 Stomach Cancer: Symptoms, Causes, and Support Strategies
Stomach Cancer: Symptoms, Causes, and Support Strategies
Stomach cancer or gastric cancer is a type of cancer that affects your stomach. It happens when cancer cells start to grow and spread in your stomach. Stomach cancer is also referred to as gastric cancer.
Unfortunately, stomach cancer doesn’t usually have any symptoms during the early stages. Most stomach cancer cases are caught at a more advanced stage after symptoms appear. This makes treatment more difficult. Thus supporting your body naturally becomes more important.
In this article, you will learn what stomach cancer is. You will understand the symptoms of stomach cancer. You will learn about the types of stomach cancer. I will go over the risk factors for stomach cancer. You will learn about the diagnosis process and conventional treatment options for stomach cancer. I will discuss the functional root cause factors for stomach cancer. Finally, I will offer my top natural support strategies to improve your health and well-being.
What Is Stomach Cancer
Your stomach is a sac-like organ in your abdomen. It plays a critical role in your digestive system. After you chew your food, it moves into your esophagus, a long tube inside your throat and chest. Your esophagus connects with your stomach at the gastroesophageal (GE) junction right under your diaphragm. Through your esophagus, food can move into your stomach, where digestion continues. Your stomach produces gastric juices to digest food before it can move into your duodenum and small intestine (1).
Stomach cancer is also referred to as gastric cancer. It is just one form of cancer that affects a digestive organ inside your abdomen. Stomach cancer happens when cancer cells begin to grow inside your stomach. Stomach cancer affects your stomach.
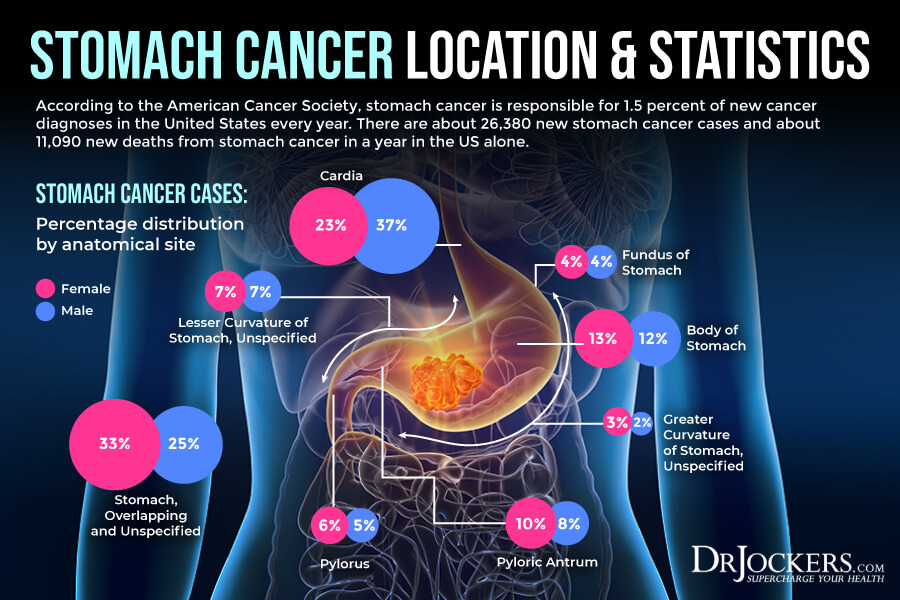
Your stomach has 5 parts, 3 within the proximal stomach and 2 within your distal stomach. The proximal stomach is the area where your stomach creates acid and the digestive enzyme, pepsin, to make gastric juice for digestion. This is where the intrinsic factor is made, which is a protein necessary for vitamin B12 absorption. The distal portion is where food mixes with gastric juice and then releases into your small intestine (1).
Parts of your proximal stomach include:
- Cardia: The cardia is the first section of your proximal stomach located the closest to your esophagus.
- Fundus: The fundus is the upper portion of your stomach found next to the cardia.
- Body (corpus): The corpus is the main section of your stomach, right between the upper and lower portions.
Parts of your distal stomach include:
- Antrum: The antrum is the lower portion of your stomach near the small intestine and serves as a place to mix food with gastric juices for digestion.
- Pylorus: The pylorus is the last portion of your stomach with a valve to allow emptying into your small intestine.
