 Chronic Pain: Root Causes and Natural Support Strategies
Chronic Pain: Root Causes and Natural Support Strategies
Everyone experiences pain in their life regularly. You may accidentally cut your finger in your kitchen, stub your toe, twist your ankle, or feel sore after a workout. Pain becomes a problem when it’s chronic.
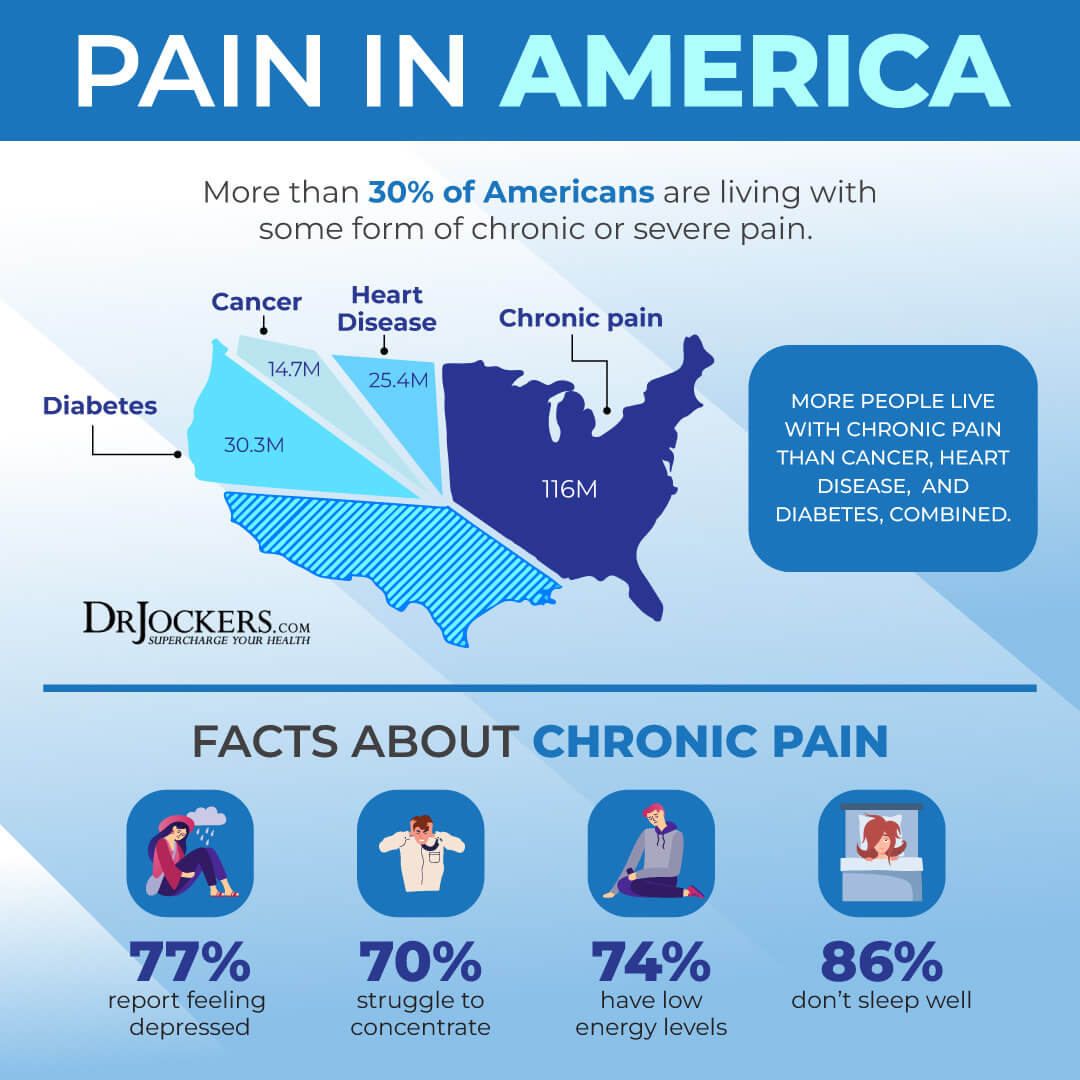
Millions of people in the United States are living with some form of chronic pain, including low back pain, chronic headaches and migraines, joint pain, digestive pain, fibromyalgia, and autoimmune conditions. Chronic pain can seriously interfere with your daily activities, work, studies, family life, social life, and emotional well-being. It may even lead to disability. Fortunately, by addressing the root causes of your chronic pain and using natural support strategies, you may reduce chronic pain and regain your health.
In this article, you will learn what chronic pain is. I will go over the common symptoms of chronic pain. You will learn about the causes and risk factors for chronic pain. I will explain the diagnosis and conventional treatment options for chronic pain. You will learn about the root causes of chronic pain. Finally, I will offer my best natural support strategies for chronic pain to improve your health and well-being.
What is Chronic Pain
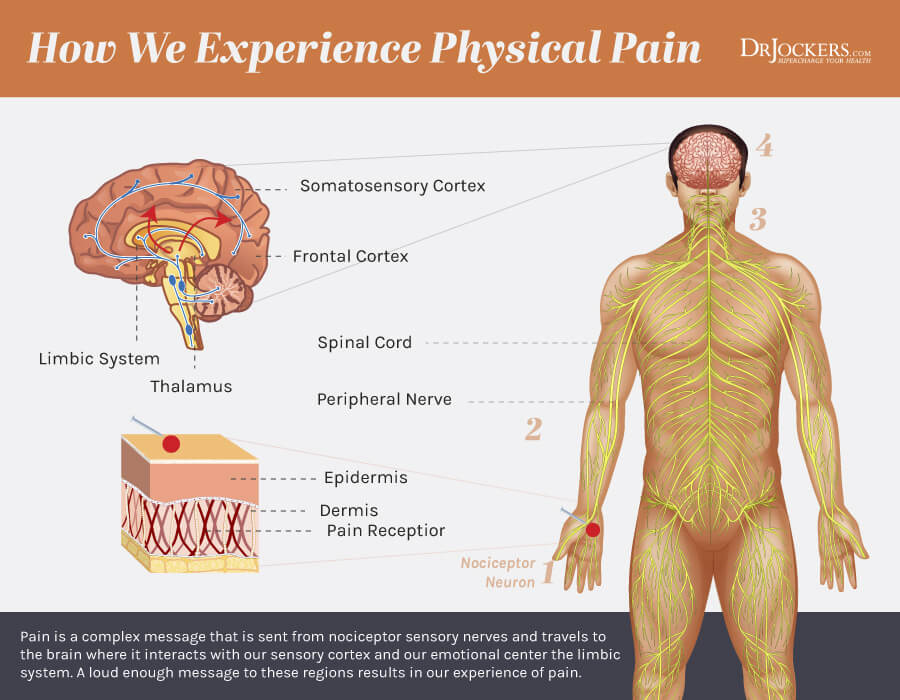
Pain signals that there is something off with your body. It causes an uncomfortable or unpleasant feeling to signal that something is off and needs care. Pain is essentially a protective mechanism. Without pain, you would be walking around with a broken foot without letting it rest and heal.
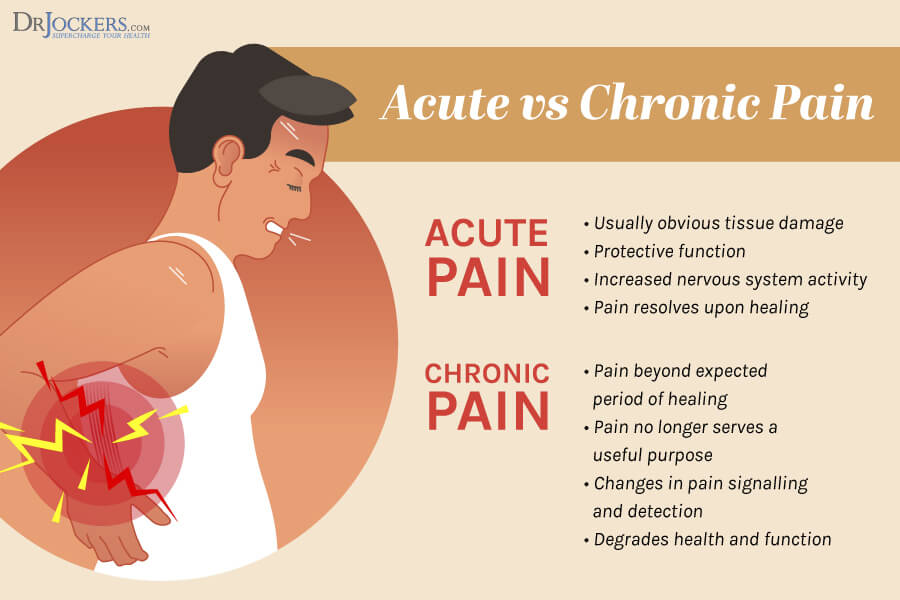
There are two types of pain: acute and chronic. Acute pain comes suddenly and it’s caused by something very specific. Acute pain may happen because of an injury, accident, surgery, dental work, burn, cut, infection, labor and childbirth, and other specific events. Acute pain may last for a couple of hours, a day, a few days, a few weeks, or in some serious cases, a few months. Acute pain gradually gets better over time and eventually goes away completely.
Chronic pain is pain that lasts longer than six months. It is ongoing that is either present daily or comes back over and over again in flares. It may start with a specific event, such as an injury or illness, as acute pain but it just stays around without completely going away. It may happen without a specific trigger or known reason. In both cases, your body’s pain signals stay active for months or years (1, 2, 3, 4).
Chronic Pain Symptoms
Symptoms of chronic pain can be anywhere from mild to severe. They may change throughout the day, week, or month. They may be debilitating and lead to disability in many cases.
There are different forms and symptoms of chronic pain, including:
- Headaches and migraines
- Muscles tension and pain
- Joint pain and arthritis
- Back pain
- Pelvic or bladder pain
- Nerve pain
- Fibromyalgia or widespread body pains
- Cancer-related pain
Chronic pain may cause feelings of:
- Soreness
- Stiffness
- Throbbing pain
- Shooting pain
- Burning sensation
- Stinging sensation
- Dull ache
- Mixed types of pain
Chronic pain may cause tense muscles, low energy, changes in appetite, limited ability to move your body, fatigue, and poor sleep. It may greatly affect your emotional well-being by contributing to anger, mood changes, anxiety, fear of reinjury or certain activities, and depression.
Chronic Pain Causes and Risk Factors
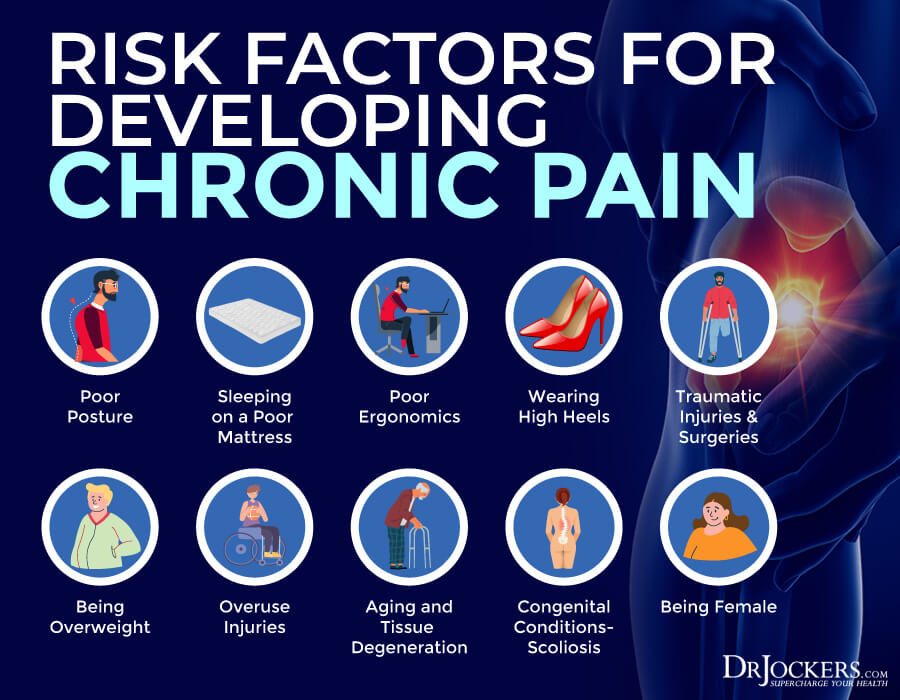
Chronic pain may develop for a variety of reasons. It is often unclear or complex. The following factors may cause or increase your risk of developing chronic pain:
- Poor posture
- Sleeping on a poor mattress
- Lifting or carrying heavy objects without poor posture
- Wearing high heels
- Traumatic injury
- Being overweight or obese
- Overuse injuries and unattended injuries
- Congenital conditions, such as scoliosis
- Aging and degenerative changes of the spine
- Being female
- Injuries or surgeries
- No obvious physical cause
There are various health issues that may cause or increase the risk of chronic pain, including:
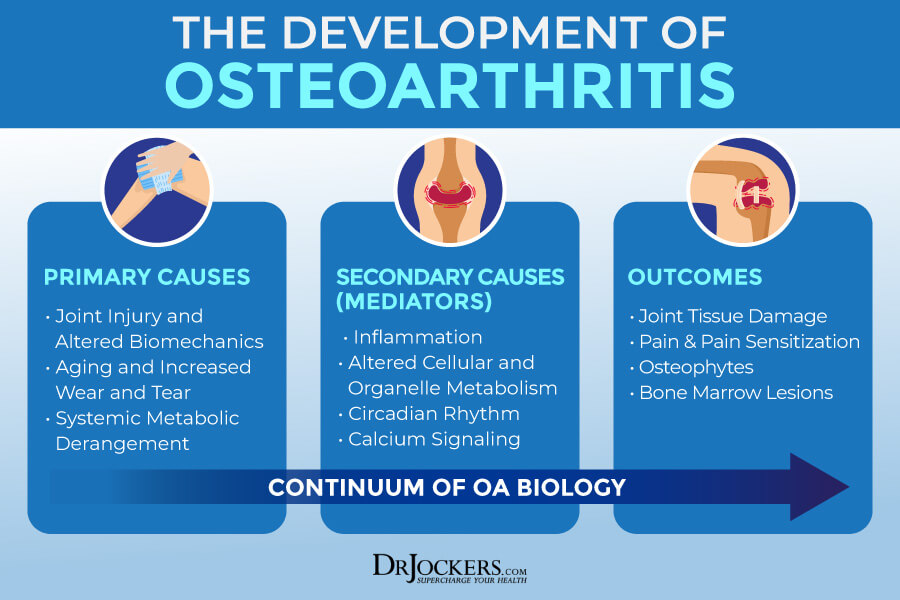
- Osteoarthritis
- Rheumatoid arthritis
- Fibromyalgia
- Chronic fatigue syndrome
- Interstitial cystitis
- Endometriosis
- Vulvodynia
- Tempomomadiualar joint dysfunction (TMJ)
- Multiple sclerosis
- Stomach ulcers
- Gallbladder disease
- Irritable bowel syndrome (IBS)
- Irritable bowel diseases (IBDs)
- Other autoimmune and chronic diseases
- Cancer
- AIDS
 Diagnosis and Conventional Treatment
Diagnosis and Conventional Treatment
To diagnose chronic pain, your healthcare provider will go over your health history and symptoms. They will check where your pain is, when did it start, how intense it is, how does it feel how often do your experience it, what makes it better or worse, and how are your stress levels.
They will check if you have any ongoing health issues or had any recent illnesses or surgeries. After a physical exam, they will order some tests to look into the potential cause of your chronic pain. Tests may include blood tests, urine tests, stool tests, electromyography, x-rays, MRI, CT scan, reflex and balance test, nerve conduction, and spinal fluid tests.
Conventional treatment methods may depend on the type of chronic pain you are experiencing. The goal of the treatment is always to reduce pain and reduce or eliminate discomfort during your daily activities. If you are dealing with muscle or joint pain, improving mobility, flexibility, and strength may also be part of your treatment plan.
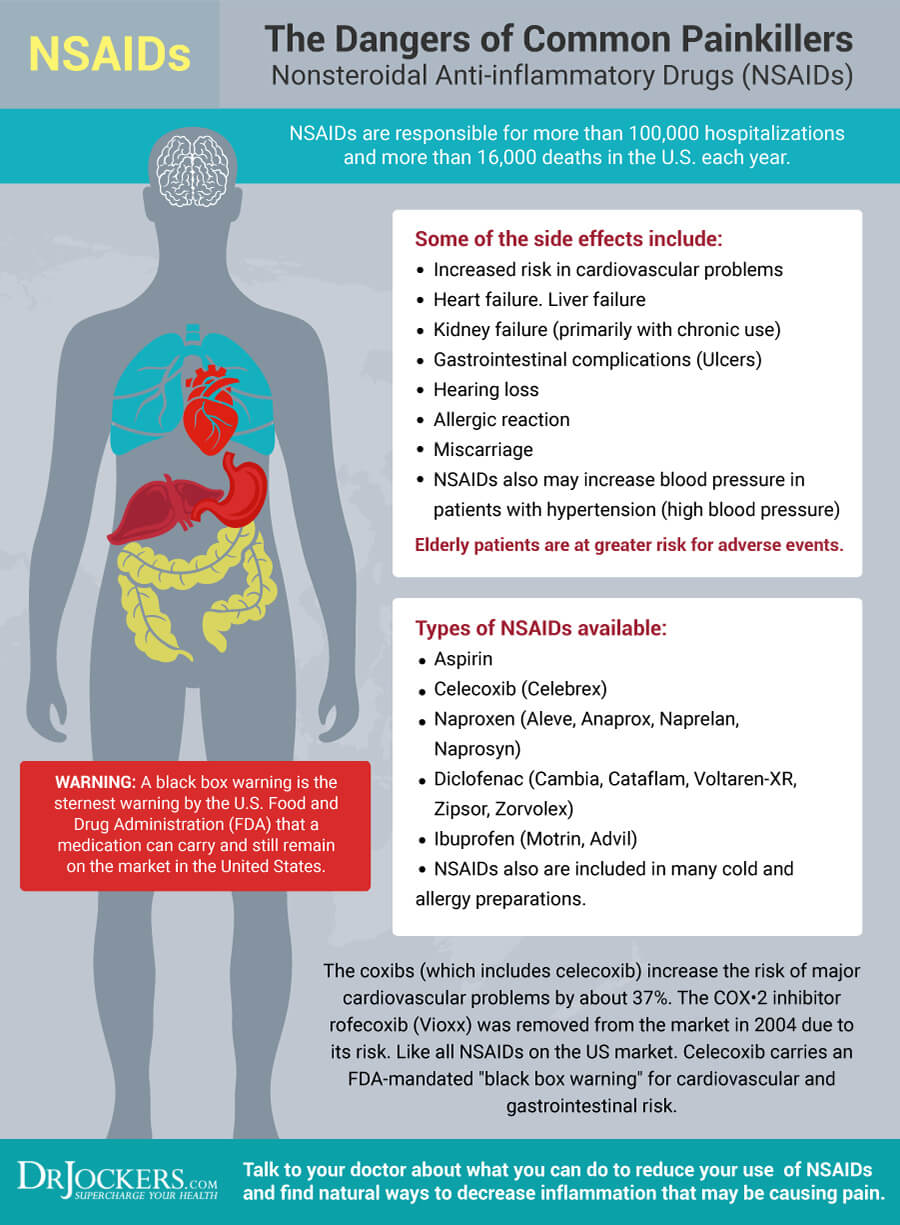
Your doctor may prescribe various medications including over-the-counter (OCT) or prescription pain-relievers, such as acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, opioid pain relievers, such as codeine, morphine, and hydrocodone, adjuvant analgesics, such as anticonvulsants and anti-depressants, corticosteroids, muscle relaxants, sedatives for anxiety or sleep, topical pain relievers, and depending on where you live, medical marijuana. Beyond medication, there are a variety of options your doctor may recommend.
