Diverticulitis: Causes, Symptoms & Natural Support Strategies
Is it possible to heal diverticulitis naturally? Let’s say a routine colonoscopy has confirmed that the abdominal complications you have been experiencing are a consequence of diverticulitis. You have been prescribed antibiotics as the recommended conventional treatment for the disease but is this approach in your best interest?
Antibiotic treatment has its own risks and can cause pain within the first few days of treatment in which patients are then usually prescribed narcotics. So what should you do?
Ignoring signs of the failing health of your digestive tract can lead to worsening symptoms, weakened immunity, and the possibility of interventions like unnecessary surgery in the future. Fortunately, there are many things you can do to support gut and digestive health and in this article, I will go over my top 4 steps.
What Causes Diverticulitis?
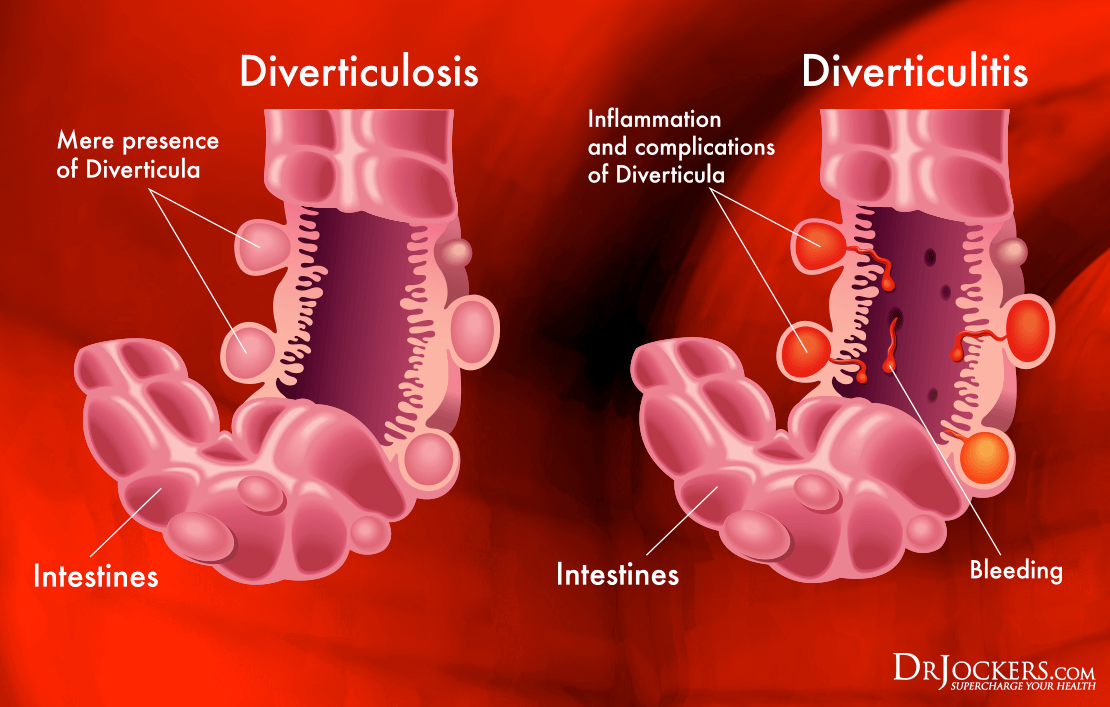
Small, tubular-shaped bulging sacs along the gastrointestinal tract increase in prevalence with age affecting 70% of individuals before they reach 80 years old (13). These pouches are called diverticula and usually concentrate along the colon. Inflammation of one diverticulum or several diverticula can be triggered by a hard mass of feces causing bacteria overgrowth and a resulting infection known as diverticulitis. (1)
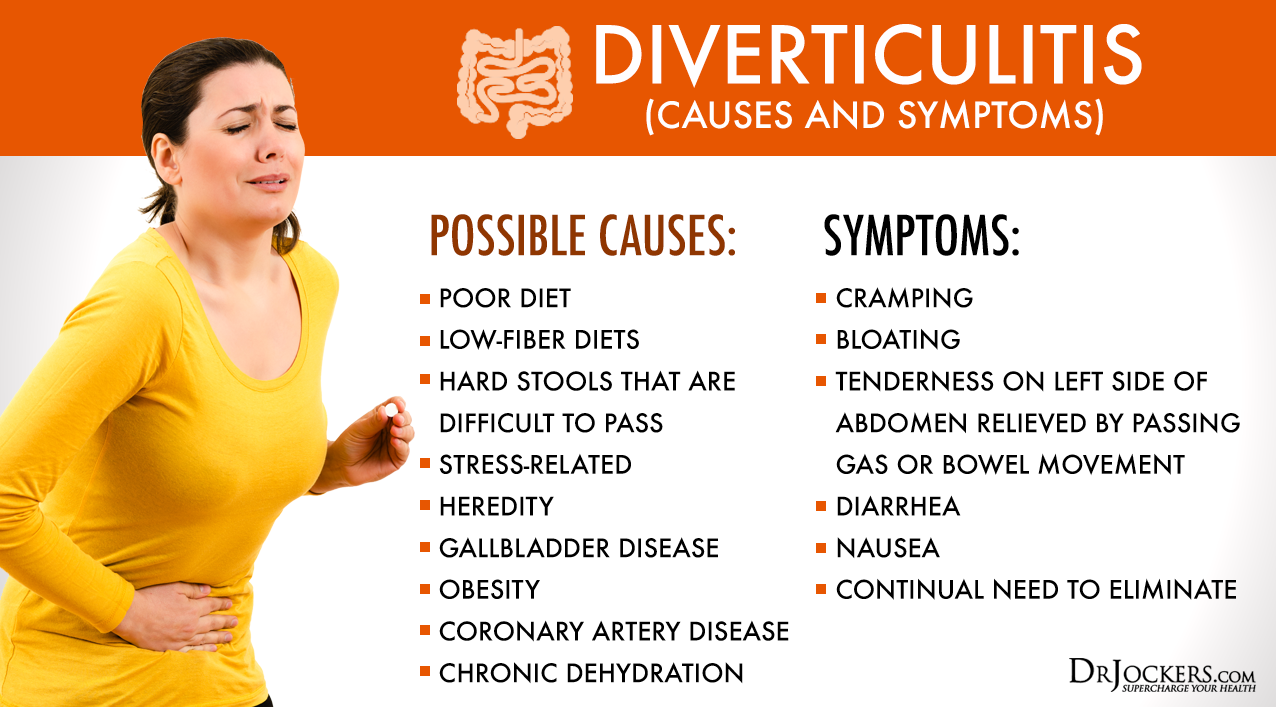
Various influences contribute to impacted diverticula and infection. One of the greatest factors believed to affect incidence rates is diet. Today our bodies are burdened with managing poor dietary habits in a culture consumed by processed goods, sugar, and trans-fats. Our busy lifestyle has us neglecting the healthy lifestyle choices we should be making.
As a consequence, we deny ourselves sufficient time to exercise, lack antioxidant and fiber-rich plant-based foods in our diet, and temporarily mask the stress and pain we feel with anti-inflammatory drugs, laxatives, and poor habits like smoking. For these reasons, diverticulitis is referred to as a “disease of modern man” (12).
A combination of these poor lifestyle habits causes inflammation of the diverticula sacs. As fecal matter hardens and bacteria accumulate, these pouches grow increasing pressure on the intestinal wall leading to worsening symptoms. Abnormal gut flora are also associated with impaired mucus membranes along the intestines and the upregulation of inflammatory cytokines (13).
