 Type I Diabetes: Symptoms, Risk Factors, and Support Strategies
Type I Diabetes: Symptoms, Risk Factors, and Support Strategies
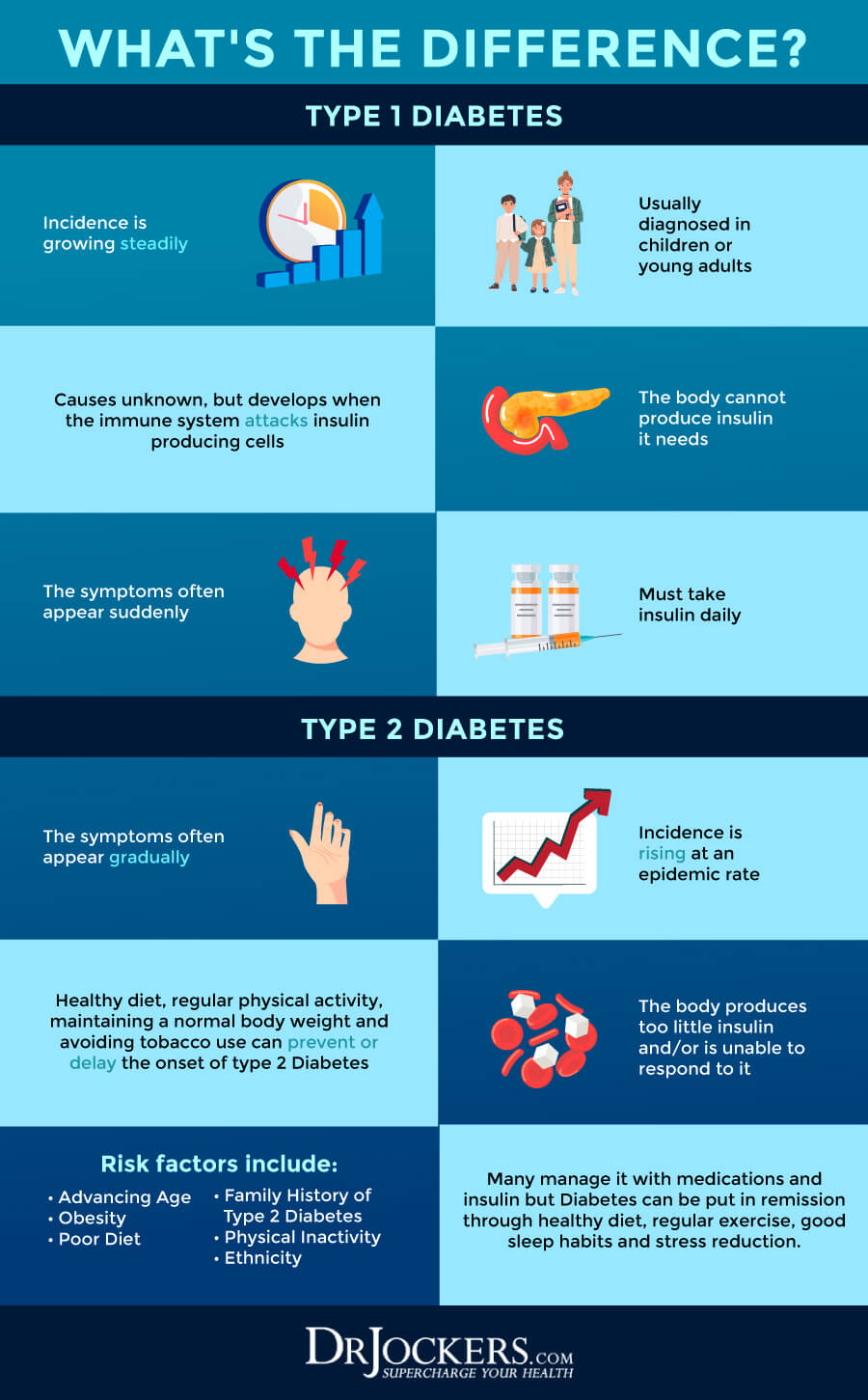
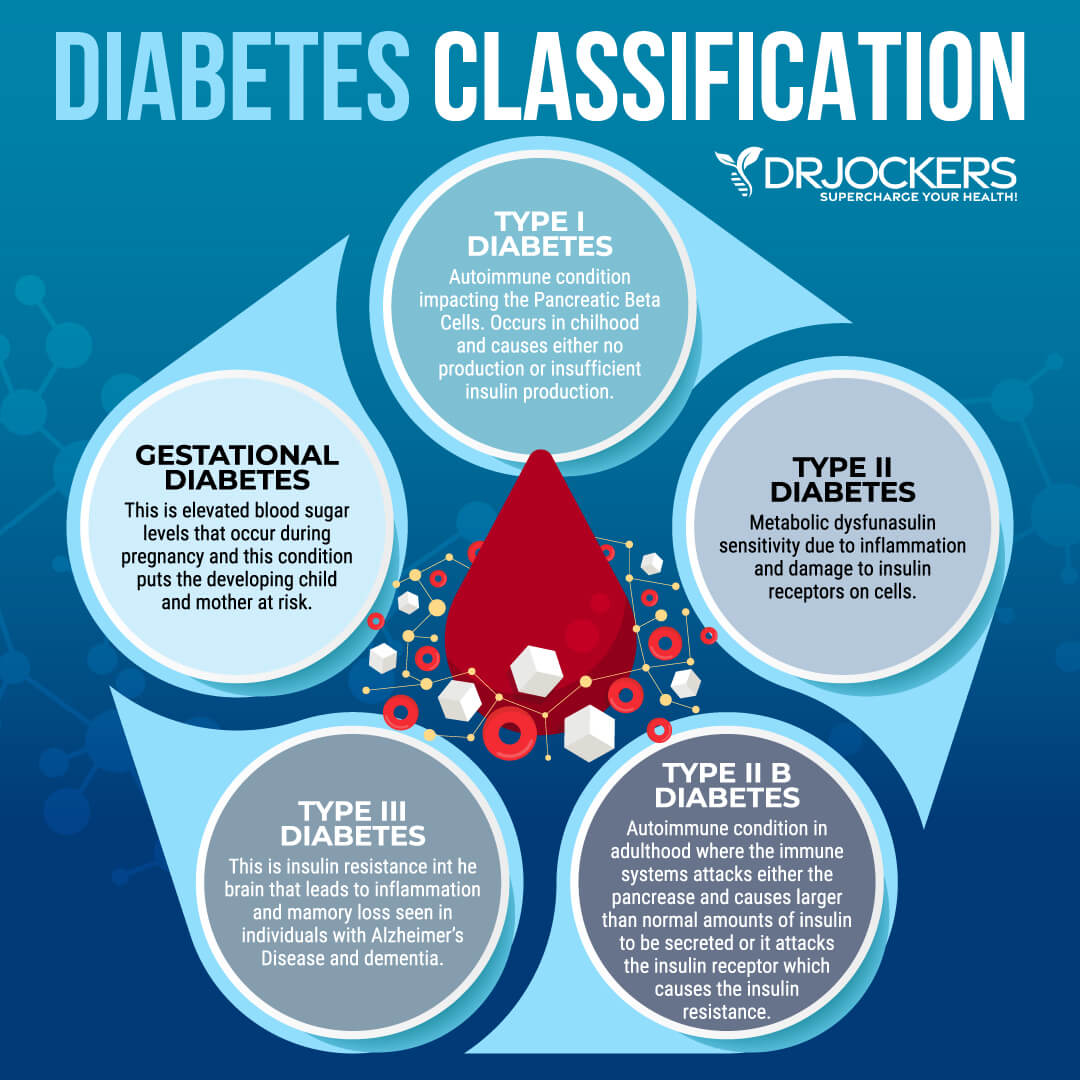
Type 1 diabetes is an autoimmune disease that is less common than type 2 diabetes and only affects between 5 and 10 percent of all patients with diabetes. If you have type 1 diabetes, it means that your body is unable to make insulin to handle the glucose in your body.
This means that your body will need insulin through medication. However, needing insulin doesn’t mean that you cannot improve your symptoms and health naturally. There are some natural dietary and lifestyle strategies that can support your health if you have type 1 diabetes.
In this article, you will learn what type 1 diabetes is. You will understand its symptoms. I will explain the pathogenesis of type 1 diabetes. You will learn about its risk factors. I will go over the diagnosis and conventional treatment strategies for type 1 diabetes.
You will learn about the root cause factors that may increase the risk of type 1 diabetes. Finally, I will share my top natural support strategies for those with type 1 diabetes to improve their health and well-being.
What is Type I Diabetes
Type 1 diabetes is a chronic health condition. In a healthy body, your pancreas makes the hormone insulin to take care of blood glucose. If you have type 1 diabetes, it means that your pancreas cannot make insulin.
According to the Centers for Disease Control and Prevention (CDC), type 1 diabetes is much less common than type 2 diabetes (1). It only affects about 5 to 10 percent of all diabetes patients (1). Though it tends to develop during childhood, during the teenage years, or in young adults, it can develop in anyone at any age (1).
Type I Diabetes Symptoms
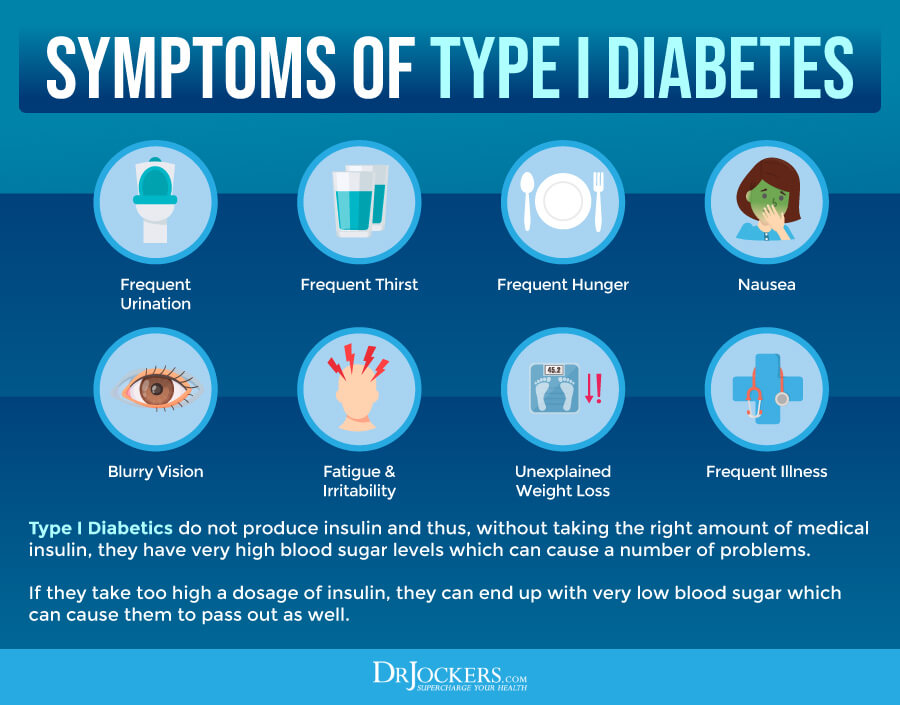
Symptoms of type 1 diabetes may include (2):
- Having to pee often and often during the night
- Feeling very thirsty frequently
- Feeling very hungry
- Losing weight without trying
- Blurry vision
- Numbness or tingling in the hands or feet
- Fatigue
- Dry skin
- Sores that heal slowly
- More infections than usual
- Nausea, vomiting, or stomach pains
Pathogenesis of Type I Diabetes
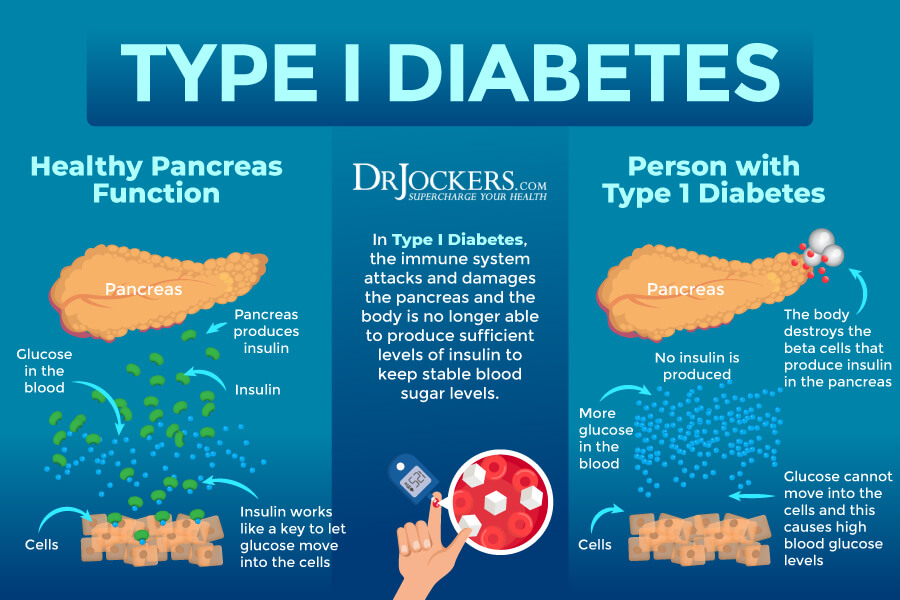
Insulin is an essential hormone in your body that allows your cells to use glucose from food for energy. Insulin helps glucose to get from your blood into your body’s cells. If your cells received enough blood glucose for energy, your liver and muscle tissues will store what’s remaining in the form of glycogen. When you need extra energy, your body can break glycogen down into blood glucose and release it into your system.