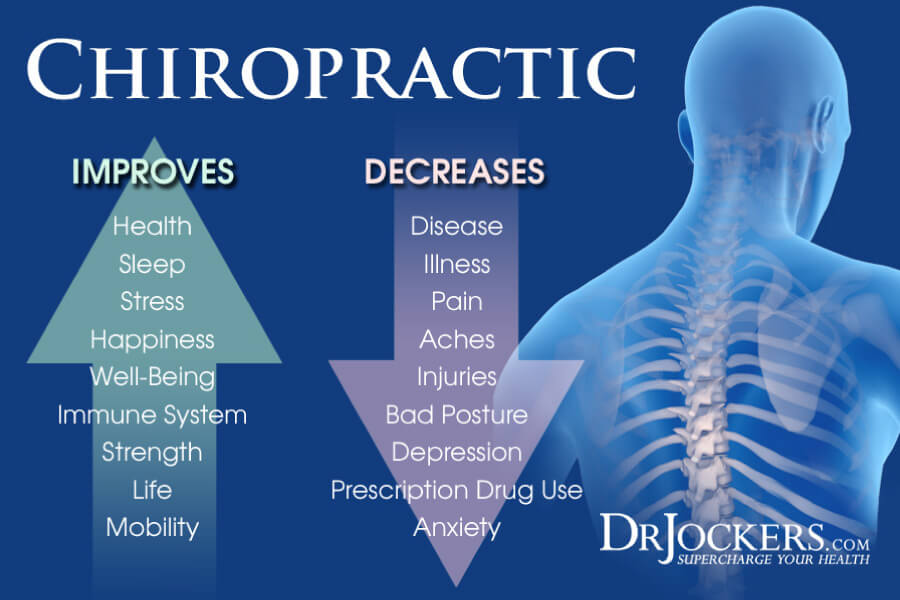
Electrical stimulation may help to lower pain with the help of mild electric shocks to your muscle. Nerve block injections may help to block nerves from sending pain signals. Epidural steroid injections may reduce pain. Surgery may be necessary to correct old injuries and structural issues. Physical therapy can help to strengthen your muscles and help you regain mobility. Some traditional healthcare providers also recommend medical massage therapy, acupuncture, chiropractic care to relieve pain.
Mental health therapy, counseling, art therapy, or music therapy may be recommended to cope with the emotional consequences or emotional causes of chronic pain. Your doctor may recommend some lifestyle strategies, including losing weight, not smoking, stretching, exercise, yoga, tai chi, and meditation (3, 4, 5, 6).
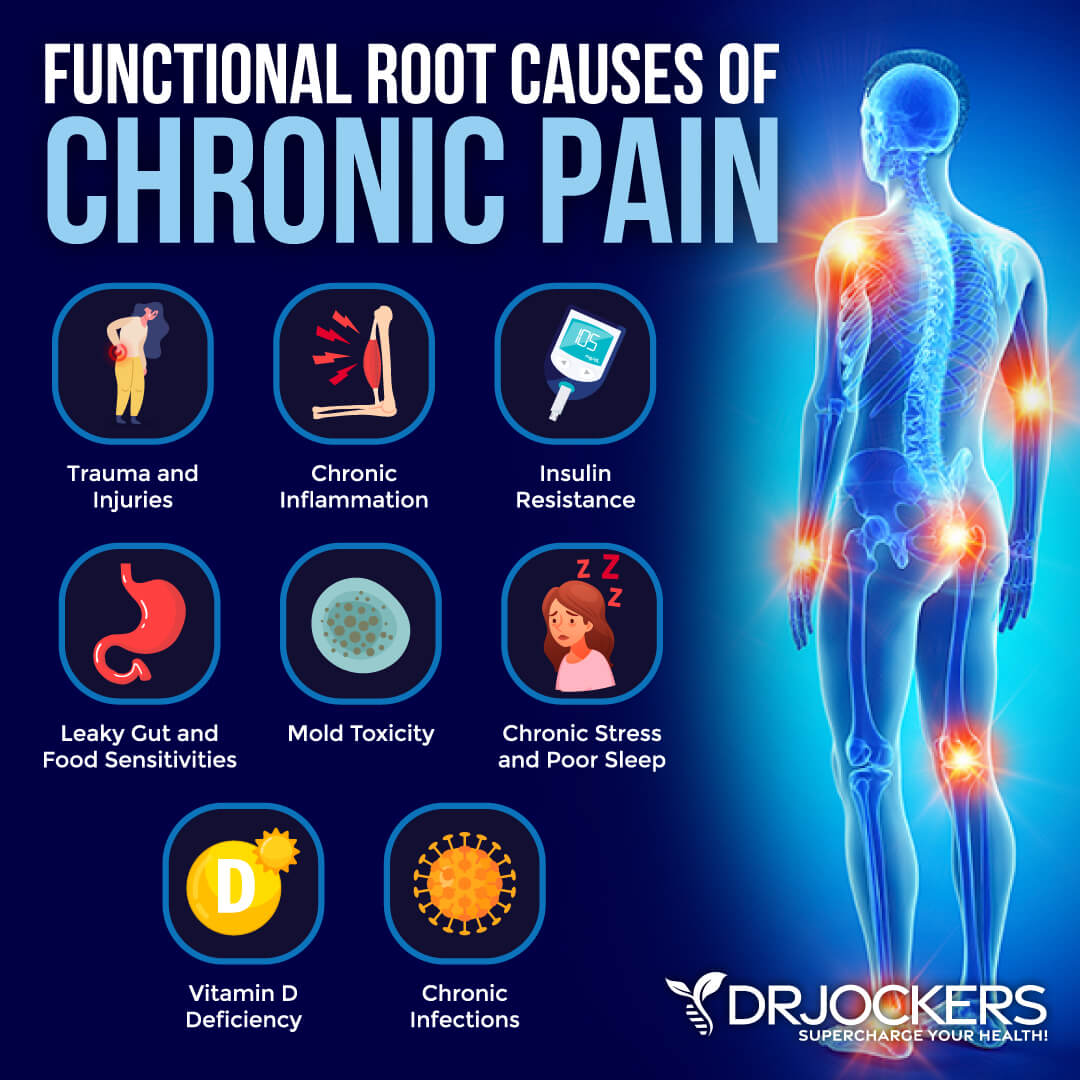
Chronic Pain Root Cause Factors
To improve chronic pain, first, you have to understand the root cause factors of your pain. These factors may or may not directly cause your pain but can certainly contribute to underlying health issues that can increase your risk of pain.
Trauma and Injuries
Trauma and injuries, including accidents, falls, physical attacks, and sports injuries, the first result in acute pain. However, in many cases, symptoms may drag on and lead to chronic pain. According to a 2015 book, Brain Neurotrauma: Molecular, Neuropsychological, and Rehabilitation Aspects published by CRC Press/Taylor & Francis, neurotrauma due to spinal cord injuries and TBIs may cause chronic neuropathic pain (7).
A 1993 study published in the Archives of Physical Medicine and Rehabilitation has found that chronic pain, chronic headaches, chronic neck and shoulder pain, and chronic back pain are common with TBIs and post-concussion syndrome, even in the case of milder injuries (8).
You don’t need to suffer from a serious injury, traumatic injury, or TBI though to have chronic pain. Sometimes people have a difficult time achieving full recovery after a surgery or an acute small accident. In other cases, ignoring the problem, not taking a rest, not seeking physical therapy, or not making posture or lifestyle changes can cause chronic pain.
As a 1994 study published in the Journal of Orthopedic and Sports Physical Therapy demonstrates, overuse sports injuries are a common cause of chronic pain (9). It may start with a twisted ankle or tight hamstring that could get better within a few days or weeks, but if you continue to push through the pain without strengthening your body and correcting imbalances, you may end up with chronic pain.
Chronic Inflammation
Chronic inflammation is an underlying problem in most chronic health issues. It is not different when it comes to chronic pain. Chronic pain is often a warning sign that you are dealing with chronic inflammation.
According to a 2021 article published by StatPearls, you may develop chronic inflammation, if you miss to eliminate a pathogen causing acute inflammation, have been exposed to low level of environmental toxins, are dealing with an autoimmune issue, your cells are experiencing oxidative stress or mitochondrial dysfunction, your cells have trouble mediating inflammation, or you have recurrent episodes of the same acute pain (10).
Many inflammatory and autoimmune diseases, such as rheumatoid arthritis, IBDs, lupus, and fibromyalgia, are characterized by chronic pain. According to a 2017 review published in the Journal of Neuroscience Research, most autoimmune disorders are characterized by chronic pain which in some cases may be linked to T cell activation and cytokine release (11).
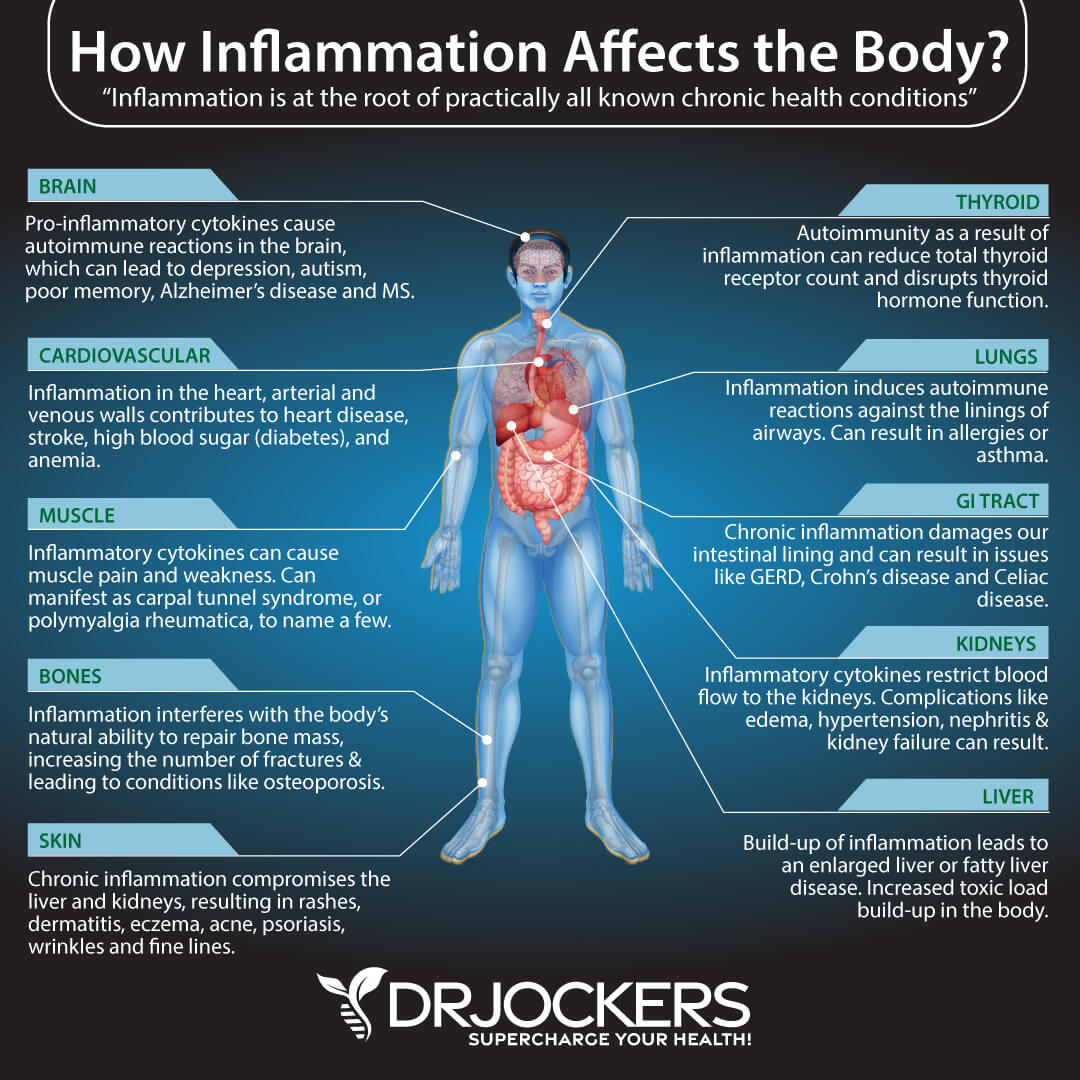
Insulin Resistance
Insulin resistance means that your body is unable to respond to insulin well and convert glucose properly for energy. This will cause your pancreas to overwork and create more insulin. Over time, this can lead to blood sugar issues, prediabetes, and type 2 diabetes. Insulin resistance is one of the main underlying causes of chronic inflammation and related symptoms and health issue. Thus insulin resistance may be linked to chronic pain.
There is increased evidence suggesting that insulin resistance may be one of the culprits behind fibromyalgia. A 2019 report published in PLoS One has found that insulin resistance may be an underlying reason behind fibromyalgia and related chronic pain (12). A 2021 study published in Pain Physician has also found a possible link between insulin resistance and chronic pain (13).
However, fibromyalgia pain is not the only chronic pain that may be linked to insulin resistance. A 2017 review published in Joint Bone Spine has found a possible connection between insulin resistance and rheumatoid arthritis (14). A 2015 study published in Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy have linked insulin resistance to pelvic pain (15).

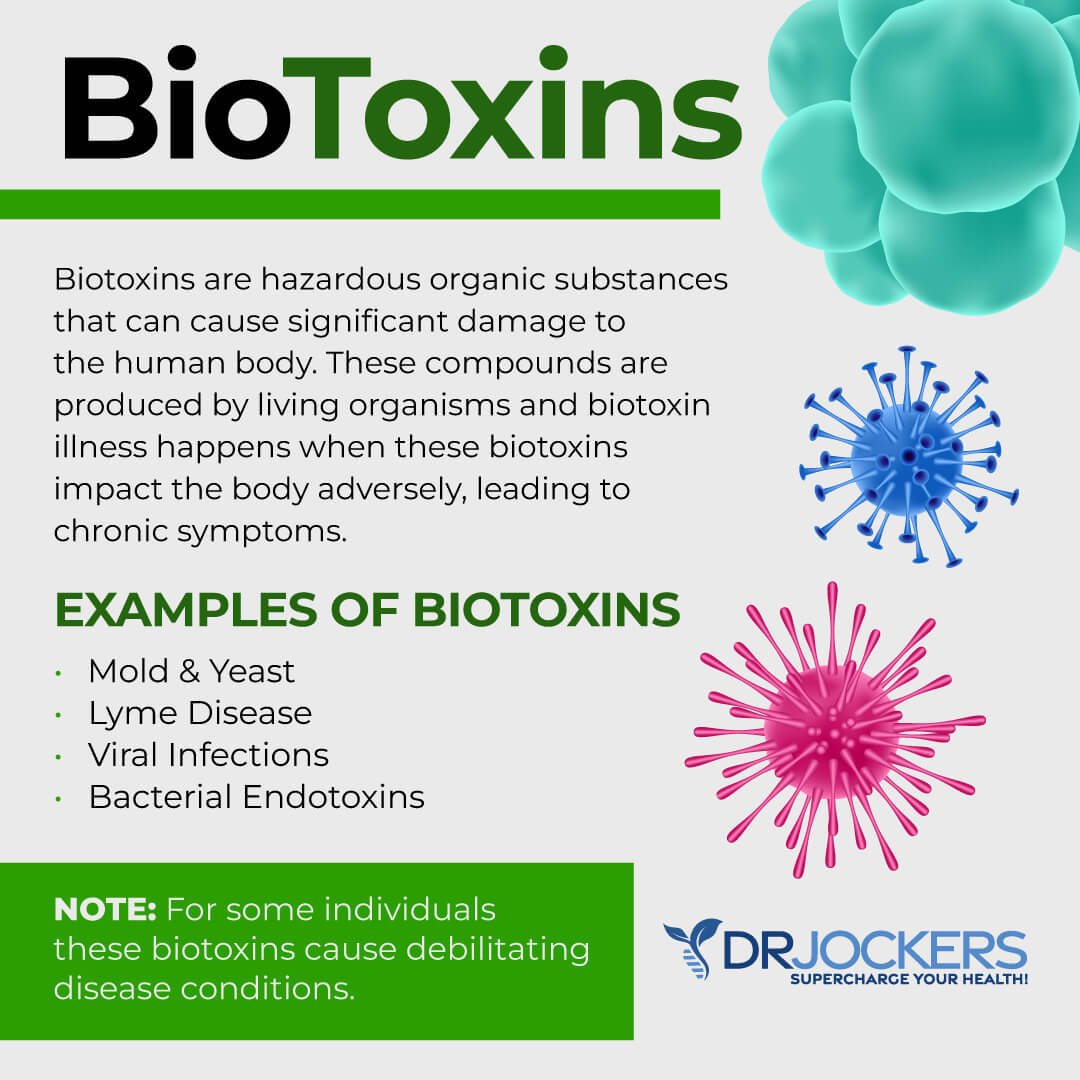
Chronic Infections
According to a 2021 article published by StatPearls, chronic infections may lead to chronic inflammation, which may result in chronic pain as well (10). These chronic infections may include viral, bacterial, fungal, and parasitic infections.