Diverticulitis Symptoms:
Diverticula are rare to cause problems but when they do they cause significant abdominal pain and discomfort. Many people mistake diverticulitis with appendicitis, but diverticulitis typically shows up with pain on the left side of the bowel. Appendicitis is characterized by pain on the lower right side of the stomach and may be a medical emergency. Diverticulitis symptoms may include: (13)
- Nausea
- Change in bowel habits
- Fever
- Flatulence
- Cramping
- Diarrhea
- Constipation
- Bowel pain, typically on the left side
- Red coloring or blood in stool
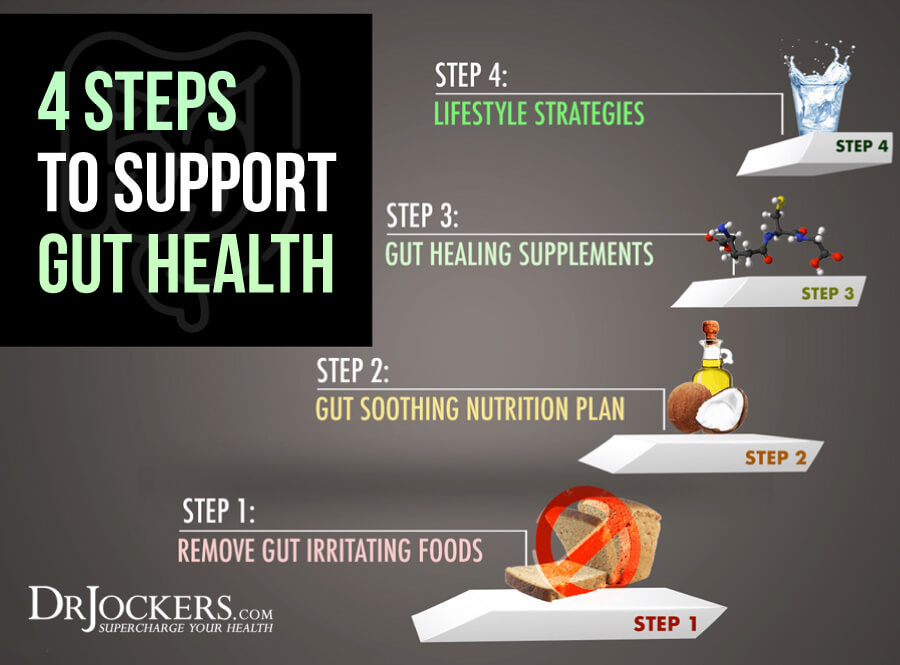
1) Remove Gut Irritating Foods
Common food allergens associated with diverticulitis include gluten, grains, corn, soy, nuts, and seeds. These foods, commonly GMO crops, disturb the balance of beneficial bacteria present in the gut leading to gastrointestinal disturbances and a weakened immune response.
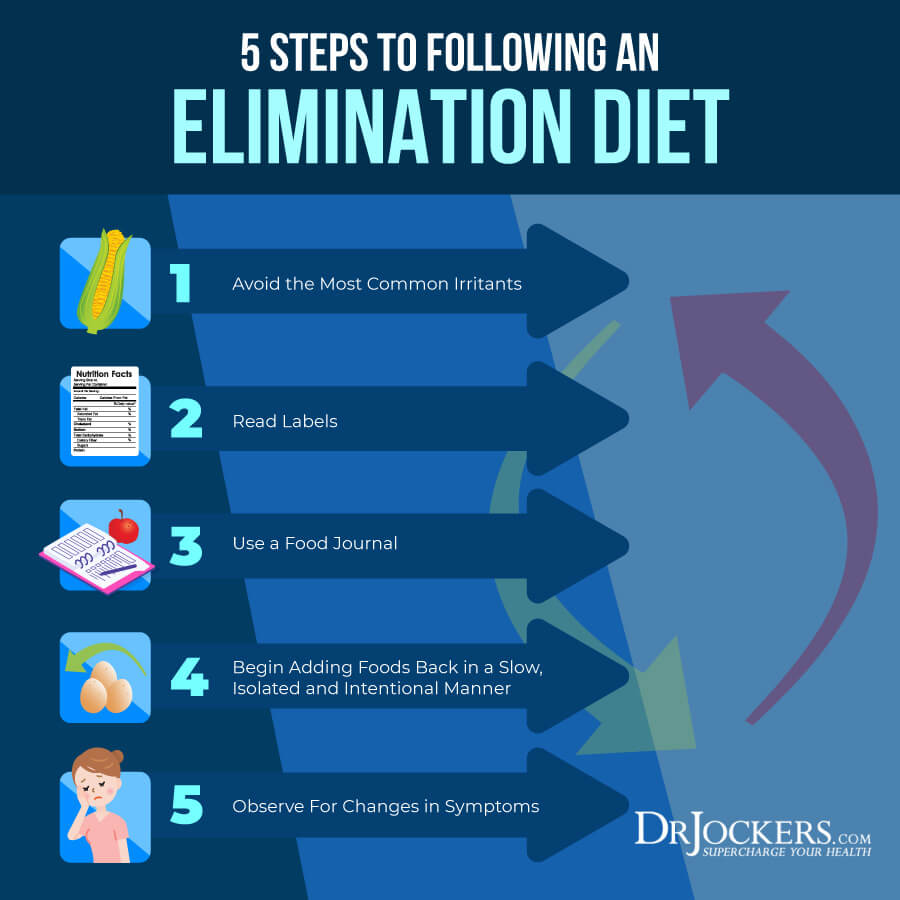
Clinically, diverticulitis is comparable in symptoms to irritable bowel syndrome (IBS). In a study, these patients have low concentrations of good bacteria, heightened inflammation, and weakened immune systems. By addressing food sensitivities through an elimination diet, the patients’ symptoms significantly improved. (14)
Some patients report experiencing pain in the lower left lower abdomen when consuming foods like seeds and nuts feared to become lodged into a diverticulum (12). However, diverticulitis can be accompanied by other bowel complications like irritable bowel syndrome making the cause of diverticulitis hard to identify.
Learn what food irritants trigger your diverticulitis symptoms by learning these 5 Steps to Following an Elimination Diet. Giving your gut the rest it needs from food irritants can help you heal your gut and improve digestive health.
2) Gut Soothing Nutrition Plan
Eating foods that have anti-inflammatory properties and support the immune system is one of the best lifestyle changes you can make to heal diverticulitis. These foods are inexpensive, effective, and safe.
It is important to note that these foods are not currently FDA-approved to prevent, mitigate, treat, or cure diverticulitis. With that said, I believe they can be a very helpful part of a healing plan.
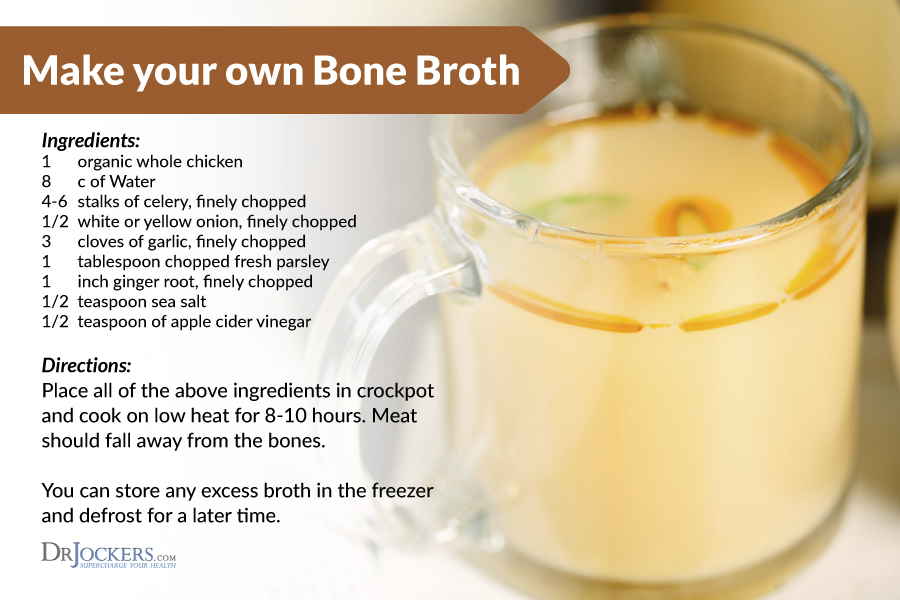
Bone Broth:
Sip on bone broth as you would drink tea throughout the day or add it to your favorite meals to give your soups and stews a health boost. Bone broth prepared from 100% grass-fed meat bones is loaded with benefits for the digestive tract.