In a healthy body, your pancreas creates enough insulin to handle all the blood glucose in your body. However, if you have type 1 diabetes, it means that your body cannot make insulin, and therefore, it’s unable to process glucose. This means that the glucose that you get from food cannot get into your cells.
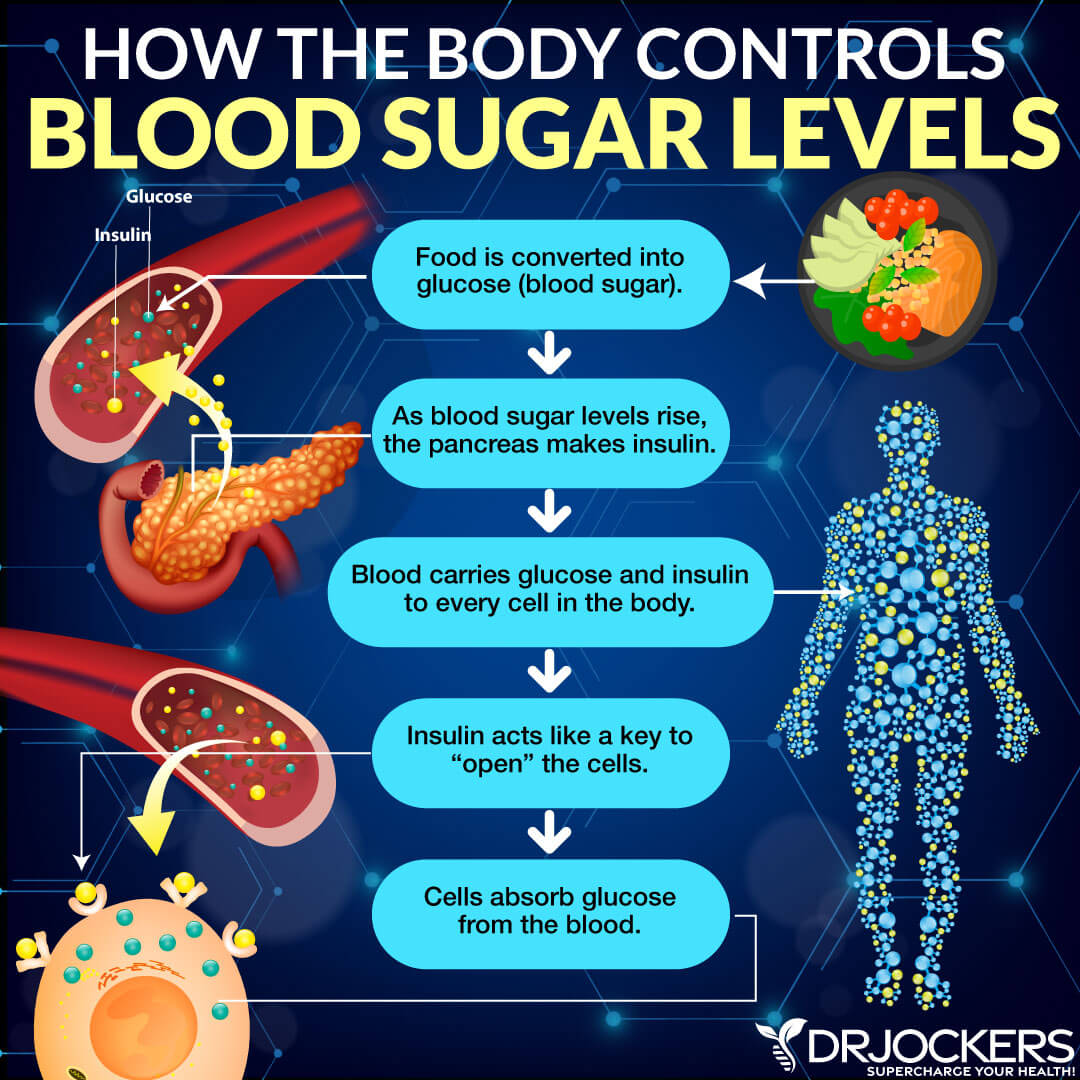
This leaves the glucose circulating in your blood without arriving at its destination and getting converted into energy. Having high blood glucose levels due to untreated type 1 diabetes can result in a number of short-term and long-term health issues (1).
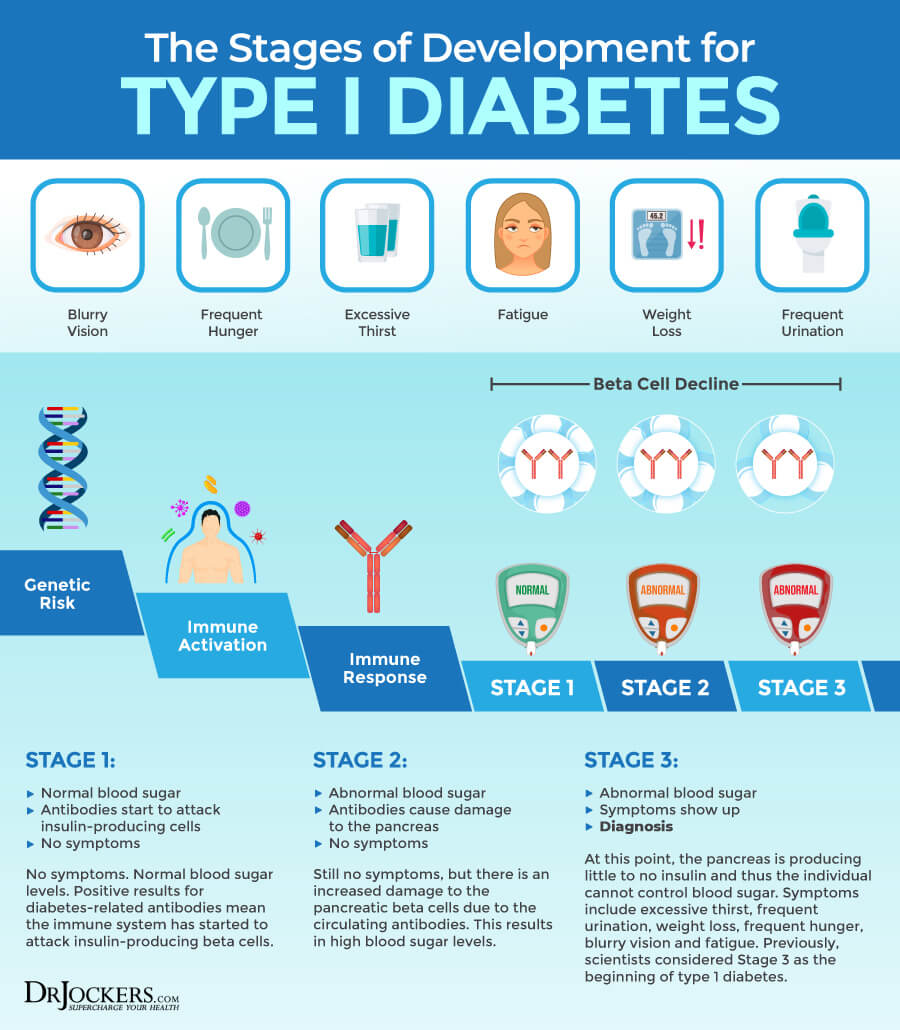
Type 1 diabetes is very different from type 2 diabetes. Type 2 diabetes, which is a much more common issue, develops because of insulin resistance and reduces insulin secretion. According to our current knowledge, type 1 diabetes is caused by autoimmunity. According to a 2018 review published in Endocrine Connections, it develops because of the autoimmune destruction of endocrine pancreatic beta cells (3).
Researchers found that genetic, immunologic, and environmental factors may also play a role in the destruction of these beta cells resulting in insulin deficiency. This autoimmune destruction may take several months to several years to develop before symptoms occur, and the patient may test positive for antibodies.
A 2006 scientific paper discussed that while type 1 diabetes has no cure, the development of this autoimmune destruction may be preventable (4). The author discusses that antibody assays may make it possible to identify the risk of developing the disease. The paper suggests that understanding the pathogenesis and looking at the genetic and environmental risk factors of type 1 diabetes are critical for future research to identify appropriate preventative measures. Later in this article, I will go over some natural support strategies that may improve your health.
Risk Factors for Type I Diabetes
The risk factors and causes of type 1 diabetes are not yet completely understood. Risk factors for type 1 diabetes may include (4):
- Age: Children, teenagers, and young adults are more likely to develop type 1 diabetes.
- Family history: If you have a parent or sibling with type 1 diabetes, you are more likely to develop the condition yourself.
- Race or ethnicity: In the United States, white individuals are more likely to develop type 1 diabetes than Hispanic, Latino, or African American individuals.
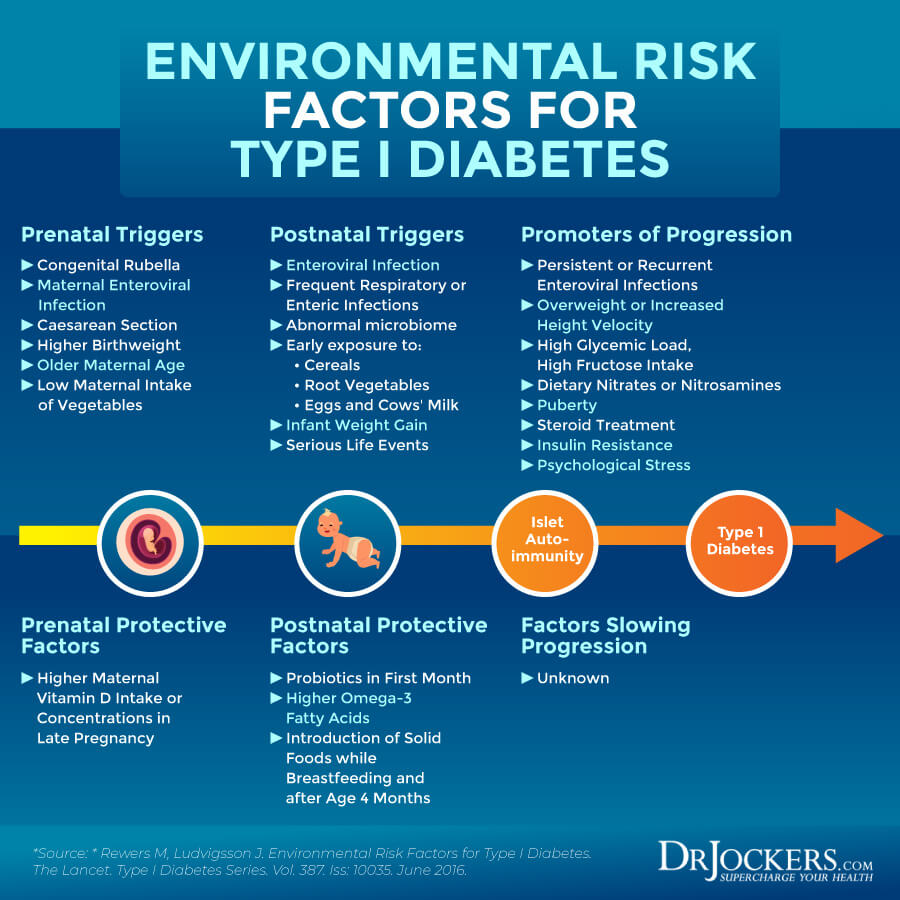
- Environmental factors: While it’s not clear, certain viral infections may increase the risk of type 1 diabetes. Type 1 diabetes is also more common in colder climates, which suggests that climate may play some role.