The Epstein-Barr Virus (EBV) is a common culprit behind chronic pain. According to a 2021 study published in Frontiers in Immunology, EBV infections may cause chronic fatigue syndrome, which is often characterized by chronic pain (16). A 2021 study published in The Spine Journal has found that chronic bacterial infections may lead to chronic back pain (17).
A 2017 study published in Frontiers in Medicine has found that chronic musculoskeletal pain, sleep disturbance, fatigue, and depression are common in Lyme disease patients (18). A 2020 review published in Pain has discussed how chronic pain cases may increase as a result of the pandemic as long hauler syndrome is increasingly prevalent (19).
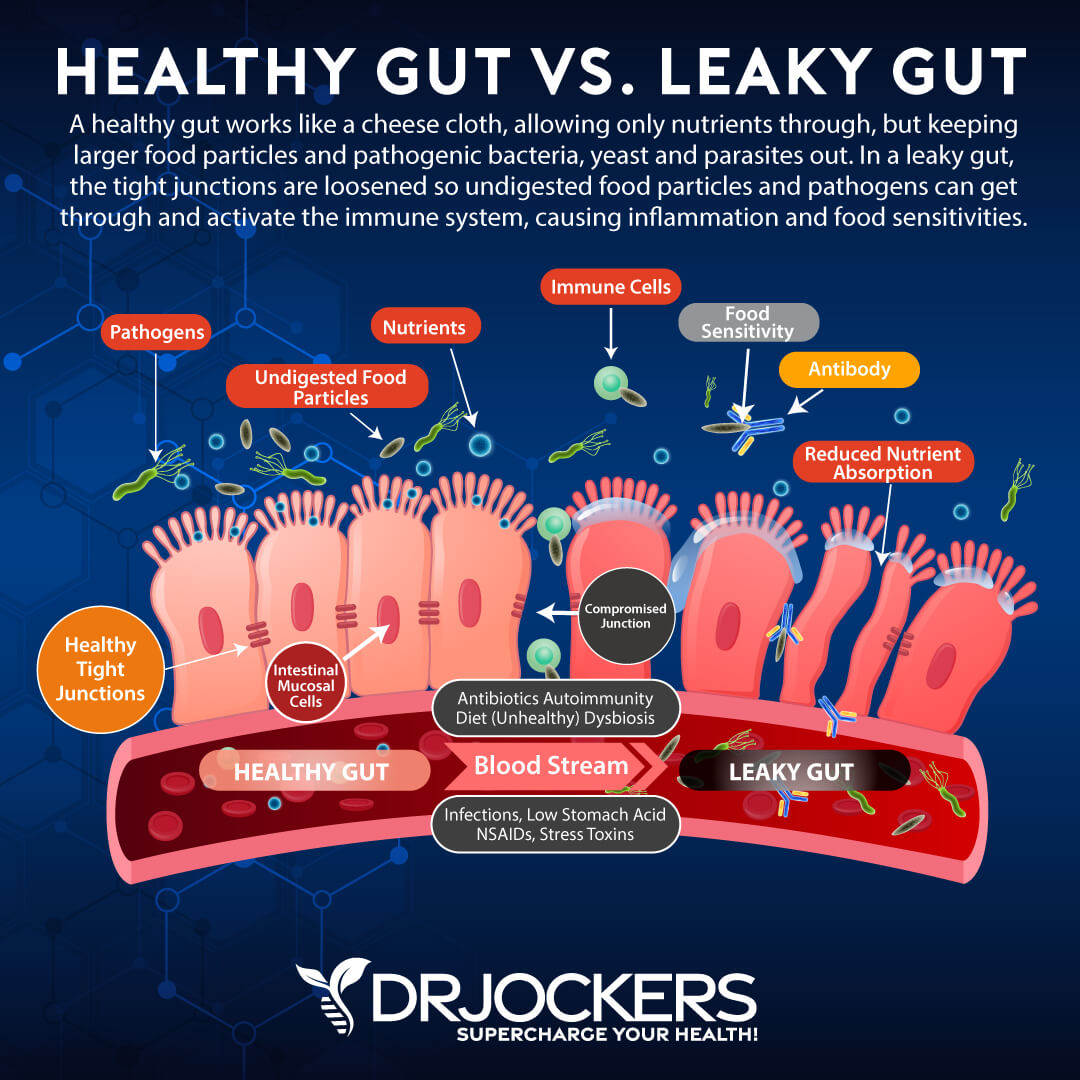
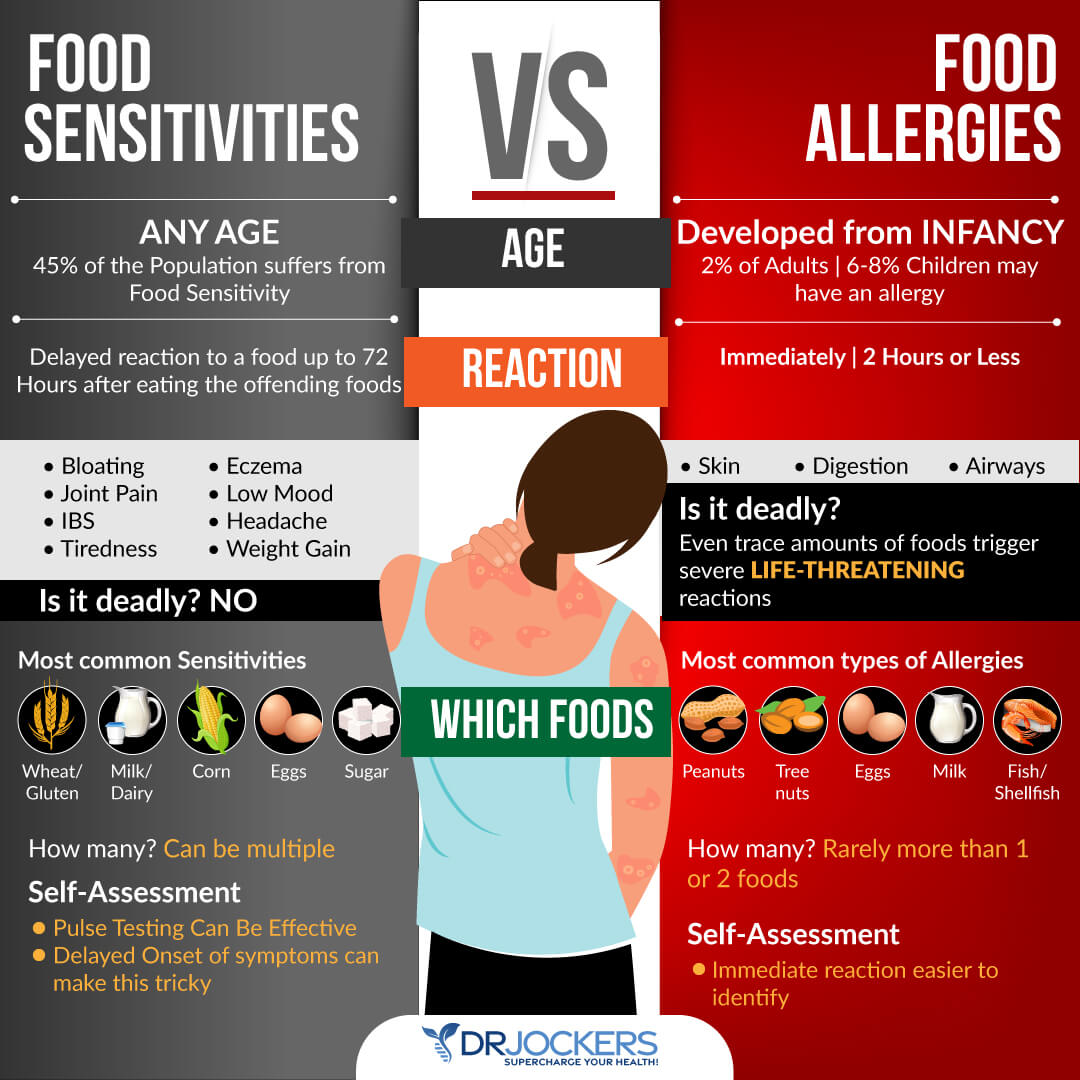
Leaky Gut and Food Sensitivities
Your gut is connected to your entire body. If your gut microbiome balance and gut health is off, it can increase chronic inflammation in your body and lead to various health issues, including chronic pain. Leaky gut syndrome means that your gut lining has developed larger holes that can allow toxins, pathogens, and larger food particles to pass into your bloodstream along with nutrients.
This can cause gut microbiome imbalance, chronic inflammation, autoimmunity, and chronic symptoms. Food sensitivities may also increase chronic inflammation, gut microbiome imbalance, chronic pain, and other chronic symptoms.
A 2017 study published in Frontiers in Immunology and a 2020 review published in the International Journal of Molecular Sciences have linked leaky gut syndrome to autoimmune diseases (20, 21). As you know, many autoimmune conditions, including rheumatoid arthritis, IBDs, lupus, MS, and autoimmune thyroid dysfunction, can cause chronic pain along with other chronic symptoms.
A 2020 systematic review published in BMC Musculoskeletal Disorders has found that gut microbiome imbalance and poor gut health biomarkers may increase the risk of fibromyalgia (22). A 2015 review published in Mediators of Inflammation has found a link between leaky gut and IBDs (23). A 2020 study published in Nutrients has found that addressing dietary patterns, including food allergies and sensitivities may help to address chronic pain (24).
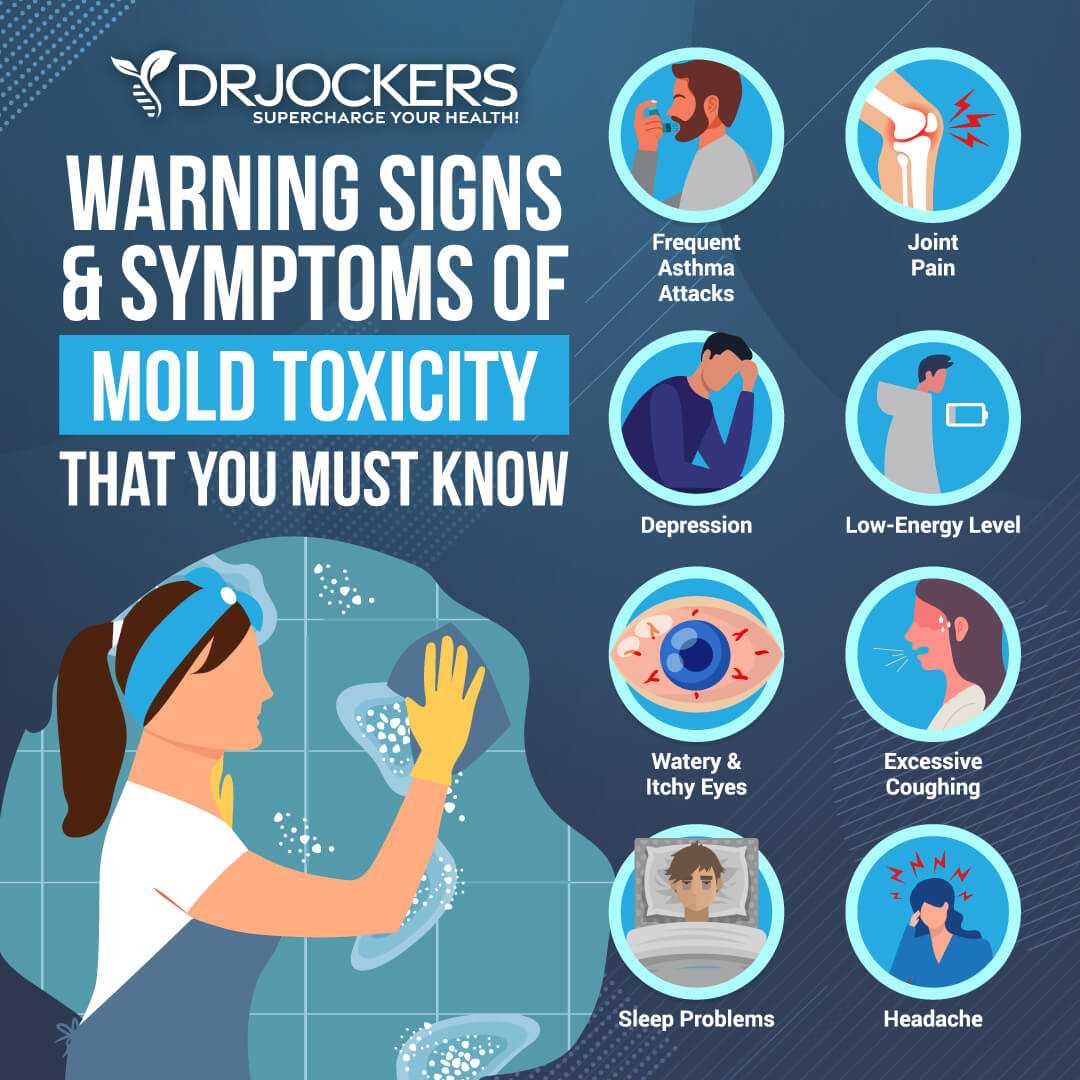
Mold Toxicity
Mold is a fungus that can grow on almost anything. It can thrive in many conditions but most specifically in warm temperatures and high moisture environments both indoors and outdoors. Mold loves to hide in your bathroom, kitchen, basement, behind wallpaper, behind drywall, and under your carpet. It can become a serious issue if you have a moisture leak or flooding or live or work in an unkempt or old building.
Chronic mold exposure can lead to mold toxicity, chronic inflammation, chronic pain, and other chronic symptoms. A 2013 study published in Toxins (Basel) has found that mold mycotoxins are commonly found in those with chronic fatigue syndrome and may be responsible for their symptoms (25). A 2014 study published in Toxins (Basel) has found that mold mycotoxins can lead to chronic illness (26).
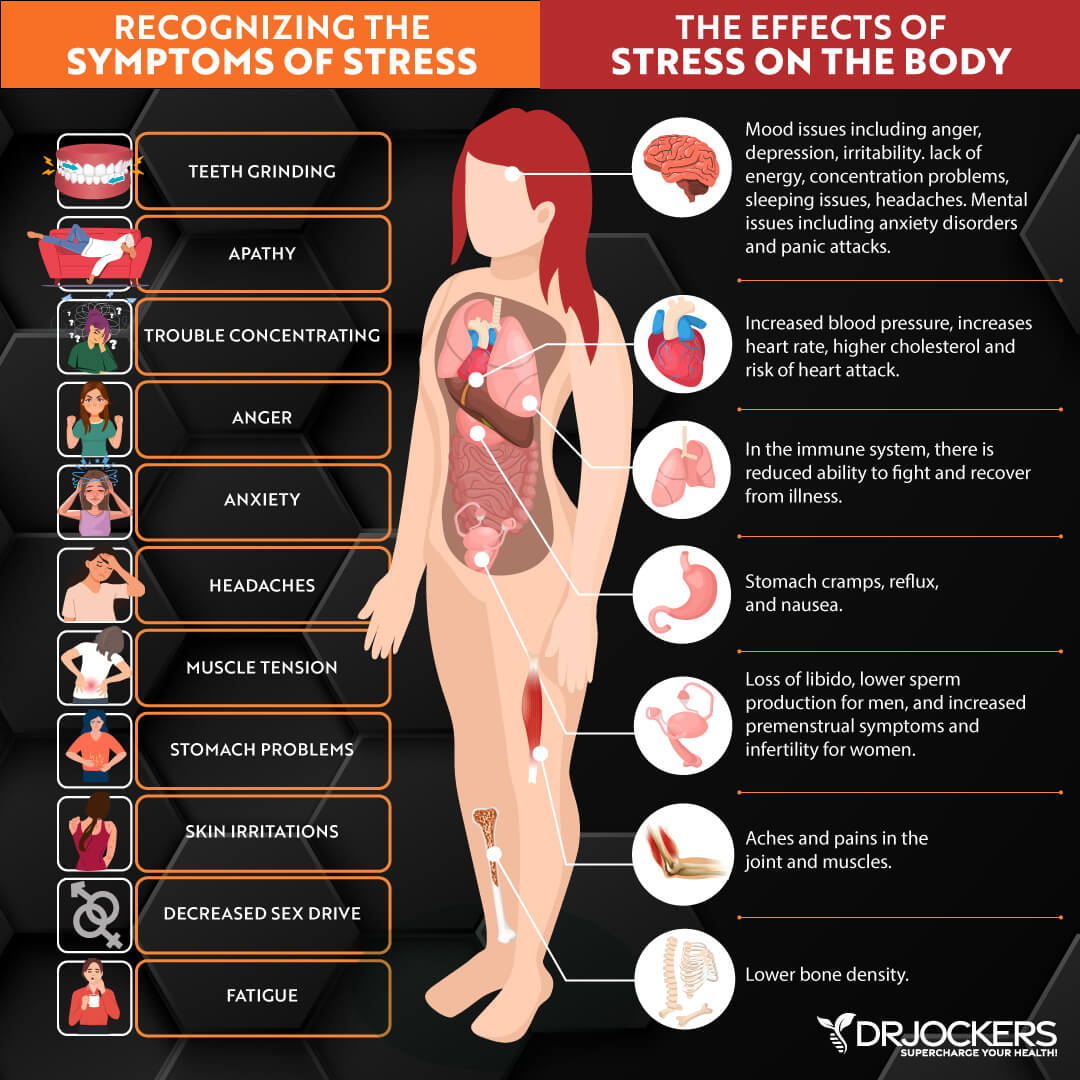
Chronic Stress & Poor Sleep
Chronic stress and poor sleep can increase chronic inflammation in your body. This can lead to chronic pain and other chronic symptoms. According to a 2017 review published in Chronic Stress (Thousand Oaks), chronic stress and chronic pain may just be two sides of the same coin (27).