It contains essential nutrients like magnesium, potassium, and calcium to stimulate healthy gut function. It is also high in collagen and amino acids glycine, glutamine, and proline which inhibit bacterial inflammation by fueling macrophages and lymphocytes to support wound healing. (2, 3)
Incorporating bone broth into your day is simple. You can drink it at any time of your day or even use it as a meal replacement. You may make homemade broth with the recipe in the image below or you can buy organic bone broth at health food stores and online.
My favorite pre-made brand is Kettle & Fire which uses grass-fed bones, organic vegetables & herbs, and a slow cooking process to extract all the minerals and nutrients into the broth. You can find Kettle and Fire at many grocery stores or check it out here for 20% off your order.
Coconut Oil:
The medium-chain triglyceride, lauric acid, is broken down in the body into an antibacterial compound called monolaurin. Monolaurin can help alleviate concerns with indigestion and constipation by reducing inflammation and inhibiting pathogenic bacteria buildup (10, 11).
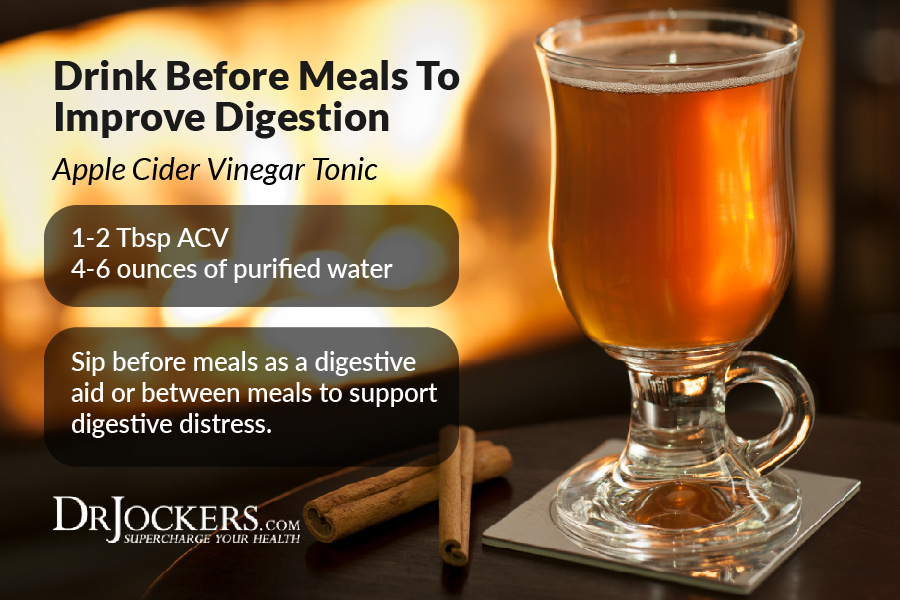
Apple Cider Vinegar:
Due to its high acetic acid content, apple cider vinegar has potent antimicrobial properties that can reduce the overgrowth of bacteria in the colon and aid in the removal of waste from the body (15). Acetic acid promotes colonic transit by improving alkalinity in the digestive tract and providing immune support by regulating homeostatic factors that limit oxidative stress and inflammation (16).
Ginger:
This therapeutic plant has been traditionally used for its medicinal properties for thousands of years. You too can use it to help with symptoms of nausea and indigestion you experience during a flare-up. Used regularly, ginger contains over 100 different chemical compounds that relax the lining of smooth muscle in the gut and aid in cleansing the digestive tract. (9)
Turmeric:
In individuals with acute diverticulitis, inflammation is believed to be the major cause of symptoms. Treating diverticulitis with anti-inflammatory agents like turmeric is one of the best strategies to find relief from symptoms and healing. Turmeric has been shown to heal inflammation associated with bowel diseases and heal tissue damage along the digestive tract (17).
When anti-inflammatory supplements are taken, individuals with diverticulitis can find complete remission from symptoms (13).
Fermented Foods and Drinks:
Foods like sauerkraut, coconut water kefir, kimchi, and pickles are excellent for intestinal health because of the healthy bacteria they contain. These probiotic foods reduce inflammation in the gut and decrease the permeability of the intestinal lining which can promote digestive diseases (4).
3) Gut Healing Supplements
In diverticulitis, the gut is severely worn down and needs the help of advanced supplementation to heal and rebuild. Clinically, I will use a wide variety of key supplements to help support gut health.
It is important to note that these supplements are not currently FDA-approved to prevent, mitigate, treat or cure diverticulitis and they should not be confused as such. With that said, I believe they can be very helpful to include in your healing plan.
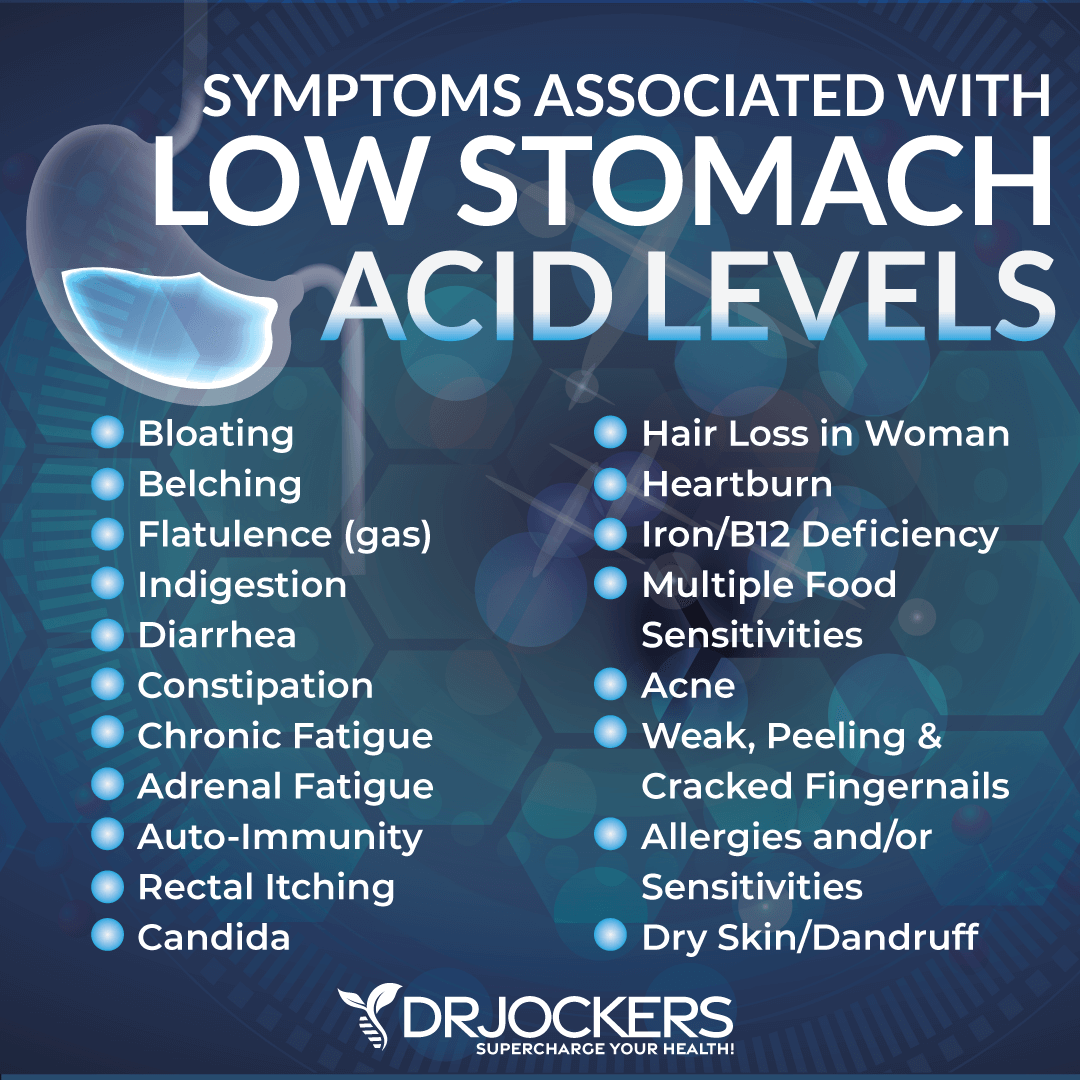
Betaine HCL:
Low hydrochloric acid (HCL) in the stomach can give rise to a variety of digestive disturbances that fuel bacteria overgrowth and infection in the intestines (22). As we get older, the production of HCL in the stomach begins to naturally decrease and may be partly to blame for the increased incidence of diverticulitis following age 40.