Diagnosing Type I Diabetes
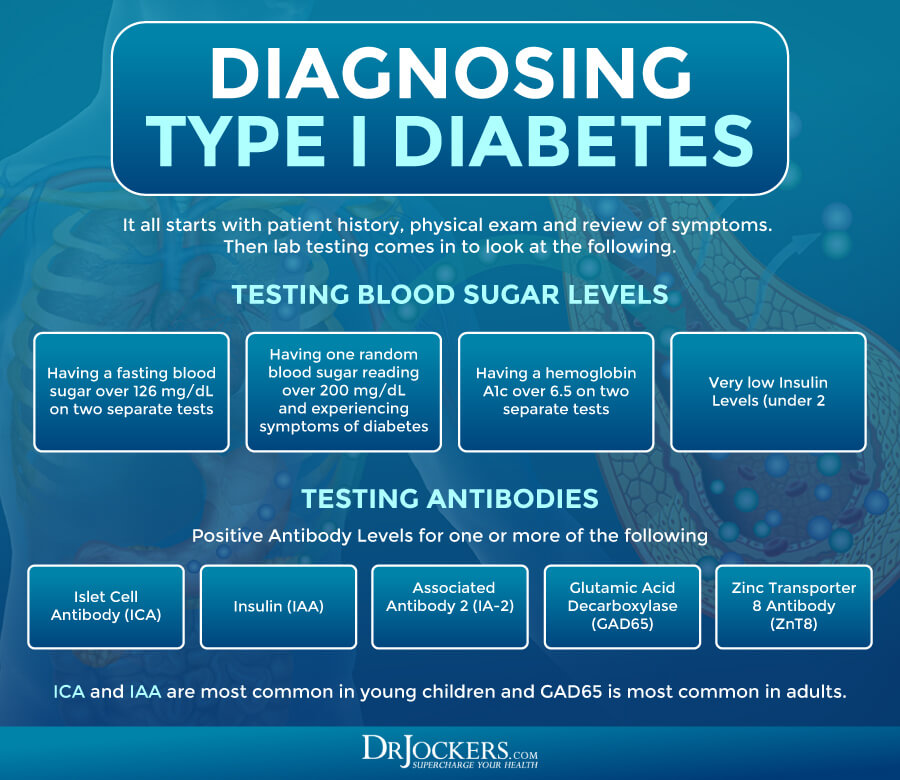
After going over your symptoms, medical history, and family history, and a physical examination, your doctor may suggest a number of tests for an appropriate diagnosis. Type 1 diabetes is usually diagnosed when your test results meet at least one of the following criteria:
- Having a fasting blood sugar over 126 mg/dL on two separate tests
- Having one random blood sugar reading over 200 mg/dL and experiencing symptoms of diabetes
- Having a hemoglobin A1c over 6.5 on two separate tests
Because the diagnostic criteria are similar for type 2 diabetes, sometimes misdiagnosis happens. When a person with type 1 diabetes is misdiagnosed with type 2 diabetes, doctors usually only notice the mistake when the patient’s symptoms worsen, or complications occur despite treatment. When a patient’s blood glucose becomes too high, diabetic ketoacidosis happens. This means that the patient becomes very ill and usually ends up at the doctor’s office or in the hospital. It is common for someone to receive a diagnosis of type 1 diabetes after an incident of ketoacidosis.
Since type 1 diabetes can develop quickly and untreated diabetes can become a serious issue, it’s important that you seek medical help if you are experiencing symptoms of type 1 or type 2 diabetes. Doctors may also run specific antibodies to look for autoimmune activity.
The most well studied antibody’s for type I diabetes include Islet Cell Antibody (ICA), Insulin (IAA), Insulinoma Associated Antibody 2 (IA-2), Glutamic Acid Decarboxylase (GAD65) and Zinc Transporter 8 Antibody (ZnT8). ICA and IAA are most common in young children and GAD65 is most common in adults
Conventional Treatment Options
If you have type 1 diabetes, it means that your body is unable to create its own insulin. This means that your doctor will prescribe insulin to support your body in using your blood glucose and control your symptoms. You will need to take insulin daily. While most patients use a daily injection, others may use an insulin pump.
An insulin pump is a port attached under your skin that injects insulin into your body as needed. It is perfect for those who don’t want to inject themselves and also helps with high and low blood glucose levels (6).
Insulin pumps use short-acting and rapid-acting insulin, but not long-acting, since the pump is programmed to deliver a small amount continuously to keep your blood sugar levels even. A pump is more accurate than shots, helping you better manage blood sugar levels. You’ll have fewer blood sugar lows, which is important if you often have hypoglycemia.
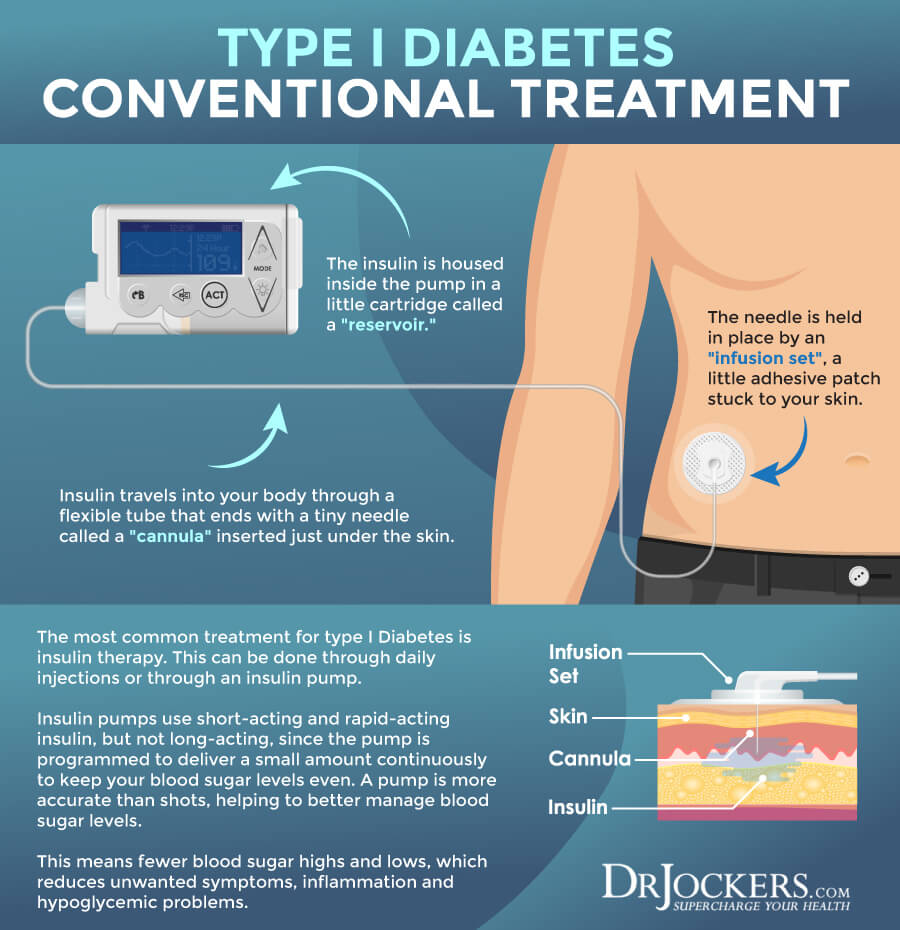
Along with daily insulin, your doctor will likely recommend dietary changes and exercise to help control your blood sugar levels. You will need to get your blood glucose tested regularly to know how much insulin you need (6).
You may also prescribe metformin, an oral diabetes medication (7). In the past, this was only prescribed to those with type 1 diabetes. However, some people with type 1 diabetes can develop insulin resistance and may be prescribed metformin to lower their blood glucose levels by decreasing glucose production in the liver.
Some evidence suggests that two injections of the tuberculosis vaccine may help type 1 diabetes. A 2020 systematic review and meta-analysis of randomized controlled trials published in the Journal of Diabetes Research has found that the bacillus Calmette-Guerin (BCG) tuberculosis vaccine may help patients with type 1 diabetes to stabilize their blood sugar levels for several years (8). However, this treatment option is currently not available on the market as it is still undergoing research and testing and doesn’t have the Food and Drug Administration (FDA)’s approval. Nonetheless, it may become a conventional treatment option in the near future.
Other medications that are currently waiting for FDA approval include Sotagliflozin (Zynquista), an oral medication that can be taken along with insulin (9). This medication helps to lower the absorption of glucose in the gut and also helps to excrete blood glucose through urine. Since similar drugs are already available for type 2 diabetes, there is a good chance that it will be approved for type 1 diabetes in the near future.
Root Cause Factors for Type I Diabetes
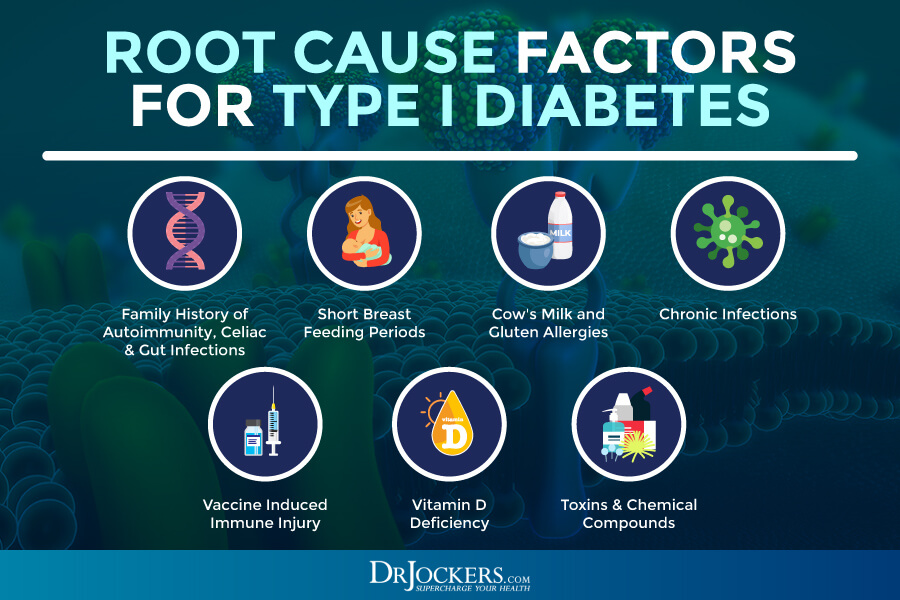
Science is not completely clear on why some people develop type 1 diabetes. However, there is some evidence that certain root cause factors may contribute to or increase the risk of developing type 1 diabetes. Here are the main root cause factors for type 1 diabetes:
Family History of Autoimmunity, Celiac & Gut Infections
Type 1 diabetes is an autoimmune condition. Having one autoimmune condition or having a family history of autoimmunity can increase the risk of developing another autoimmune disease. It’s not surprising that a family history of autoimmunity can increase the likelihood of developing type 1 diabetes. Among all autoimmune conditions, a family history of Celiac disease can be particularly triggering for the development of type 1 diabetes. Besides autoimmunity, gut infections can also increase your risk. Gut infections can increase chronic inflammation and the increased risk of autoimmunity.
A 2005 study published in Pediatric Diabetes has found that certain environmental factors may play a role in young, previously healthy children developing beta-cell autoantibodies (10). Researchers looked at autoantibodies to glutamic acid decarboxylase (GAD) and autoantibodies to tyrosine phosphatase (IA-2A) in 1-year-old children to check their risk factors for type 1 diabetes.
Out of 6,000 children, 126 children had both GADA and IA-2A and 1156 children had one of these two autoantibodies. They found that drinking cow’s milk formulas, low education level of the mother, and being born in the spring can increase the risk. More interestingly, they found that celiac disease in grandparents, maternal gastrointestinal infection, type 2 diabetes in grandparents can also increase the risk of autoantibodies and the risk for type 1 diabetes in children.