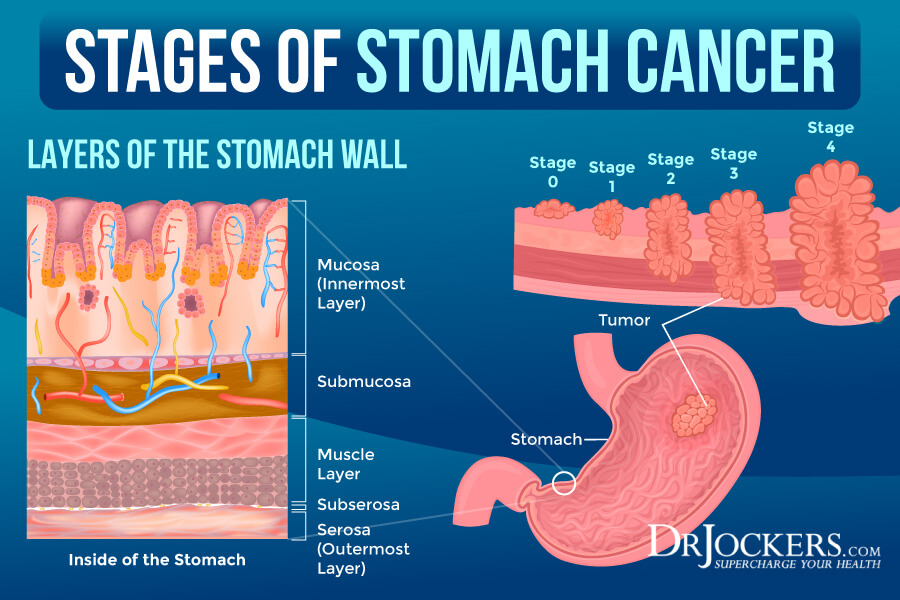
Stomach cancer may also affect your stomach wall. Understanding what part of your stomach wall is affected by stomach cancer is necessary for staging. Your stomach wall has 5 layers:
- Mucosa: The mucosa is the innermost layer of your stomach wall where digestive enzymes and stomach acid are created. This is also the area where stomach cancer may start.
- Submucosa: The submucosa is a supporting layer next to the mucosa.
- Muscularis propria: The muscularis prorpia, is on the other side of the submucosa. It is a thick muscle layer that supports mixing and moving what’s inside your stomach.
- Subserosa: Subserosa is one of the outer layers of your stomach wall.
- Serosa: The serosa is the outermost layer of your stomach that wraps and protects it.
According to the American Cancer Society, stomach cancer is responsible for 1.5 percent of new cancer diagnoses in the United States every year (2). There are about 26,380 new stomach cancer cases (15,900 men and 10,480 women) and about 11,090 new deaths (6,690 men and 4,400 women) from stomach cancer in a year in the US alone (2).
Symptoms, treatment options, and the outlook of stomach cancer may differ from other gastrointestinal cancers, such as colorectal, small intestine, pancreatic, or liver cancer.
Stomach cancer may take years to develop. At first, it starts with pre-cancerous changes in the inner lining of your stomach. Unfortunately, these early pre-cancerous changes usually don’t result in symptoms and can go undetected until cancer develops, and more serious symptoms appear.
Stomach Cancer Symptoms
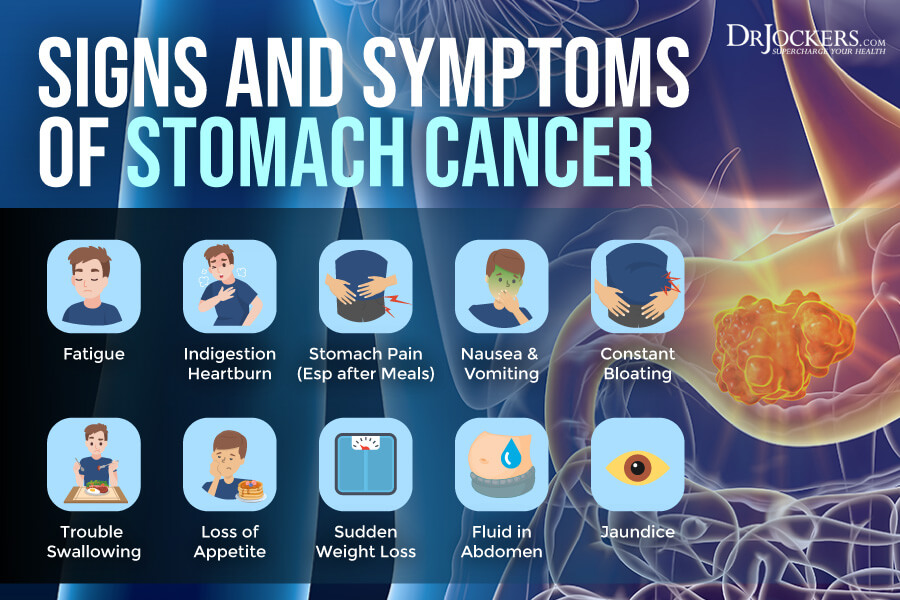
Unfortunately, there are generally no early signs and symptoms of stomach cancer, which means that early diagnosis is difficult. Most people get diagnosed with stomach cancer at a more advanced stage.
