyroid Problems
The thyroid is a butterfly-shaped gland found at the front of your neck. It makes thyroid hormones which are critical for metabolic, digestive, muscle, bone, and brain health. Thyroid problems are common in women. They often go hand in hand with other hormonal imbalances. Thyroid problems can affect other hormones in your body and can cause abnormal menstruation, including missing periods, late periods, or heavy periods. On the other hand, estrogen also affects the thyroid.
According to a 2011 study published in the Journal of Thyroid Research, understanding the role of estrogen may be a key element to understanding thyroid health (6). Estrogen triggers the production of thyroglobulin, a thyroid precursor hormone.
Too much estrogen or estrogen dominance can lead to too much thyroglobulin and an enlarged thyroid. Too little estrogen can cause too little thyroglobulin leading to other thyroid issues. No wonder that hormonal fluctuations throughout a woman’s life, especially during perimenopause, may increase the risk of thyroid problems.
Low Libido
Low libido can occur for a variety of reasons, including physical and emotional factors. It can become increasingly common during perimenopause and menopause. A 2000 study published in The Permanente Journal has found that low libido, difficulty with orgasms, and lower frequency of sex are connected to a variety of factors (7).
These factors may include biological factors, such as lower testosterone and hormonal changes, mental and emotional issues, such as depression and other psychiatric illness, cultural issues, such as societal attitudes towards aging and older women, and interpersonal problems, such as relationship issues.
Other hormonal issues that affect women, including polycystic ovarian syndrome (PCOS) and endometriosis, can lead to low libido as well. PCOS is a condition caused by hormonal imbalance and metabolic issues that may lead to menstrual irregularity, pain, acne, excess hair growth, obesity, and low libido. A 2019 study published in the Journal of Psychosexual Health has found that women with PCOS had a lower sexual desire and more difficulties with sexual arousal (8).
Endometriosis is a painful condition that impacts many women. Tissue that’s normally grown inside your uterus grows outside of it, impacting the ovaries, fallopian tubes, and the tissue lining of the pelvis that may affect the menstrual cycle, sexual function, and libido. According to a 2020 review published in Facts, Views, and Vision in ObGyn, endometriosis can lead to problems with sexual function and relationship difficulties (9).
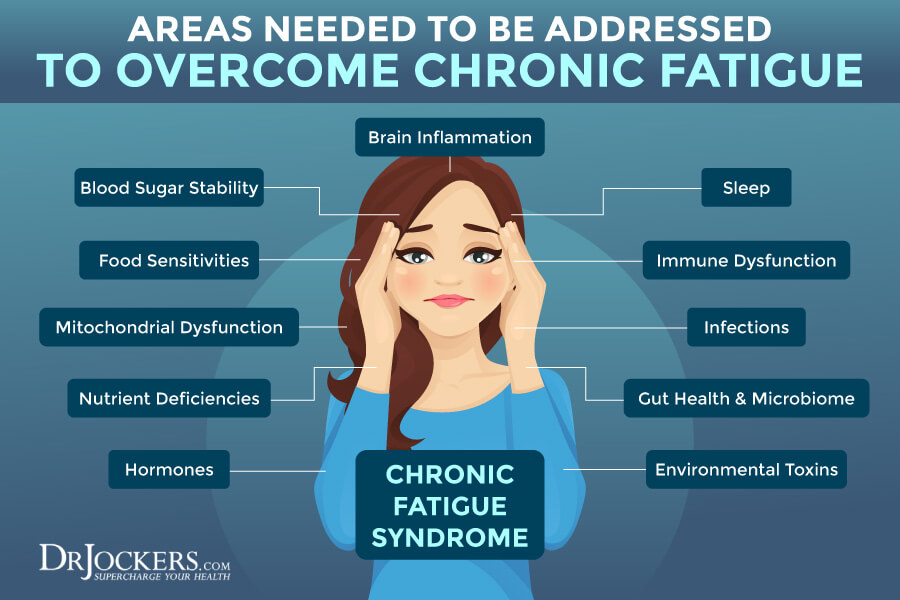
Fatigue
Fatigue may develop due to physical, emotional, environmental, and lifestyle factors. Fatigue and trouble sleeping are common symptoms in women during the perimenopausal and menopausal transition. Hormonal fluctuations and reduced levels of progesterone can decrease the ability to relax, affect the brain, and interfere with sleep.
According to a 2019 study published in the Journal of Menopausal Medicine, having trouble falling asleep, waking too early, and frequent awakenings are common during menopause (10). This may be caused by a variety of factors, including vasomotor symptoms, ovarian hormone changes, restless leg syndrome, periodic leg movement syndrome, and obstructive sleep apnea.
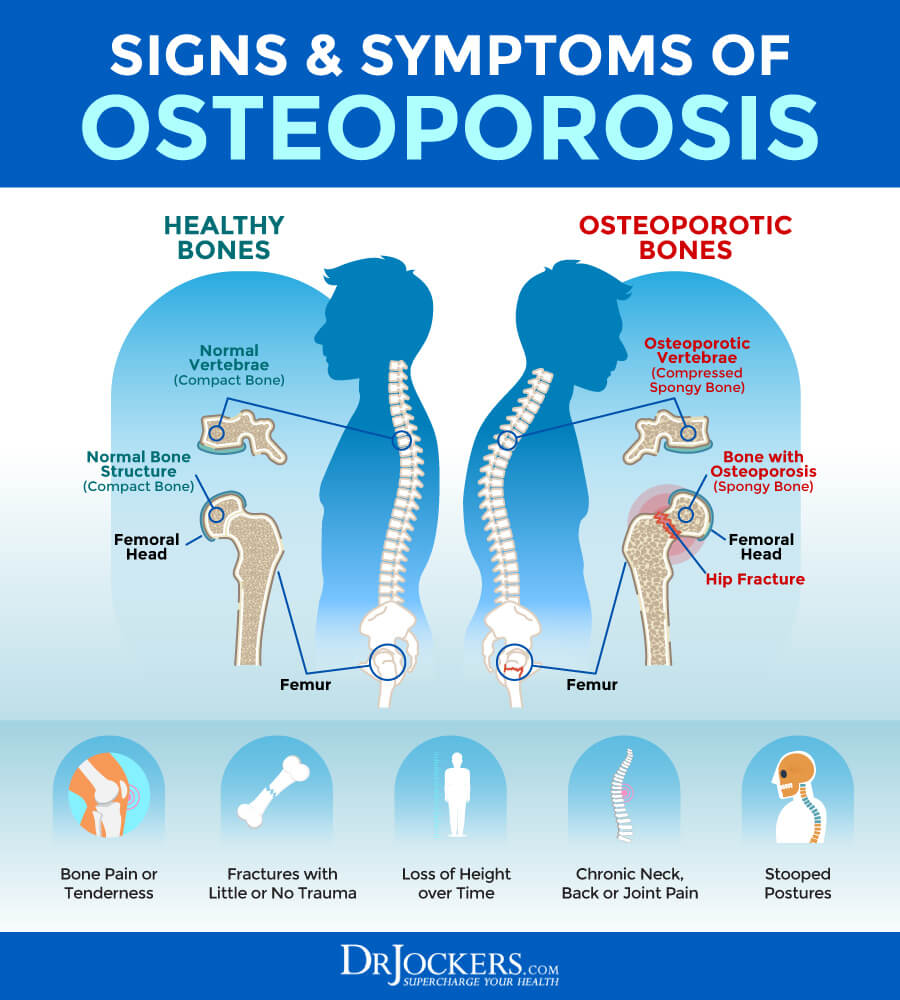
Osteoporosis
Osteoporosis is a disease that is characterized by thin, weak, and fragile bones that can fracture easily, usually in the hip, spine, and wrist. Poor nutrition, smoking, hyperthyroidism, certain medications, eating disorders, certain chronic health issues, and other factors can increase the risk of osteoporosis. Low estrogen and menopause also increase the risk of osteoporosis.
A 2015 study published in the Journal of Midlife Health has found that decreased estrogen levels can increase the risk of osteoporosis in menopausal women (11). A 2015 study published in Chronic Diseases in Translational Medicine has found that menopausal hormone therapy may reduce the risk of osteoporosis (12).
Hair Thinning
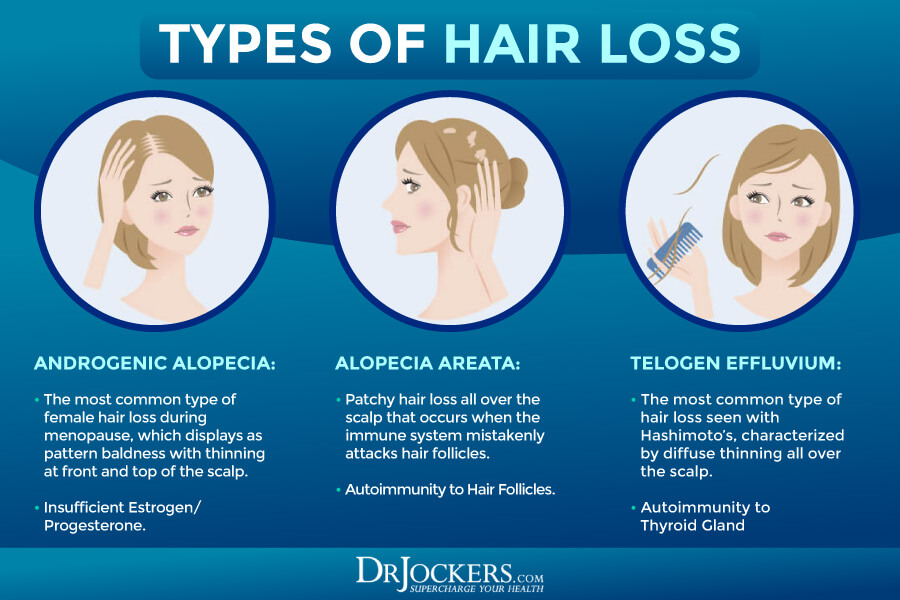
Hair thinning is a common concern in women’s health that is often caused by hormonal shifts. Many women experience hair thinning after giving birth. Hair thinning is also a common women’s health complaint during perimenopause and menopause.
During perimenopause and menopause, hormonal shifts and a decrease in estrogen is often the culprit behind hair thinning. However, stress, lack of certain nutrients, or other illnesses may also play a role. A 2016 review published in Menopause Review has found that poor nutrition, especially the lack of amino acids, vitamins, including vitamin C and A, and B vitamins, and minerals, including zinc, magnesium, calcium, iron, copper, selenium, and silicon can all influence hair thinning in menopause (13).