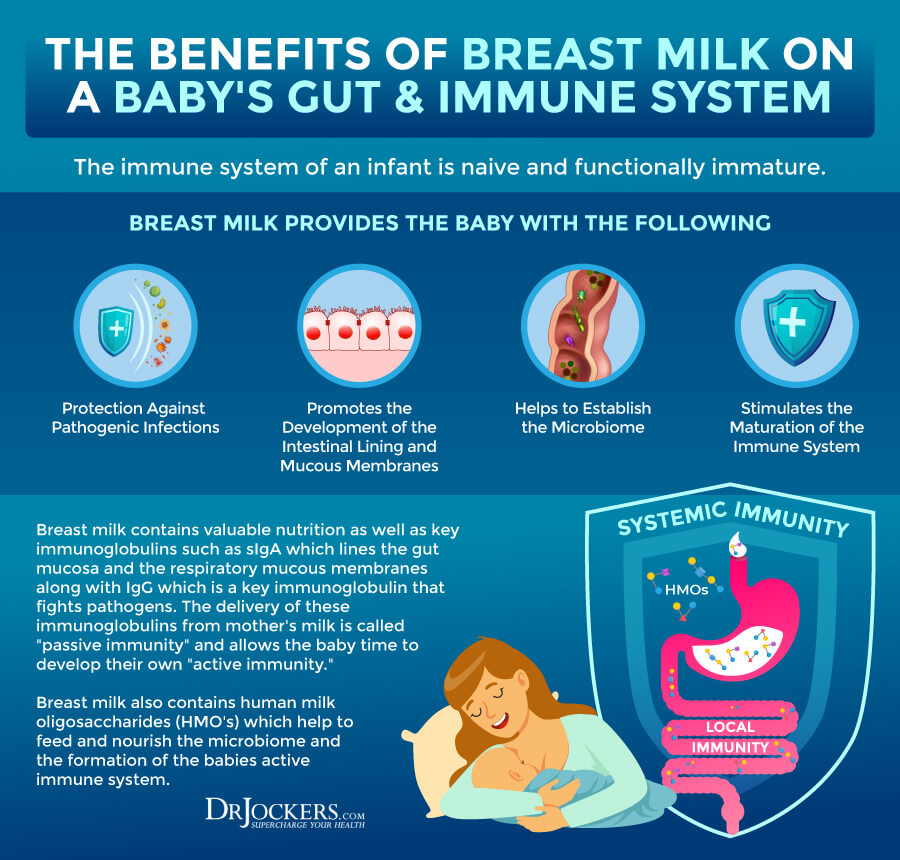
Short Breastfeeding Periods
Breast-feeding is incredibly important for a baby’s development. It is not only nourishment for the child but helps them to develop their immune system and strengthen their digestion. Since type 1 diabetes often develops during childhood, it may not surprise you that short-term breastfeeding may contribute to the risk of developing type 1 diabetes.
A 2001 study published in Diabetologia has found that babies who were breastfed only for short-term, or less than 4 months, had an increased risk of progressive beta-cell autoimmunity and type 1 diabetes (11). They also found that children who were breastfed for at least 4 months had a reduced risk of developing type 1 diabetes.
A 2007 study published in the British Journal of Nutrition looking at 5-year-old children has also found breastfeeding and the early introduction of formulas may be linked to an increased risk of GADA, IAA and/or IA-2A and the risk of type 1 diabetes (12). A 2016 review published in Lancet has found that breastfeeding may play a protective role and still breastfeeding when introducing cereals to the child’s diet may reduce the risk of type 1 diabetes and autoimmunity (13).
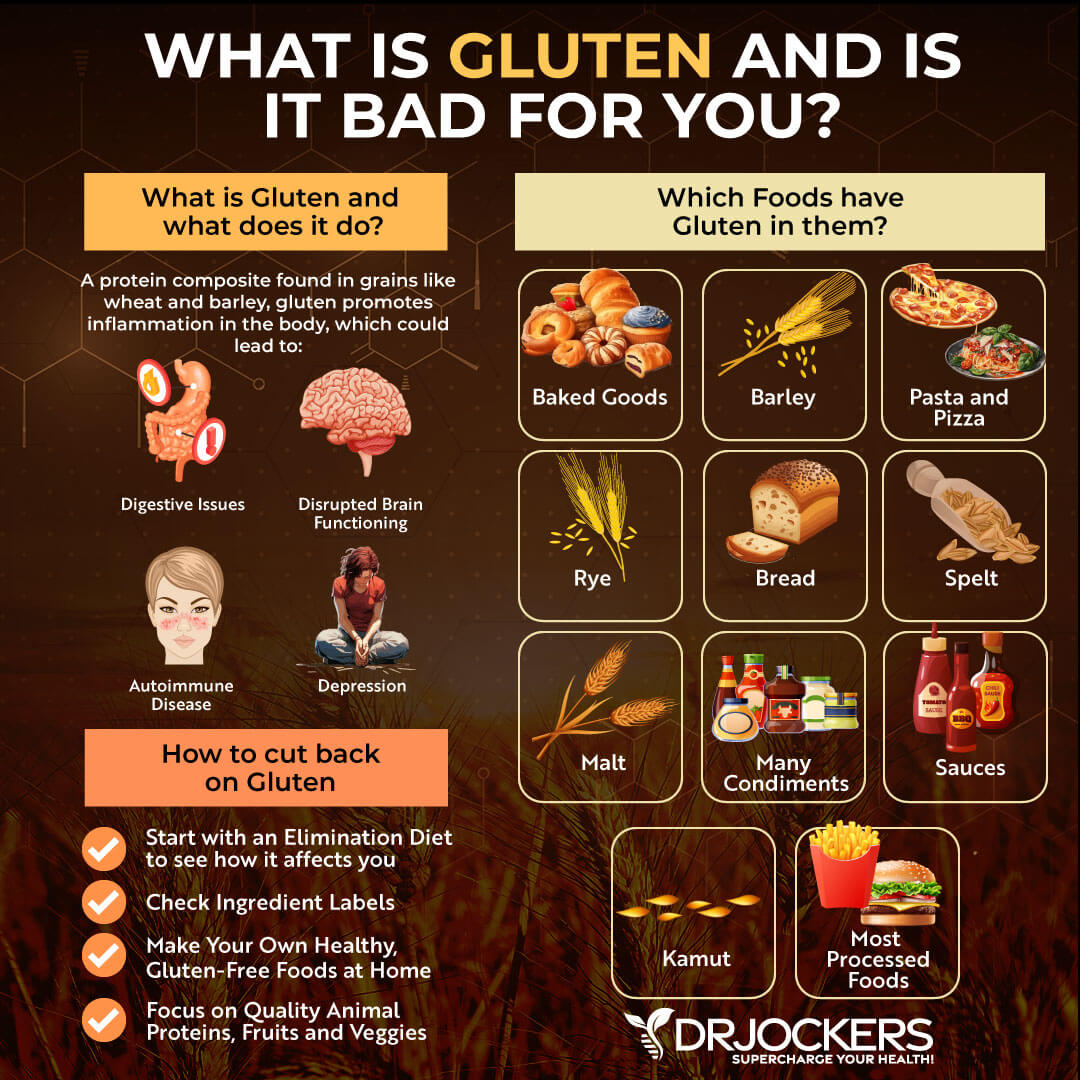
Cow’s Milk and Gluten Allergies
The pregnant and breastfeeding mother’s diet and the diet of the infant are critical for the growing baby’s development and health. It may also affect the child’s health growing up. Exposure to cow’s milk and gluten allergies may increase the risk of developing type 1 diabetes.
Cow’s milk is a common cause of food allergies and food sensitivities. It also increases the risk of gut health issues, inflammation, and autoimmunity. Increasing evidence suggests that it may contribute to the development of type 1 diabetes. A 2000 study published in BMJ has found that early exposure to cow’s milk during pregnancy can increase the risk of type 1 diabetes in children (14).
A 2015 study published in Pediatric Diabetes has found that cow’s milk during childhood may be associated with islet autoimmunity and type 1 diabetes (15). A 2021 study published in Pediatric Diabetes has also found that cow’s milk introduced during pregnancy may result in type 1 diabetes later on (16).
Gluten is another common allergen and cause of food sensitivities, inflammation, and other health issues. Eating gluten during pregnancy or feeding gluten to the child may also contribute to type 1 diabetes. A 2014 review published in Diabetologia has found that dietary gluten in children may contribute to the development of type 1 diabetes (17).
A 2018 study published in Nutrients has found that following a gluten-free diet during pregnancy may reduce the risk of type 1 diabetes in the child (18). A 2016 review published in Lancet has also linked cow’s milk and gluten-containing cereals to the increased risk of type 1 diabetes and autoimmunity (13).
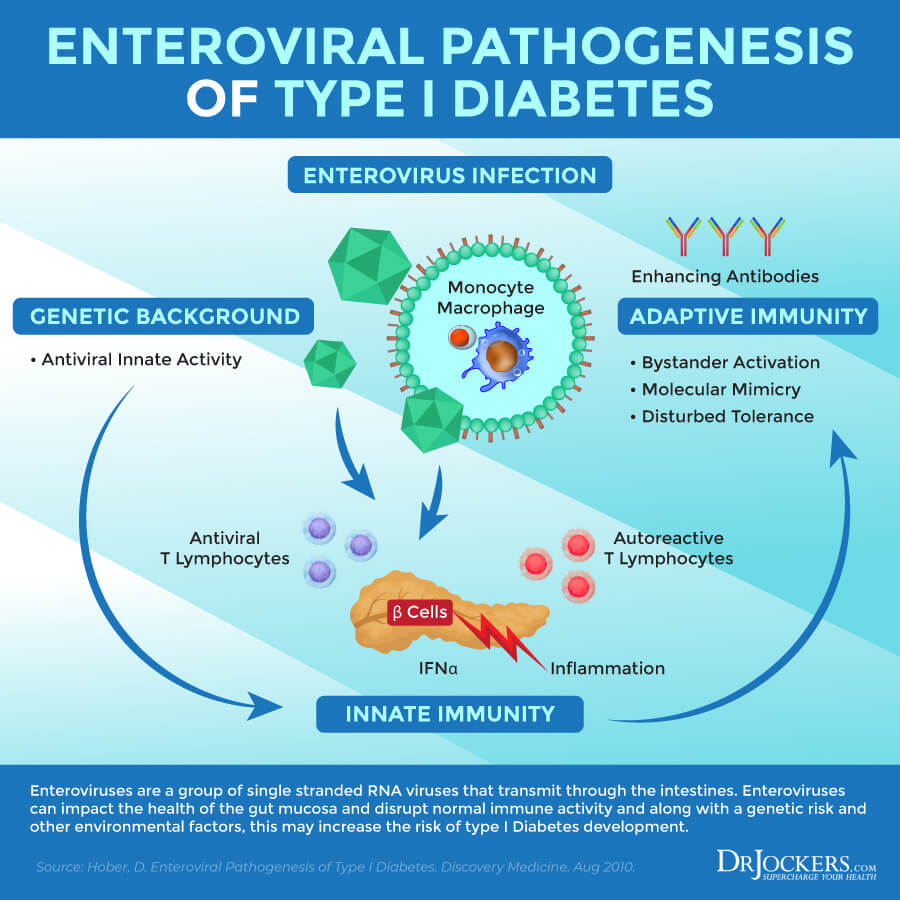
Chronic Infections
Chronic infections are often the cause of autoimmune and chronic health conditions. Type 1 diabetes is no different. A 2016 review published in Lancet has found that chronic infection may increase the risk of type 1 diabetes and autoimmunity (13). Though viral infections are more well researched and understood, according to the review, we cannot completely rule out bacterial infections either as a potential contributing factor to type 1 diabetes.
A 2014 review published in the Journal of Pathogens has found that genus enteroviruses, such as Enterovirus A, Enterovirus B, Enterovirus C, and Enterovirus D and Rhinovirus A, Rhinovirus B, and Rhinovirus C, may increase the risk of type 1 diabetes (19). A 2012 study published in Diabetes has found that enteroviruses may interfere with the healthy functioning of the gut mucosa and increase the risk of beta-cell damage and type 1 diabetes (20).