Supplementing with Betaine HCL during a meal is important to stimulate digestive enzymes so that foods, especially protein compounds, are broken down more easily improving digestive motility and preventing bacterial fermentation. We use acid prozyme for the Betaine HCL support.
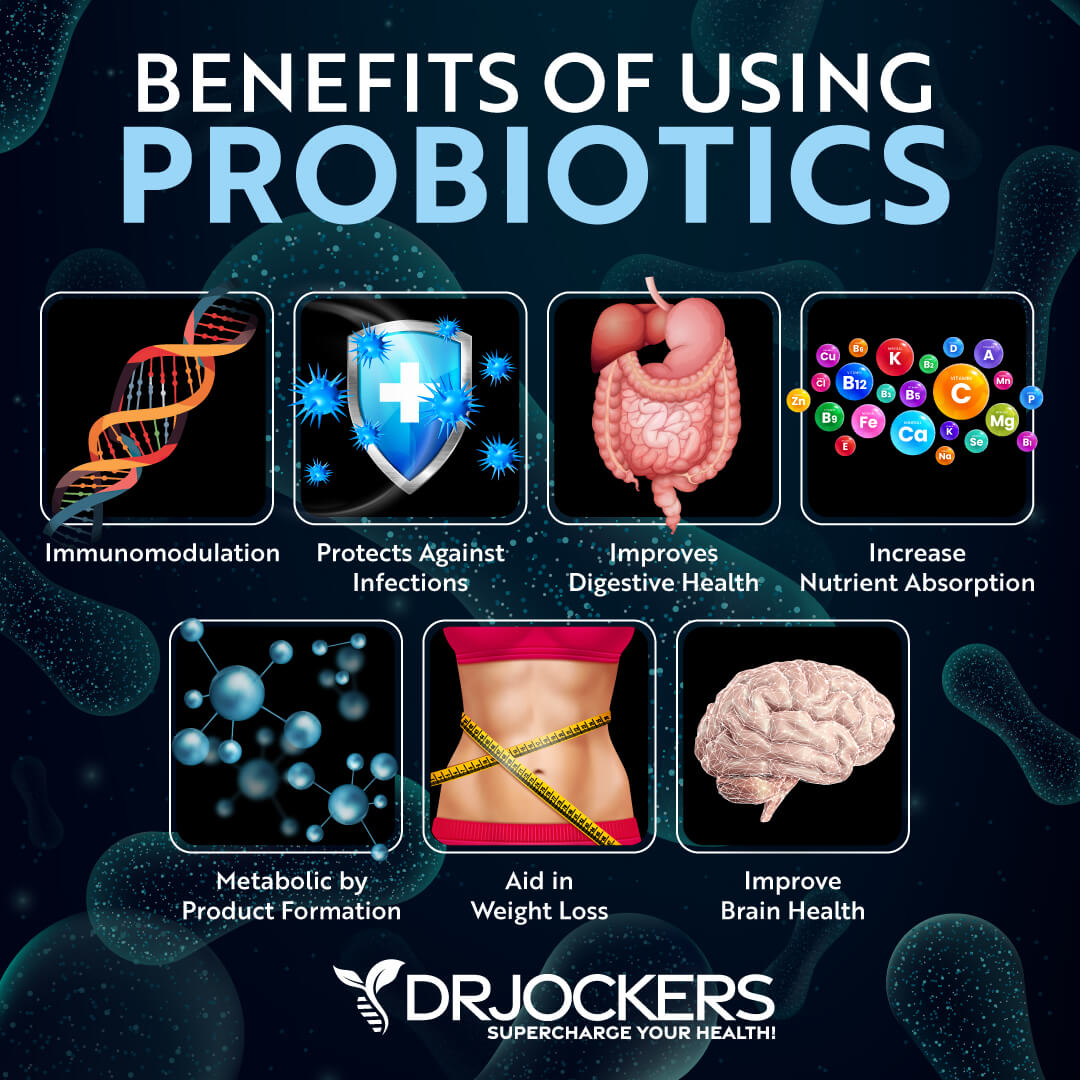
Probiotics:
Abnormal bacterial flora in the gut is associated with slowing colonic transit which increases the risk for stagnation of fecal matter in diverticula. Supplementing with live probiotics can support your immune system in fighting infection.
Taken regularly, probiotics can reduce gas, bloating, diarrhea, and constipation. When used in conjunction with anti-inflammatory agents, probiotic treatment resulted in the treatment of 100% of individuals in a study following 1 year. (13)
Digestive Enzymes:
Individuals with diverticulitis could use any extra help to improve digestive function. Enzymes enhance the ability for food to be metabolized and easily absorbed into the body.
To ease digestive disturbances, digestive enzymes help your gut function optimally and can include a multi-complex of enzymes such as protease, amylase, and lipase. I recommend Super D-Zyme to help support digestive health.
Aloe Vera:
Aloe vera is a potent medicinal plant used for enhancing detoxification pathways, modulating the immune response, and stimulating healthy gut function. Aloe vera extract inhibits pathogenic bacteria in the intestines thus encouraging regular bowel movements (19).
Aloe vera regulates pH and can relieve symptoms of both constipation and diarrhea associated with diverticulitis by decreasing inflammation in the gut (18). The aloe vera I personally use can be found here.