Major Root Cause Factors
Understanding the major underlying factors behind women’s health issues is critical for finding natural solutions. Let’s get into it.
Insulin Resistance & Dysglycemia
Insulin resistance means that your body cannot respond to insulin as it should, and it cannot use blood glucose as it should for energy. This means that your pancreas has to start making more and more insulin to keep up. Over time, this will make your blood glucose levels go up, leading to all kinds of problems.
Insulin resistance can lead to blood sugar imbalances, prediabetes, diabetes, and all kinds of chronic health issues. Dysglycemia means that your blood sugar levels go either go too low or too high. Dysglycemia is common in diabetes.
A 2017 review published in Concise Review for Clinicians has found that weight gain in women around menopause can increase the risk of various health issues, including cardiovascular disease, hypertension, hyperlipidemia, and blood sugar issues (5). A 2009 article published in Current Opinions in Obstetrics and Gynecology has found that insulin resistance, type 2 diabetes, and gestational diabetes can increase health risks in women (14).
A 2021 study published in the Journal of Women’s Health has found that dysglycemia can affect pregnancy outcomes, including the health of the mother and the baby (15). A 2013 study published in Diabetes Care has found that dysglycemia is common post-menopause and may increase the risk of weight gain and diabetes (16).

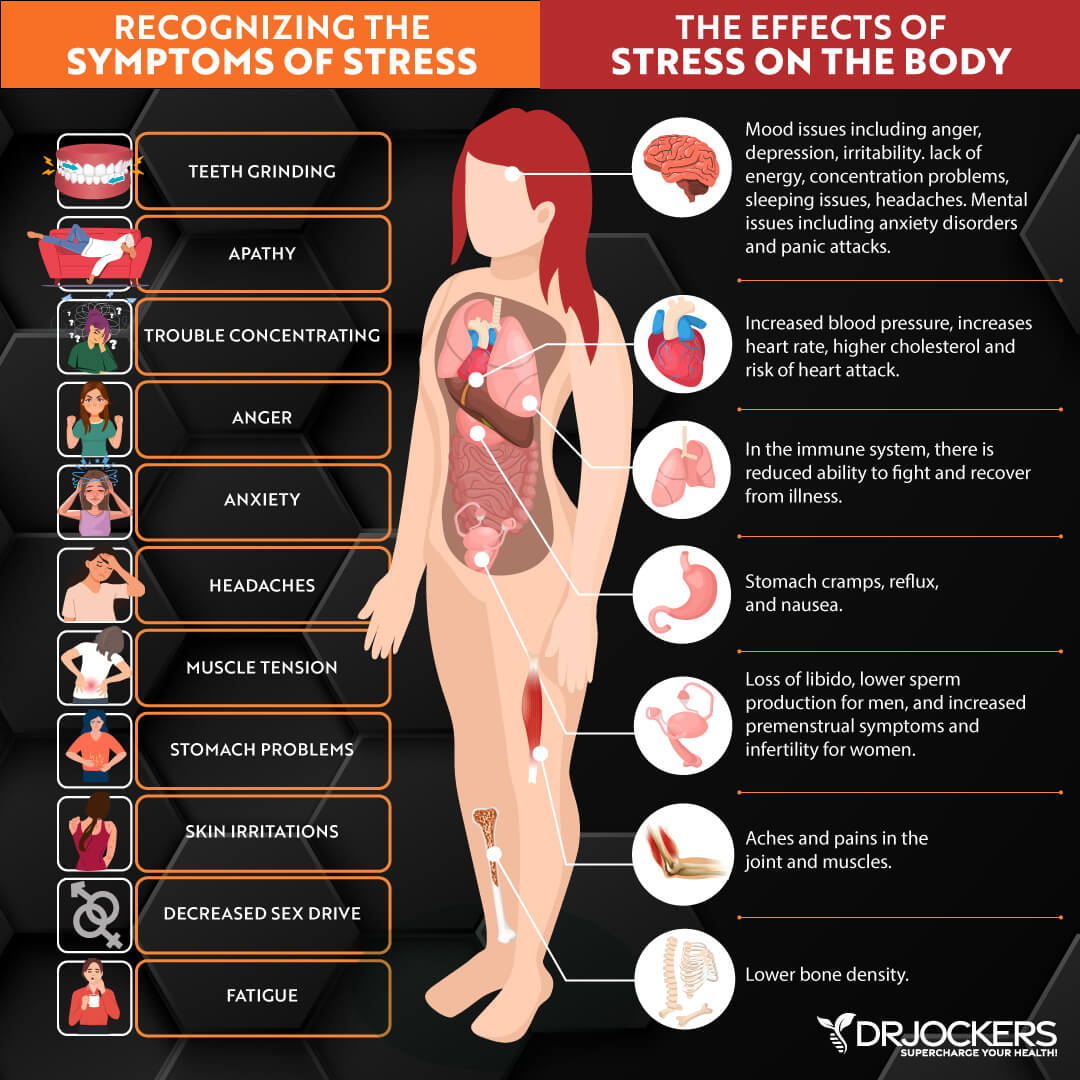
Chronic Stress & Poor Sleep
Chronic stress and poor sleep can increase chronic inflammation, gut microbiome imbalance, hormonal imbalance, pain, chronic symptoms, and chronic health issues. Thus, chronic stress and poor sleep may impact women’s health. A 2019 study published in the Journal of Menopausal Medicine has found that having trouble falling asleep, waking too early, and frequent awakenings are common during menopause (10).
According to a 2018 study published in the Archives of Sexual Behavior, stress is more likely to lower the libido of women than men (17). A 2015 study published in the Journal of Sexual Medicine has found that poor sleep can also negatively impact sexual behavior, libido, genital response, and partnered sexual activity in women (18).
A 2021 study published in BMC Women’s Health has found that hot flashes, sweating, depression, and anxiety associated with perimenopause, menopause, and postmenopause may affect sleep quality (19). Sleep quality itself can also increase depression, anxiety, fatigue, and other perimenopausal and menopausal symptoms. A 2010 study published in the Journal of Midwifery and Women’s Health has found that perceived stress can impact the symptoms of menopause and influence the attitude towards aging and menopause (20).
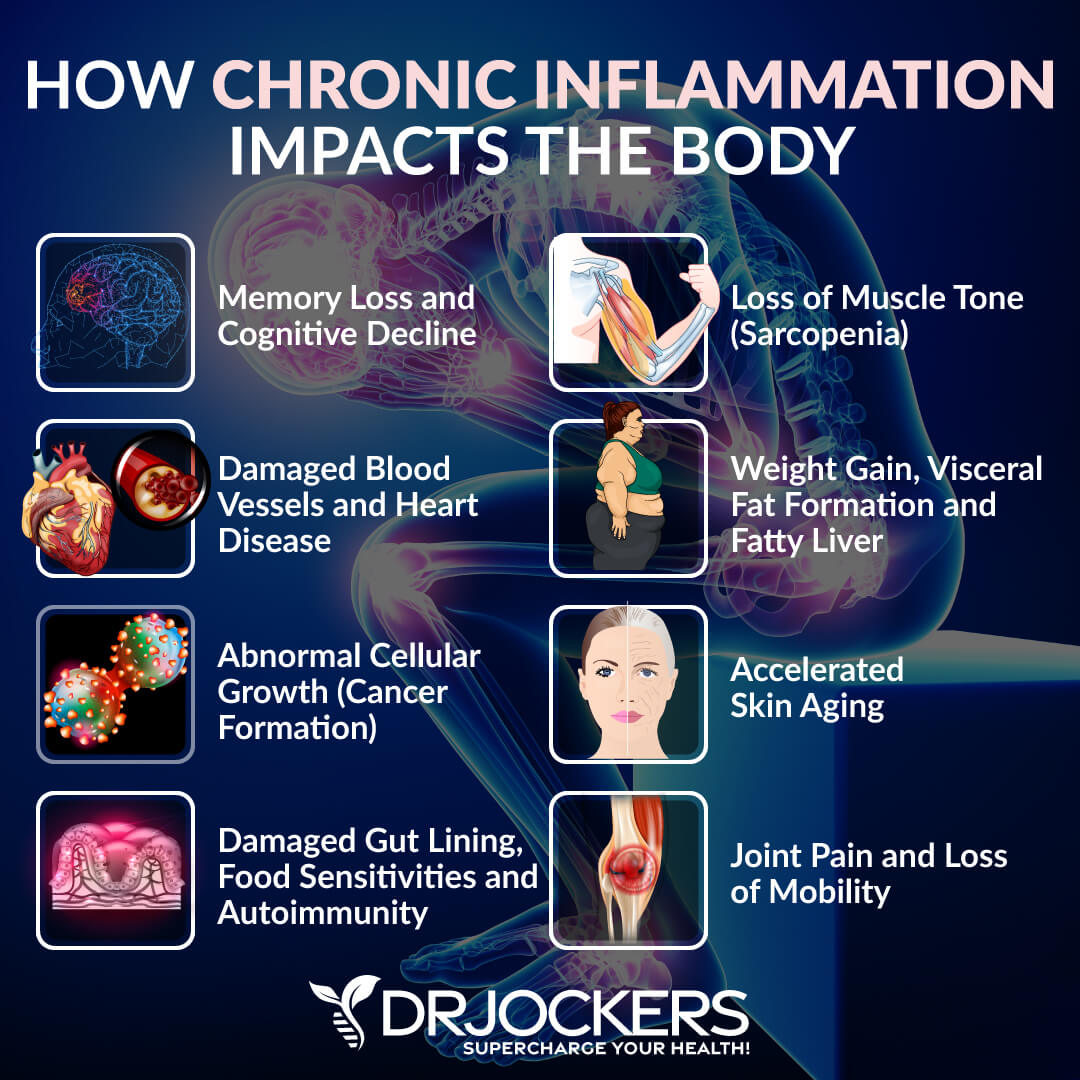
Inflammation & Autoimmunity
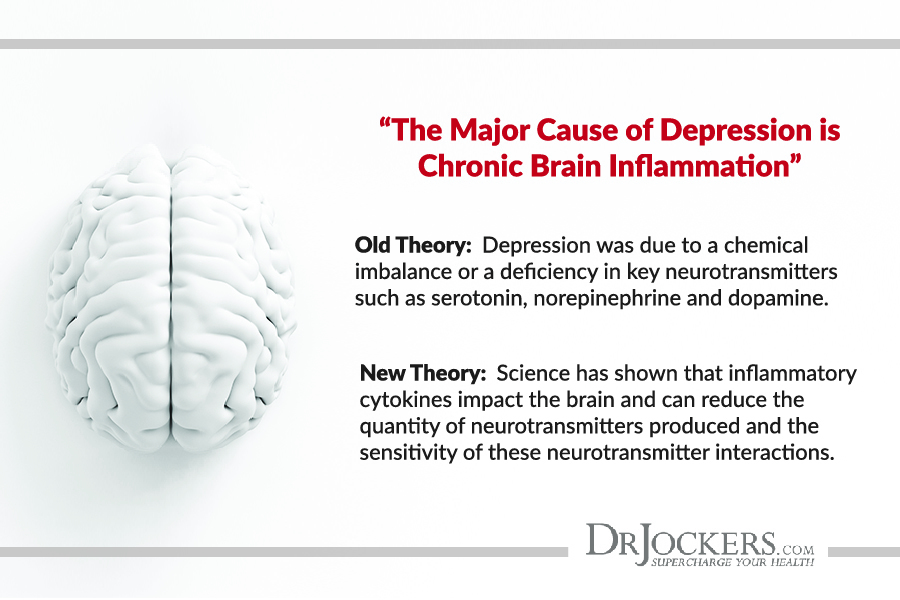
Chronic inflammation can increase the risk of various symptoms and health issues in anyone. It can also influence women’s health. Dealing with an autoimmune disease can also impact women’s health issues.