A 2011 review published in Seminars in Immunopathology has also found that enteroviral infections can affect the health of the gut mucosa and pancreatic health thus may play a role in the pathogenesis of type 1 diabetes (21). A 2012 review published in Reviews in Diabetes Studies has suggested that targeting viral infections may help to prevent type 1 diabetes (22).
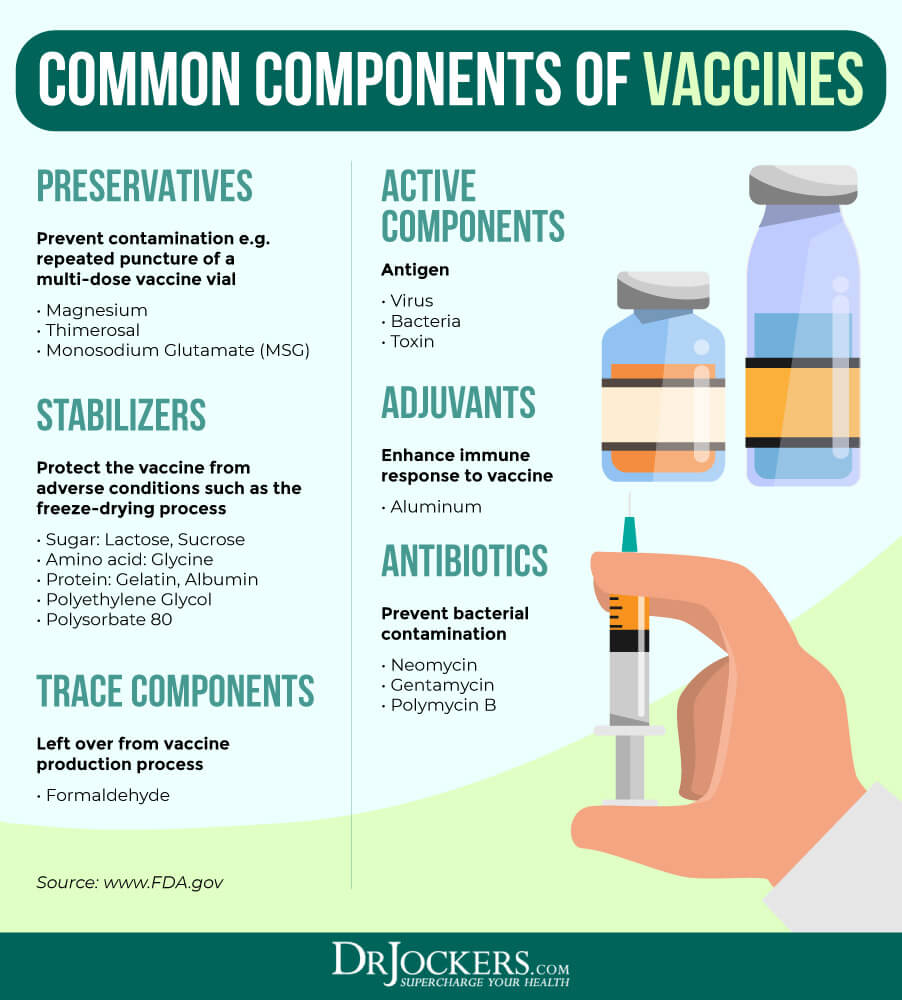
Vaccine-Induced Immune Injury
Vaccination is a controversial subject. Childhood vaccinations have rapidly increased over the past decades. According to the National Vaccine Information Center, children currently get 34 doses of 10 viral and bacterial vaccines before they turn 5 or enter kindergarten (23). The problem is that while their vaccines may help to reduce the risk of certain infections, they don’t go without some serious health risks and issues. For example, they may contribute to the development of type 1 diabetes.
For example, according to the National Vaccine Center, the mumps and rubella virus can both impact the pancreatic islet cells and mumps live vaccines may also do the same increasing the risk of type 1 diabetes (23). They may also increase the risk of inflammation, gut health issues, and other issues that may cause autoimmunity. A 2016 review published in Lancet has found an association between the BCG vaccine and the risk of type 1 diabetes and autoimmunity (13).
A 2003 study on 4400 children published in the Annals of the New York Academy of Sciences has found the vaccinations may affect GADA and IA-2A and increase the risk of type 1 diabetes in children (24). A 1999 study published in BMJ has warned against the long-term effects of vaccines and recommended that the public needs to be more informed about them (25). The study has found that vaccines may increase the risk of type 1 diabetes.
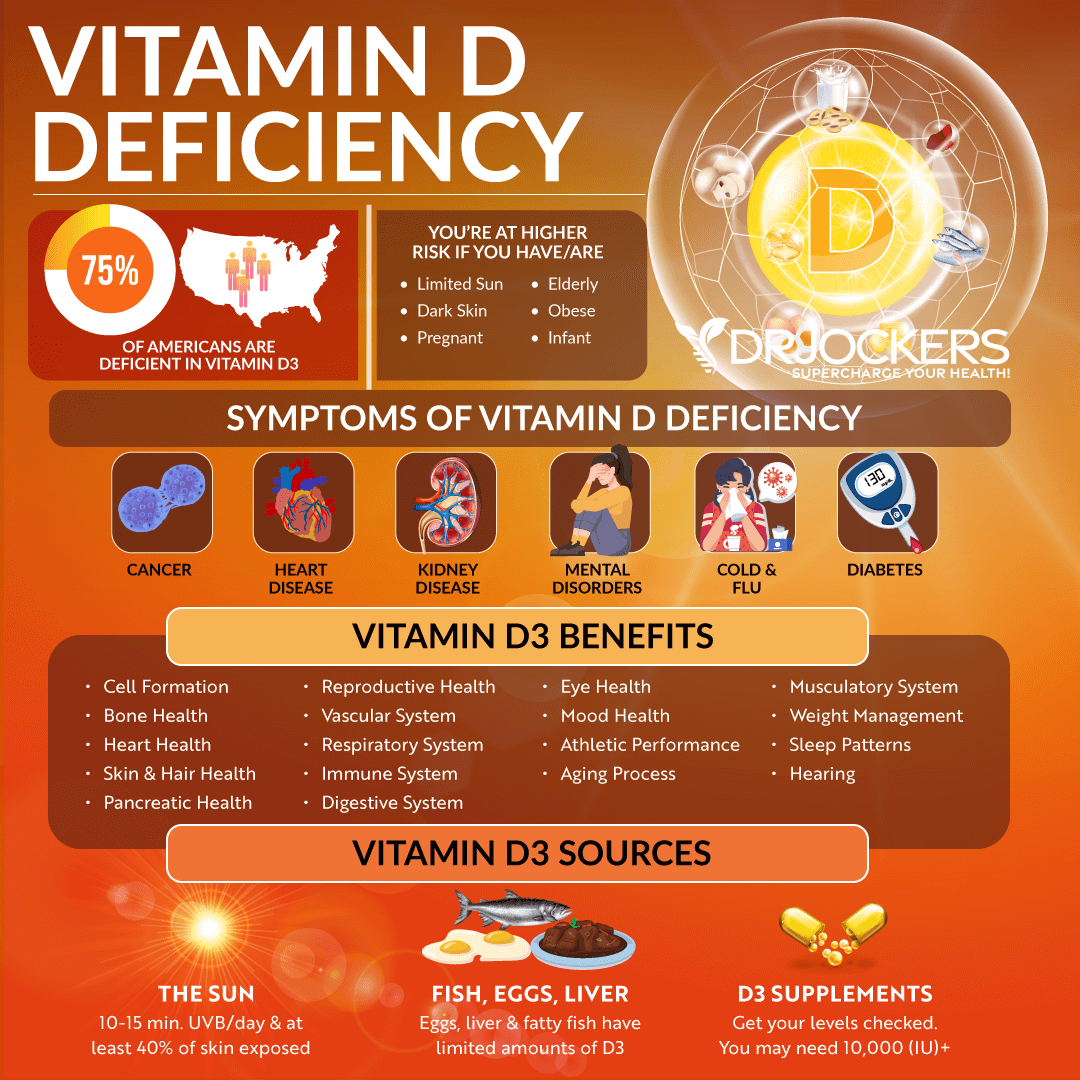
Vitamin D Deficiency
Vitamin D is a very important nutrient for immune health, brain health, bone health, and other areas of your health. A 2016 review published in Lancet has explained that vitamin D is critical for immune and metabolic pathways that play a role in the development of type 1 diabetes (13).
While us adults meet our vitamin D needs through sun exposure, diet, and supplementation, babies rely on their mother. After birth, they received most of their vitamin D through breast milk, and before birth through the umbilical cord. Maintaining optimal vitamin D levels during pregnancy is critical to prevent pre-eclampsia, low birth weight, preterm birth, and other complications.
A 2009 review published in Acta Diabetologia has found that there may be a connection between vitamin D deficiency early in life and developing type 1 diabetes later (26). A 2013 study published in the International Journal of Endocrinology has also found that vitamin D deficiency is common in type 1 diabetes (27). This is important to note because vitamin D plays a role in pancreatic and immune health, and deficiencies may increase the risk of type 1 diabetes or worsen its symptoms.
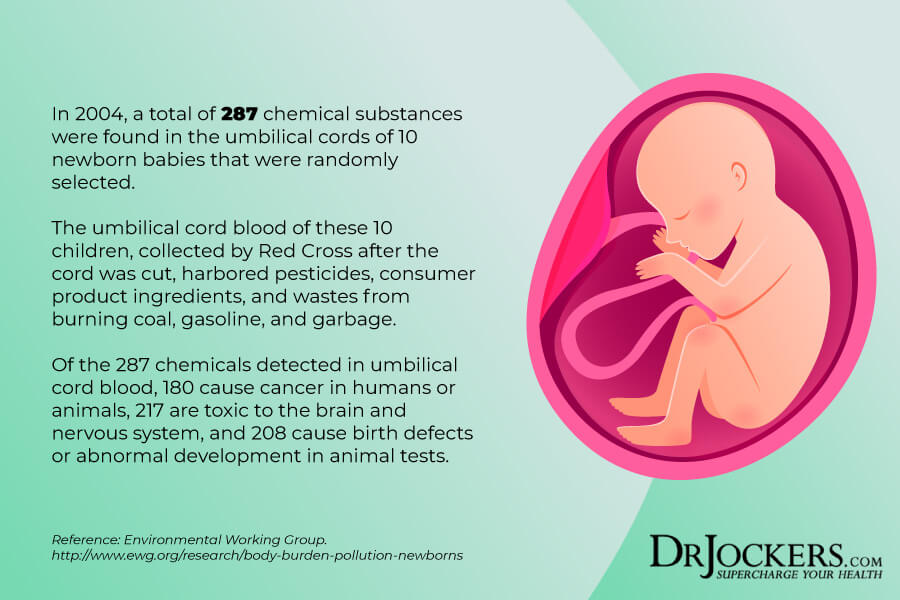
Toxins & Chemical Compounds
Our modern world has brought us a lot of technological advances and other conveniences. Unfortunately, these advances and our modern life didn’t come without toxins and chemicals. Exposure to toxins and chemical compounds, however, can greatly impact our health and among other health issues, can increase the risk of type 1 diabetes.
A 2016 review published in Lancet has found that toxins in food and water and various mycotoxins may increase the risk of type 1 diabetes and autoimmunity (13). A 2019 review published in the Journal of Epidemiology Community Health has found that environmental toxins, including air pollution, arsenic, pesticides, persistent organic pollutants, bisphenol A, and phthalates, can increase the risk of type 1 diabetes (28).
A 2018 study published in Frontiers in Endocrinology (Lausanne) has found that exposure to endocrine-disrupting chemicals in early life can increase the risk of type 1 diabetes (29). A 2020 study published in the International Journal of Molecular Sciences has found that endocrine-disrupting chemicals can interrupt beta-cell and immune function and contribute to the development of type 1 diabetes (30).