They found that the limbic brain, including the hippocampus, amygdala, and ventromedial prefrontal cortex, play a role in chronic pain, chronic stress, posttraumatic stress, and depression. A 2015 review published in the Malaysian Journal of Medical Sciences has found that chronic pain may increase during times of stress (28).
A 2011 study published in the Journal of Clinical Psychology has found that addressing emotions and emotional stress is critical when it comes to chronic pain (29). A 2016 review published in The Journal of Pain has found that psychosocial factors, such as stress, anxiety, and depression, may play a role in chronic pain (30).
A 2013 study published in The Journal of Pain has found that disrupted sleep may increase chronic pain (31). A 2008 review published in Reviews in Pain has found that insomnia and chronic pain often co-occur (32). A 2019 study published in PLoS One has found that sleep deprivation may increase pain sensitivity (33). A 2021 study published in Science Reports has found that chronic poor sleep can increase chronic back pain and related disability (34).
Moreover, chronic pain can increase chronic stress and interfere with your sleep. Poor sleep may also increase chronic stress and chronic pain. Chronic stress can disrupt your sleep, increase chronic pain, and make it more difficult to deal with chronic pain emotionally. As you see, chronic stress, poor sleep, and chronic pain can turn into a vicious cycle unless you address all parts of the triangle.
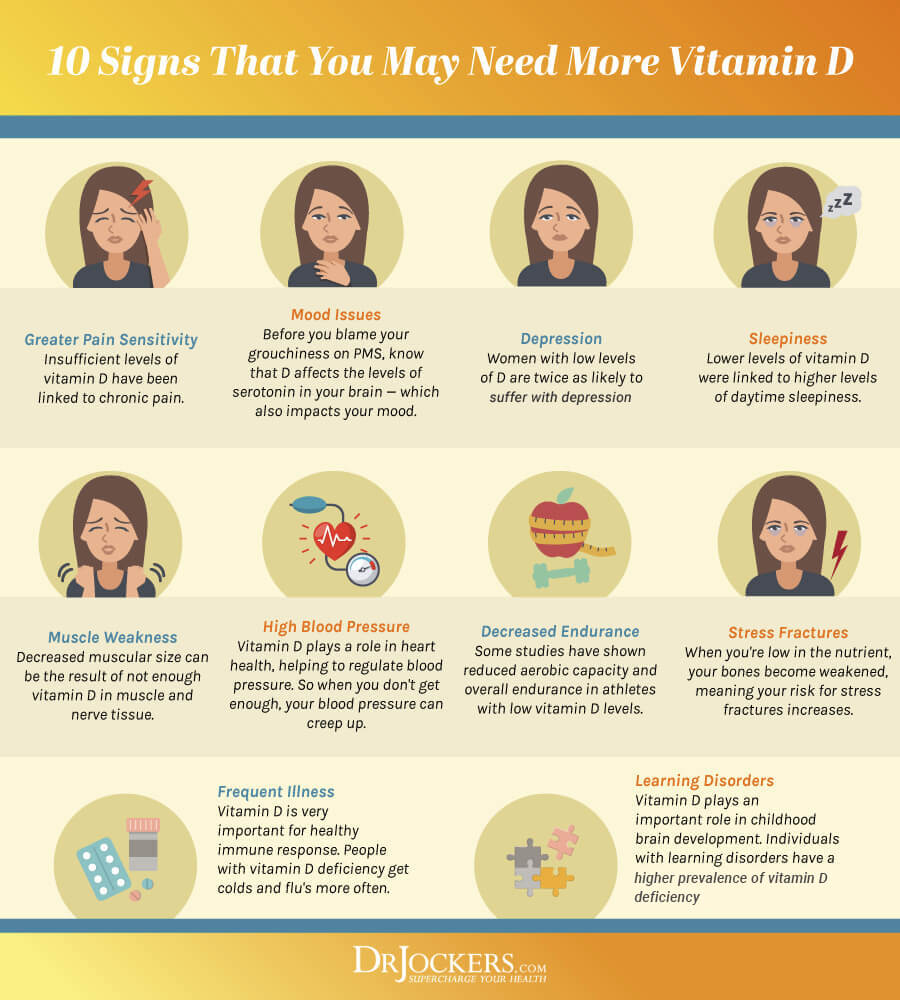
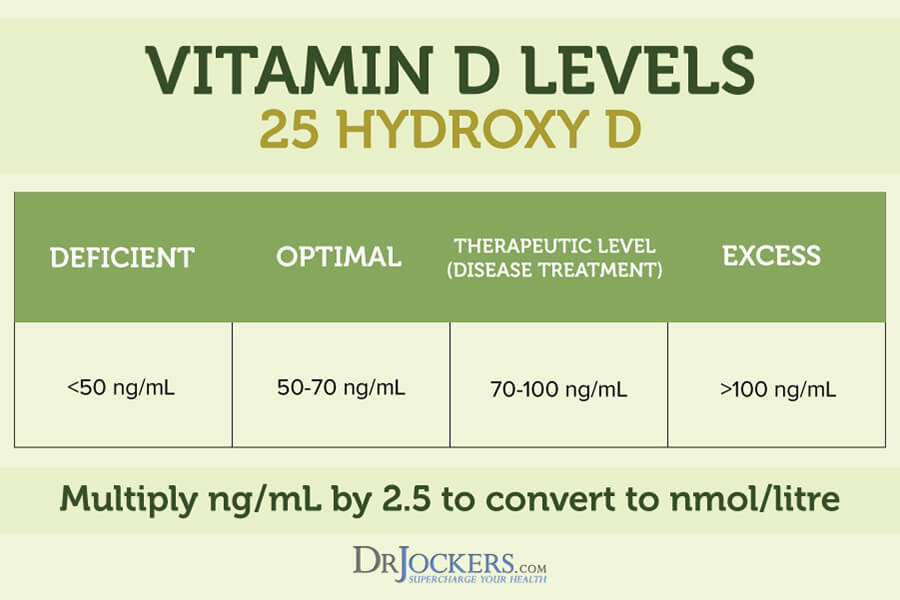
Vitamin D Deficiency
Vitamin D is an essential vitamin that your body makes when the rays of the sun penetrate your skin. You can also get vitamin D through some foods and supplementation.
Vitamin D is essential for your body, including for bone, muscle, immune, brain, and mental health. Due to our indoor lifestyle and lack of supplementation, vitamin D deficiency is very common unfortunately and it can lead to chronic pain and chronic health issues.
A 2013 case report series published in Palliative Medicine has found that vitamin D deficiency may increase the risk of chronic pain (35). A 2018 systematic review and meta-analysis published in Public Health Nutrition has also found a link between low vitamin D levels and chronic pain (36).
Chronic Pain Testing Strategies
To check if you are dealing with chronic inflammation and identify related root causes of your symptoms and health problems, I recommend a number of testing strategies.
GI MAP
My favorite test to look at your gut health and identify gut inflammation, bacterial pathogens, parasitic pathogens, viral pathogens, normal flora, dysbiotic flora, potential autoimmune triggers, and all intestinal health markers is the GI Map Stool Analysis. This test looks for gut function markers, such as calprotectin, zonulin, and sIgA.
Calprotectin can detect gut inflammation and markers associated with gut infections, irritable bowel syndrome, and inflammatory bowel diseases. Zonulin is used as a biomarker for an impaired gut barrier, leaky gut syndrome, autoimmune diseases, cancer, and neurodegeneration.
Secretory IgA (sIgA) looks at markers of mucosal immunity, immunological reactions to pathogenic infections, and signs of gut inflammation. This is the best and most comprehensive gut test I have found and it helps me tremendously to identify the root cause of my patients’ health issues and help them to repair their body and regain their health naturally.
Food Sensitivities
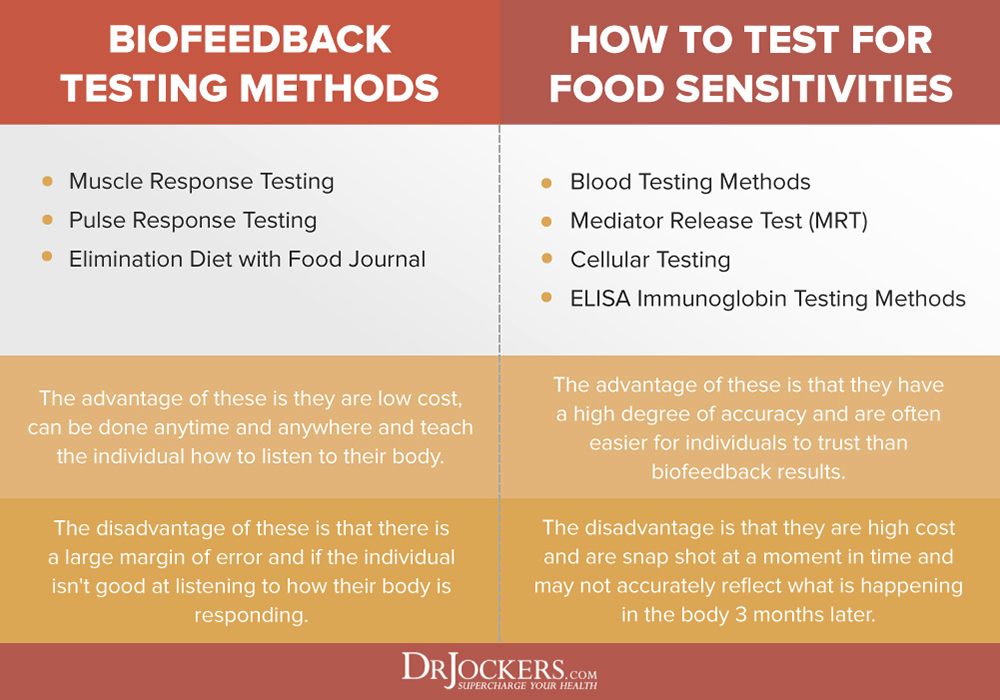
I also recommend food sensitivity testing. There are many blood tests for food sensitivities are on the market. The best one I could find and often recommend to my patients is the Advanced Food and Chemical Sensitivities test. However, it’s impossible to test for every single food through a blood test.
I also recommend that you try a Pulse Test or Muscle Response Testing. These two biofeedback testing should help you to identify your food sensitivities and get to know your body better. Additionally, I also recommend an elimination diet to spot your food sensitivities for certain. Since food sensitivities can change over time, I recommend repeating testing once a year or if new symptoms arise.
Blood Markers for Inflammation
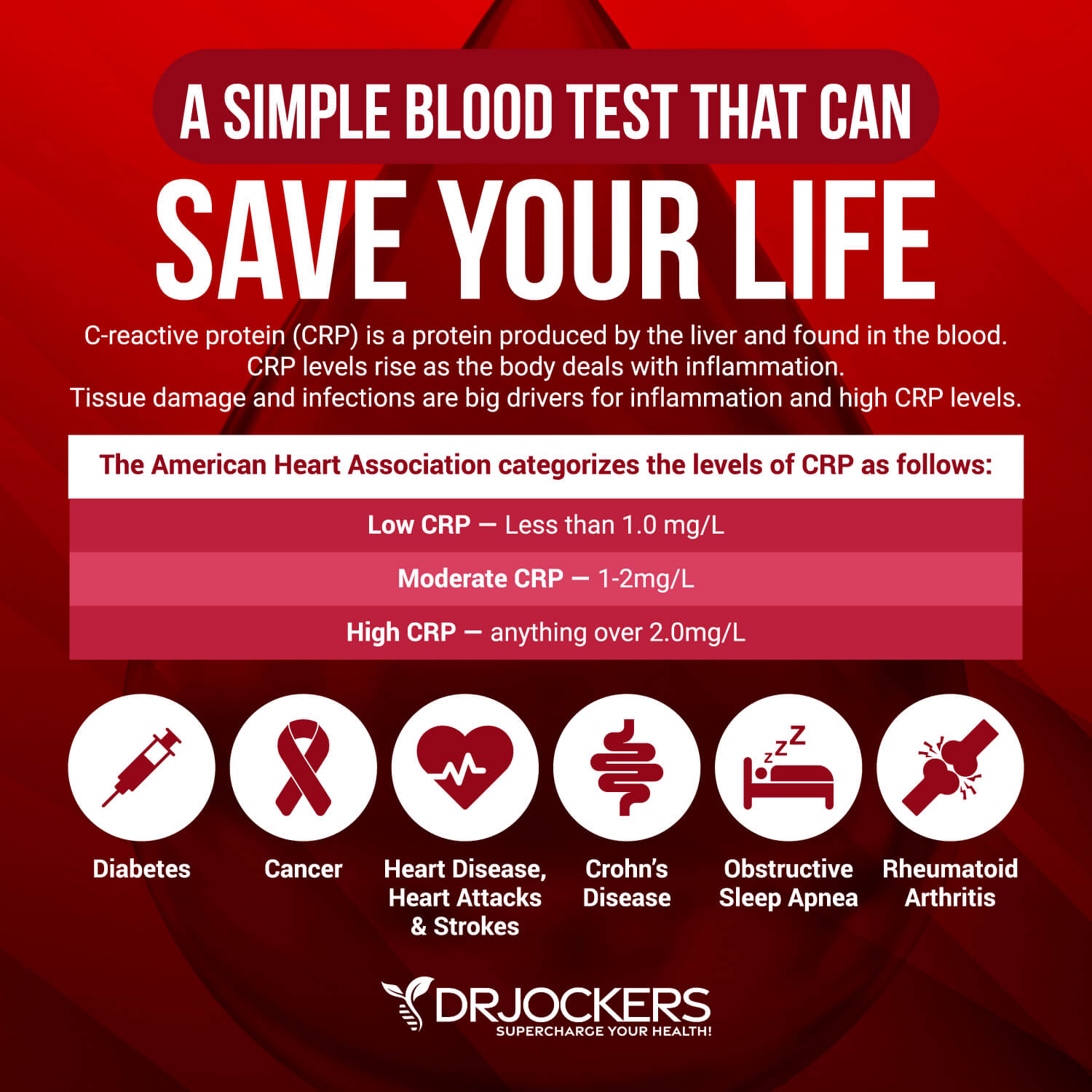
I recommend a number of blood markers for inflammation, including. hs-CRP, ESR, serum ferritin, and liver enzymes.
Hs-CRP
The C-Reactive Protein or CRP test is a key test I recommend. It measures a protein (CRP) produced in your liver that indicates inflammation levels in your body. The clinical range is between 0 and 3 mg/L while the optimal range is 0 to 1 mg/L.
When I see levels over 1 mg/L, I know the individual is having an inflammatory response that could be due to acute trauma or chronic conditions.
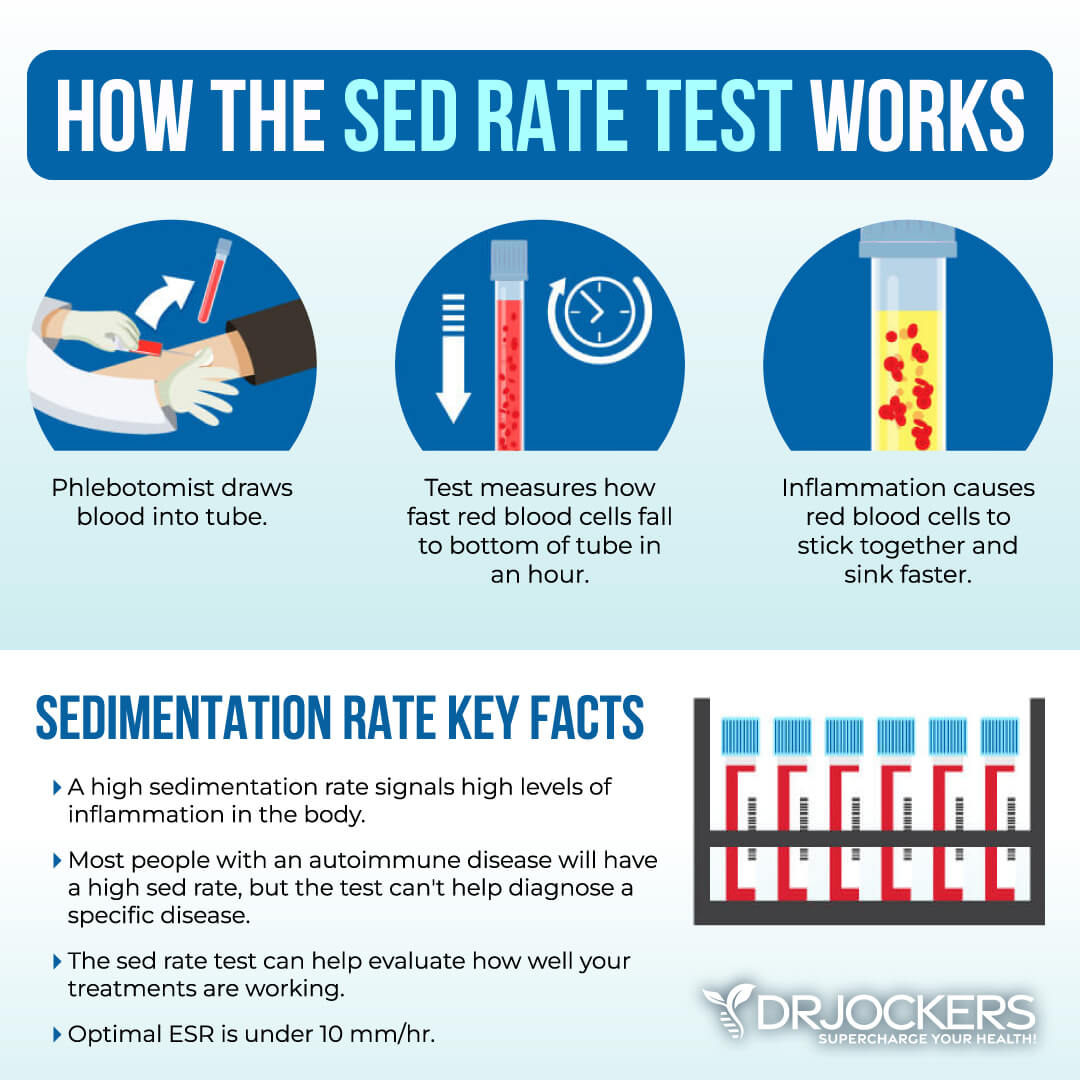
ESR and Platelet Levels
The erythrocyte sedimentation rate (ESR) is a common hematology test to look for inflammation. It refers to the rate at which your red blood cells in anticoagulated whole blood go down in a standardized tube over a period of one hour. Anything over 20 mm/hr is a sign of significant inflammation and optimal results should be under 10 mm/hr.