A 2020 study published in the Journal of Neuroinflammation has found that system inflammation during perimenopause can increase the risk of neurodegenerative issues later in life (21). A 2019 review published in Frontiers in Endocrinology (Lausanne) has found that the endocrine transitions between puberty and menopause, as well as potential pregnancies and breastfeeding, can increase the risk of chronic inflammation and autoimmunity in women’s health (22).
Hashimoto’s thyroiditis is an autoimmune form of hypothyroidism where your thyroid gland produces too much thyroid hormones. It is more common in women than men. According to a 2017 review published in Menopause Reviews, thyroid issues are increasingly common in postmenopausal and elderly women, and it can increase their risk of bone fractures, depression, cognitive issues, cardiovascular disease, and mortality (22). A 2007 study published in the Journal of Obstetrics and Gynecology has found that both hyper- and hypothyroidism can worsen menopausal symptoms (23).
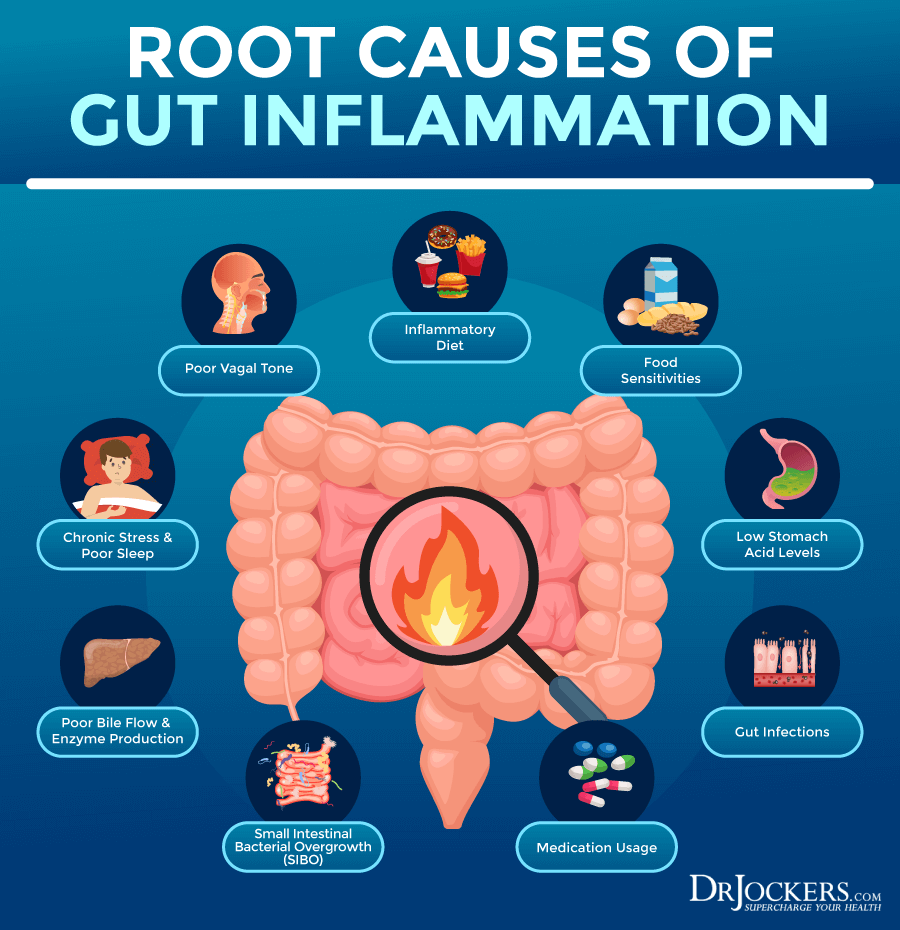
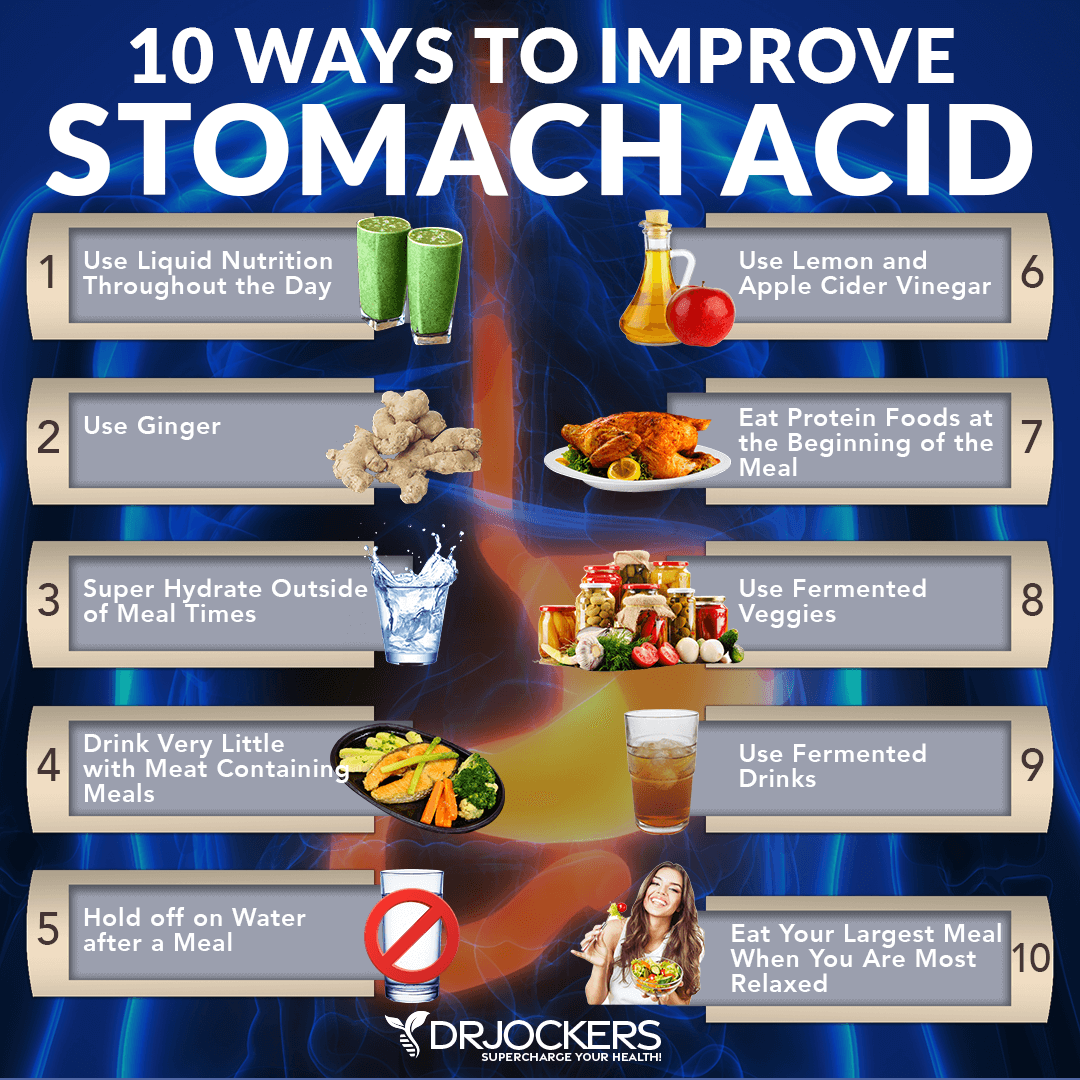
Gut Dysbiosis & Low Stomach Acid Levels
Gut dysbiosis and low stomach acid levels can seriously impact women’s health and increase symptoms. It can increase chronic inflammation, the risk of autoimmunity, pain, and chronic symptoms. The risk of gut health issues can increase during menopause, while these gut problems can increase menopausal symptoms as well.
A 2020 study published in JCI Insight has found that gut inflammation and gut permeability can increase from perimenopause to menopause (25). This may explain why many women develop more gut problems during menopause. A 2020 review published in Menopause has also found that due to the shifts in estrogen, the gut microbiome changes during menopause which can increase the risk of weight gain, metabolic rate, and insulin resistance (26).
A 2008 study published in the Journal of American Academy of Nurse Practitioners has found that over 40 percent of perimenopausal and menopausal women have gastroesophageal reflux yet about 80 percent of these women haven’t been diagnosed with gastroesophageal reflux disease (GERD) upper-GI disorder (27). GERD is usually the result of low levels of stomach acid. Since this is an issue so overlooked, yet so prevalent in women, stomach acid levels need more attention in women’s health.
Chronic Infections
Chronic infection can increase chronic inflammation in the body. They can also contribute to other health issues, chronic symptoms, and impact women’s health and menopausal transition.
A 2003 review published in the American Family Physician has found that chronic illness, including HIV infection, can affect sexual function (28). A 2020 study published in the Journal of Medicine and Life has found that frequent vaginal infections, such a Candida and Gardnerella, are a common culprit in low sexual function (29).