Natural Support Strategies
If you have type 1 diabetes, there are some natural support strategies that can help to support your health and wellness. Here is what I recommend:
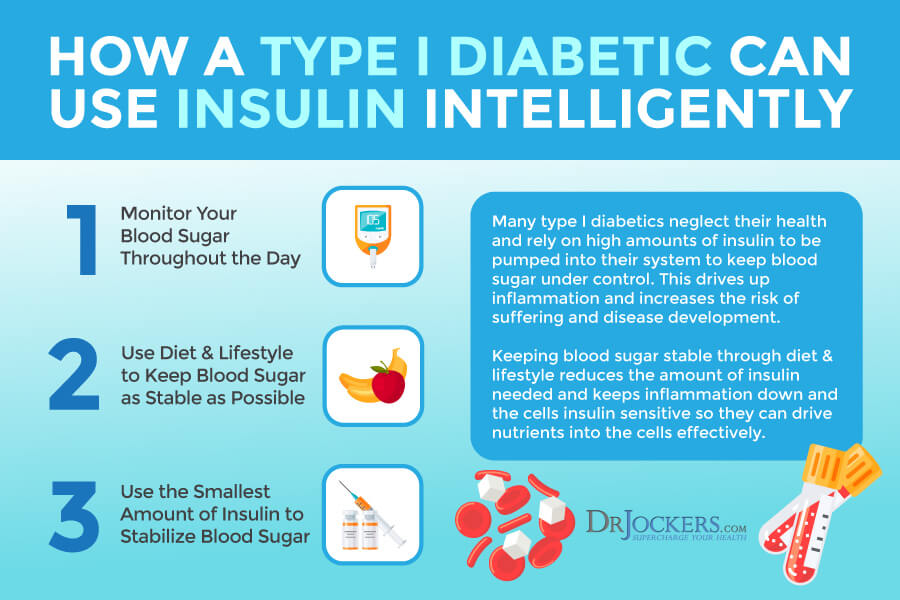
Use Insulin Intelligently and Monitor Blood Sugar
Having type 1 diabetes means that your body cannot make insulin (1). This means that you have to administer insulin. However, it’s critical that you use insulin intelligently and monitor your blood sugar levels. Keep up with your doctor’s appointments, get your blood sugar tested at your doctor’s office, and get other necessary lab work done to monitor your health.
Monitor your blood sugar at home. Make sure to keep your blood sugar levels stable with the help of a healthy diet and lifestyle, so you only need to administer the smallest amount of insulin possible, yet stay healthy and energized. In the next sections, I will share some dietary and lifestyle strategies that can help to keep your blood sugar stable and stay well.
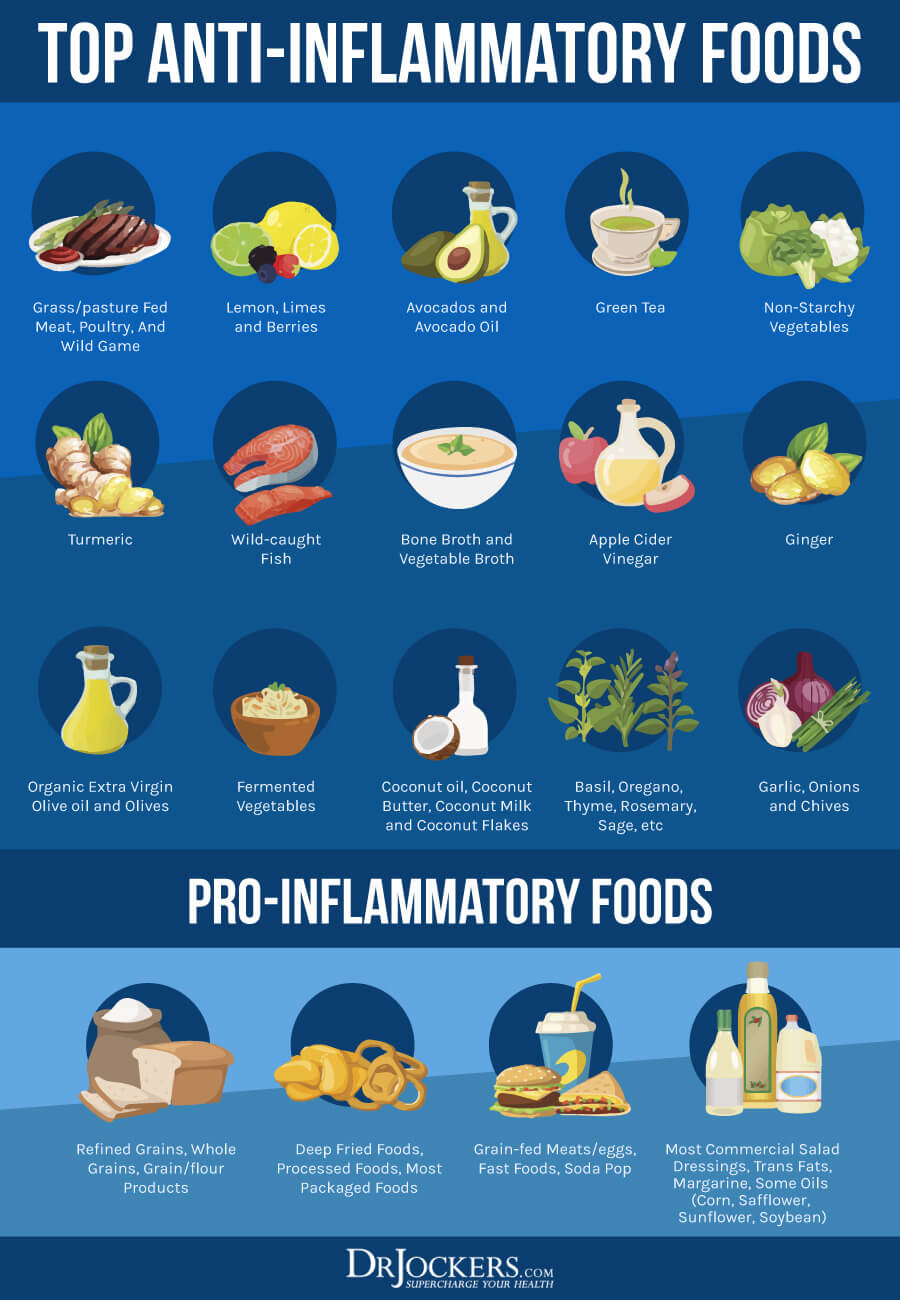
Anti-Inflammatory Nutrition Plan
According to a 2007 study published by the Beth Israel Deaconess Medical Center, decreasing inflammation is one of the most important things that can support the treatment and management of type 1 diabetes (31). Diet is definitely a big part of that.
Avoid inflammatory foods, including refined sugars and carbs, refined oils, highly processed foods, junk food, additives, preservatives, and unnatural ingredients. I recommend that you follow an anti-inflammatory nutrient plan high in greens, vegetables, a limited amount of low-glycemic index fruits, herbs, spices, fermented foods, grass-fed beef, grass-fed butter and ghee, pasture-raised poultry and eggs, wild-caught fish and seafood, and wild game. I recommend that you eat a high-fat, low carbohydrate diet. Eat plenty of healthy fats, such as grass-fed butter and ghee, lard, coconut oil, coconut, avocados, avocado oil, extra virgin olive oil, and olives.
Choose organic options whenever it’s possible and available to you. If you are unable to find or afford organic options for all your produce, I recommend that you follow the rule of the dirty dozen and clean fifteen. If food is on the list of dirty dozen, it’s important that you always choose organic. If it’s on the list of clean fifteen, organic is still ideal, but if it’s not available, you may choose non-organic. If your product is not organic, make sure to wash it very well and peel it if possible.
Test for and Avoid Food Sensitivities
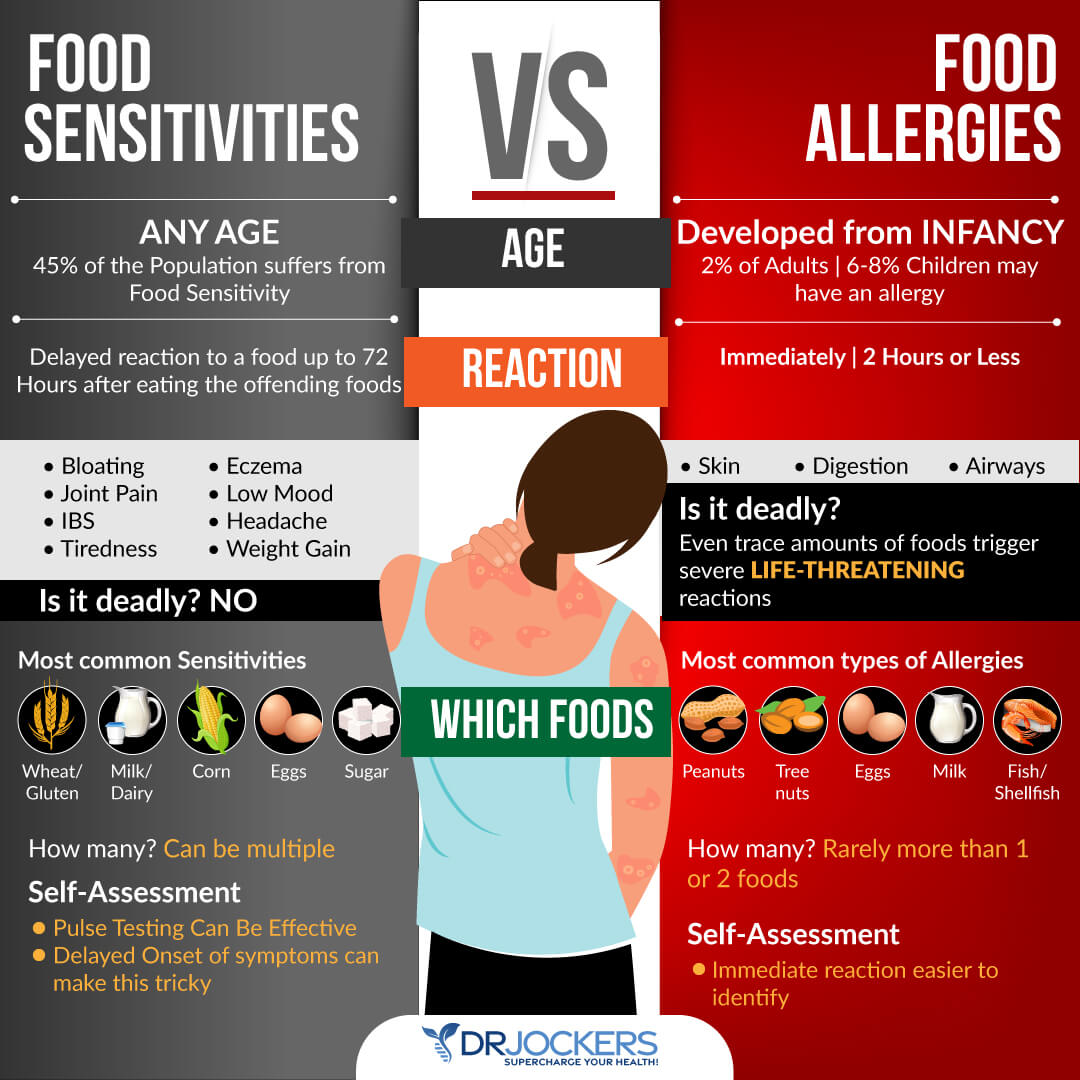
Food sensitivities are different from food allergies. Food allergies cause an immediate reaction, including hives, difficulty breathing, puffiness, digestive issues, or other symptoms after eating a food that you are allergic to. Food sensitivities, on the other hand, don’t lead to an immediate reaction but will result in chronic issues over time. You may eat food and only experience symptoms a few hours or days later, and inflammation and internal damage may also occur over a period of weeks, months, or even years.
Sensitivities to gluten, cow’s milk, and dairy can contribute to the symptoms and risk of type 1 diabetes n (14, 15, 16, 17, 18, 13). Other food sensitivities can also increase inflammation which can interfere with the management of type 1 diabetes (31). Common food sensitivities include gluten, dairy, sugar, corn, soy, eggs, legumes, and shellfish. However, you may find that you are sensitive to other, less common, foods.
I recommend that you test for food sensitivities and avoid foods that you are sensitive to. There are various blood tests that can help identify food sensitivities. However, they don’t test for every food, and false results can also happen. To understand your body better and test for all foods you consume, beyond blood tests, I recommend that you try an elimination diet, pulse test, or muscle response testing. You can find information on these on my website.
Once you find your sensitivities, it is important that you immediately remove them from your diet. However, food sensitivities can change over time. I recommend that you test for them regularly, at least once a year, or if new symptoms occur. If you find new food sensitivities, remove them from your diet. You may also find that your recovery from certain food sensitivities over time. However, I recommend that you stay away from gluten, refined sugar, and conventional dairy for good.