You can also look at platelets as a measurement tool of inflammation and the stickiness of blood. Platelets elevated above 250 is a sign of inflammation. The sweet spot for platelets is between 175 and 250. Below 175, immune function and blood clotting are compromised; the same is true for levels above 250.
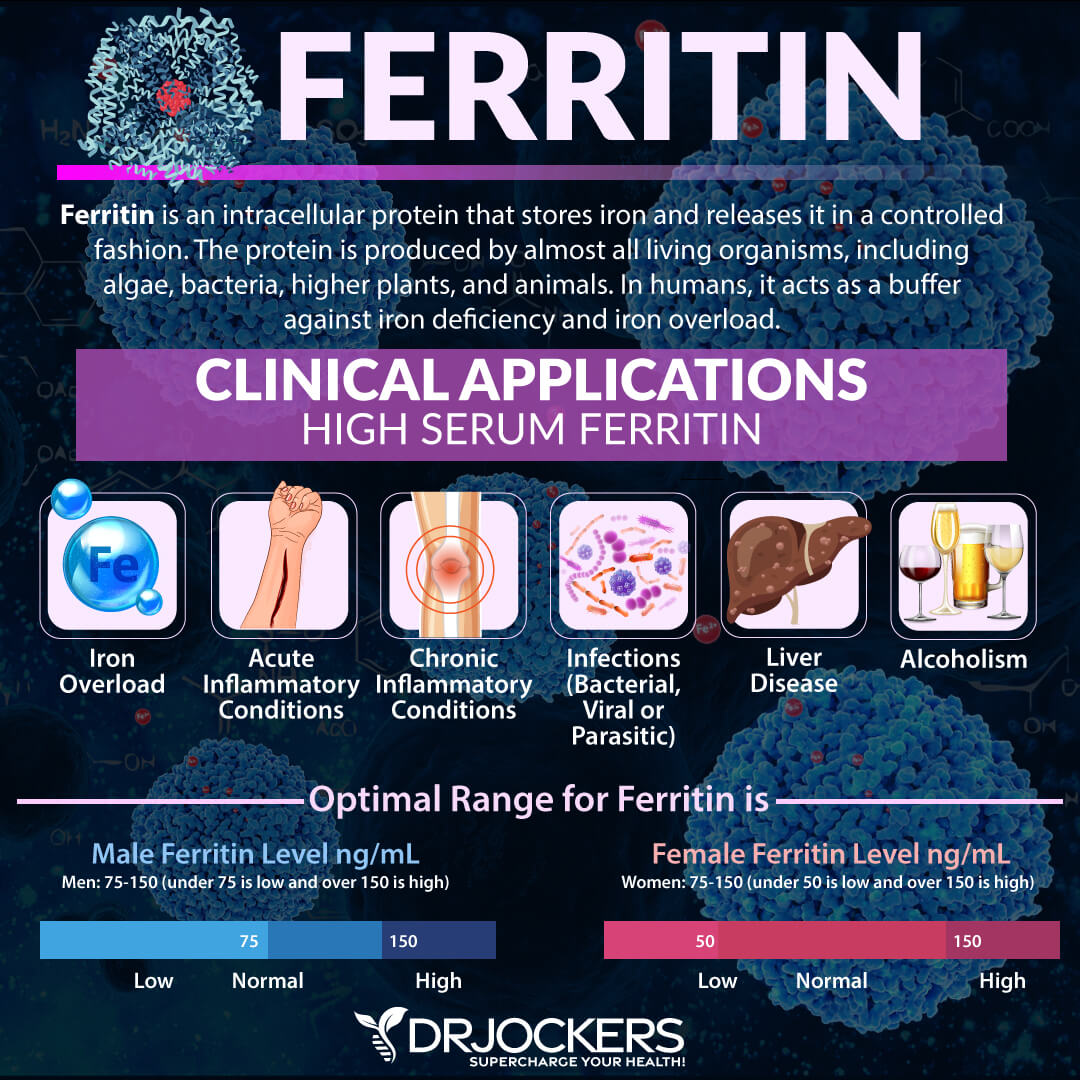
Serum Ferritin
Serum ferritin measures the level of ferritin in your body to detect iron deficiency anemia and other health issues. Elevated serum ferritin levels may indicate inflammation, liver disease, autoimmune disease, or even cancer.
The clinical range is 30 to 400 and the optimal range is 50 to 150 for females and 75 to 150 for males. Anything over 150 may be an indication of infection or oxidative stress based inflammation.
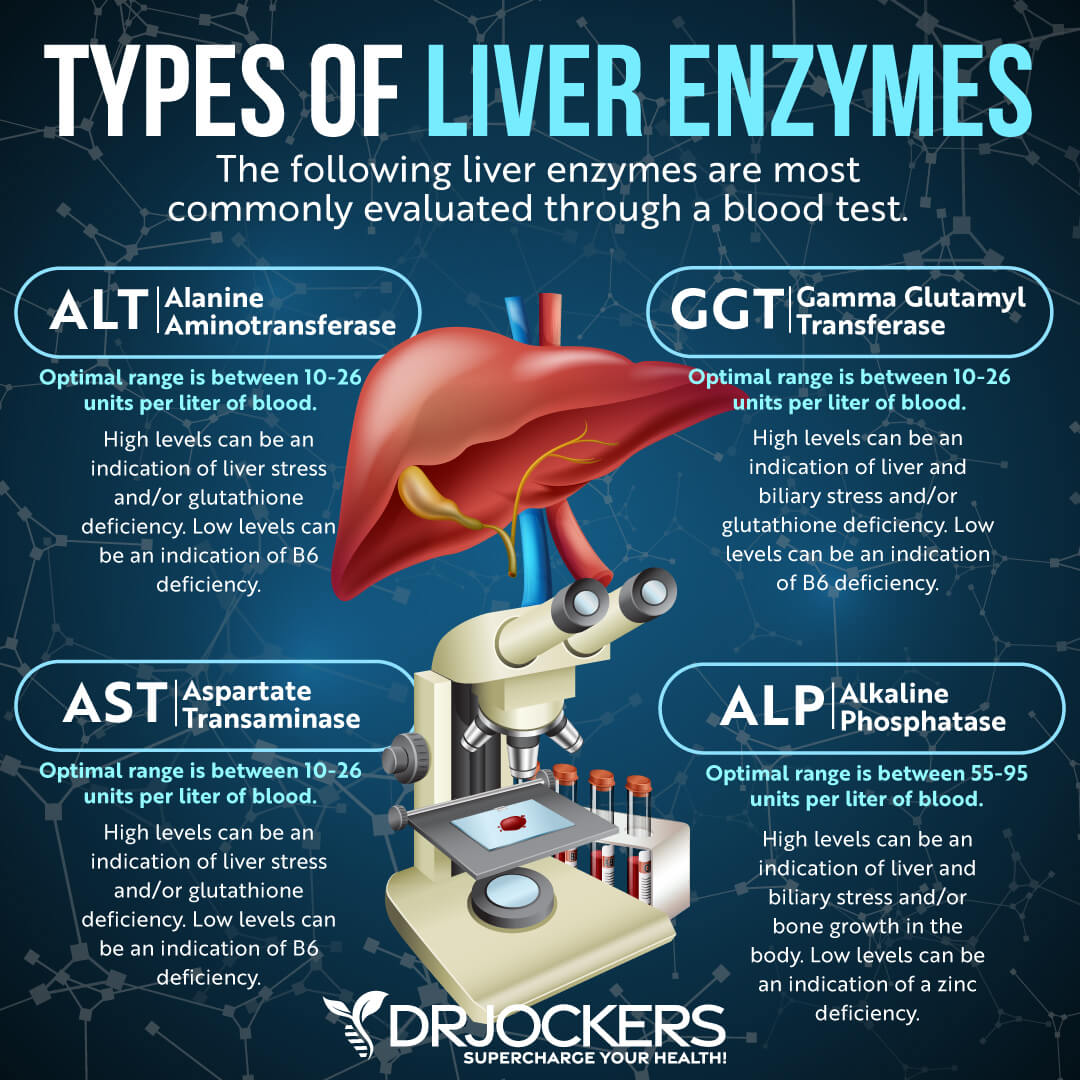
Liver Enzymes
Liver enzyme levels may also indicate inflammation, as well as liver, gallbladder, bile, or kidney issues. Alkaline phosphatase is a liver enzyme that is made by the mucosal cells that line the bile system of the liver and helps normal bile flow. Elevated levels (over 95) may indicate inflammation and liver and gallbladder problems.
Alanine aminotransferase (AST) is a liver enzyme. Elevated levels may indicate inflammation. Normal levels are between 10 and 26 IU/L.
Aspartate transaminase (ALT) is an enzyme present in the liver that spills out during times of increased liver stress. Elevated levels may indicate inflammation Normal levels are between 10 and 26 IU/L.
Gamma-Glutamyl Transpeptidase (GGT) is an enzyme in the liver, pancreas, and kidneys. Elevated levels may indicate inflammation and liver disease, usually due to alcoholism and/or sluggish gallbladder or gallstone obstruction. Normal levels are between 10 and 26 IU/L. Levels lower than 10 IU/L can be an indication of a vitamin B6 deficiency.
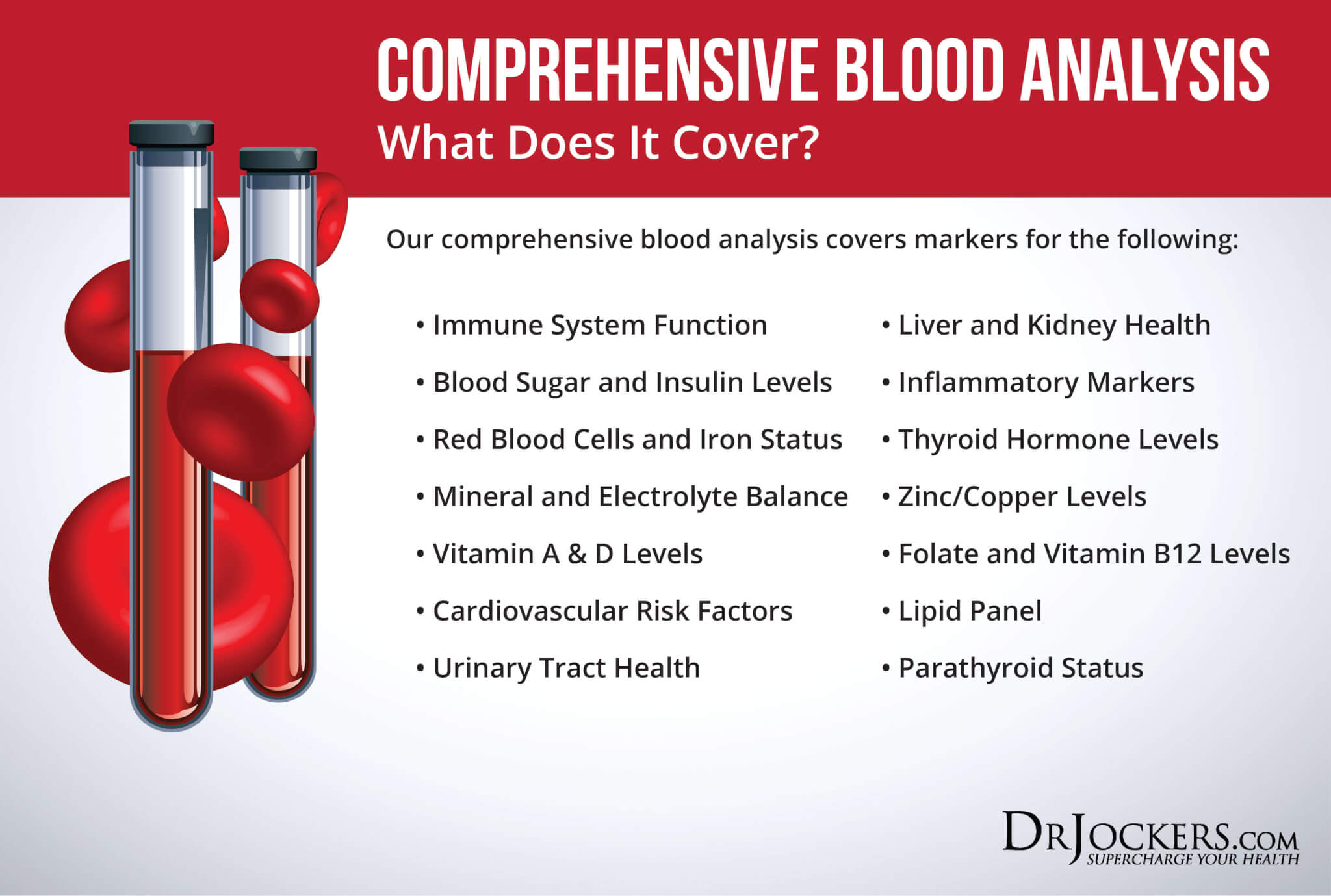
Comprehensive Blood Analysis
To check for these health markers, I recommend a Comprehensive Blood Analysis (CBA). This is the most detailed blood test that looks at all of these markers of inflammation. This test is more sophisticated than most conventional doctors are able to order.
It examines all parameters for inflammation, blood sugar levels, thyroid function, zinc and copper ratio, vitamin A and D levels, a complete metabolic panel, complete blood count, liver function, nutrient deficiencies, and more. I recommend getting the Comprehensive Blood Analysis done regularly both as a preventative measure and to monitor your inflammation levels and progress.
Natural Support Strategies
Now that you understand the potential causes, risks, and root cause factors of chronic pain, it’s time to learn about how to address these issues to improve your chronic pain. Here are the natural support strategies I recommend for chronic pain:
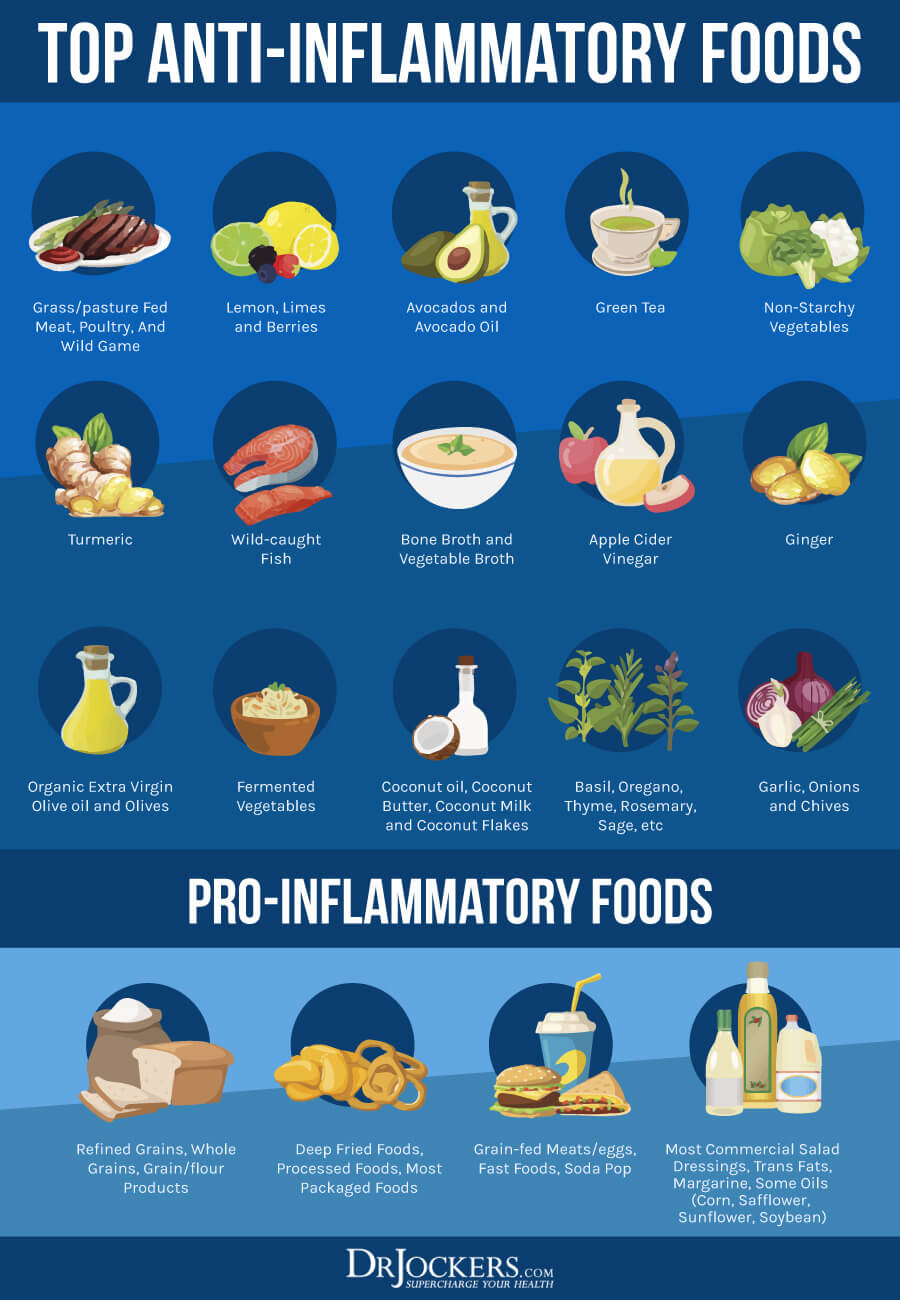
Anti-Inflammatory Nutrition Plan
A 2020 study published in Nutrients has found that addressing dietary patterns, including food allergies and sensitivities may help to address chronic pain (24). Researchers found that eating lots of antioxidant, mineral, vitamin, and fiber-rich diet, lots of polyunsaturated fatty acids is important.