DGL (Deglycrrhizinated Licorice Extract):
DGL enhances digestive function by releasing secretin to thicken intestinal mucus. It is an adaptogenic herb that can heal gastric lining by reducing pathogenic bacteria and suppressing inflammatory responses. (23)
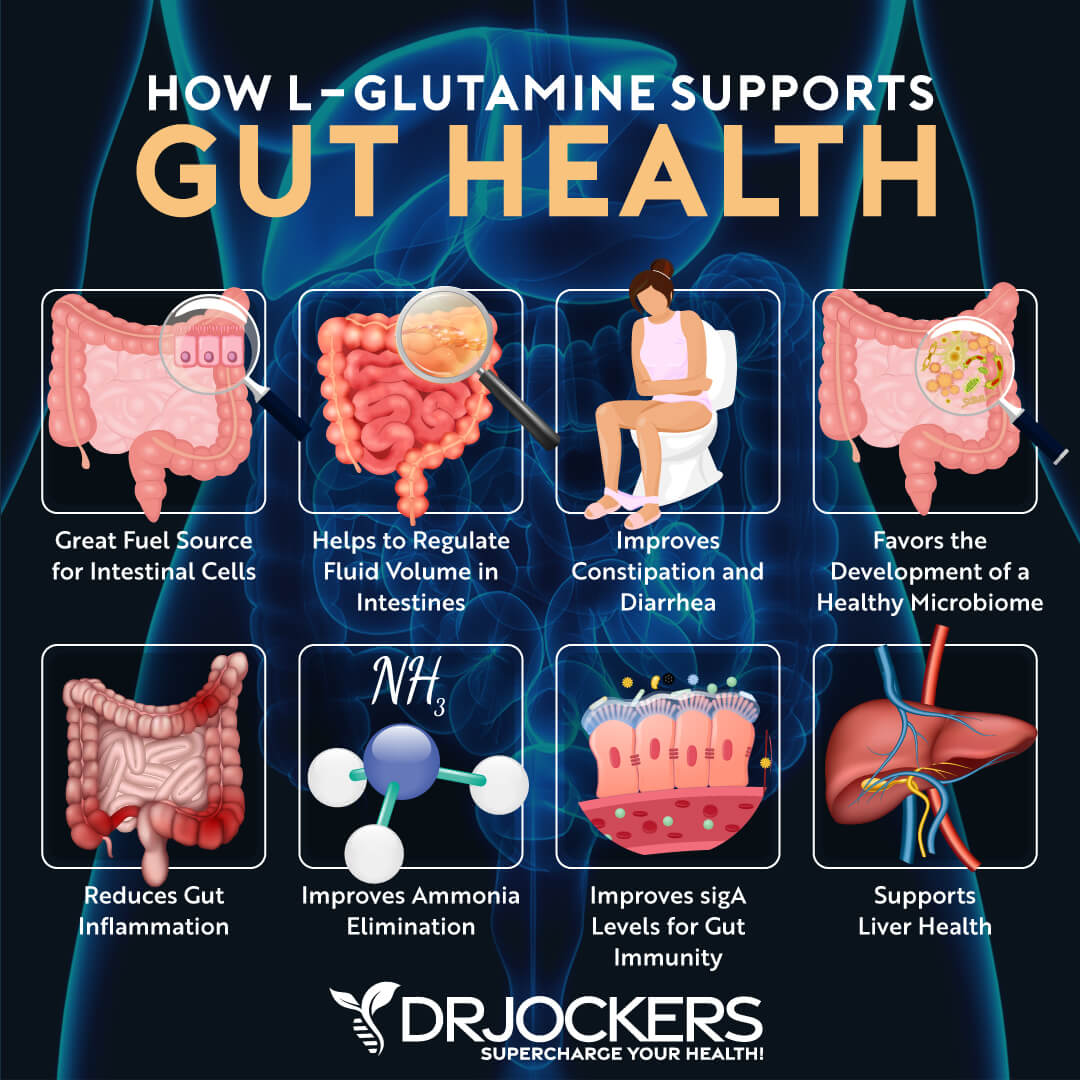
L-Glutamine:
Preserve your gut health with the essential amino acid, L-glutamine. The addition of L-glutamine into your diet can repair tissue damage and improve the mucosal lining that is needed to prevent the obstruction of fecal matter in diverticula.
L-glutamine can also reduce your food sensitivities by repairing gut problems associated with leaky gut. In addition, it reduces gut inflammation and supports the healing of the intestinal cells (20, 21).
Gut Repair Supplement:
Consider supplementing your diet with Gut Repair which combines aloe vera, DGL, and L-glutamine with other essential nutrients identified in improving colon health. The powerful impact of these nutrients works to heal your digestive tract by soothing the intestinal membrane, enhancing gut flora, and reducing inflammation.
This supplement is not currently FDA-approved to prevent, mitigate, treat or cure diverticulitis and should not be confused as such. With that said, this is a fantastic supplement to support and soothe your digestive system.
4) Lifestyle Strategies
These lifestyle strategies are critical to supporting your digestive health and reducing the risk of diverticulitis problems in the future. Be sure to put these all into action daily to keep your bowels healthy and strong.
Reduce Stress and Move Your Body:
The vagus nerve which runs from the brain to the gut is responsible for the secretion of stress and inflammatory hormones like cortisol and histamine into the gut. Therefore, stress directly contributes to the inflammation of the gut and strain on the immune system which can cause flare-ups with diverticulitis. (7, 8)
Incorporating physical activity into your life can help alleviate stress emotionally and physically. Exercise decreases the circulating levels of the stress hormone cortisol in the body, and increases oxygen flow to cells improving circulation and natural detoxification pathways. Studies show that exercise improves regularity and reduces pain. (6)

Consuming The Right Amount of Fiber:
Eating fiber-rich foods promotes regularity by acting as a cleaning agent for the digestive tract. Although harder to digest, raw fibrous foods like celery, carrots, and apples contain enzymes that support digestion. Some of these foods can be challenging on people with diverticulitis.
However, other forms like avocados, artichokes, jicama, bananas, and steamed broccoli and cauliflower may be easier on the digestive tract and can help eliminate your reliance on taking laxatives that can cause harm (4, 5).
Individuals who consume a plant-based diet have been found to carry fewer toxic agents in the gut microflora than those who primarily eat meat (6). For some individuals they do better with more fiber while others need less. Try to find the right amount for your body.

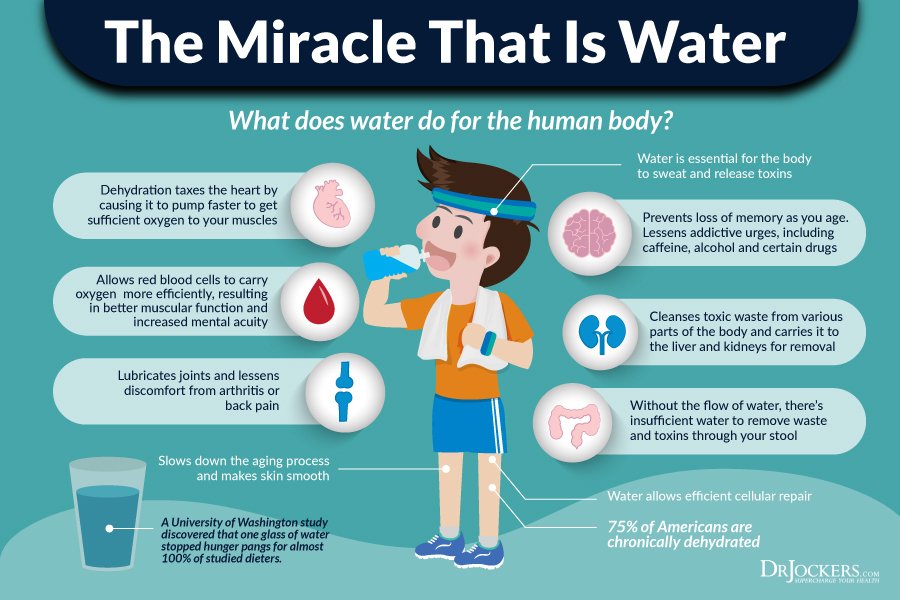
Optimal Hydration:
Decrease your alcohol and caffeinated beverage intake and swap them with purified water. Both alcohol and caffeine dehydrate the colon and alcohol can increase the accumulation of mucus in the colon contributing to infection.
Drink at least 1 gallon of water a day to super hydrate the digestive tract and add bulk to stool. Water also contributes to a healthy mucus barrier along the intestines for efficient waste elimination. The more fiber you consume, the more water you must consume as these work together to remove waste material from the body.