Reduce Stress & Improve Sleep
Reducing inflammation is one of the most critical aspects of managing type 1 diabetes (31). Since chronic stress and poor sleep can both increase inflammation, reducing stress and improving your sleep are both critical. When you are stress or tired, you are more likely to experience sugar cravings or reach for unhealthy snacks and comfort foods, which can interfere with your blood sugar balance. This makes stress reduction and quality sleep even more important.
To reduce your stress levels, I recommend that you try meditation, breathwork, guided relaxation, visualization, positive affirmation, gratitude, positive thinking, journaling, and prayer. Spend time in nature and move your body regularly. Spend time with loved ones. Seek a supportive and uplifting community. But don’t forget to have regular me-time as well.
To ensure quality sleep, I recommend that you avoid electronics, food, alcohol, sugar, and caffeine in the evening. Find relaxing activities that help you relax and wind down, such as arts and crafts, coloring, board games, crossword puzzles, playing cards, supportive conversations, reading, taking a healing bath, sipping on herbal tea, meditation, journaling, or prayer.
Make sure that your bedroom is a supportive sanctuary with a supportive mattress, comfortable pillows, and bedding. Try using an essential oil diffuser with some calming oils like lavender oil or a salt lamp for further calm.

Regular Movement & Exercise
Another way to reduce inflammation to support type 1 diabetes management is movement and exercise (31). A 2019 study published in Frontiers in Endocrinology (Lausanne) has found that young people with type 1 diabetes are often afraid of exercise because they fear hypoglycemia (32). Yet exercise is very important. Consulting with your doctor can help to remove fear and learn how to exercise safely.
According to the American Diabetes Association, before you start exercising, it’s important that you make sure that your blood sugar levels are stable (33). Always consider how certain exercises are affecting you and adjust your activity, diet, and insulin accordingly. Try to sit less, and it’s associated with higher blood sugar levels.
Stay active throughout the day. Start your day with stretching, yoga, or a short walk. Get up and stretch and move your body regularly instead of sitting in front of the screen all day. Aim to shake out your body a bit every hour. Take a stroll during lunchtime if you can. Take the stairs, walk or bike instead of driving whenever possible, play with your kids or pets, dance to your favorite song, or schedule a social walk. Go for a hike or find another outdoor activity over the weekend.
Exercise regularly. Aim for 5 times a week for at least 20 minutes a day. Practice a mix of strength and resistance training, such as bodyweight workouts, exercises with resistance bands, weight training, CrossFit, kettlebell workouts, or TRX, cardiovascular workouts, such as jogging, swimming, biking, dancing, or aerobics classes, and low-impact activities, such as yoga, Pilates, barre workouts, walking, swimming, TaiChi, QiGong, or aqua fitness classes. Always consult your doctor before starting an exercise routine and monitor your blood sugar levels.

Optimize Vitamin D Levels
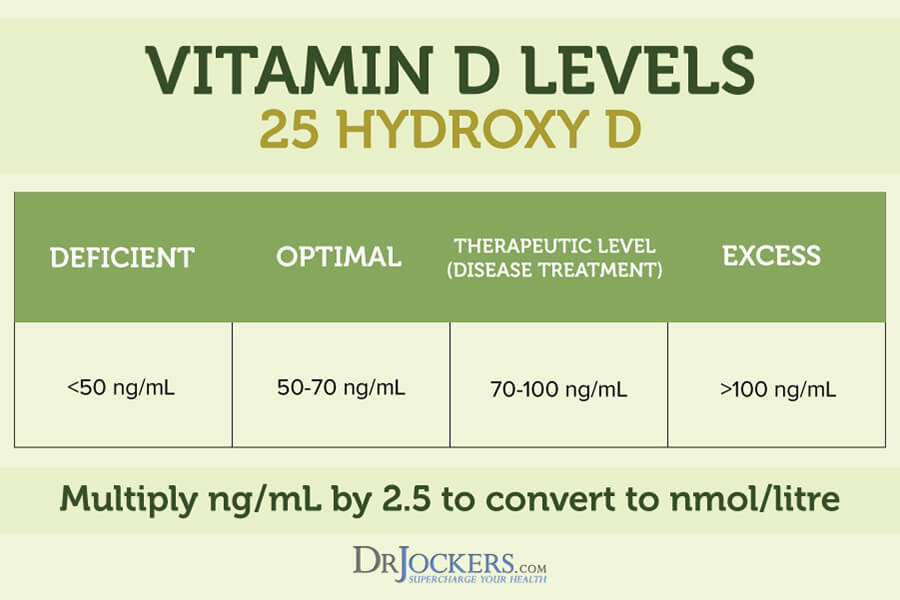
According to a 2013 study published in the International Journal of Endocrinology, vitamin D deficiency is common in type 1 diabetes (27). Optimizing your vitamin D levels is important for managing type 1 diabetes and reducing the risk of complications and worsening symptoms.
A 2010 study published in the Annals of Saudi Medicine has found that supplementing with 4,000 IU of vitamin D over 12 weeks helped to improve the glycemic score of patients with type 1 diabetes (34). A 2014 study published in Minerva Pediatrics has found that supplementing with 50,000 IU of vitamin D3 biweekly for 3 months helped to improve the HbA1C levels of children and adolescents with type 1 diabetes (35). Furthermore, a 2018 study on children with type 1 diabetes published in Pediatric Endocrinology, Diabetes, and Metabolism has found that 3,000 IU/day vitamin D supplementation for a year has helped to slow the decline of beta-cell function and improve glycemic control (36).
Most people are not getting enough sunshine or consuming enough vitamin D from food. Therefore, most people need to supplement to optimize their vitamin D levels. As you can see from these research studies, supplementation can be particularly beneficial for those with type 1 diabetes. Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and inflammation control. I recommend taking a vitamin D3 supplement with at least 3,000-5,000 IU’s of vitamin D3 and at least 90 mcg of vitamin K2.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for major health conditions is going to be between 70-100 ng/ml.
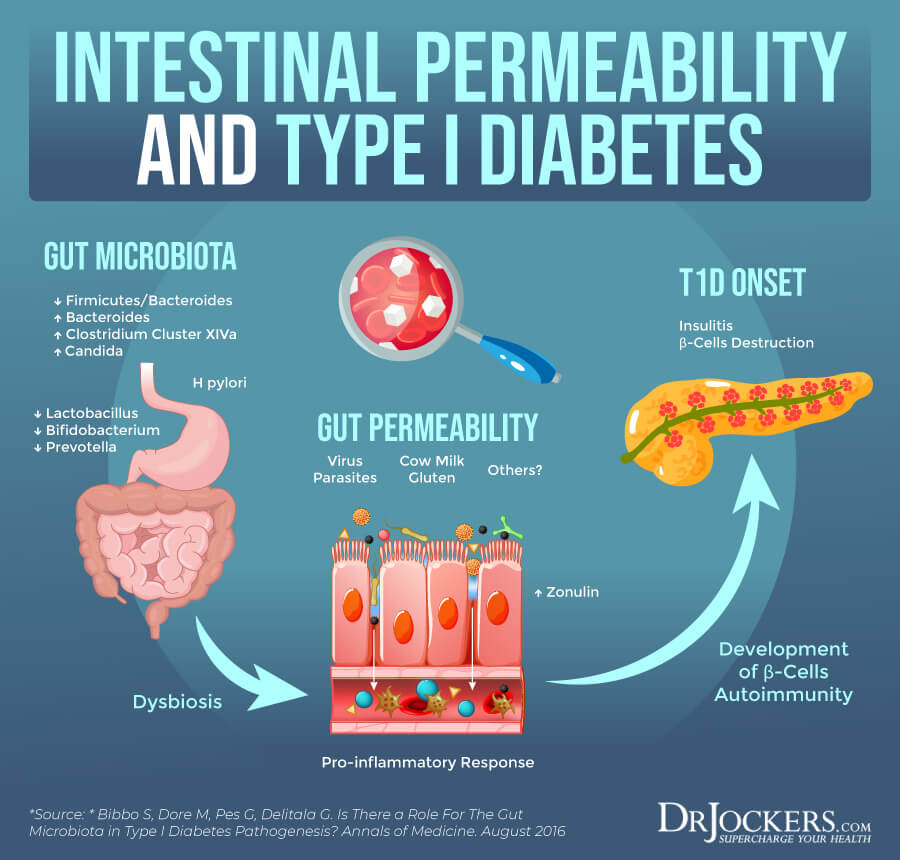
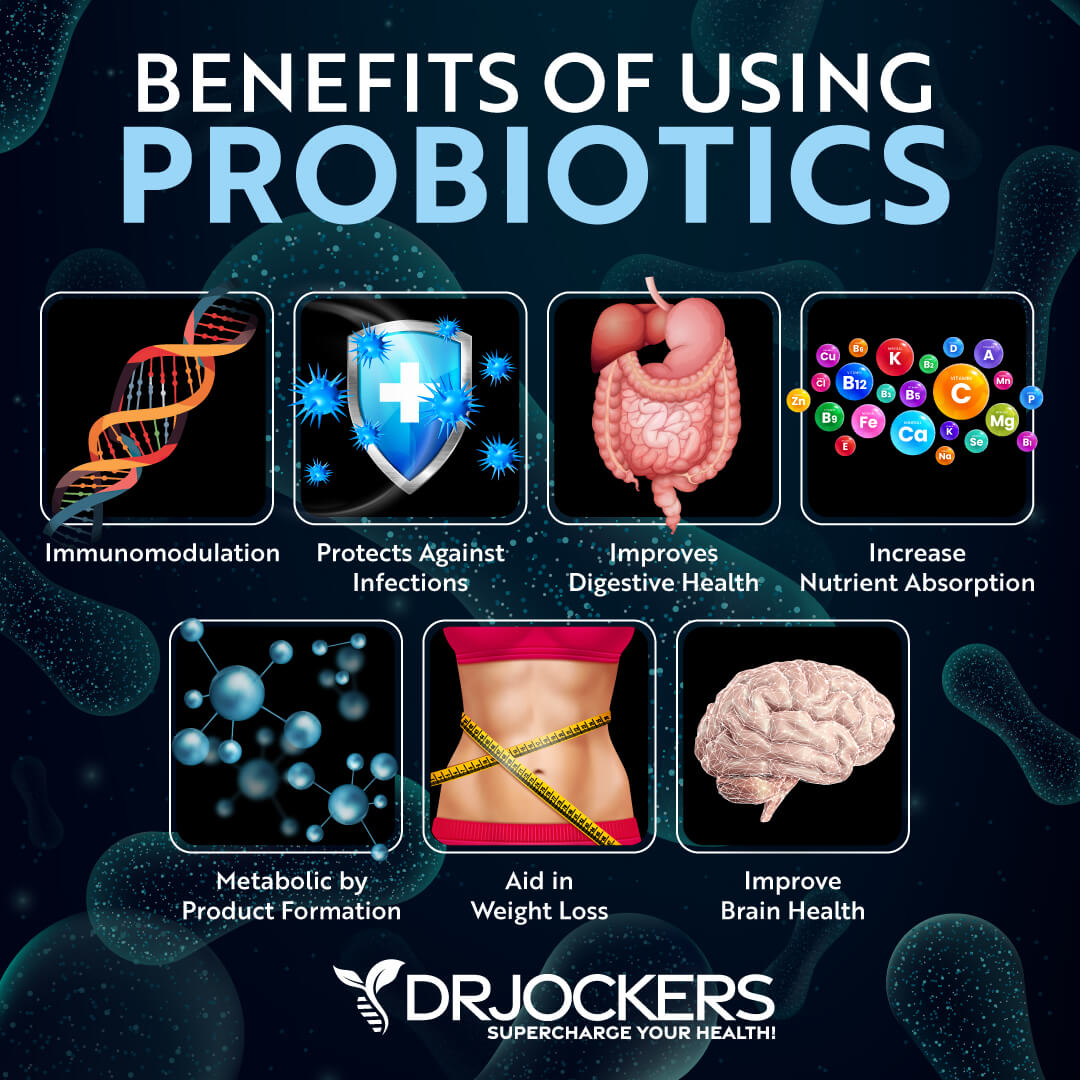
Use Probiotics
A poor microbiome balance can increase inflammation and increase the risk of or symptoms of all kinds of health issues. Taking probiotics to support your microbiome balance can also help with type 1 diabetes. Prebiotics are the fiber that feed and support probiotics and may further support your gut health.