Some people may benefit from following a low-histamine or lactose-free diet. Probiotics and when it’s right, prebiotics may be helpful. The ketogenic diet and intermittent fasting may be beneficial, but for some migraines, headaches, and neuropathic pain some thrive on a low-fat plant-based diet, and for musculoskeletal issues, a higher protein diet may be best.
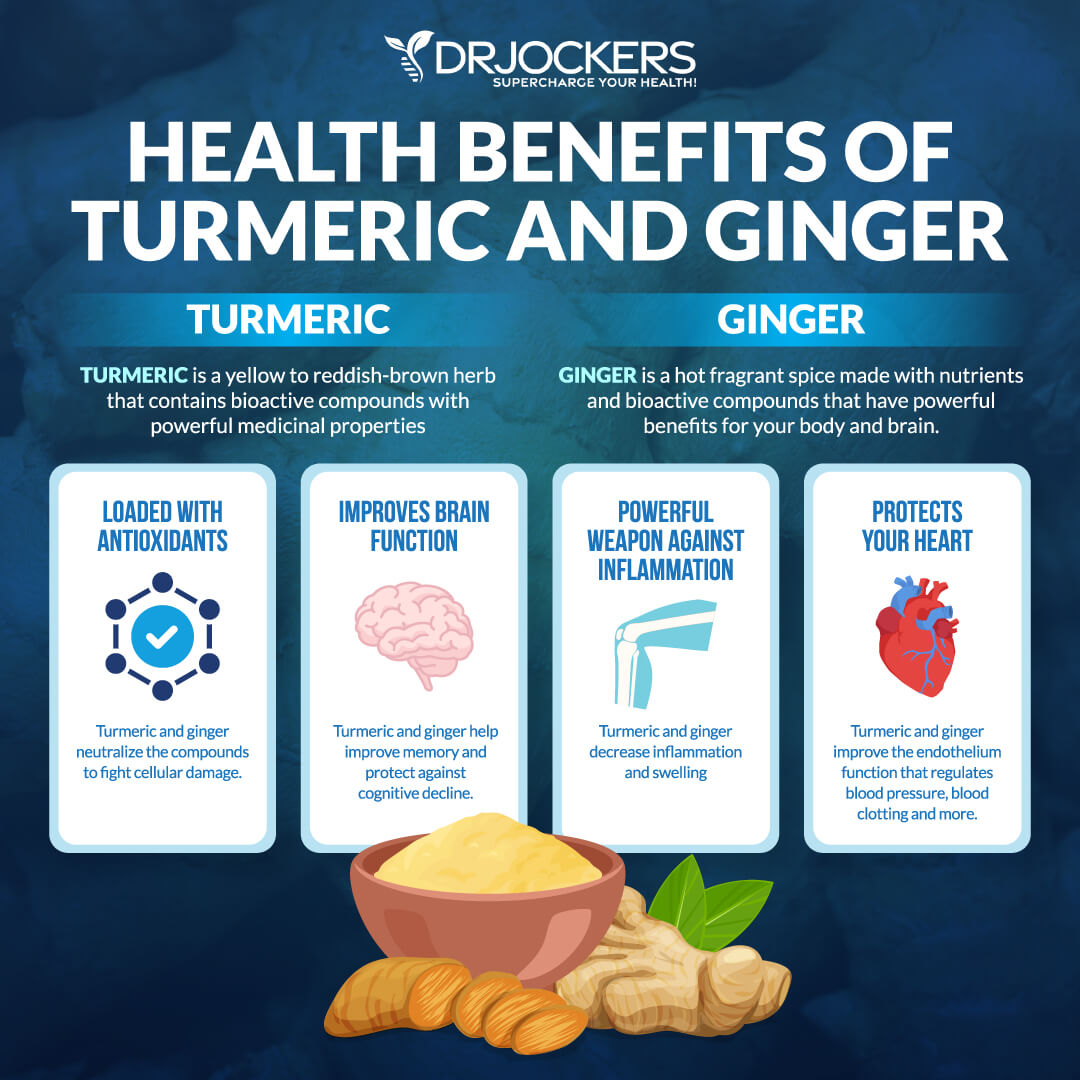
Focus on anti-inflammatory, nutrient-dense whole foods, such as greens, vegetables, sprouts, herbs, spices, fermented food, grass-fed beef, pasture-raised poultry and eggs, wild-caught fish, and wild game. Eat plenty of healthy fats, such as coconut oil, grass-fed butter and ghee, avocados, olives, and extra-virgin olive oil. Use anti-inflammatory spices, such as turmeric, ginger, onion, garlic, oregano, basil, rosemary, and cinnamon. You may learn more about the anti-inflammatory ketogenic diet I recommend for most people by reading this article.
Remove Food Sensitivities
A 2020 study published in Nutrients has found that removing certain food sensitivities, such as gluten, dairy, or high-histamine foods may be beneficial (24). You may benefit from testing for and removing foods that you may be sensitive to. Common food sensitivities include sugar, gluten, eggs, dairy, shellfish, seafood, soy, corn, and legumes. However, you may be sensitive to some less common items.
There are various blood tests used for food sensitivities. However, they only test for certain foods, and false results are not uncommon. You may try a pulse test or muscle testing to test your body’s reaction to any food. Additionally, I recommend an elimination diet. It is the best way to discover your personal food sensitivities. Remove all common and suspected food sensitivities for 4 weeks, then introduce them one-by-one back to your diet. Use a food journal to track your body’s reactions.
If you find a food that you are reacting to, remove them right away. You may try to introduce them again to double-check, but if you notice a reaction again, remove them. Since food sensitivities can change over time, I recommend performing these tests every year or if new symptoms or health issues occur. You may learn more about how to reduce food sensitivities by reading this article.
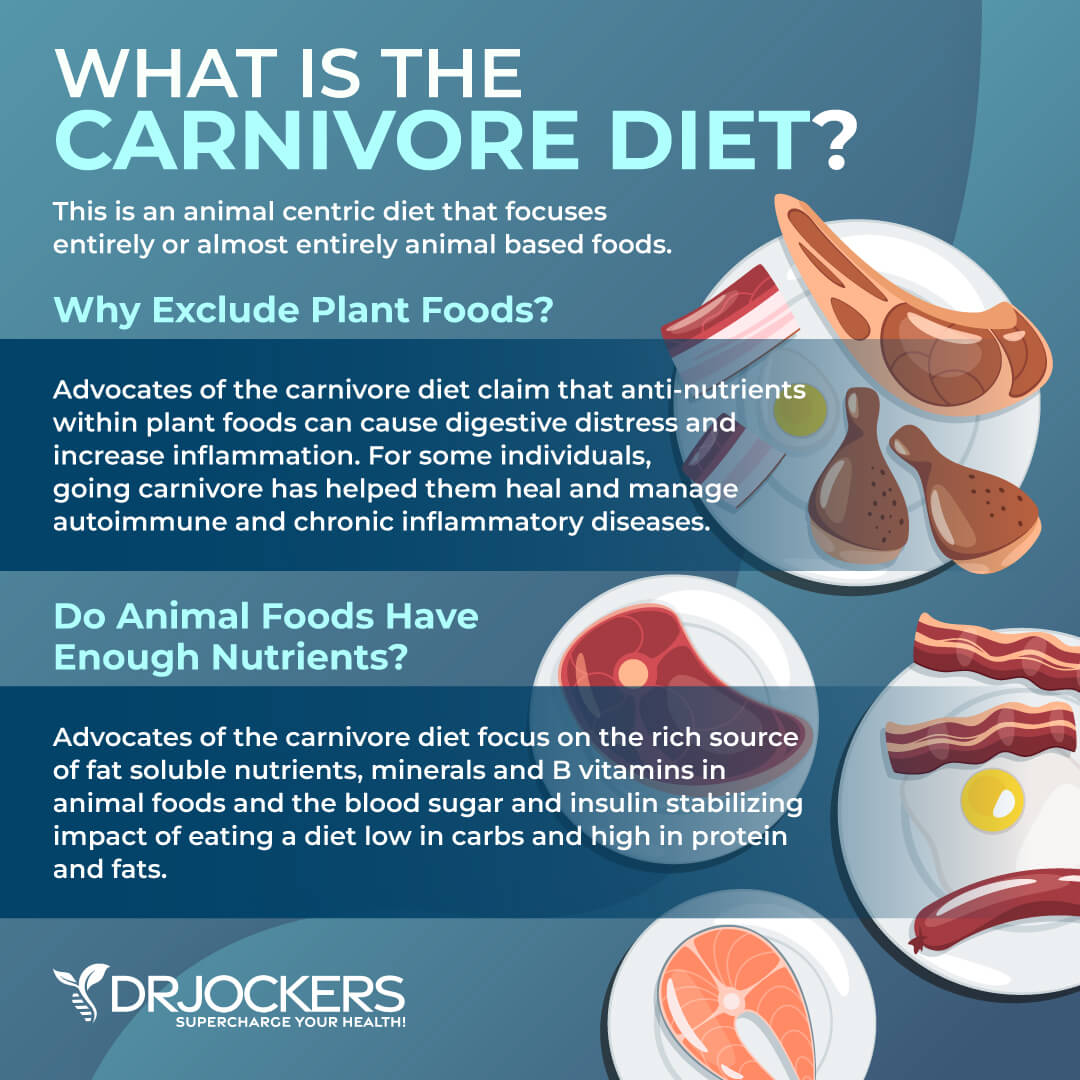
Consider a Low-FODMAP or Carnivore Diet
You may benefit from considering the low-FODMAP or Carnivore diet short-term. FODMAP stands for Fermentable, Oligo, Di-, and Monosaccharides, and Polyols. High-FODMAP foods include foods that are high in lactose, fructose, fructans, and polyols.
High-FODMAP foods tend to include many vegetables and fruits, legumes, dairy, sweeteners, grains, some alcohol, certain herbs, and certain teas. Some people have trouble digesting foods that are high in FODMAPs and develop all kinds of problems. A low-FODMAP diet is commonly used to improve small intestinal bacterial overgrowth (SIBO) and other digestive disorders.
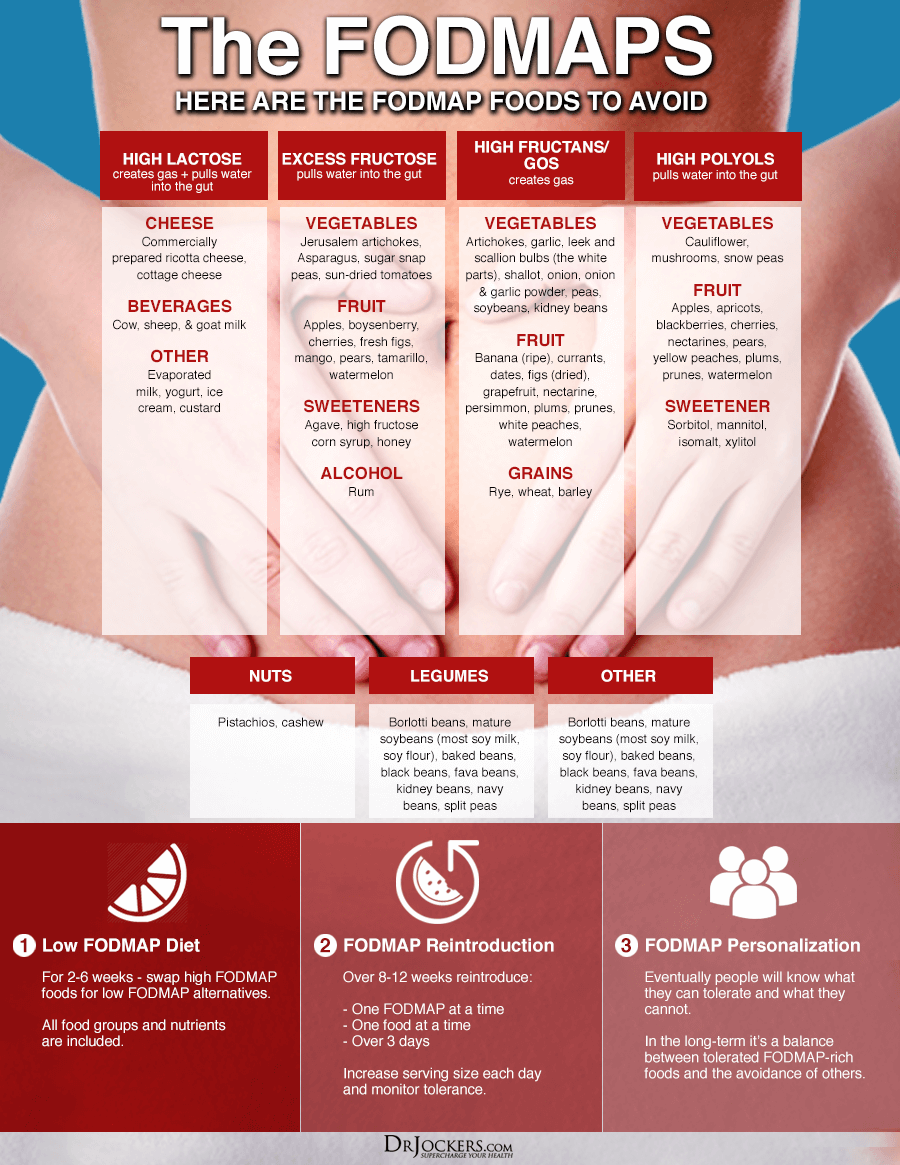
The Carnivore Diet is a low-carbohydrate, high-protein diet that includes meat, fish, organ meats, and in some cases, other animal foods, such as eggs or certain dairy. It is naturally low in FODMAPs. Used short-term, the Carnivore Diet may help to reduce inflammation, digestive issues, pain, and other problems.
A 2016 study published in the Scandinavian Journal of Pain has found that a low-FODMAP diet may help to decrease pain and improve quality of life in those with fibromyalgia (37). A 2017 study published in Nutricion Hospitalaria has also found that a low-FODMAP diet may benefit those with fibromyalgia (38).
A 2018 review published in the International Journal of Pediatrics has found that a low-FODMAP diet may help to reduce chronic pain in abdominal pain disorders (39). You may learn more about the low-FODMAP diet here and the Carnivore diet here.
Practice Intermittent Fasting
Intermittent fasting is a type of eating. It cycles between a period of fasting and a period of eating within one day. The most common form of intermittent fasting includes 16 hours of fasting including your overnight sleep and 8 hours reserved for your meals to meet your nutritional needs.
Intermittent fasting may improve autophagy, insulin sensitivity, digestion, inflammation, and other factors of health. It may help to reduce chronic pain.
A 2020 study published in Nutrients has found that intermittent fasting is one of the dietary strategies that may help to reduce chronic pain (24). A 2019 study published in Cell has found that intermittent fasting may reduce inflammation and symptoms of inflammatory diseases (40). A 2021 animal study published in the British Journal of Nutrition has found that intermittent fasting may help to reduce inflammation in osteoarthritis (41).
If you are new to intermittent fasting, begin with a 12-hour fast including your overnight sleep starting after dinner until the next day at breakfast. Gradually increase your fasting window by delaying breakfast and/or choosing an earlier dinner.
Most people feel the best with the 16:8 approach but you may find that fasting for a bit less or longer than 16 hours works better for you. To learn more about the benefits of intermittent fasting and the best intermittent fasting strategies, I recommend this article.
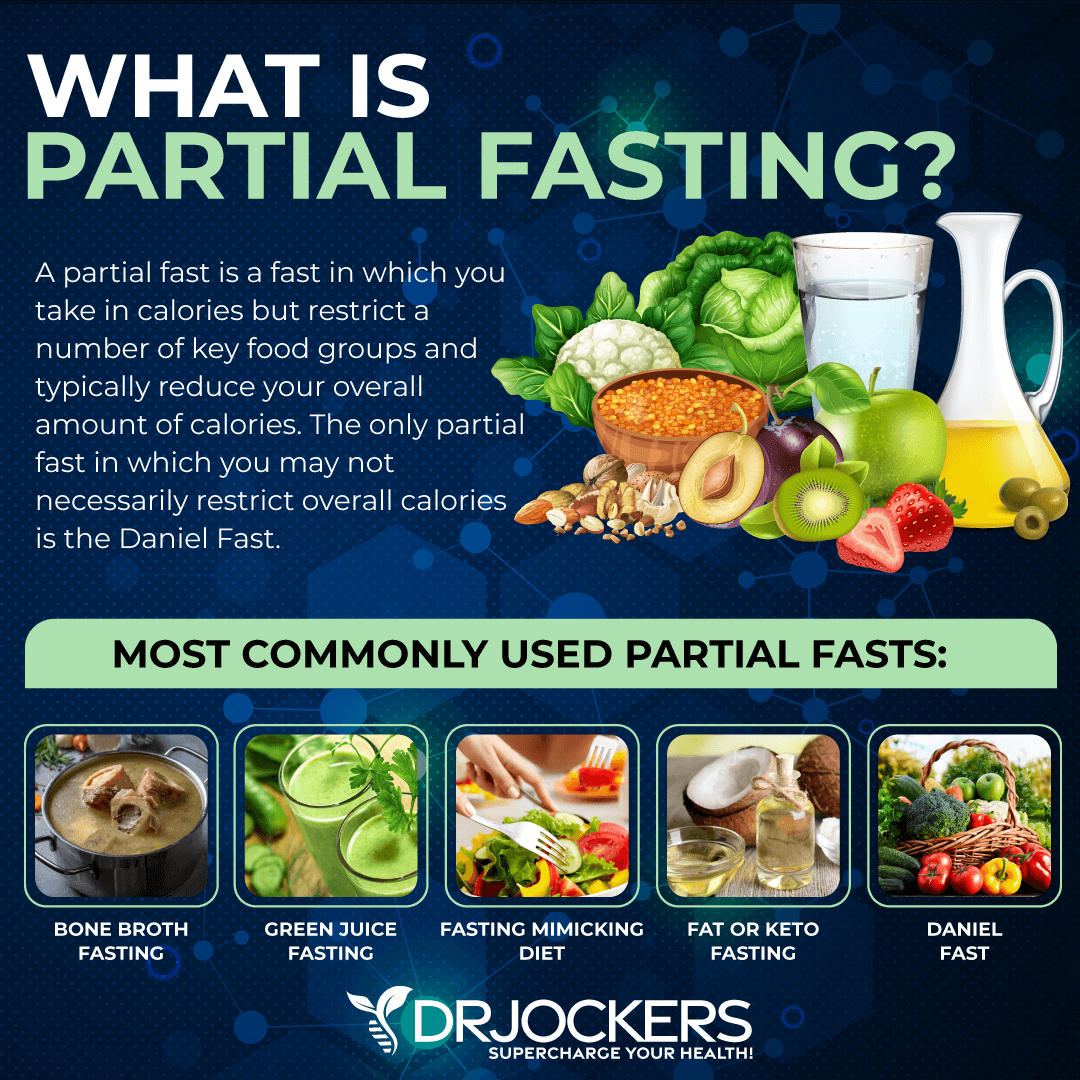
Consider a 3-5 Day Water or Partial Fast
If you are doing well on an intermittent fasting lifestyle, you may want to consider a 3–5-day water or partial fast. A 2016 study published in Cell Reproduction has found that Fasting Mimicking Diet® (FMD®), a partial fasting strategy, may help to reduce symptoms of MS and autoimmunity (42).