Healthy Bathroom Habits:
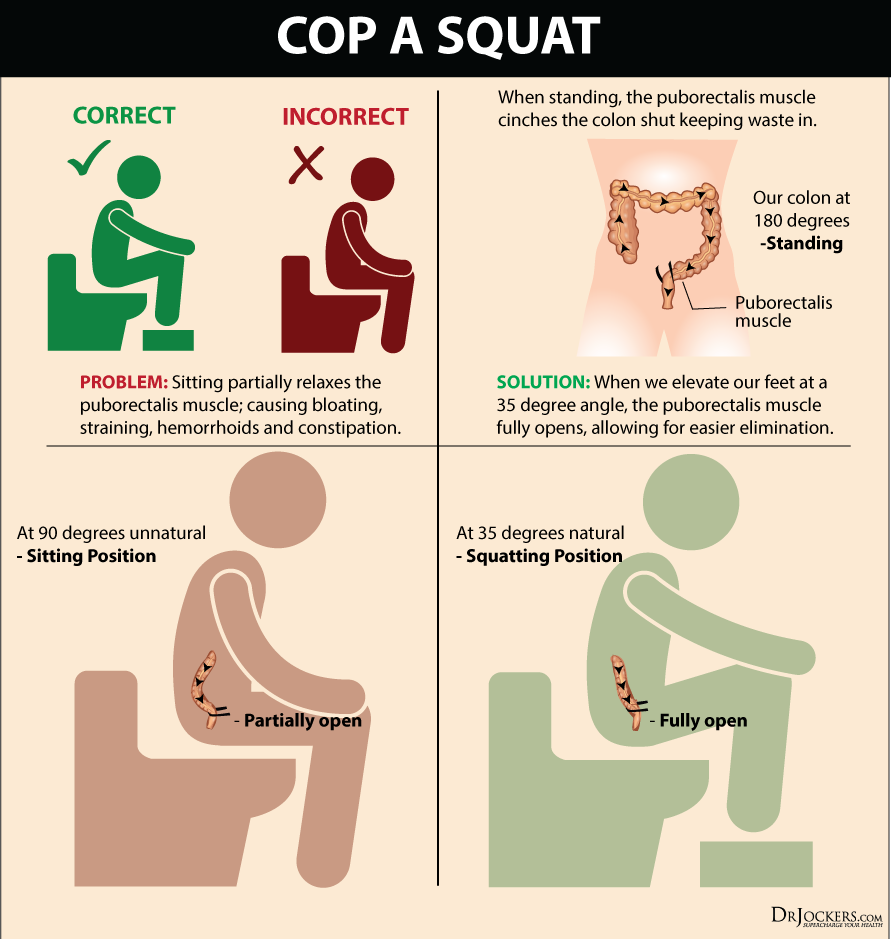
Avoid straining to go the bathroom which puts more pressure on the intestinal wall. Instead, use the toilet in a squatting position by placing your feet around the toilet or using a stool to lean forward relieving tension in the intestines.
When you do feel the urge to go, don’t hesitate to use the bathroom because holding it in encourages bacteria and toxins to be reabsorbed back into the gut and body.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!








I wish I had known this info in 2001. I had 9 inches of my gut taken out due to diverticulitis. Had troble for years afer the surgery. Doctors never told me about natural cures . The hipocratic oath went out the window in my case.
So sorry to hear about this Ronnie! Please pass this article on so others will know what to do!!
I WAS VERY IMPRESSED WITH YOUR CLEAR ,INFORMATIVE VIOEO ON TREATING DIVERTICULITIS….I AM 74 & HAVE BEEN DIAGNOSED WITH DIVERTICULITIS..I AM A UK RETIREE LIVING IN PUERTO VIEJO COSTA RICA…I AM UNABLE TO SOURCE MOST OF YOUR RECOMENDED FOOD SUPLIMENTS HERE…HOWEVER THEIR IS AN ABUNDANCE OF NATURAL ORGANIC FOODS…PLEASE RECOMEND BEST D.I.Y.USE OF NATURAL WHOLE PLANT..VEGITABLE AVAILABLE..REGARDS PETER
Thank you Peter! I mention some of the top foods above in the article. You may also want to try an AutoImmune Elimination Program: https://drjockers.com/autoimmune-elimination-program/
Blessings!
Dr. Jockers, I had 6″ of my Colon Cut out 4 months after I retired from a 22 year career in law Enforcement. I’ve had my good days and days where I thought I’d have to drive myself to the ER. This last flare up had me on the toilet for 3 days of continuous blood in my stools. I’ll follow your plan and see if i can get my colon back to normal.
So sorry to hear this!! Praying you get fast results Gary!! Be Blessed!
Firstly, is it actually possible to cure diverticulitis? I had a colonoscopy recently and I was told I have a few small areas of diverticulitis. Will the “pockets” actually go away?
I have read about the 4 steps. I am not sure exactly where to start. Should I start with an elimination diet? Or should I start with simply removing gut irritating foods?or should I start with adding gut soothing foods? And how long should I do one of these before starting the next?
And at what stage do I add in the gut healing supplements? And do I need to take them all?
And what about the fibre rich diet? Do I do that too?
I find the structure and order of things here hard to follow.
These are excellent questions, and I have the same ones, particularly how many supplements to take and for how long. Seven supplement pills a day seems like a lot.
Some simple answers to the questions above would be very helpful.
An elimination diet (which eliminates common gut irritating foods) along with gut healing nutrition, supplements, and lifestyle strategies. It is best done altogether. Our digestive health restoration program details a full protocol: https://drjockers.com/the-digestive-health-restoration-program/
I’ve been dealing with this disease for 15 years +. I’ve been thinking of selective surgery before it gets any worse.I would like to try a natural way first. I have been doing some of the stuff listed in this article, but with no specific plan.
Hey Dennis, it could be helpful to work with one of our coaches to help you put together a plan! You can get in touch with Michael at michael@drjockers.com if you are interested or have any specific questions!
I’m 35 and have been dealing with it for a couple years now. Thanks for this info! Do you know if it’s common for someone my age? I also don’t have a gallbladder
Hey Lauren, unfortunately these kinds of issues are becoming common for people of all ages! Blessings!
Hello..was just diagnosed with diverticulitis..An acute one that came on like nothing..Im on 2 antibiotics and no appetite so i hve to force myself to eat something so i can take the pills..And still hve diarrhea..Will i get it again wen the flare up goes away with the antibiotics? This is so new to me..Being that its my first time having it i am kinda scared..
Most likely Sarah. If the conditions in your body that caused the flare up to occur are not addressed, then it will likely continue to occur. I would recommend following the information in this article! You can also email michael@drjockers.com if you would like to work on a coaching plan for this!
you really should but suggest that flare ups of divuticulitis could be caused by low fiber diet….Try HIGH fiber such as nuts!
Yes getting adequate fiber is important, however, nuts are very irritating to the gut and I would not recommend them for diverticulits. Better to get your fiber from vegetables like avocado and steamed cruciferous veggies.
Gracias so much!!! … tengo diveritculitis, no tengo Gallbladder, mi propio cuerpo rechaza muchos de los alimentos que le molestan pero hasta que no me eduque en el tema no comprendía lo que mi inside me decía …mucha disciplina es necesaria, para no comer nada que es irritable, y siempre siempre vivir con el probaotico del colon, hay que buscar la forma de encontrar el balance correcto que es diferente en cada individuo, pero todo lo que usted a escrito es la única forma de vivir con este padecer .. muchas veces cuando me he sentido bien y no sabia que tenia diverticulitis, me he alejado de la dieta y el tratamiento y en muy poco tiempo la crisis a regresado, pero ahora que se lo que tengo y lo malo de vivir en Crisis .. seré mas disciplinada .. Gracias, Gracias !!!!!