Signs and symptoms of more advanced stomach cancer may include (3):
- Fatigue
- Indigestion
- Nausea
- Vomiting
- Constant bloating
- Frequent heartburn
- Trouble swallowing
- Stomach pain, especially after meals
- Loss of appetite
- Feeling satiated from a small amount of food
- Sudden weight loss
- Fluid in the abdomen
- Bloody stool
- Jaundice
Types of Stomach Cancer
There are several types of cancer that may start in the stomach. However, if you are diagnosed with stomach cancer, in most cases, it means adenocarcinoma. Most information on symptoms, treatment, and research is also related to this form.
According to the American Cancer Society, about 90 to 95 percent of stomach cancer are adenocarcinomas (1). Adenocarcinomas start at the gland cells inside the mucosa. There are two types of adenocarcinomas: intestinal and diffuse type. Intestinal types of adenocarcinomas usually have a better outlook because targeted drug therapy may help to target certain gene changes from cancer. Diffuse types of adenocarcinomas usually grow and spread faster and are more difficult to treat and have a poorer prognosis than the diffuse type.
Other types of cancer that start and affect the stomach may include:
- Gastrointestinal stromal tumors (GISTs): GISTs start in the intestinal cells of Cajal found in the wall of your stomach. Some forms of GISTs are more likely to grow fast and spread into other parts of your body.
- Neuroendocrine tumors (NETs): NETs, including carcinoids, begin to develop in specific cells of your stomach that act like nerve cells or endocrine (hormone-making) cells. NETs are usually slower-moving cancer that generally doesn’t spread to other areas of your body, however, in some cases, they can grow and spread fast.
- Lymphomas: In some cases, lymphomas, which affect the lymphocytes of your immune system, may start to develop in the stomach wall.
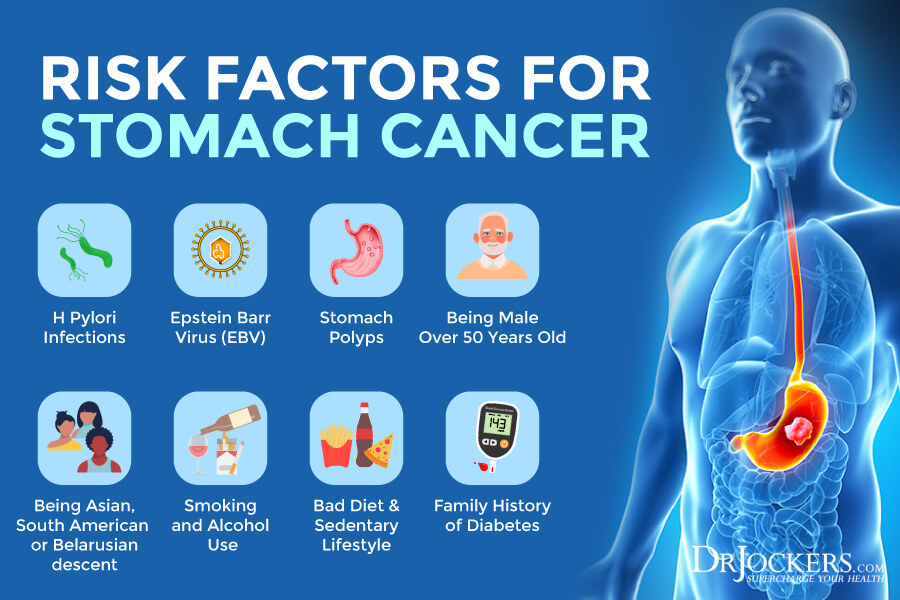
Risk Factors for Stomach Cancer
Certain risk factors that may increase your risk of developing stomach cancer may include (3):
- Lymphoma
- H. pylori infections
- Epstein-barr virus (EBV)
- Stomach polyps
- Tumors in other areas of your digestive system
- Being 50 or older
- Being male
- Smoking
- Being Asian (especially Korean or Japanese), South American, or Belarusian descent
- Family history of diabetes
- Having a sibling or parent with stomach cancer
- Eating too much salty food
- Eating too much overly processed food
- Eating too much meat
- Not cooking or storing food properly before eating
- Sedentary lifestyle
- History of alcohol abuse
Diagnosis and Conventional Treatments
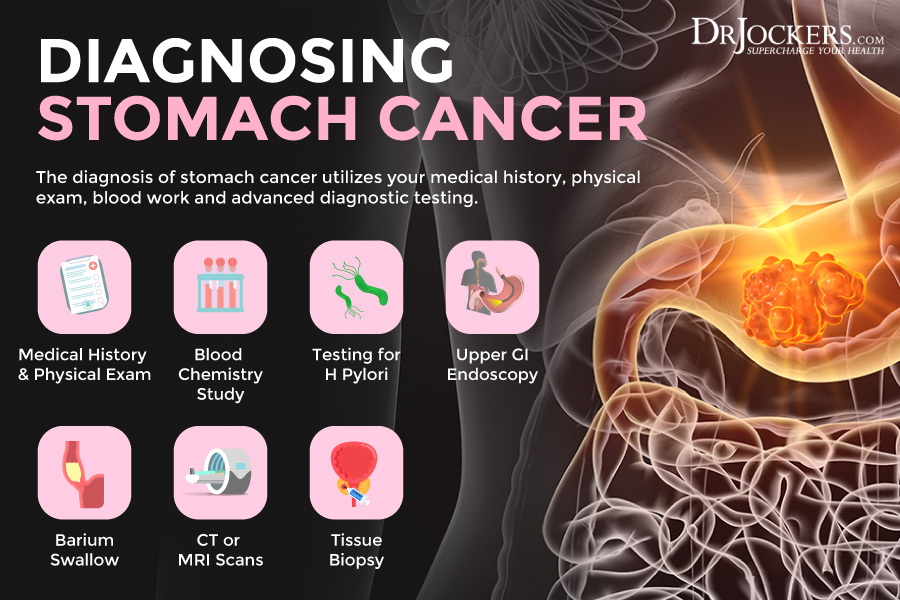
As I mentioned earlier, early diagnosis of stomach cancer is rare since the disease doesn’t have symptoms in the early stages. Stomach cancer is usually diagnosed at its more advanced stages.