A 2021 study published in MedRXiv has found that the Epstein Barr Virus (EBV) may increase the risk of breast cancer (30). A 2018 study published in Viral Immunology has found that increased estradiol levels can cause the reactivation of the EBV virus (31).
A 2021 study published in PLoS One has found that intestinal parasitic infections can increase nutritional imbalance, iron deficiency, and maternal anemia in pregnancy, and low birth weight (32). A 2016 study published in the European Journal of Microbiology and Immunology has linked Toxoplasma gondii parasitic infection and toxoplasmosis to increased menopausal symptoms, such as digestive issues, migraines, breast pain, low back pain, and dizziness (33).
A 17-year study and retrospective analysis published in 2019 in BMC Public Health has found that Lyme disease is more common in females (34). The study has found that 60 percent of the over 2,300 Lyme disease cases looked at were women. Researchers found that the incidents peaked between ages 61 and 65 and 6 to 10, suggesting that older women and young girls are at higher risk of the disease.
A 2006 research published in Immunology has found that while men and women get bit by Lyme-carrying ticks, women are more likely to get reinfected. This may be due to different immunological responses (35). Women’s bodies are more likely to release spontaneous cytokines.
It seems that postmenopausal women show a Th2-directed and anti-inflammatory immune reactivity with increased IL-10-mediated suppression of the pro-inflammatory response, which may explain the risk and frequency of reinfection in women.
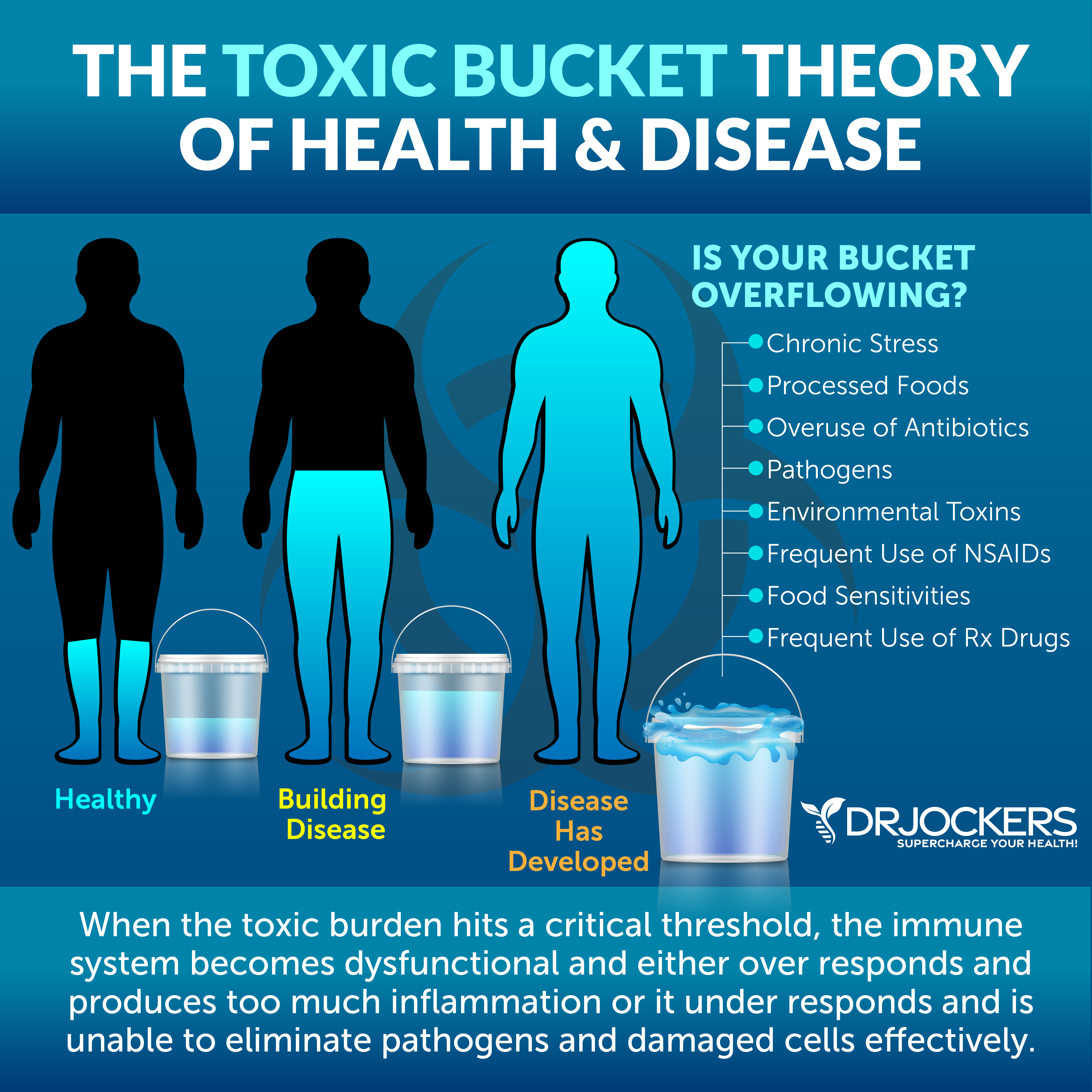
High Toxin Exposure
High toxin exposure is another issue that can cause major health problems in everyone but can be particularly harmful to women’s health. A 2019 study published in JBRA Assisted Reproduction has found that environmental toxins and endocrine-disrupting chemicals can negatively impact female reproductive health (36).
Glyphosate is an herbicide used for broad weeds and grasses. According to a 2018 study published in Environmental Health, glyphosate exposure can increase the risk of pregnancy issues and reduce gestational length (37).
Mold is a type of fungus that can hide in your bathroom, in your basement, under your carpet, behind old wallpaper, or just about any warm, moist, and damp environment. Mycotoxins from mold can pose a serious health risk including for women’s health.
According to a 2018 paper published in the Journal of Biological Regulators and Homeostatic Agents, mold exposure can increase mast cell activation and histamine intolerance (38). Histamine intolerance, among other symptoms, can increase the risk of menstrual issues, interstitial cystitis, fatigue, weight gain, and digestive issues that affect women.
Bisphenol A or BPA is an industrial chemical found in certain plastic products such as water bottles and cheap containers. It is a very harmful toxin and endocrine disruptor that can impact women’s health. A 2015 review published in the International Journal of Environmental Research and Public Health has found that BPA can increase the risk of female infertility (39).
Heavy metals are another issue that can cause hormonal imbalance and disrupt women’s health. A 2017 animal study published in the International Journal of Environmental Research and Public Health has found that exposure to methylmercury can cause sexual dysfunction (40).
A 2002 review published in Environmental Research has found that toxicity from cadmium, mercury, lead, nickel, and arsenic may be more harmful to women’s health than men’s health (41). It is more likely to cause allergies, skin issues, and bone health issues, and may affect pregnancies negatively as well.
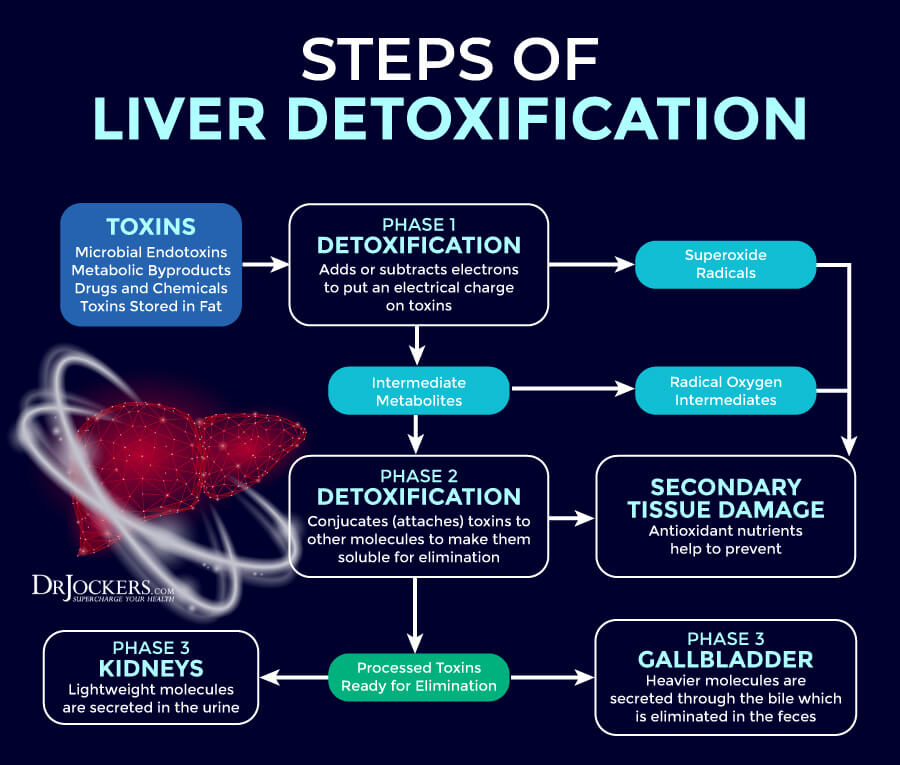
Sluggish Liver Function
The liver is a major detoxifying organ. Sluggish liver function can reduce your body’s ability to cleanse itself, which can lead to various health issues. According to a 2013 review published in Gastroenterology and Hepatology (NY), women are more likely to experience liver issues, such as autoimmune hepatitis, liver failure, benign liver lesions, and primary biliary cirrhosis (42).
Slugging liver function can increase the risk of excess estrogens, low thyroid, weight gain, and other women’s health issues. A 2014 study published in the Brazilian Journal of Medical and Biological Research has found a link between nonalcoholic fatty liver disease and weight gain (43). A 2013 study published in the Nigerian Postgraduate Medical Journal has found that there is a link between liver function and thyroid problems (44).