A 2017 study published in Molecular and Cellular Endocrinology has also found that FMD® may help to reduce the risk and support the treatment of autoimmune diseases (43). A 2002 study published in Forchende Komplementarmedizine und Klassisch Natuheildkunde has found that short-term fasting is safe and may help to improve chronic pain, symptoms of rheumatoid arthritis, and chronic fatigue syndrome (44).
The FMD® is a partial fasting plan that is high in nutrients, low in protein, and low in carbohydrates. It’s a 5-day protocol that you can do every 8 to 12 weeks or every month, depending on your health goals.
Other partial fasting strategies include Juice Fasting (only drinking green juice and in some cases, green smoothies for a period of time), Bone Broth Fasting (only drinking bone broth for the period of your fast), the Fat or Keto Fast (a high-fat and low-calorie diet to improve ketosis), and the Daniel Fast (a vegetarian fast based on Biblical principles). You may learn more about partial fasting from this article.
If you are doing well on more advanced intermittent fasting and practicing partial fasting, you may be ready for a water fast. Water fasting means that you are staying away from food completely for the period of your fast.
You are only drinking plenty of purified, clean water throughout the day and in some cases, also some calorie-free herbal tea. Water fasting is a very advanced fasting strategy that I only recommend if you are experienced with fasting and only after a consult with your healthcare provider You may learn more about water fasting here.
Reduce Stress and Prioritize Good Sleep
Chronic stress and poor sleep may increase the risk and symptoms of chronic pain (26,27, 28, 29, 30, 31, 32, 33). If you want to improve your chronic pain, addressing stress and sleep are essential. Reduce stressful situations, tasks, and interactions with people that bring you down as much as possible. Instead of scrolling the news and social media, choose a specific time during the day to check it and forget about it for the rest of the day.
Choose activities that uplift you and spend time with supportive friends and family. Spend time in nature regularly. Practice prayer, meditation, breathwork, gratitude, guided relaxation, and positive affirmation.
Avoid electronics, sugar, heavy foods, and alcohol in the evening. Engage in relaxing activities before going to bed, including crossword puzzles, coloring, board games, reading, journaling, meditation, and healing baths. Go to bed and wake up around the same time every day. Support your sleep with a comfortable mattress, pillows, and bedding, calming colors, essential oils, blackout curtains, and a sleep mask.

Regular Movement and Exercise
Exercise may seem counter-productive when you are dealing with chronic pain, but it can be actually helpful. According to a 2015 review published in the Best Practice and Research in Clinical Pharmacology, moderate exercise 2 – 3 times a week may help to reduce chronic pain (45). A 2017 review published in the Cochrane Database of Systematic Reviews has also found that exercise may help to improve chronic pain in adults (46). According to a 2019 study published in the Journal of Evidence-Based Integrative Medicine, practicing yoga twice a week for two weeks may help to lower chronic pain (47).
I recommend moving your body regularly. Start your day by stretching out your body or some yoga, a short walk, or some rebounding. Get up to stretch and shake out your body regularly throughout the day. Take a stroll at a nearby park, take the stairs, play with your kids or pets, and try an impromptu dance session. End your day with some easy stretching.
Exercise regularly, ideally at least 20 – 30 minutes 5 times a week. Incorporate regular strength and resistance training to improve your muscle, bone, and joint strength. Weight training with free weights or weight machines, bodyweight exercises, kettlebell training, TRX, and CrossFit are great ideas.
Try low-impact exercises that strengthen your body, improve balance and flexibility, and calm your mind in the process, such as yoga, pilates, Barre, Tai Chi, or Qi Gong. Add some cardio through swimming, biking, hiking, brisk walking, or jogging. If you are dealing with chronic pain due to an overuse injury, sports injury, or accident, work with a physical therapist to strengthen your body and to return to your regular activities safely.

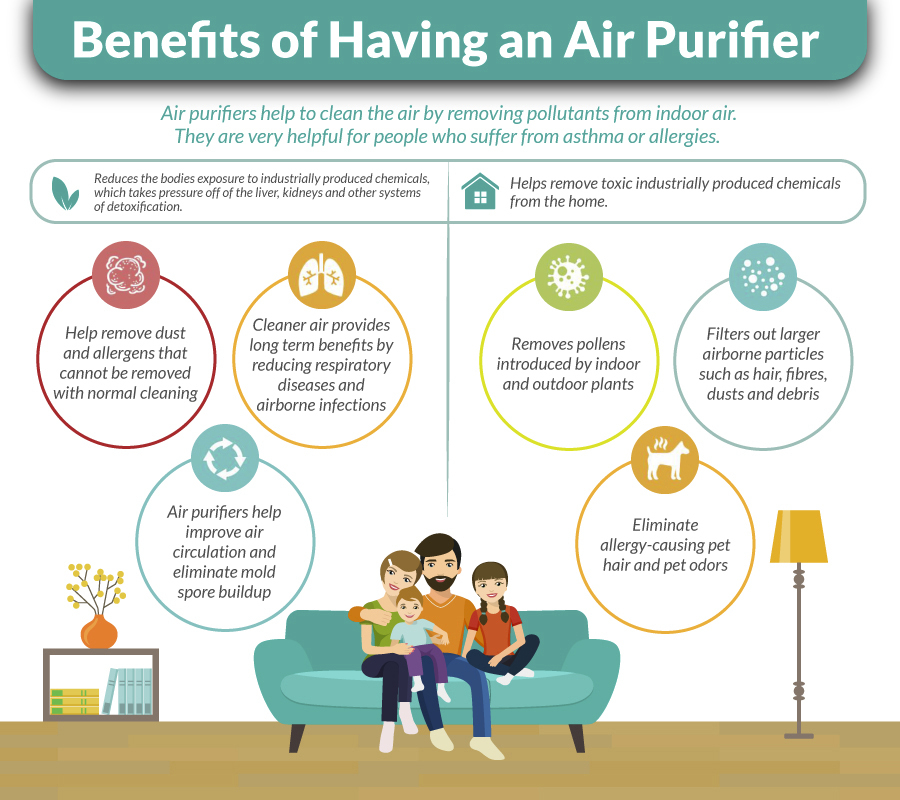
Remove Mold and Improve Air Quality
Chronic mold exposure and mold mycotoxins may increase the risk and symptoms of chronic pain (24, 25). Removing mold and improving indoor air quality is critical. Check your home for mold, including at hidden places. Work with a professional mold remediation specialist to remove mold from your home and offer tips to reduce mold problems. Eliminate any moisture leaks. Use a dehumidifier during warmer months and in places with lots of moisture and humidity in the air, such as your bathroom.
Invest in a high-quality HEPA air filtration system or Air Doctor to remove mold, allergens, and toxins from your indoor air. Get some indoor plants to improve oxygen in your home. Spend regular time in nature on fresh air.
Physical Therapies
You may benefit from physical therapies and bodywork, including physical therapy, chiropractic care, massage therapy, or acupuncture on a regular basis. According to a 2017 study published in the Turkish Journal of Physical Medicine and Rehabilitation, physical therapy may help to improve chronic low back pain (48). A 2017 study published in the Journal of Manual and Manipulative Physical Therapy, manual physical therapy may help with chronic pain (49).
A 2018 case report published in the Journal of Chiropractic Medicine has found that chiropractic care may help to improve chronic pain (50). A 2003 randomized trial published in the Journal of Alternative and Complementary Medicine has found that massage therapy may be beneficial for those with chronic pain (51). A 2018 review published in the Journal of Pain has found that acupuncture may be effective for reducing chronic pain (52).
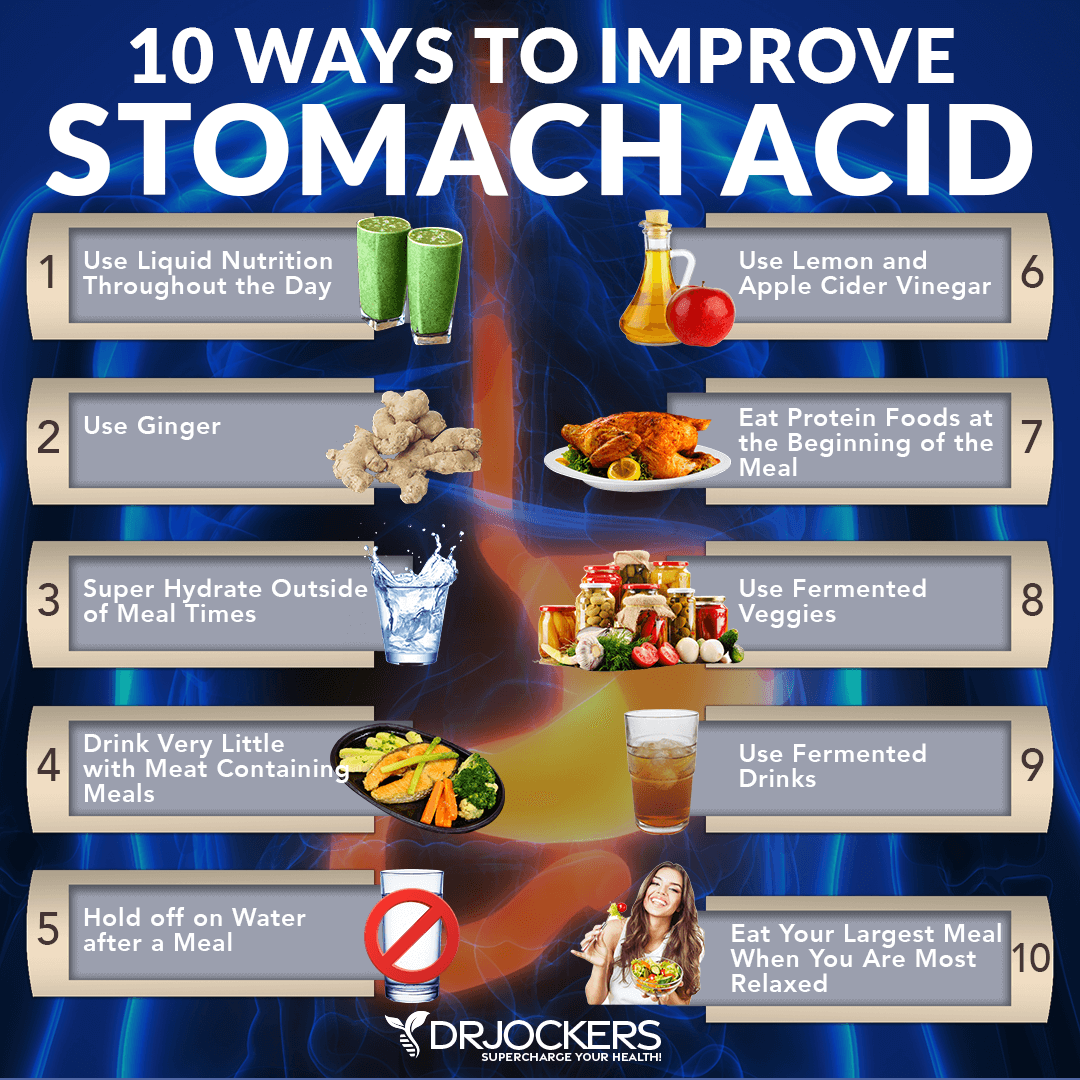
Remove Gut Infections and Optimize Stomach Acid Levels
Chronic infections and gut microbiome imbalances may contribute to chronic pain (10, 16, 17, 18, 19, 20, 21, 22, 23, 24). Testing and treating gut infections is critical for recovery if you have abdominal bloating or other digestion symptoms. I recommend a GI Map Stool Test to understand your digestive health and help appropriate lifestyle changes and supplementation for improved digestive health. For Candida overgrowth, I recommend the Candida Support Pack, for parasite overgrowth, the Parasite Support Pack, and for SIBO, the SIBO Support Pack.
To reduce stomach acid, consider taking Betaine HCL with meals. I recommend Super Digest HCL. Take it regularly with your meals. Eating slowly and mindfully may also reduce symptoms of low stomach acid and aid digestion.
Drink plenty of water throughout the day. However, when you are eating meat or any sort of heavier food, you should stop drinking water or other liquids at least 30 minutes before the meal, except if you need to take a supplement with 2 ounces of water.
Holding off water during these meals will reduce any potential dilution of the gastric juices and allow for better digestion. Drink ginger tea regularly to improve your digestive juices. Lemon water or apple cider vinegar mixed with water may also help to improve stomach acid levels. Try fermented foods and drinks, such as sauerkraut, kimchi, fermented vegetables, kombucha, coconut kefir, and coconut yogurts.
Heal the Gut Lining
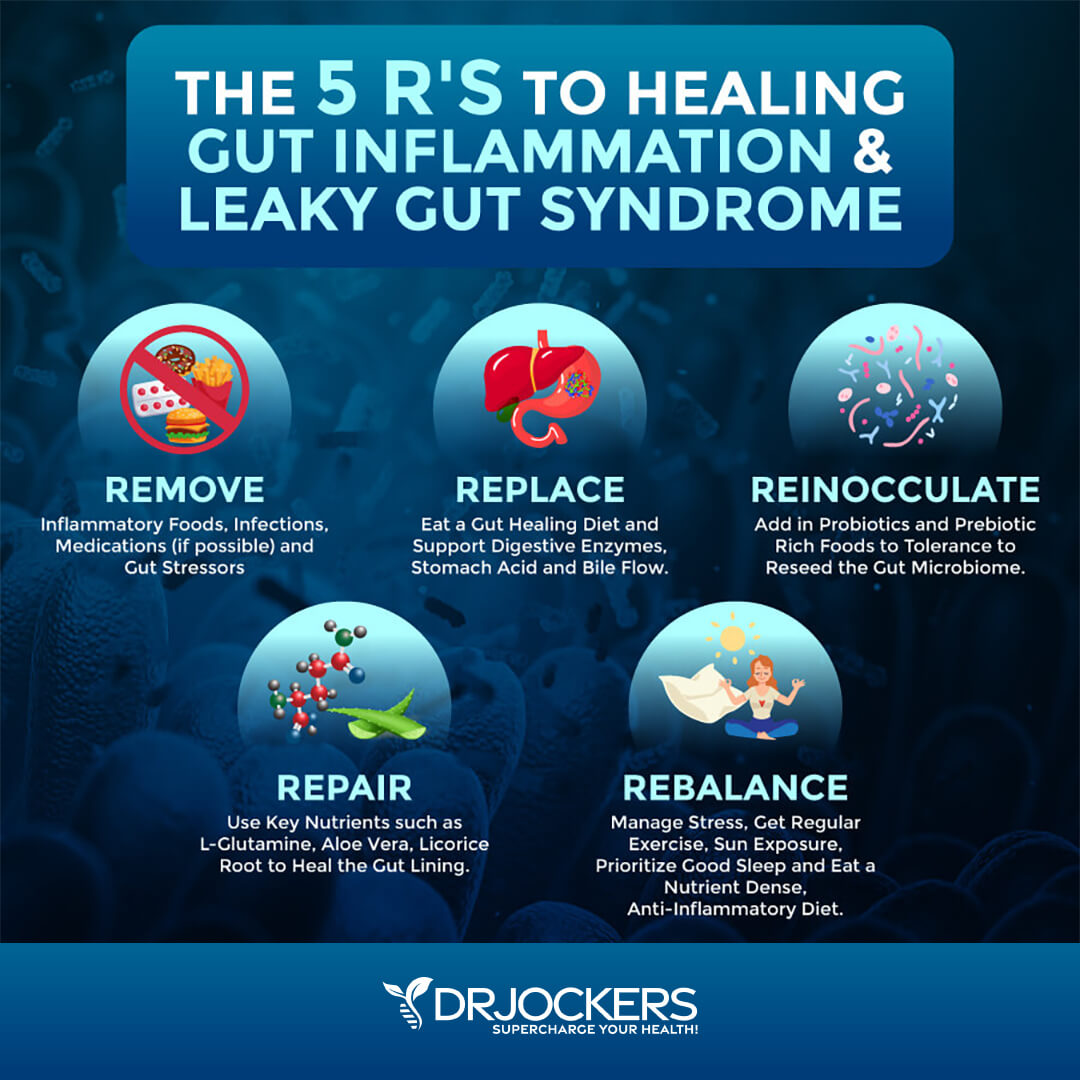
Leaky gut and gut microbiome imbalance are some of the common culprits behind chronic pain (20, 21, 22, 23, 24). Improving your gut lining is critical to recover from leaky gut syndrome and restore gut flora balance.
The key to heal the gut lining is to reduce gut inflammation by following the 5 R’s. The first R is removing inflammatory foods, infections, gut stressors and medications that damage the gut lining (including NSAIDs and Opioids).