Your doctor will go over your symptoms, health, and family history, and perform a physical exam to check for any abnormalities and issues. Next, they will likely order a blood test, including testing for H. pylori bacteria, complete blood count (CBC), and other blood chemistry studies. They will order other diagnostic tools to look for abnormalities and tumors in your stomach and esophagus, including upper gastrointestinal endoscopy, barium swallow, biopsy, x-rays, CT scans, or other imaging (3).
The treatment of stomach cancer depends on many factors, including the stage of cancer, health history, age, and overall health. Conventional treatment methods may include chemotherapy, radiation therapy, chemoradiation, targeted therapy, immunotherapy, and surgery. Left untreated, stomach cancer can spread to your liver, lungs, lymph nodes, and bones (3).
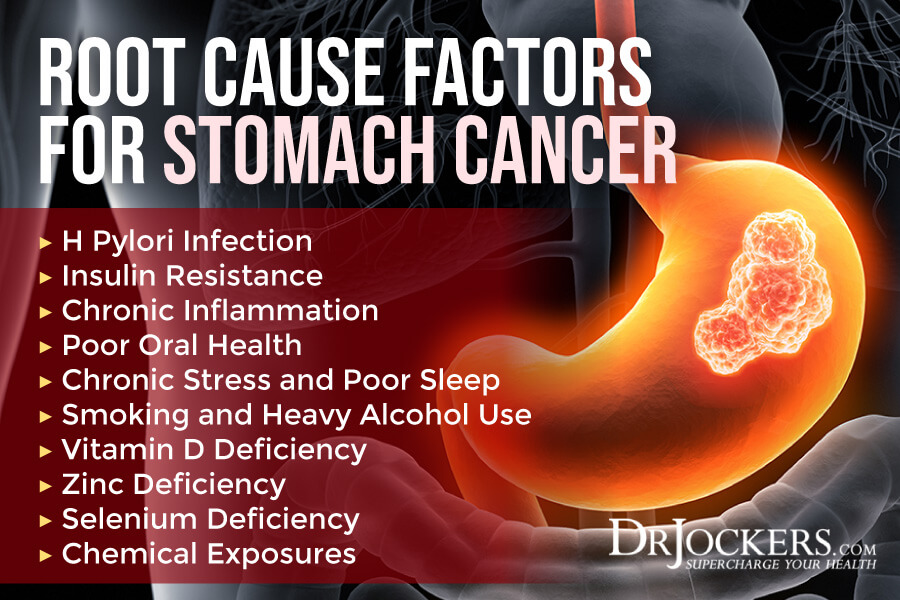
Functional Root Cause Factors
Understanding the risk factors of stomach cancer is important for prevention and treatment. However, understanding the functional root cause factors of stomach cancer is just as critical.