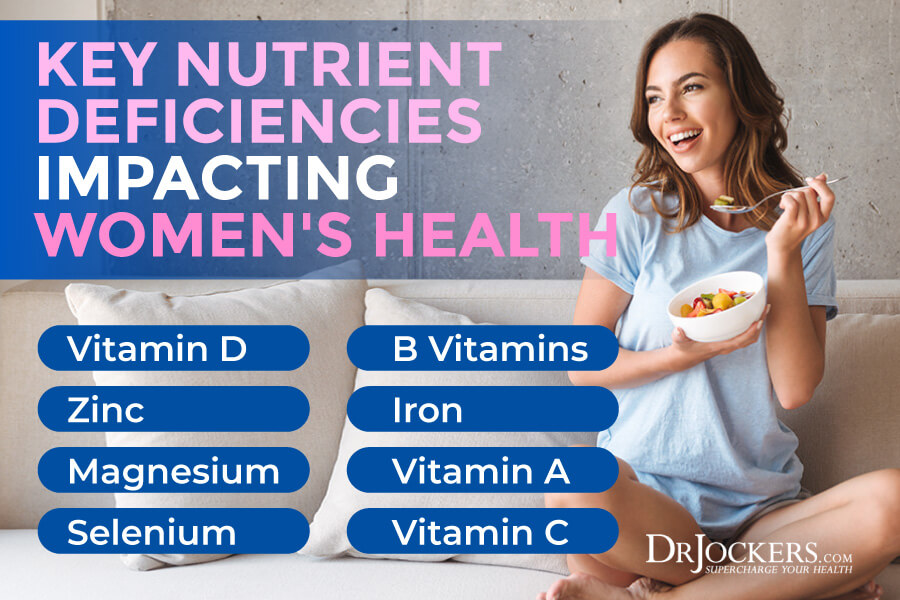
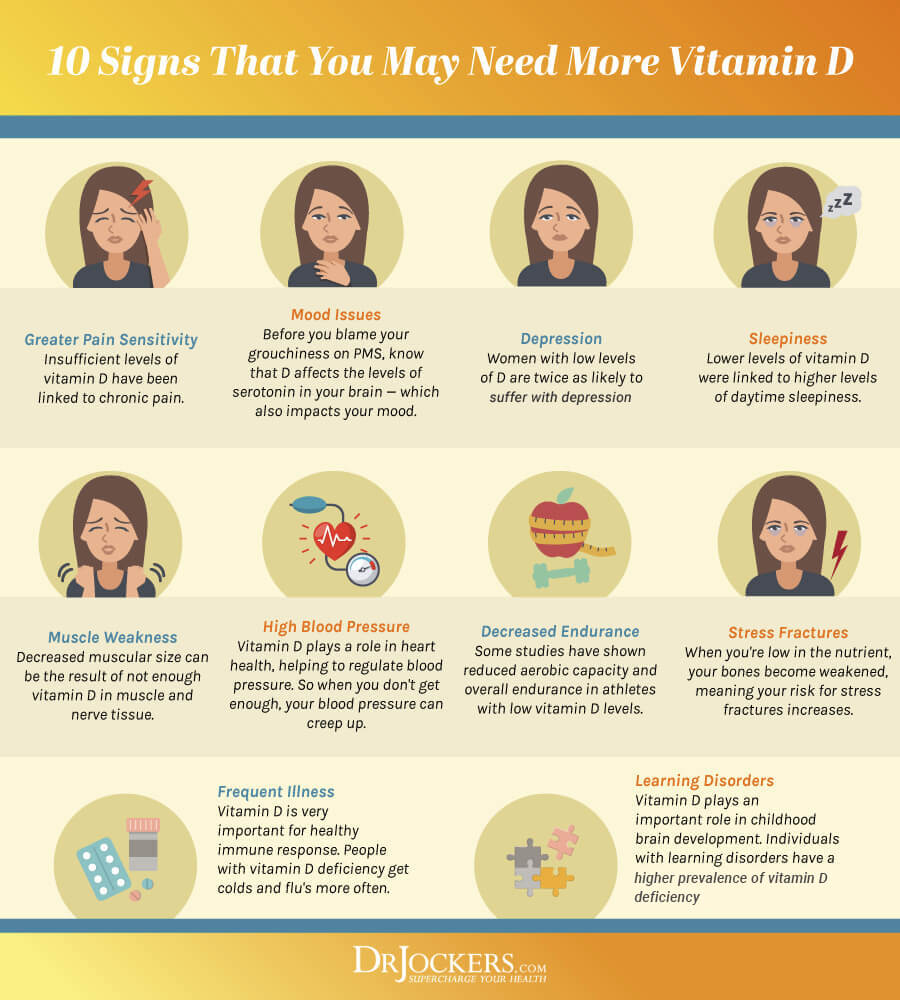
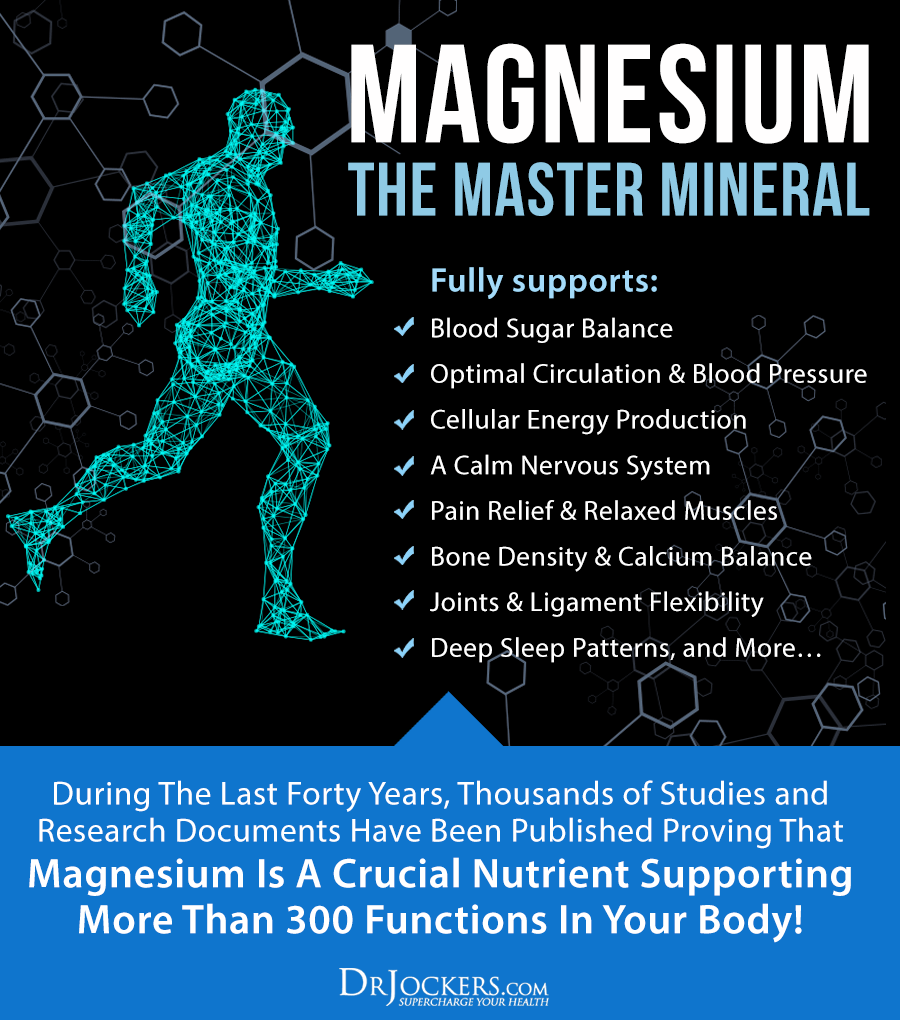
Nutrient Deficiencies
Nutrient deficiencies may occur due to a poor diet, poor absorption, underlying health issues, or certain medications. Nutritional deficiencies, however, can increase the risk or worsen the symptoms of women’s health issues, including perimenopause and menopause symptoms. Deficiencies in zinc, B vitamins, iron, vitamin D, and magnesium are some of the most common issues.
A 2016 review published in Menopause Review has found that poor nutrition, especially the lack of vitamins, including vitamin C and A, and B vitamins, and minerals, including zinc, magnesium, calcium, iron, copper, selenium, and silicon, can all influence hair thinning in menopause (13). A 2016 study published in the European Journal of Obstetrics, Gynecology, and Reproductive Biology has found that vitamin D deficiency can lead to depression, low libido, lower chance of orgasm, and lower sexual satisfaction in young women (45).
A 2011 study published in the Journal of American Dietary Association has found that nutrient deficiencies, including deficiencies in iron, vitamin B12, and folate, can increase the risk of anemia in postmenopausal women (46). A 2009 study published in the Journal of Nutrition has found that zinc deficiencies are common in young women and might be a concern for women’s health (47).
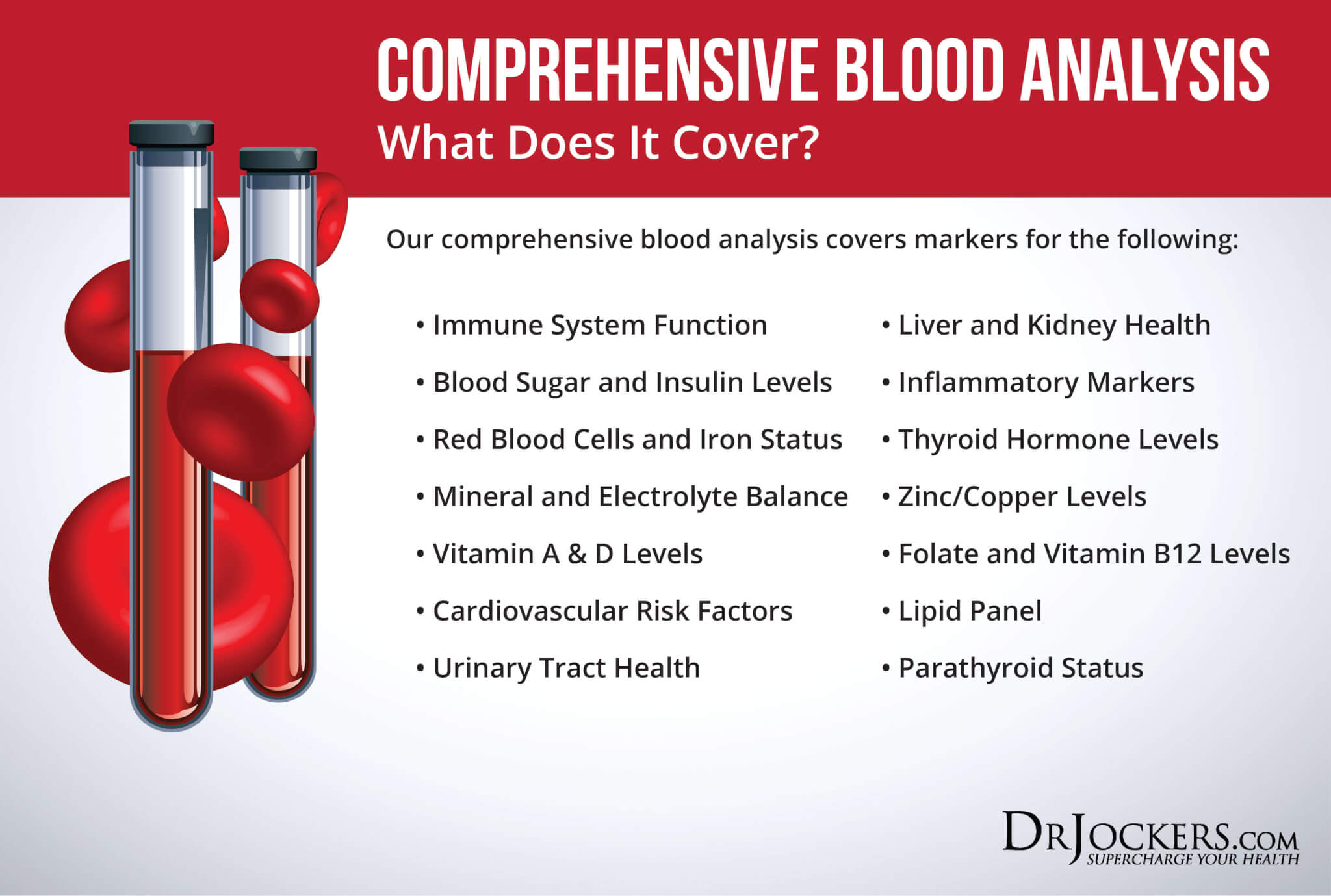
Key Functional Labs
There are a number of key functional labs I use and recommend to determine your risk factors and uncover the root causes of endometrial cancer. Here is what I recommend.