What else do you recommend to get fiber. Cannot eat alot of the cruciferous vegetables, or spinach, due to Hashimoto’s Thyroiditis. And must also stay gluten free due to Hashi’s as well ! This makes it very hard to find things to make up for what I cannot consume. Use Flaxseed and eat alot of salad with romaine and butter lettuce, this is about all I can think of!
Hey C, You should be okay with cruciferous veggies as long as you lightly steam them. Here is a helpful article: https://drjockers.com/hypothyroidism-nutrition-plan/
The info was clear and concise…thanks!
Thanks for reading Thelma!
I’m a very healthy young looking 80 years old woman struggling with Diverticulitis for years. I refuse to take antibiotics for a couple of years now.
I know now that stress brings the attacks on.
I read it all and found a lot of good information.
Questions. Coconut water good. Or is it only coconut water kefir?
And was the Leaky Gut video for Diverticulitis?
Thank You, Carole
Hey Carole, coconut water tends to be high in sugar which may not be good for people with diverticulitis. Kefir is fermented and will be lower in sugar. Also, the leaky gut video information will definitely be helpful for you!
Dr Jockers, I have had diverticulitis and duodinitis before. I have managed to overcome both by following a gluten free low carb diet and one of the big helps is coconut water! I use the kind that has no added sugar! It has helped me to be relieved of the pain of diverticulitis and cured my psoriasis of 50 years!
Great to hear that Pamela!
Great info. However the majority of the food you recommend for healing the gut (fermented food) is definitely not recommended for people suffering from high histamine and mast cell disorder. So what can be done to find a good set of foods to help healing if you are suffering from high histamine?
Thanks for your help
Hey Mary, this article has some good information and includes a histamine shopping guide: https://drjockers.com/suffering-histamine-intolerance/ referencing both articles, you should be able to pinpoint the best foods for you!
I was diagnosed with diverticulitis the last week in March. Since having my youngest daughter 16 years ago I developed an intolerance to lactose, and my body was never the same (just for a little background).
When I started eating again I was very scared and unsure of what would bring on another flare up. I have since been adopting more of the vegan lifestyle and have been enjoying it. I’m still really nervous about what to eat, and if this is the best path to take.
My digestive tract seems to agree with it. I currently have purchased most of my meals i.e. Beyond meat, Gardein, fruit (bananas, cantaloupe, papaya), white rice, white bread. I don’t know which veggies to start with because most green vegetables make me very gassy, which I’m scared of.
Can you please advise because I’ve always been a big vegetable eater, now I’m scared of it.
Thanks,
Patricia
Hey Patricia! Glad to hear you are feeling better on a vegan diet, I am not a huge fan of the processed meat replacements. Maybe try out some of the information outlined in this article: https://drjockers.com/follow-vegan-ketogenic-diet/
Hi….I just got out of the hospital – I had a major bleed for 5 days where I required blood transfusions. I have had diver for over 30 years and I EAT CLEAN! Everything you suggest, I’ve done for years. I have NEVER experienced anything like this. I had no pain just a severe bleed. They never found out exactly where the bleed started but told me that surgery is my last resort and it looks the same all the way through. They sent me home with a weeks worth of Pantoprazole and I started a probiotic. I wasn’t sore before, but I certainly am now and terrified to eat. Do you have any suggestions as I really do not want to go through this again?
Hey Rebecca, sorry to hear about this. Water or bone broth fasting may be something to consider. Email michael@drjockers.com for more information!
I am 70 years old, female, who thought she was managing osteoarthrits pain successfully. Under a Dr’s care for 5 years, been taking tramadol & ibprophen while maintaining a healthy weight, daily exercise and healthy food choices to include, protien, carbs, fats & fiber. SURPRISE! Now abdominal pain, constipation, pain during bm
sent me to Internist where diagnosed with Diverticulitis. Put me on amoxicillin 8 days, liquid diet, soft carbs, etc. While resting read everything I could find on how to treat this disease naturally.
Came accross YOU! Now going to follow you program and hope for improvement. I will start to wean off 5 years of tramadol 300 mg per day for neck & hand pain, switched from ibprophen to acetaminophen. Ab pain still exists upon awakening but, improved since anti-biotics, diet change, etc. I am ready now for a complete makeover that is natural and holistic! Thank you for reading this and I remain positive and hopeful I can heal myself outside of traditional meds. Patti Rosencrantz
You can do this Patti!! Thanks for reading!
I have been dealing with diverticulitis for years (I’m 66). I follow your reccomended suppliment and food protocol but I’m now in the grip of a full blown infection (lower left quadrant pain, low grade fever, nausea, gas,
chills…yeah…the whole shebang) going on 24 hours. I’m fasting, drinking ginger water, aloe vera juice, bentonite clay (liquid), probiotics. I don’t want to take (Cipro) antibiotics, but how long do I let this infection go on before I consider it?
Hi Lynda, I had the same scenario a year ago, so bad I couldn’t raise my left knee/ hip to go upstairs because inflammation affected hip. In desperation( I was in Spain so didn’t know any alternative health guys) I googled the best homeopathic remedy for Diverticulitis flare up. Nux Vomica 30 strength was suggested. Within 24 hours the pain was reduced to 20% and by next day totally gone. Along with homeopathic Sulphur which I take effectively for topical thrush or skin yeast infection caused by gut. Both these remedies work well for me. When I got back yo UK, my homeopath said she always recommends Nux vomica for bowel issues. She also suggested supplementing with Milk Thistle tincture to help my liver help my digestion. It’s proved useful in regulating bowel movements. It’s detox though so start small doses and see what works for you. Antibiotics are probably the worst thing you can take as they kill off the good gut bacteria though not always the bad guys. I hope this helps. Many blessings, Earth or angelic whichever works :-}. This is a great website and source of infornmation. Thank you Dr Jocker
Great to hear you got results!! Be Blessed my friend!
Thank you for this very informative article, Dr. Jockers. I didn’t see an answer in the comments above regarding healing diverticula (if there was one, so sorry I missed it); is it possible to get rid of them altogether (maybe with cabbage juice or something)?
Many thanks!
There have been some cases in which the diverticula have healed Christi but not always! Oftentimes, maintaining a healthy lifestyle can keep flare ups away.
Hi Dr Jockers: I’ve been have stomach issues for a while now and it turns out that I have Diverticulitis I was in the hospital for a few days and I still get the flare ups from time to time I am scared to eat anything because of my flare ups I know you said to fast for a few days and I do that but after I fast I still have flare ups should I just have the problem resolved by having surgery done to remove the infected pouches?
I would not recommend surgery as a first option Angela. There are many factors to consider here including food sensitivities, your microbiome, potential parasitic infections, keeping the diverticula as clear as possible, etc. This is a health challenge I would highly recommend working with one of our coaches on. You can reach out to michael@drjockers.com if you would like more insight on this!
Thank you, this is one of the best articles I have come across and I have read lots of them. I see a naturopath regularly now since June and have been advised of most of this but still so much to learn. Between this and my nerve pain, osteoporosis and osteo- arthritis my diet has changed significantly. I am a big fan of natural methods so try not to take too many prescriptions other than my weekly osteoporosis one and daily nerve pain pills. Everything else is either natural or supplements suggested by my naturopath. Sometimes it is difficult to have good meals without the dairy, egg, wheat and barley already on my list so always trying recipes from internet. Hope to gain some weight back soon but haven’t lost anymore since I changed my diet in June at least. For everyone out there, it takes time and patience to eat well and get used to this. I am going to stick with it as long as it takes.
Thank you for sharing that Bonnie!
So comprehensive, thank you so much!! Bookmarked and will be using it to remind me what to do.
Great to hear this Linda!! Be Blessed!