Functional root cause factors of stomach cancer may not directly cause stomach cancer but may lead to health issues and problems that may increase your risk of stomach cancer. Understanding the functional root cause factors for stomach cancer is critical for reducing your risk and supporting recovery from the disease. Here are the functional root case factors of stomach cancer:
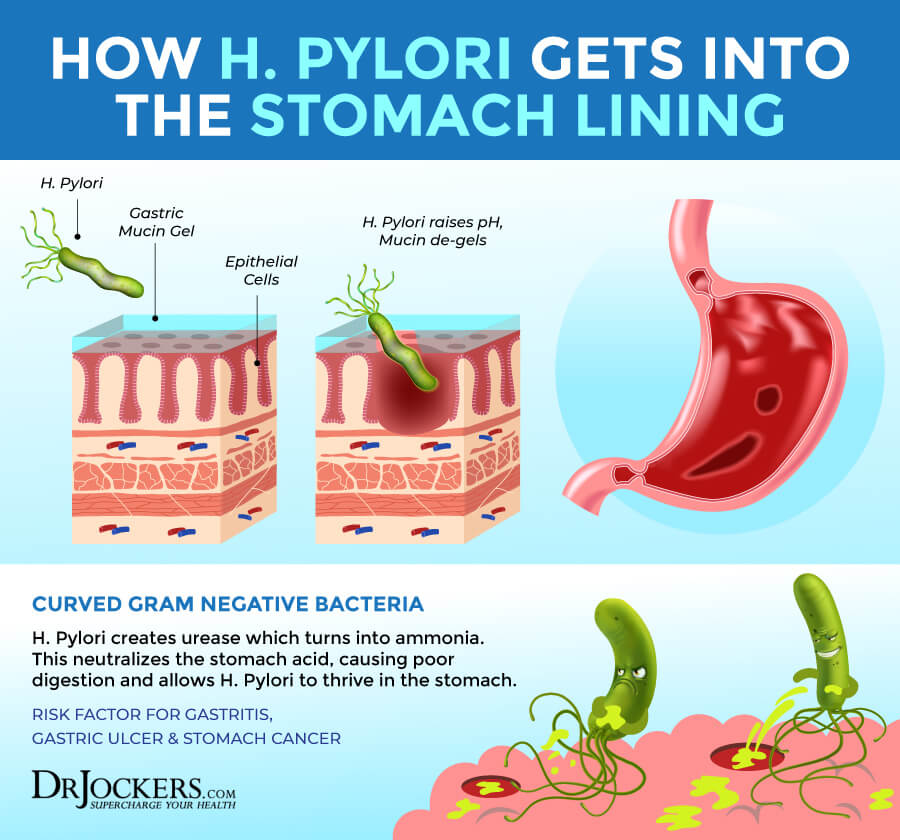
H Pylori Infection
Helicobacter pylori or H pylori is a type of bacteria that can affect your digestive system. H pylori infections may cause bloating, belching, gas, abdominal pain, vomiting, heartburn, and other digestive symptoms. It can increase the risk of ulcers in your stomach and small intestines. It may also increase the risk of stomach cancer.
A 2016 review published in Gastroenterology has found that eliminating H pylori infection may reduce the risk and incidence of stomach cancer (4). A 2020 large cohort study published in Gastroenterology has found that H pylori infection may increase the risk of stomach cancer (5). Researchers looked at 371,8813 patients with H pylori infection between 1994 and 2018 and looked at how many of them received the diagnosis of stomach cancer after an H pylori diagnosis.
Researchers found that participants who were smokers and/or were ethnic or racial minorities and males had a higher risk than non-smokers, females, and white male participants. Researchers found that addressing H pylori decreased the risk of stomach cancer in cases when H pylori were completely eradicated (5).
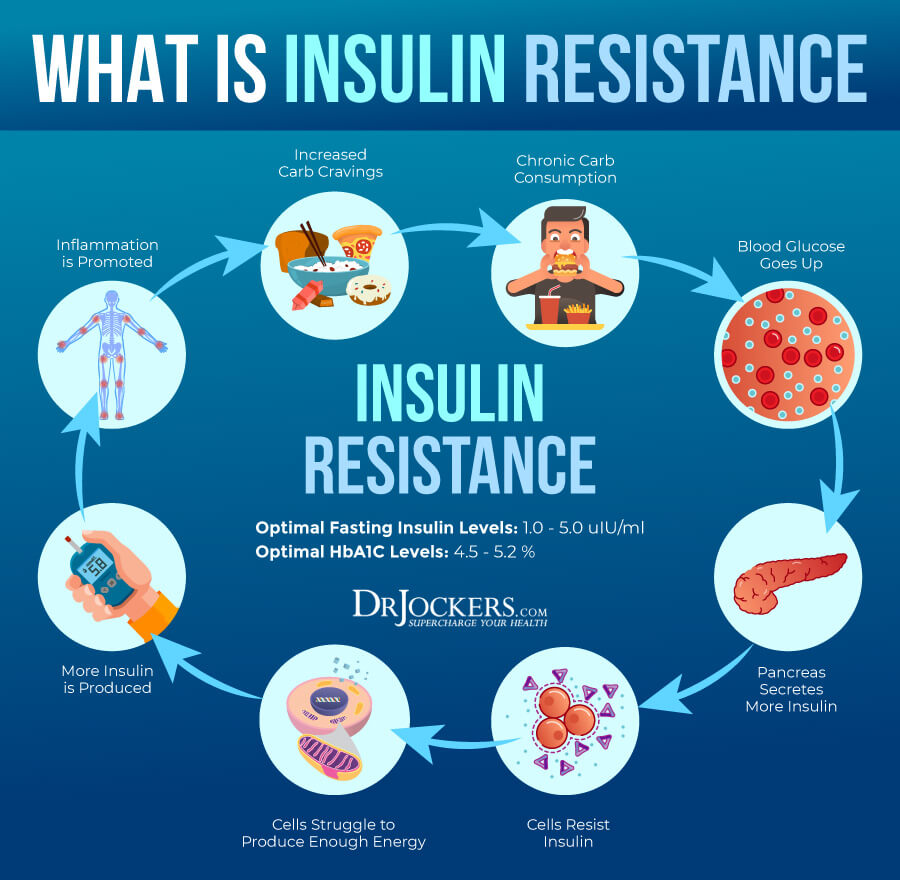
Insulin Resistance
Insulin is a hormone made by your pancreas. It helps to control the amount of glucose that gets into your bloodstream and helps to balance your blood glucose levels. Insulin resistance means that your body cannot respond to insulin properly and is unable to use blood glucose for energy.