Inflammation: Hs-CRP, ESR, LDH & Serum Ferritin
There are a number of tests I recommend to check for underlying inflammation, including Hs-CRP, ESR, LDH, and serum ferritin testing.
The C-Reactive Protein or CRP test is a key test I recommend. It measures a protein (CRP) produced in your liver that indicates inflammation levels in your body. The clinical range is between 0 and 3 mg/L while the optimal range is 0 to 1 mg/L. When I see levels over 1 mg/L, I know the individual is having an inflammatory response that could be due to acute trauma or chronic conditions.
ESR refers to the rate at which your red blood cells in anticoagulated whole blood go down in a standardized tube over a period of one hour. Optimal ESR rates are between 0 and 10 mm/hr.
LDH is an enzyme found in all living cells. Elevated levels may indicate inflammation. Optimal levels are between 140-180. Levels over 180 indicate inflammation and levels under 140 indicate reactive hypoglycemia.
Serum ferritin measures the level of ferritin in your body to detect iron deficiency anemia and other health issues. Elevated serum ferritin levels may indicate inflammation, liver disease, autoimmune disease, or even cancer. The clinical range is 30 to 400, and the optimal range is 25 to 150 for females and 50 to 150 for males. You can get these labs done on our Comprehensive Blood Analysis here.
Insulin Resistance: Fasting Insulin, HbA1C, Thyroid Panels and Lipid Profile
I recommend a number of tests to check for insulin resistance, including fasting insulin levels, HbA1C, full thyroid panels and a lipid profile.
Blood sugar imbalances may increase your risk of inflammation. In addition to testing your HbA1C levels, I recommend checking your fasting insulin levels. Testing your fasting insulin can recognize elevated blood sugar levels and can detect inflammation, insulin resistance, blood sugar issues, and diabetes. The clinical range for fasting insulin is 2.6 – 24.9 uIU/ml and the optimal range is 1.0 – 6.0 uIU/ml.
Blood sugar imbalances are one of the main causes of inflammation, so I recommend checking your hemoglobin A1C (HbA1C) levels. Your HbA1C levels measure your average blood sugar over the past 2 to 3 months. Hemoglobin A1C (HbA1c) gives the average amount of glucose in your blood or blood sugar over the past 3 months making it one of the top tests for inflammation and diabetes. The clinical range is between 4.8 and 5.6 while the optimal range is 4.5 – 5.2.
Having a balanced ratio of LDL to HDL and triglycerides to HDL is essential for your health. We are looking for low HDL or high triglycerides as a sign of insulin resistance. Ideally, we are looking for an LDL: HDL ratio: 3:1 or less, 2:1 being optimal.
Ideally, we are looking for an LDL: HDL ratio: 3:1 or less, 2:1 being optimal. We are also looking at a triglyceride: HDL ratio of 2:1 or less, 1:1 being optimal. Higher rates may indicate insulin resistance and inflammation. Optimal levels:
- HDL cholesterol: The idea range is 55 to 90. Levels above 100 can indicate chronic inflammation or active infection in the body.
- Triglycerides: The ideal range is 40 to 80.
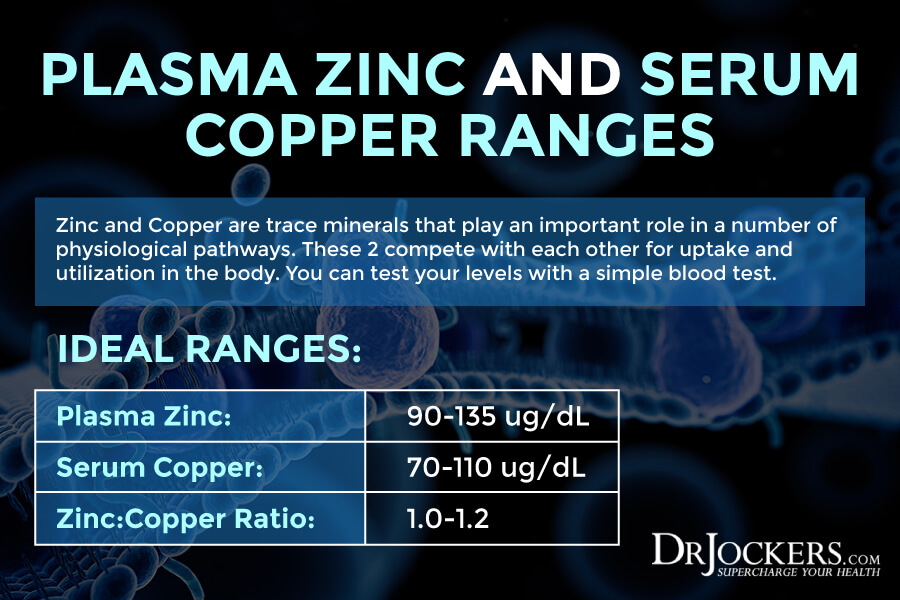
Vitamin D, Plasma Zinc: Serum Copper Ratio
Since vitamin D and zinc deficiencies and high copper levels may increase the risk of endometrial cancer, I recommend checking your vitamin D and zinc: serum copper ratio.
Vitamin D3 is an important vitamin that most of our population is deficient in. Poor levels may indicate inflammation. Normal levels of vitamin D are between 50-100 ng/mL
Checking your plasma zinc levels is the best way to determine zinc levels in your body. Ideal plasma zinc levels are between 90–135 ug/dL and for serum copper it should be 70–110 ug/dL. Zinc and copper compete against each other as antagonists to regulate physiological pathways. A proper balance between the two is essential for maintaining good health. I recommend checking your plasma zinc and serum copper levels and their balance. The proper zinc:copper ratio should be between 1–1.2.
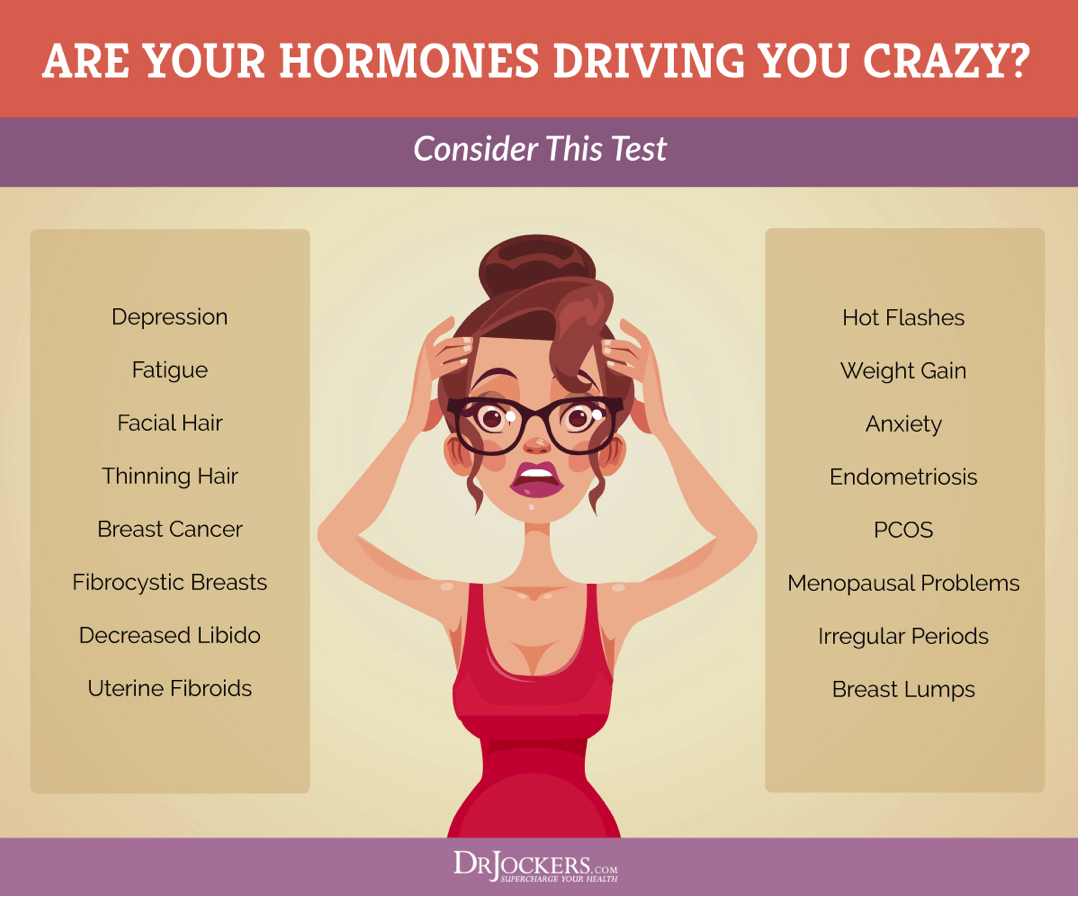
DUTCH Test to look at Estrogen Metabolites
I also recommend the DUTCH Test™ — Dried Urine Test Comprehensive Hormones to check for estrogen metabolites. This test offers a complete hormonal panel. Beyond estrogen metabolites and estrogen levels, it looks at progesterone, testosterone, cortisol, DHEA, and melatonin levels.