A 2019 review published in Microorganisms has found that probiotics and prebiotics may help to reduce the destruction of beta-cells, lower inflammation, decrease an autoimmune response, and restore gut integrity in type 1 diabetes (37). A 2020 systematic review and meta-analysis has also found the probiotics and prebiotics may help to improve metabolic outcomes, glucose control, and gut microbiome balance in type 1 diabetes (38).
I recommend taking a high-quality probiotic supplement daily. I also recommend eating probiotic-rich fermented foods, such as kimchi, sauerkraut, fermented vegetables, coconut kefir, and kombucha, to support your microbiome balance through diet as well.
You may also add some prebiotic-rich foods, including garlic, onion, leeks, asparagus, Jerusalem artichokes, jicama, chicory roots, and dandelion greens. However, not everyone does well with prebiotics. If you are on a low-FODMAP diet or the carnivore diet for another health reason, or you are experiencing digestive issues when consuming too many prebiotic-rich foods, cut back on your prebiotic intake. The key is to always listen to your body.
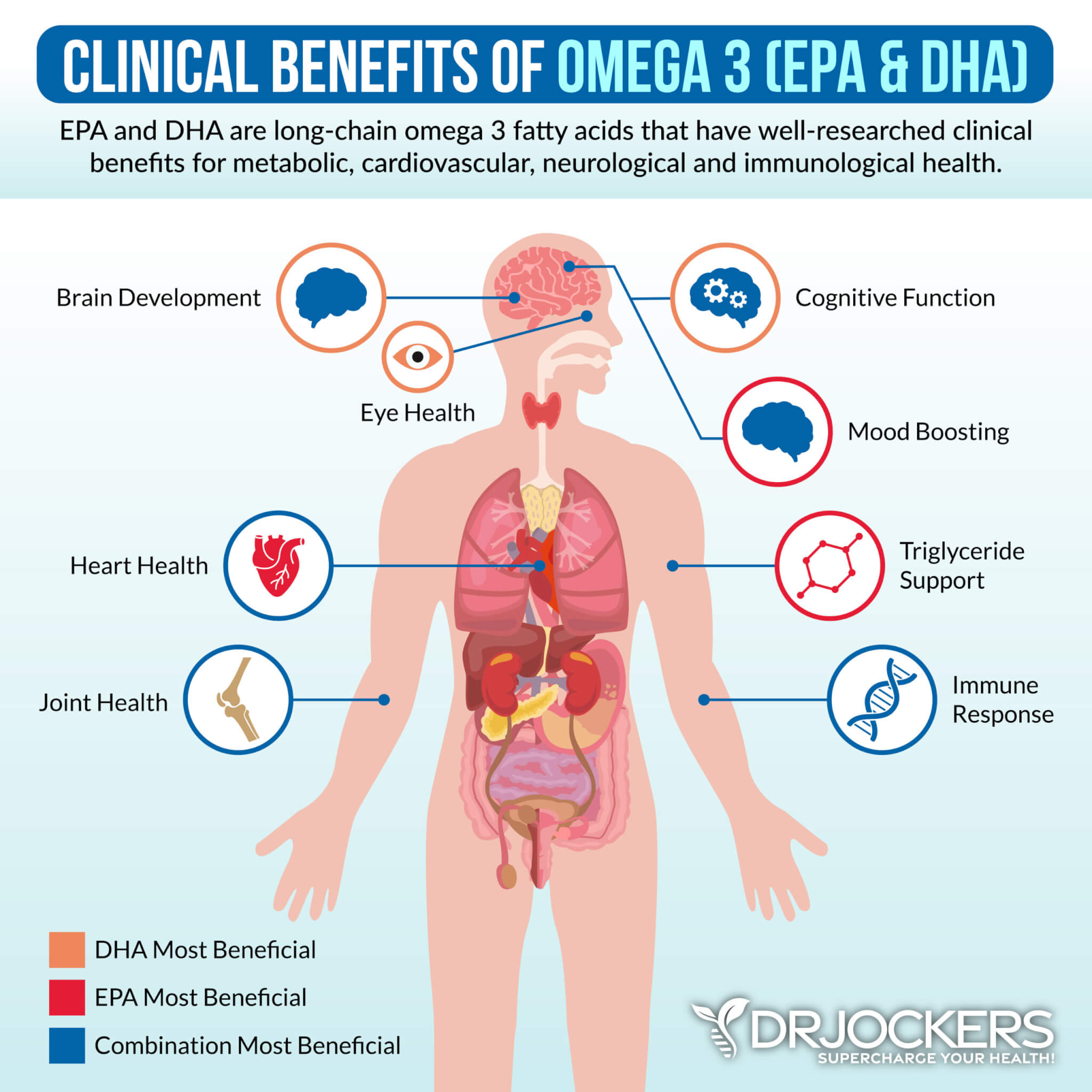
Use Omega-3 Fatty Acids
Omega-3 fatty acids are anti-inflammatory fatty acids found in algae, fish, seafood, hemp seeds, flax seeds, and chia seeds. Using omega-3 fatty acids may be a good idea if you have type 1 diabetes. A 2017 study published in the Journal of Clinical Investigation has found that omega-3 fatty acids may help to reduce autoimmunity (39).
I recommend consuming a lot of foods that are rich in omega-3 fatty acids, including wild-caught fish and seafood, hemp seeds, chia seeds, and flax seeds. To reduce inflammation and optimize your health, I recommend that you also take a high-quality omega-3 fish oil supplement every day.
Support Magnesium and Zinc Levels
Magnesium is an essential mineral for your blood sugar levels, brain health, muscle health, mental health, blood pressure levels, and other areas of your health. Zinc is another critical mineral for your immune health and metabolic function. Taking magnesium may be a good idea if you have type 1 diabetes.
A 2015 review published in the Current Opinions of Clinical Nutrition and Metabolic Care magnesium, zinc, and chromium may help with glycemic control in type 1 diabetes (40). A 2019 study published in Biometals also found the magnesium, zinc, copper, and selenium can support patients with type 1 and type 2 diabetes (41).
I recommend that you add foods that are rich in magnesium, such as greens, nuts, and seeds, and foods that are rich in zinc, such as grass-fed beef, pasture-raised poultry and eggs, wild-caught seafood, nuts, and seeds. Meeting your daily needs and optimizing your magnesium and zinc levels through diet alone, however, is difficult. I recommend taking a high-quality magnesium and zinc supplement daily.

Consider Using Resveratrol
Resveratrol is found in the skin of grapes, red wine, and berries. It is a plant compound that acts as an antioxidant and helps to reduce inflammation. A 2017 study published in the Journal of Exploratory Pathology has found that resveratrol may be beneficial for those with type 1 diabetes (42). A 2020 study published in Nutrients has found that resveratrol can act as an anti-inflammatory and antidiabetic agent and is safe and effective for patients with type 1 diabetes (43).
I recommend eating foods high in resveratrol, including grapes, blueberries, cranberries, pistachios, and cacao. I recommend supplementing with resveratrol to lower inflammation levels and improve your blood sugar levels.

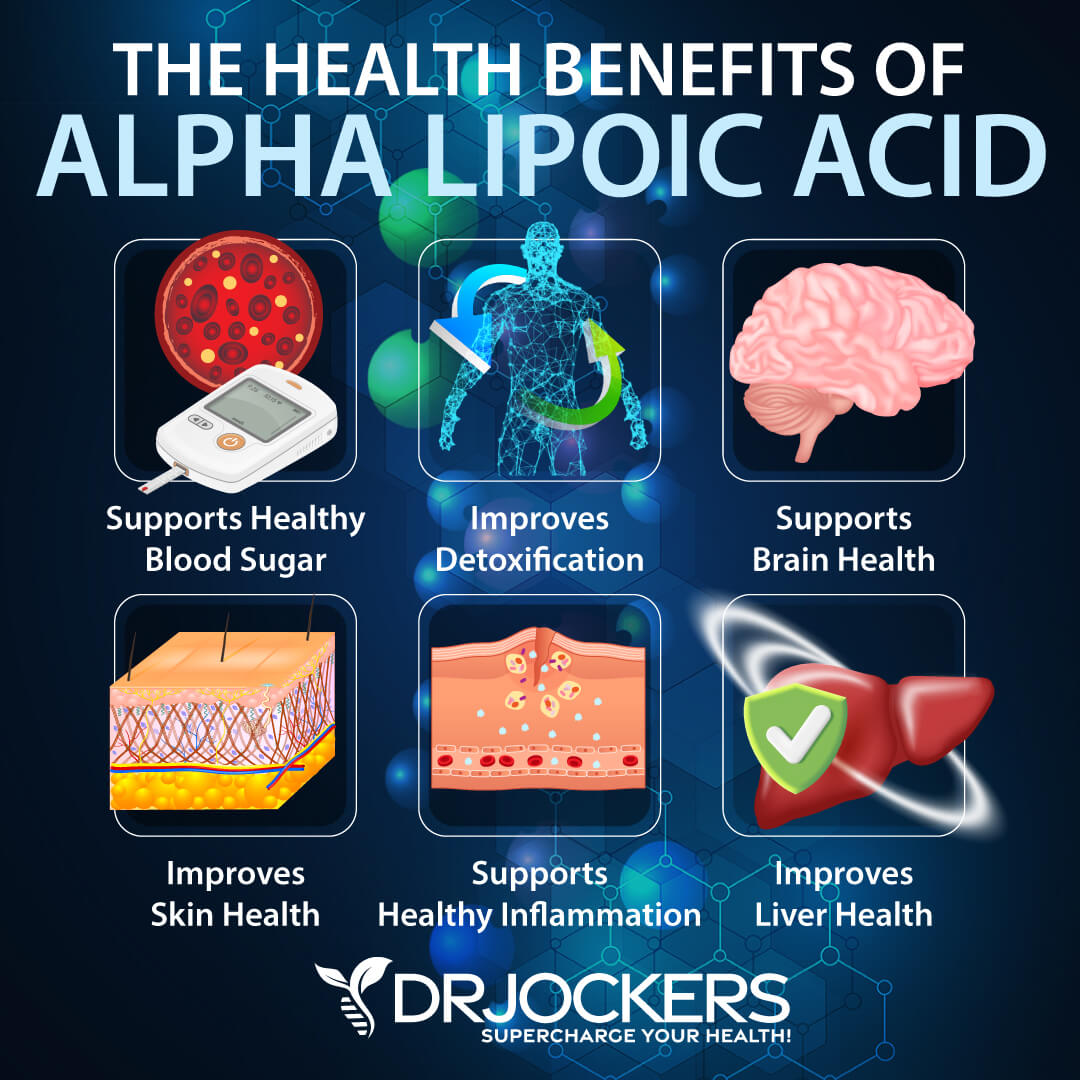
Consider Using Alpha-Lipoic Acid
Alpha-lipoic acid is an antioxidant that may benefit those with diabetes. A 2008 review published in Nutrition Reviews has found that alpha-lipoic acid helps to improve insulin resistance, diabetic neuropathy, and oxidative stress in diabetic patients with type 1 or type 2 diabetes (44). A 2011 study published in the Frontiers of Pharmacology has found that alpha-lipoic acid is safe for diabetic patients and may help with diabetic neuropathy (45).
I recommend eating foods high in alpha-lipoic acid, including kidney, liver, spinach, eggs and broccoli. I also recommend daily supplementation with alpha-lipoic acid.
Final Thoughts
Type 1 diabetes is a chronic disease. If you have type 1 diabetes, it means that your body is unable to make insulin to handle the blood glucose circulating in your system. If you have type 1 diabetes, you need to take daily insulin.
However, you can still support your health and improve your condition through diet, lifestyle, and supplementation. I recommend that you follow top natural support strategies for those with type 1 diabetes to improve your health.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. We do offer long-distance functional health coaching programs. For further support with your health goals, just reach out and our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!



Another root cause I’d include (the most likely in my opinion) is the absence of pathogens. When our genetics have been tailored to fight off infections and these infections no longer exist autoimmunity happens. The countries with the lowest incidence of type I diabetes are also countries with a high risk of infectious diseases.
Yes agreed!