I just want to encourage you all suffering from diverticulitis. I had struggled for about 4 years, and lost count of how many bouts I had over that period of time. Some of them I would be able to stop before it got out of control by going on clear liquid diet for a couple of days, then soft for a day or so. I felt so hopeless, and spent many hours researching online. Don’t expect medical community to help concerning preventative things. They know how they are taught to treat the infection once you have it. They tell you what not to eat, but not what you should eat instead. I was afraid to eat anything and wasn’t getting the nutrition I needed. I ended up getting a yeast infection through my whole body, and ended having to treat that with yet another pill. I had no healthy bacteria left after the antibiotics. You can turn this around, but you will have to change your lifestyle or it will most likely return. I didn’t want anything to do with a surgery that may or may not fix the issue. For years I wouldn’t eat corn, popcorn, nuts, seeds, spicey foods, and all the stuff we are told to avoid. Now I eat all of them and have no issues. You need to take 50-60 billion good quality refrigerated probiotic daily, reduce stress when you can, eat high fiber (fruits and veggies), keep bowels moving (1 rounded tbls in the evening of Metamucil), drink lots of water. Bragged apple cider vinegar is a healthy thing to incorporate as well. I took about 2 Tbls in 8 ounce glass of water daily. I also excercized 30 minutes, at least 3 days a week. You have to figure out what your triggers are. I know it’s a lot of changes for some of you, but the alternative is surgery. At least give it a try. It worked for me. Be encouraged……you can do this!
This is great advice! Thanks for sharing!!
Hi Kathy,
The information that you shared was very helpful for me. Do you mind sending me an email so that we can converse more of what I’ve been experiencing?tiffanycobb.tc@gmail.com
Hi Kathy,
Thanks for the information. It is very helpful. My first episode happened in 2009 and then again 3 months later at which time my doctor suggested surgery and I had 9 inches of my colon removed. I recently had another episode and was put on antibiotics. I am trying to research natural remedies that will help in preventing another episode.
Thanks again for the information.
Thanks for the interesting article Dr. Jockers! I’m 42, healthy (active, good weight) and already have had two episodes of diverticulitis over the past 4 years. Beyond that, my main issues are bloating, constipation, and acidic/burning sensations in lower and upper abdomen. Much of the advice I get revolves around a low FODMAP elimination diet. However some of the foods you mention as healthy for rebalancing gut may be high FODMAPS. Any advice on what is best regarding the FODMAP craze vs your advice here? I want to prevent another attack obviously so want to choose the best method. I also suffer from moderate bouts of GERD and some foods from both approaches seem to cause acid reflux/indigestion. Another question: are underlying acid issues a precursor for diverticulitis episodes? Thanks so much!
That is a good question. Some individuals do great on a low-FODMAP, while others do better eating a higher FODMAP. You have to find what works best for you. You should give each a try for 2 weeks and see which helps improve your symptoms. Yes, low stomach acid is a major risk factor for developing diverticulits. https://drjockers.com/beat-acid-reflux-naturally/
Thanks so much!!
I am recovering from a 2 week out colon surgery and the list of foods I can have are all white foods, dairy, and sweet items. These are the foods I have been avoiding for years due to my diverticulitis. Would you please suggest the foods that will heal my colon and help my colon heal in place of these. Thank you!
Yes I would recommend the foods discussed in this article above. Praying for fast healing!
Thanks for your comments.
Hi Doctor, I found this to be a really great article. I am 30 years old and used to have great digestion, although I don’t think my diet was particularly healthy and included a lot of fast food. Around 5 months ago I had what turned out to be a diverticulitis attack with the complication of a perforation. Around 2 months later this re-occurred and I went on a low residue diet. Around 2 months after this, the diverticulitis was back again. CT scan showed that the perforation had healed, but one large bothersome diverticula was still getting inflamed. It now looks like I will be receiving surgery for this and am on a waiting list in the UK. I used to be a very active person but have recently been very stressed with my first son who is now 1 years old. Having been on a low residue diet for 6 weeks after each attack ,I have barely had a chance to try a healthy high fiber diet. What would you recommend? I am desperate to avoid surgery but it might be my only option. Many thanks
So sorry to hear this! I would recommend working with a functional health practitioner to get to the root cause: https://drjockers.com/functional-nutrition-tips-to-find-a-great-health-coach/
great article. i’m a 72 year old active woman with diverticulosis. I’ve had an emotionally stressful life like most, but i’m a caregiver to my husband several years my senior. the other night I ate a large salad with cucumbers, cherry tomatoes, lettuce and avocado and by night time I was in agony with cramping and bloating. I have several food allergies that are slight, like cucumbers. could that have been my trigger? also, I drink organic beet juice daily for nitric oxide and the water from BM was pink. was that blood, or beet juice? i’m fine now, eating things easy to digest. also, on May 7, i’m having hip replacement surgery. ugh. would this be a factor? thank you so much.
Hi Nan, It is normal for urine to be red or pink from beet pigment following consumption. Many healthy foods can be triggers for individuals with diverticulitis. Read this article for more information: https://drjockers.com/beat-digestive-problems-low-fodmap-plan/
My magic formula to get rid of Diverticulitis in 1 to 3 days.
1. No nuts, seeds or corn.
2. Pepto-Bismol or other brand 2x day.
3. ¼ of a pill, any of antibiotic you have.
4. Juice 2 carrots and Cabbage ¼ head 3x a day.
5. 1 Zantac per day.
6. Tylenol for pain if required.
Hey Jim, Thanks for sharing! Taking these medications during a flare up may help treat the symptoms but it is the conditions that are causing the flare up that won’t be addressed and re-occur. The steps above can help your gut heal. Blessings!
I had an abscess on my bowel with the pockets of fat dotted around the outside and had an operation to get rid, I lost weight and looked healthily for the first time in years
However I soon put the weight back on and I’m now back where I was prior to the op iv always liked chip shop teas and kebabs which I know cant have done me any favours. Think I’ll trysoem of your ideas above. Thanks
Hey George, Yes, the strategies above can help you!
Diverticulitis
Hi Dr. Jockeys, this is really helpful information to me. Quick question: I have diverticulitis uncomplicated of the ascending colon and I’ve only had one episode recently in my entire life and recovering from it has been difficult because I can’t seem to introduce fiber slow enough in a way that doesn’t cause pretty significant irritation. I overdid drinking coconut water and over hydrated and it actually pushed me towards shedding some of the lining of my colon.! Do you have any recommendations for how to slowly re-introduce fiber into my diet?
Sorry to hear this Doug! I would be sure to slowly reintroduce and see which types you respond best too.
Thank you Dr Jockers
SO IF YOU CANT DO CARBS OR EGGS WHAT A GOOD BREAKFAST TO EAT
You can make a protein shake with coconut milk, 1/2 avocado, berries and protein powder!
Tomorrow, Oct. 5, 2020 I have a colonoscopy.
Six years I was told I hade Diverticulosis. I found out about your Ketogenics about four years ago, so we’ll see.
My question is this; what best should I do after to clear this “drink” out of my system?
Thank you Sir,
Judy 🙂
Hey Judy, yes I would recommend doing a liver cleanse. https://drjockers.com/liver-cleanse/
If you can only do one product, I would recommend the Gut Healing Protein in shakes to help cleanse. https://store.drjockers.com/products/gi-cleanse-protein?_pos=1&_sid=9d8b7083c&_ss=r
What can I substitute for fermented drinks & food. I get a bad headache almost immediately when I consume a 1/4t. of something–not a good feeling. You also listed protein powders but everyone I have checked contains “natural flavor” of some kind. It affects me like other excitotoxins I have headache issues with. I have massive food sensitivities after being put on a couple rounds of cipro for an infection I didn’t have years ago. I’ve tried healing myself but not successfully.
Can you help with some suggestions.
Thank You!
Hello Sus, you most likely are reacting to histamine. Here is a helpful article for you: https://drjockers.com/suffering-histamine-intolerance/