The DUTCH Complete Hormone Panel is well-recognized for its ease-of-collection, coupled with comprehensive reporting that is not available from other laboratories. This test will give you the information you need to understand what is happening with your adrenals, melatonin levels and sex hormones including estrogen metabolites.
GI MAP
I also recommend a GI Map Stool Test to further understand your digestive health and help appropriate lifestyle changes for improved digestive health. This is the best and most comprehensive gut test I have found. It helps to determine whether you have underlying gut dysbiosis. It helps to identify bacterial pathogens, parasitic pathogens, viral pathogens, normal flora, dysbiotic flora.
I specifically recommend looking for Beta Glucuronidase. This test also looks at potential autoimmune triggers and all intestinal health markers. This test takes the guesswork out of your treatment and allows us to identify the gut-related root causes of your health issues.
Natural Support Strategies
There is a long list of natural support strategies that may help to improve women’s health. Here is what I recommend.
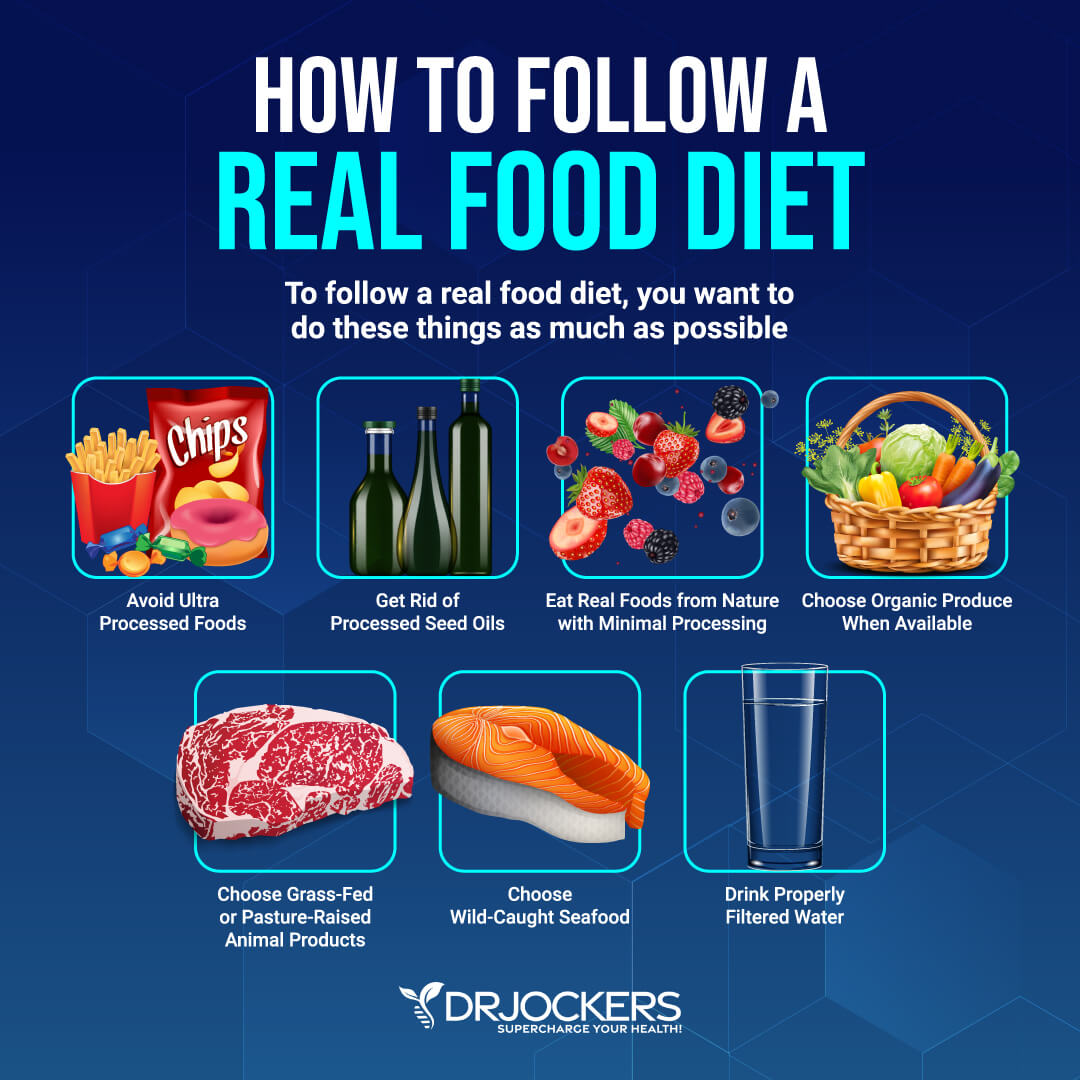
Anti-Inflammatory Nutrition Plan
A 2015 study has found that following an inflammatory diet can increase the risk of chronic health issues in women’s health, including cardiovascular disease, cancer, and mortality (48). Improving your diet and following an anti-inflammatory, nutrient-dense nutrition plan can reduce your risks and improve your health.
I recommend that you remove inflammatory foods, including refined sugar, refined oils, artificial ingredients, additives, junk food, and highly processed foods. Choose organic whenever possible. Eat an anti-inflammatory diet rich in greens, vegetables, sprouts, herbs, spices, healthy fats, low-glycemic index fruits, grass-fed beef and butter, pasture-raised poultry and eggs, wild-caught fish and seafood, and wild game.
Practice Intermittent Fasting
Intermittent fasting is a way of eating that cycles between a period when you are fasting (not eating) and a period of feasting (a window for your meals and eating) within one day. Intermittent fasting offers many benefits, including better insulin sensitivity, lower inflammation, and improved cellular repair and function. It may also help with women’s health. For example, a 2016 review published in the Journal of Midlife Health has found that therapeutic fasting may benefit women’s health, including PCOS (49).
Women, especially menstruating females, have to be careful so intermittent fasting doesn’t affect their menstrual cycle and hormonal health. For women, I recommend Crescendo Fasting. When you are doing Crescendo Fasting, you are not fasting every day. You are only fasting on 2 or 3 non-consecutive days per week. I recommend starting out with 2 days per week. You can pick any non-consecutive days, for example, Tuesday and Friday or Monday and Thursday.
On fasting days, apply the 16:8 rule. Fast for 16 hours keeping an 8-hour eating window. For example, you may be fasting from 6 pm after dinner until 10 am. Drink plenty of water throughout the day. Herbal teas without milk or sweetener are also a great option.
Avoid heavy exercise on fasting days, focus on yoga or light cardio instead. You can do strength training and more intense workouts on non-fasting days. After two weeks, you can add one more day to your fasting routine, but still practice it on non-consecutive days, for example, on Tuesday, Thursday, and Saturday. If you are doing well on 3 fasting days a week, you may add one more day of fasting at times, but don’t go over 4 fasting days per week.
You may learn about Crescendo Fasting here. I also recommend checking out my article on feast/famine cycling for optimizing the menstrual cycle.

Reduce Stress & Prioritize Good Sleep
Chronic stress and poor sleep can negatively impact women’s health (10, 17, 18, 19, 20). Reducing your stress levels and prioritizing good sleep is critical. Avoid stressful situations and people that bring you down and surround yourself with a supportive and uplifting community and tasks that feed your soul.
Stop scrolling social media and checking the news constantly, but select a designated time for it instead. Practice mindfulness, meditation, breathwork, visualization, journaling, positive affirmations, positive self-talk, and gratitude. Have some designated time for yourself and for self-care.
Develop a relaxing evening routine that calms and relaxes you. Avoid electronics, sugar, heavy food, and alcohol in the evening. Try relaxing activities, including taking a bath, reading fiction, poetry, or scripture, crossword puzzles, journaling, drawing, coloring, and meditation. Create a safe and relaxing sanctuary in your bedroom with a supportive mattress, comfortable bedding and pillows, relaxing essential oils, dim lights, and blackout curtains.

Regular Movement & Exercise
Regular movement and exercise are non-negotiable for women’s health. A 2018 study published in the Journal of Education and Health Promotion has found that physical fitness can improve sexual functioning and self-concept (50). A 2019 study published in the European Society of Cardiology has found that exercise can improve women’s health and reduce various health risks, including cardiovascular health issues, cancer, and mortality (51).
I recommend moving your body throughout the day. Start your day with stretching, yoga, grounding, or a short walk. Get up and stretch and shake your body out regularly. Try a standing desk that allows better posture and more movement. Take a short stroll or two throughout the day. Take the stairs. Park your car away from the entrance of the grocery store for an extra walk. Choose to walk or bike instead of driving closer distances when possible.
Exercise regularly, at least 20 to 30 minutes five days a week. Try a mix of cardiovascular, strength and resistance training, and low-impact workouts. Cardio, such as biking, jogging, or hiking, is great for your heart health. However, strength and resistance training, such as lifting weight, kettlebells, and bodyweight workouts, is critical for women’s health, especially as you get older and get closer or enter menopause. Strength and resistance training is important to preserve muscle tone, bone health, and strength. Lower impact workouts, such as yoga, pilates, and Barre, can help flexibility and muscle strength without a serious impact.

Improve Detoxification Pathways
Since toxin exposure and chronic infections can seriously impact women’s health, improving your detoxification pathways is crucial for improving your well-being (28, 29, 30, 31, 32, 33, 34, 35, 37, 38, 39, 40, 41). Drink lots of water to support detoxification through sweating and urine.
Try infrared saunas to promote detoxification through sweating. Practice rebounding and dry-skin brushing to support your lymphatic pathways. Support your two major detoxifying organs, your kidneys and liver, with kidney and liver support supplements, such as Kidney and Liver Support.