When this happens, your pancreas will have to make more insulin. Over time, this will lead to increased blood sugar levels and blood sugar fluctuations. Insulin resistance may increase your risk of prediabetes and diabetes, but may also contribute to other health issues, including stomach cancer.
A 2015 public health center-based prospective study of 36,475 participants published in the International Journal of Cancer has found that increased insulin and C-peptide levels due to insulin resistance may increase the risk of stomach cancer (6). A 2019 prospective multicenter case-control study published in Gut and Liver has also found a link between insulin resistance and early signs of stomach cancer (7).

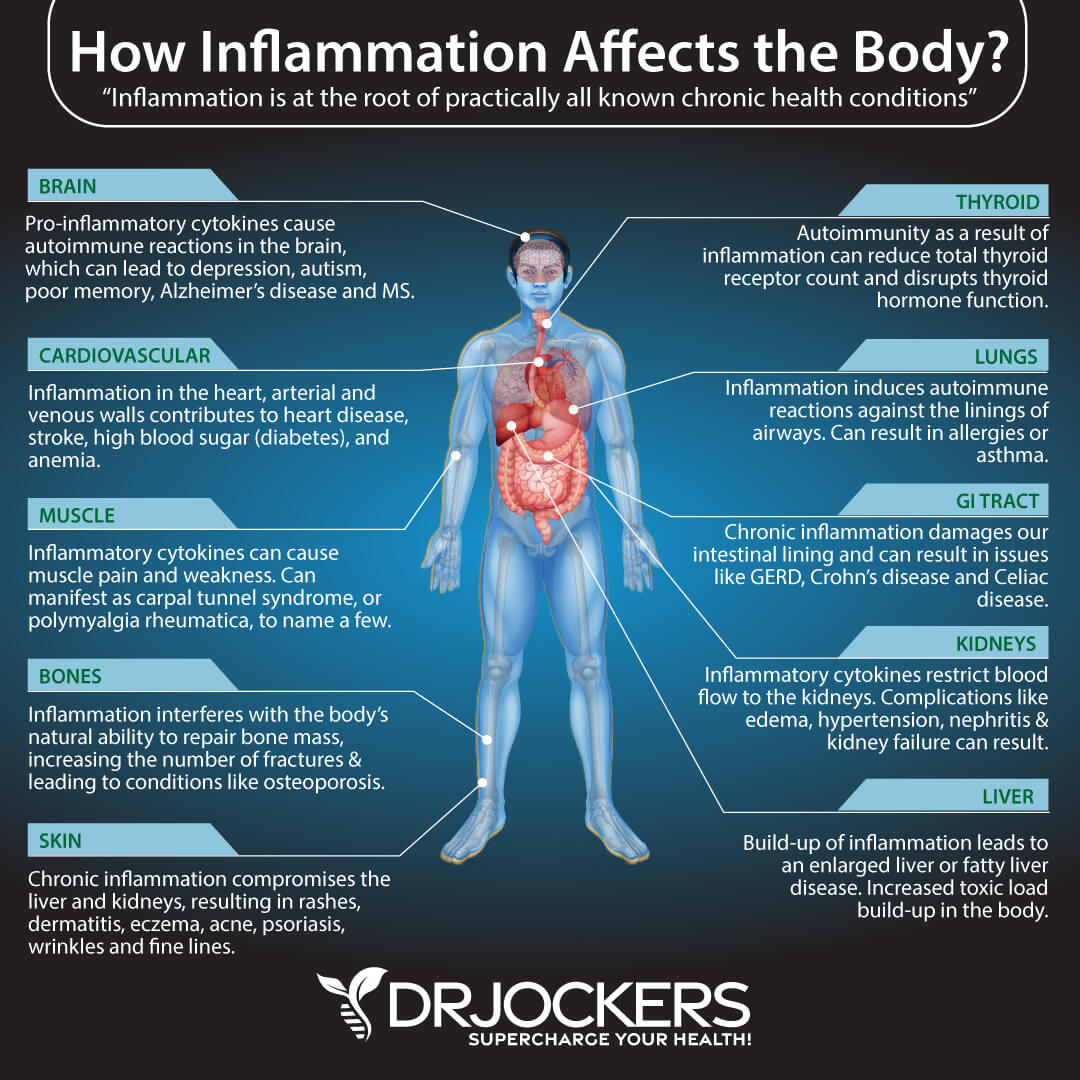
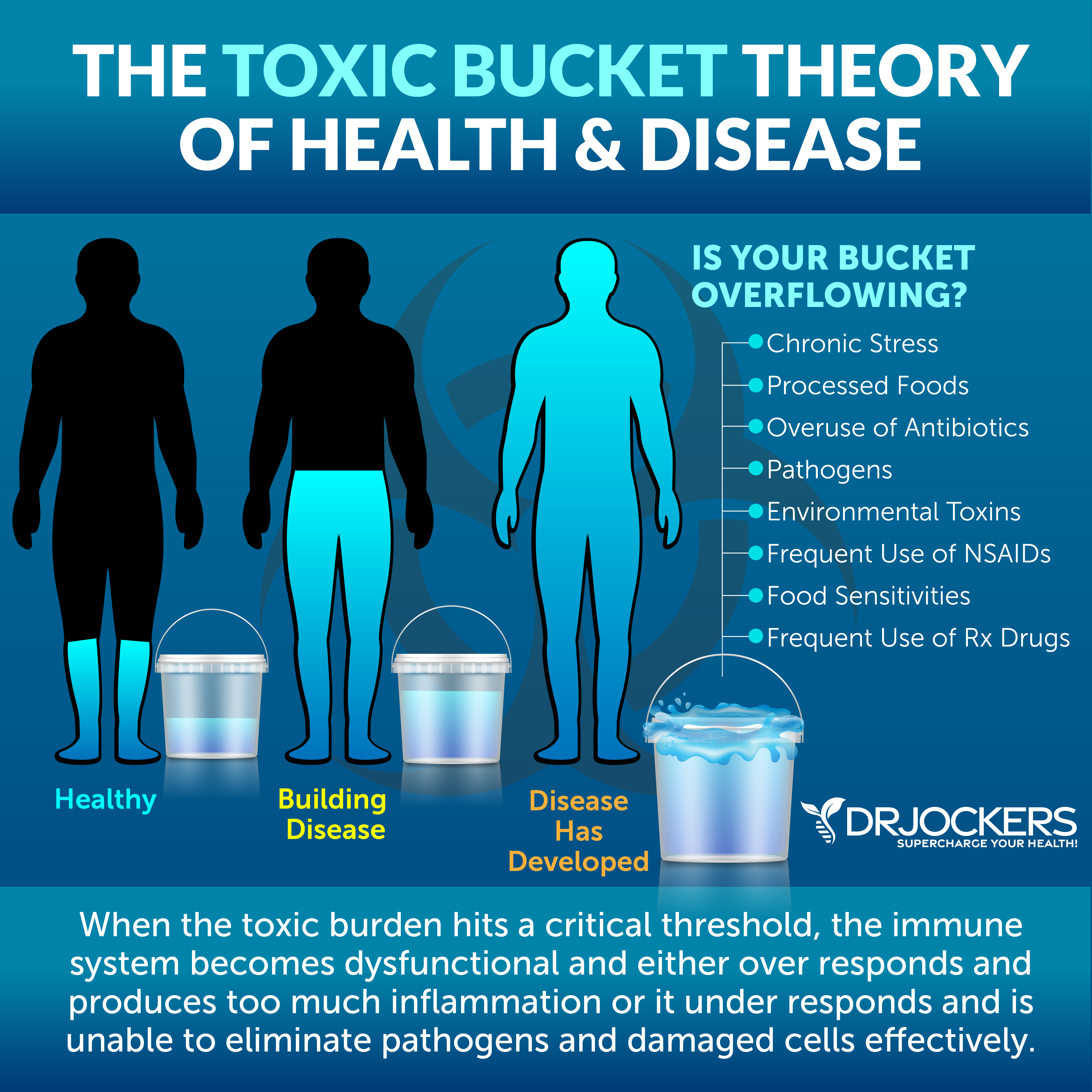
Chronic Inflammation
Inflammation is your body’s mechanism to protect you from harm, such as infections, injuries, allergens, and toxins. For example, if you get stung by a bee, your body will experience acute inflammation to support quick recovery. Acute inflammation may last for a few days or weeks and gradually gets better. It is essential for recovery.