The second R is to eat a gut healing diet, support digestive enzymes, stomach acid levels and bile flow. The 3rd R is to reinnoculate the gut with probiotics and prebiotic rich foods to tolerance in order to reseed the gut microbiome.
The 4th R is to rebuild the gut lining by using key nutrients such as L-glutamine, aloe vera, licorice root, slippery elm and butyric acid in order to heal and seal the gut lining. The 5th R is to rebalance the body with good lifestyle habits to lead an enjoyable and healthy life.
Optimize Vitamin D Levels
Vitamin D deficiency may increase the risk and symptoms of chronic pain (35, 36). Optimizing your vitamin D levels is critical. According to a 2019 study published in the Journal of American Medical Directors Association, taking vitamin D may help to reduce chronic pain in older people (53).
To improve your vitamin D levels, I recommend spending time out in the sun and eating vitamin D-rich fatty fish, egg yolks, and beef liver. Most people are not getting enough sunshine or consuming enough vitamin D from food. Therefore, most people need supplements to optimize their vitamin D levels.
Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and inflammation control. I recommend taking a vitamin D3 supplement with at least 3,000-5,000 IU’s of vitamin D3 and at least 90 mcg of vitamin K2. I highly recommend Vitamin D3/K2 Power. This supplement works to support your immune, skin, cardiovascular, and bone health.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for major health conditions is going to be between 70-100 ng/ml.
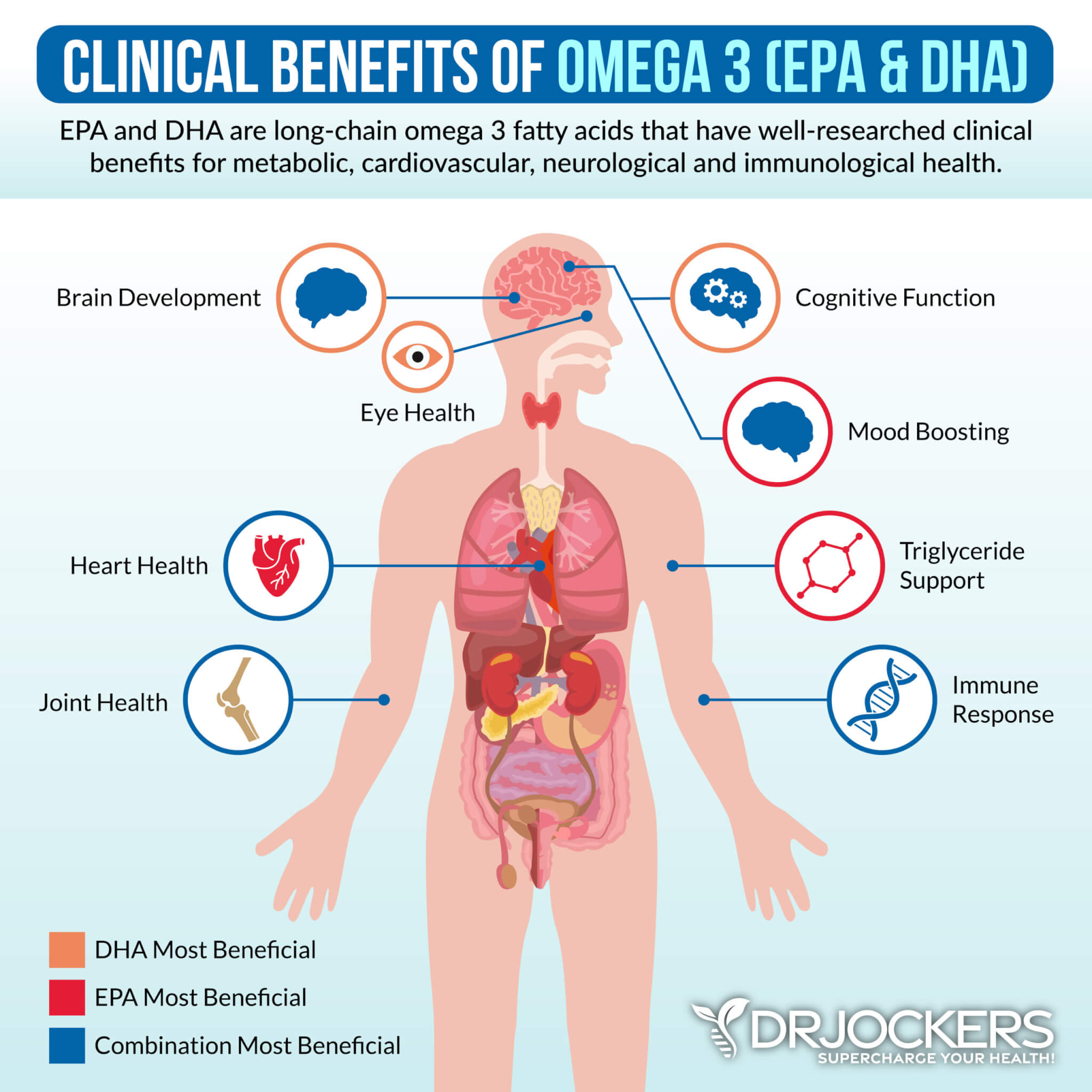
Consider Omega 3 Fatty Acids
Omega-3 fatty acids offer anti-inflammatory benefits that may help to lower chronic pain. A 2007 meta-analysis published in Pain has found that omega-3 fatty acids may help to reduce inflammatory chronic joint pain (54). A 2020 study published in Rheumatology Advances in Practice has found that omega-3 fatty acids in fish oil may help to decrease chronic pain in osteoarthritis (55).
To optimize your omega-3 levels, I recommend consuming wild-caught fish, flaxseed, chia seeds, hemp seeds, and walnuts. I also recommend taking a high-quality omega-3 fish oil supplement with EPA and DHA, such as Pro Omega Curcumin. This supplement offers anti-inflammatory benefits, reduces oxidative stress, promotes cellular recovery, supports skin health, improves the gut lining, supports vascular elasticity, optimizes cell signaling, and improves gene expression.
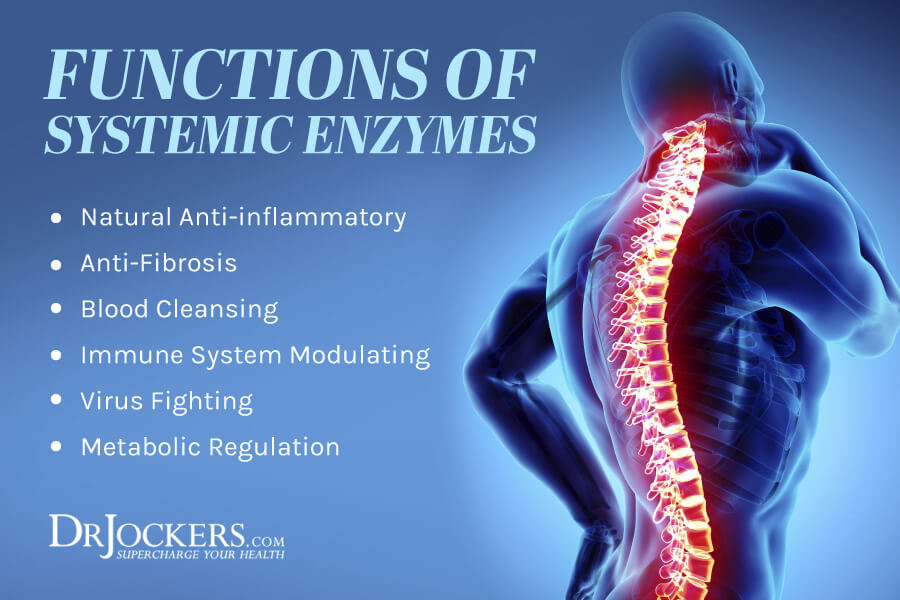
Consider Using Proteolytic Enzymes
Proteolytic enzymes are a group of enzymes that break the long chain-like protein molecules into shorter fragments called peptides then into their components, called amino acids. According to a 2008 animal study published in the Indian Journal of Pharmacological Sciences, proteolytic enzymes can help to reduce inflammation (56).
According to a 2016 review of six randomized controlled trials, proteolytic enzymes may be beneficial for knee osteoarthritis pain (57). I recommend taking Proteo Enzyme for joint inflammation.
Use Anti-Inflammatory Herbs
Using anti-inflammatory herbs may also help to reduce chronic pain symptoms. I recommend the following anti-inflammatory herbs and compounds:
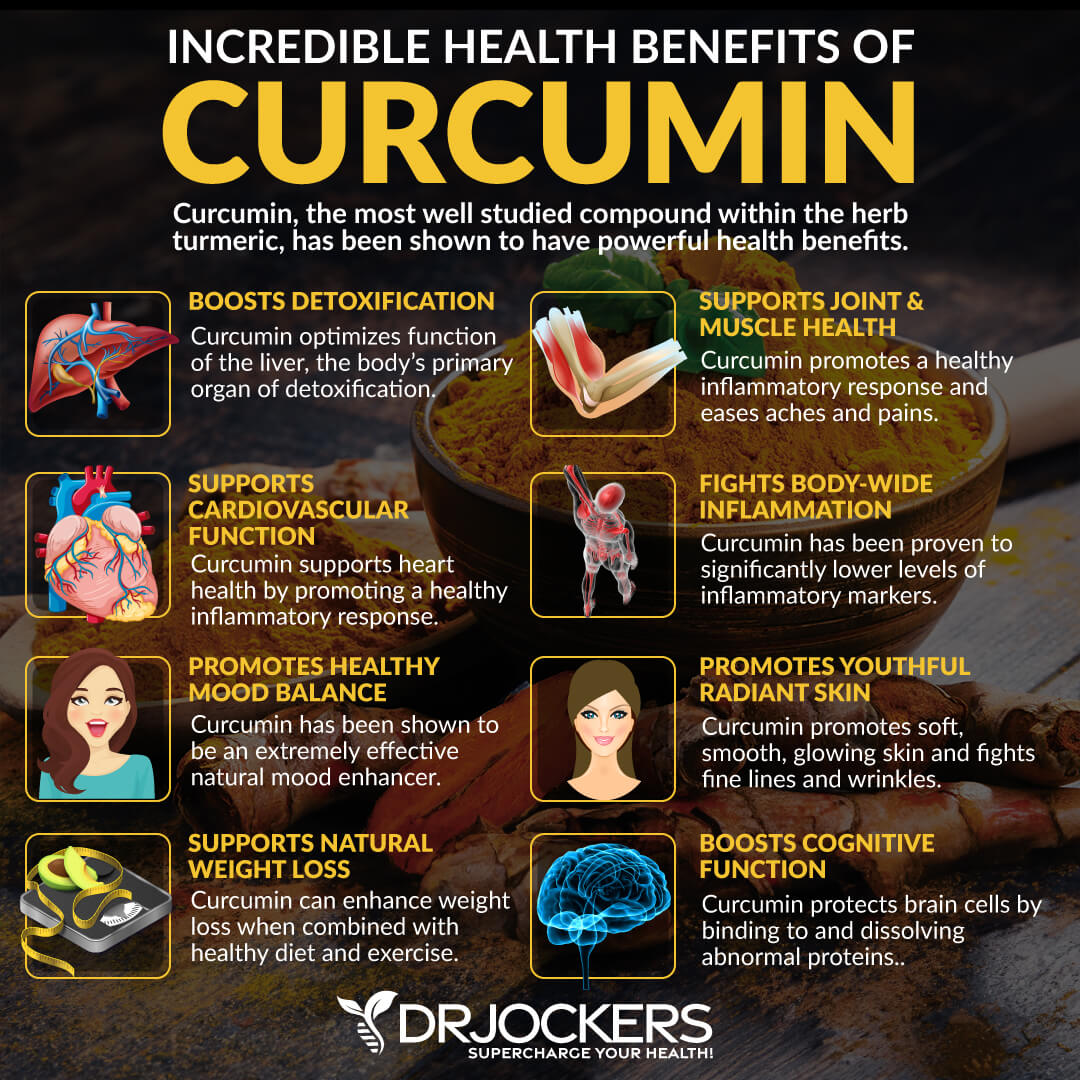
Turmeric
Curcumin is the active ingredient of one of the most research anti-inflammatory herbs, turmeric. According to a 2016 systematic review and meta-analysis of randomized clinical trials, turmeric extracts and curcumin may reduce the pain from joint arthritis (58). According to a 2016 review published in Drug Design, Development, and Therapy, curcumin has anti-inflammatory benefits for osteoarthritis (59).
Boswellia
Boswellia is a plant that produces Indian frankincense and offers anti-inflammatory benefits. According to a 2019 trial published in Phytotherapy Research, boswellia extract can be helpful in the management of knee pain(60).
A 2020 systematic review and meta-analysis published in BMC Complementary Medicine and Therapies, has also found that boswellia can have anti-inflammatory benefits for chronic joint pain (61).
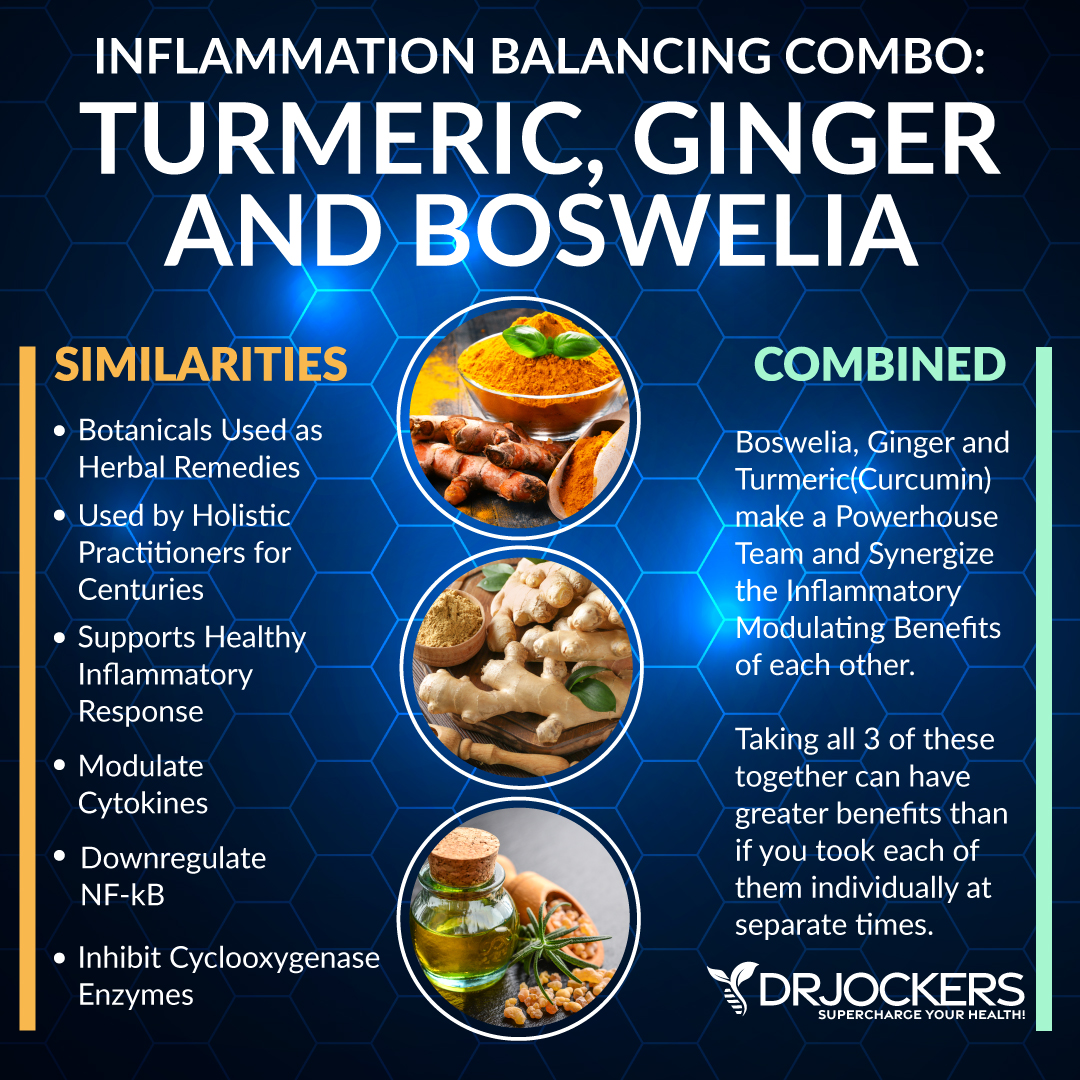
Ginger
Ginger is an anti-inflammatory herb similar to and from the same family as turmeric. According to a 2001 study published in Arthritis Rheumatology, ginger has shown positive benefits for chronic knee pain (62). A 2015 systematic review published in Nutrition Journal has found that ginger offers anti-inflammatory benefits (63).
Furthermore, a 2013 comparative study published in the International Journal of Rheumatic Disease has found that ginger and turmeric used combined have anti-inflammatory benefits for joint inflammation (64). I recommend Inflam Defense™, a supplement with a powerful combination of curcumin, boswellia, ginger, and other anti-inflammatory herbs, such as rosemary, resveratrol, quercetin, rutin, and proteolytic enzymes.
CBD Oil
Cannabidiol, or CBD, or CBD oil, is one of the over one hundred chemical compounds known as cannabinoids found in the cannabis plant, including hemp and marijuana, or Cannabis sativa. CBD oil may help to reduce chronic pain and other health issues without experiencing the mind-altering effects of THC or toxicity from pharmaceutical pain medications.
A 2012 study published in the Journal of Experimental Medicine has found that CBD oil may help to lower inflammatory and neuropathic pain (65). A 2019 systematic review and meta-analysis published in JAMA Psychiatry has found that CBD oil may help to reduce pain (66). A 2020 review published in Frontiers in Pharmacology has found that CBD oil may be an effective way to reduce chronic pain (67). You may learn more about how to use CBD oil for pain relief by reading this article.

Final Thoughts
Millions of people in the United States are living with some form of chronic pain daily. Chronic pain can seriously interfere with your daily activities, work, studies, family life, social life, and emotional well-being. It may even lead to disability. If you are experiencing chronic pain, I recommend that you follow my natural support strategies to improve your health and well-being.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!