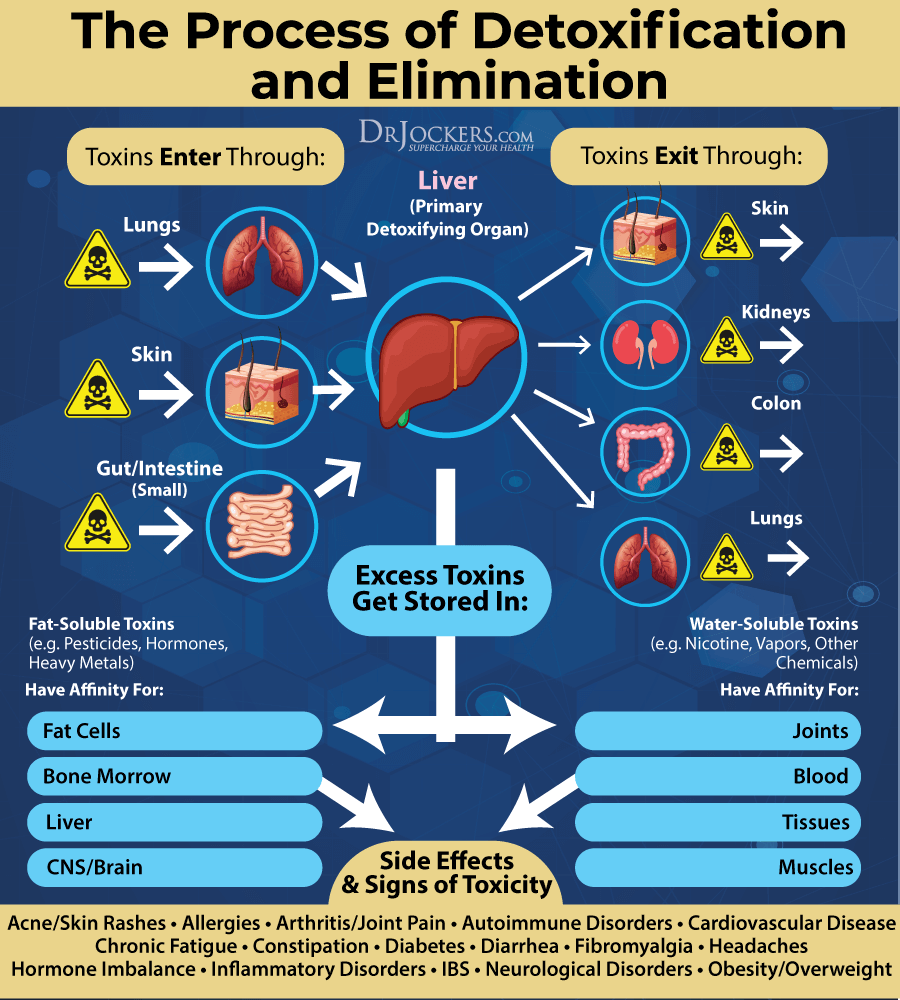
Reduce Parasites, Toxins, and Viral Load
Chronic infections and toxic load can increase the risk of various women’s health issues (28, 29, 30, 31, 32, 33, 34, 35,, 37, 38, 39, 40, 41). Reduce your toxin load by avoiding smoking and second-hand smoke, choosing organic food and organic, natural products, and reducing any other exposure to chemicals or toxins.
Use binders such as fulvic acid, betonite clay or activated charcoal to remove toxins from your intestinal tract. Follow an antioxidant-rich, anti-inflammatory nutrition plan and take high-quality probiotics and to improve your body’s ability to fight toxins and to support elimination.
Get tests for parasites, chronic viral infections, chronic infections, and toxins. We offer complex functional health tests, including Environmental Toxicity Testing, Glyphosate Testing, Mycotoxin Testing, Comprehensive Viral Panel Testing, and a GI Stool Map Analysis. Once you understand what type of toxins and infections, you are dealing with, we can help you with a personalized nutrition and supplement regimen to improve your health.

Optimize Stomach Acid Levels
Low stomach acid and acid reflux are common in perimenopausal and menopausal women (27). Follow an anti-inflammatory diet. You may benefit from liquid nutrition until your stomach acid levels and gut health improves. Try to make sure that at least half of your meals are in a liquid form, such as a protein shake or green smoothie.
Protein shakes are pre-metabolized and very easy to digest and do not depend upon HCL production. If you have low HCL, it may be helpful to drink one to two protein shakes daily to support amino acid absorption, reduce extra stress on your digestion, and support healthy stomach acid levels.
Eat your largest meals when you are most relaxed. I recommend starting your meal with protein instead of vegetables. This is because you will have your most concentrated level of HCL at the bottom of your stomach and if you need that acid to break down the protein but not the vegetables. Have the vegetables after consuming your protein sources.
Eat slowly and chew your food well. Hydrate well throughout the day between meals to help activate bowel motility and push contents through the digestive system, which will reduce microbial fermentation and toxicity in the body. However, avoid drinking water or liquids between 30 minutes before and after your meal, except if you need to take a supplement with 2 ounces of water and don’t drink water. This allows for proper stomach acid activity, sterilization, and protein metabolism.
Add fermented foods, such as sauerkraut, kimchi, pickles, pickled ginger, and other fermented vegetables that all contain organic acids, enzymes, and probiotics which help to improve digestive juice secretions.
I also recommend fermented drinks, such as apple cider vinegar, coconut kefir, and kombucha with anti-microbial benefits to help to reduce the bacterial load, especially the bacteria in the stomach such as H Pylori. Add ginger to your meals and try ginger tea to improve digestive juices and reduce gut problems. Take a daily probiotic supplement to support your microbiome health, digestive enzymes to support digestion, and a supplement with betaine hydrochloric acid to support stomach acid production and bile flow.
Support the Gut Microbiome
Gut microbiome imbalance is a common issue for women’s health that can cause chronic inflammation, autoimmunity, and various chronic health issues (25, 26). Support your gut microbiome with a gut-friendly, anti-inflammatory diet I’ve explained earlier.
You may benefit from increasing your prebiotic intake to feed healthy gut bacteria. However, prebiotics is not right for everyone. If you are on a low-FODMAP diet or a Carnivore Diet or having digestive issues with too much prebiotic fiber, back off. Eat plenty of fermented foods, such as kimchi, sauerkraut, fermented vegetables, fermented herbs, coconut kefir, and kombucha.
Take a daily probiotic supplement. Improve your postbiotics by following the tips outlined in this article.

Optimize Vitamin D Levels
Vitamin D deficiencies can seriously impact women’s health, such as increasing inflammation, depression, sexual health, and more (13, 45). Optimizing your vitamin D levels is clearly important.
To optimize your vitamin D levels, I recommend spending time out in the sun and eating vitamin D-rich fatty fish, egg yolks, and beef liver. However, sunshine and food are not enough. I recommend daily supplementation with vitamin D3.
Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and inflammation control. I recommend taking a vitamin D3 supplement with at least 3,000-5,000 IU’s of vitamin D3 and at least 90 mcg of vitamin K2. I highly recommend Vitamin D3/K2 Power. This supplement supports your immune, skin, cardiovascular, and bone health.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for major health conditions is going to be between 70-100 ng/ml.
Optimize Zinc, Magnesium, and B Vitamin Levels
Nutrient deficiencies, such as zinc, magnesium, and B vitamin levels, can impact women’s health (13, 46, 47). Thus, I recommend optimizing your zinc, magnesium, and B vitamin levels.
I recommend that you consume plenty of zinc-rich foods, including meat, poultry, and seafood. Additionally, I recommend daily zinc supplementation, such as Zinc Charge.
We test plasma zinc and serum copper levels, and the ideal ratio is roughly 1 to 1.2, meaning you should have equal or slightly higher levels of plasma zinc than you have serum copper. Fortunately, the foods that are high in zinc, such as meat, seafood, nuts, and pumpkin seeds, are also very high in copper, so you get both of these together in your diet.
To improve magnesium, I recommend Brain Calm Magnesium for energy, brain health, pain relief, bone health, muscle health, joint function, and better sleep. Mag Sleep is great if you want to improve sleep and optimize magnesium. Magnesium Oil Ultra with MSM Tropical Spray is perfect for muscle pain and relaxation.
To improve your B vitamin levels, I recommend B Strong for B vitamin complex and B12 Power. You can benefit from foods rich in B vitamins, such as meat, fish, shellfish, liver, kidney, eggs, and dark leafy greens.
Consider Thyroid Support Nutrients
Thyroid problems are common in women, and they can also impact the balance of other hormones and overall women’s health (6).To support your thyroid, I recommend Thyroid Strong. This supplement is a comprehensive freeze-dried, BSE-free, bovine, multiglandular, mineral, and herbal formula to support healthy thyroid function. It provides essential nutrients, herbal and glandular support for the production of thyroid hormones.
It supports thyroid hormone production with L-tyrosine and iodine and the conversion of T4 to T3 by selenium. Bladderwrack (Fucus vesiculosus), dulse, kelp, and Irish moss are also included in the formula as they are natural sources of iodine for support of endogenous thyroid hormone production.
I recommend 1 capsule first thing in the morning, away from food or as directed by your health care practitioner or for advanced dose, 2 capsules first thing in the morning, away from food or as directed by your health care practitioner.
Consider Female Hormone Balancing Herbs
According to a 2016 review published in Pharmaceutical Reviews, there are various herbs and botanicals that may help to support female hormonal balance, pre-menstrual and menstrual symptoms, urinary infections, menopausal symptoms, and other women’s health concerns (52).
Some of these herbs include Black Cohosh, green tea, broccoli seed extract, wild yam, Don Quai, fenugreek, cranberry, ginger, valerian, kudzu, and rhubarb. To benefit from hormone-balancing herbs, as well other nutrients, I recommend Fem Protect.
This supplement supports classic herbal hormonal balancing in the form of vitex, polygonum, and black cohosh, along with DIM and chrysin for protection and support of beneficial estrogen aromatase activity. Calcium-D-glucarate promotes the proper elimination of excess estrogens.
Resveratrol and EGCG from green tea are included for maximum antioxidant protection. Vitamins B6, B12, and folate promote proper cell differentiation.
Magnesium and calcium are also included to help support bone and hormone health. I recommend taking two capsules two times a day with or without meals or for advanced dose, 4 capsules twice a day with or without meals or as directed by your health care practitioner.
Final Thoughts
Women go through major hormonal transitions between puberty and menopause. As a result of these hormonal factors and other female-specific issues, women are at a higher risk of many health concerns, and, of course, they may also experience various female-specific health issues. Women’s health is important to understand and protect. I recommend that you follow my top natural support strategies to support women’s health and well-being.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and thrive in life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!