Chronic inflammation happens if your body feels that it is constantly under attack. Constant exposure to inflammatory, unhealthy foods, toxins, allergens, poor lifestyle choices, stress, or other triggers can cause your body to send low levels of inflammation on a constant basis. Chronic inflammation, unfortunately, can cause chronic symptoms and increase your risk of various chronic or serious health issues, including stomach cancer.
A 2008 study by the Columbia University Medical Center has found that H pylori may lead to chronic inflammation, which may increase the chance of developing stomach cancer (8). A 2013 review published in Current in Pathobiology Reports has also found that H Pylori infections may contribute to chronic inflammation and may increase the risk of stomach cancer (9).
A 2019 review published in Currents Topics in Microbiology and Immunology has found that chronic inflammation may play a critical role in stomach cancer, and addressing chronic inflammation may be important for treatment (10).
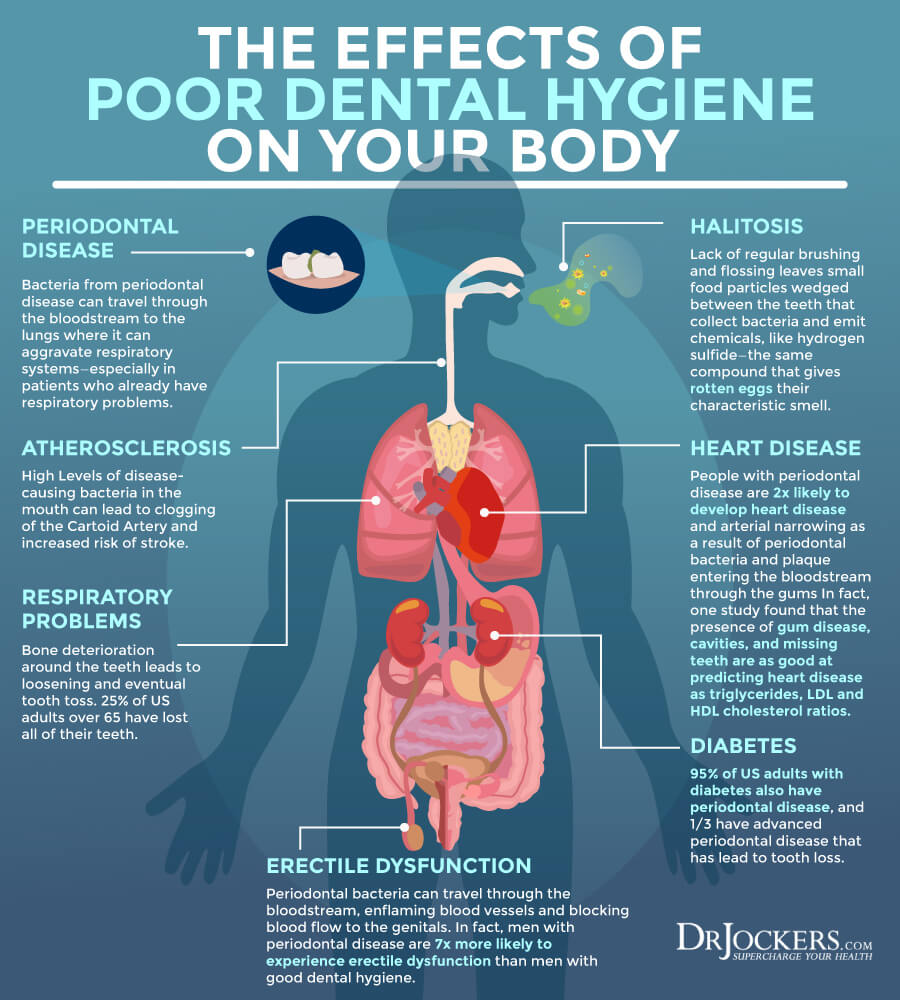
Poor Oral Health
Digestion starts in your oral cavity. It’s not surprising that poor oral health may increase your risk of stomach cancer. Not to mention that H Pylori bacteria may be using the oral cavity as a reservoir. As you know, H pylori infections are one of the major risk factors and underlying root cause factors of stomach cancer.
A 2016 review published in the World Journal of Gastrointestinal Pharmacology and Therapeutics has found that H pylori infection can take over your oral cavity and increase the risk of gastric infections (11). A 2018 prospective cohort study of 19,831 participants published in the International Journal of Cancer has found that poor oral health, tooth loss, and denture-related issues may increase the risk of stomach cancer (12).
A 2021 review published in Oncology Reports has found a link between oral microbiome health and gastrointestinal cancers, including stomach cancer (13). They selected 137 relevant studies and identified the importance of the oral microbiome in gastrointestinal tumors, diagnosis, and treatment.
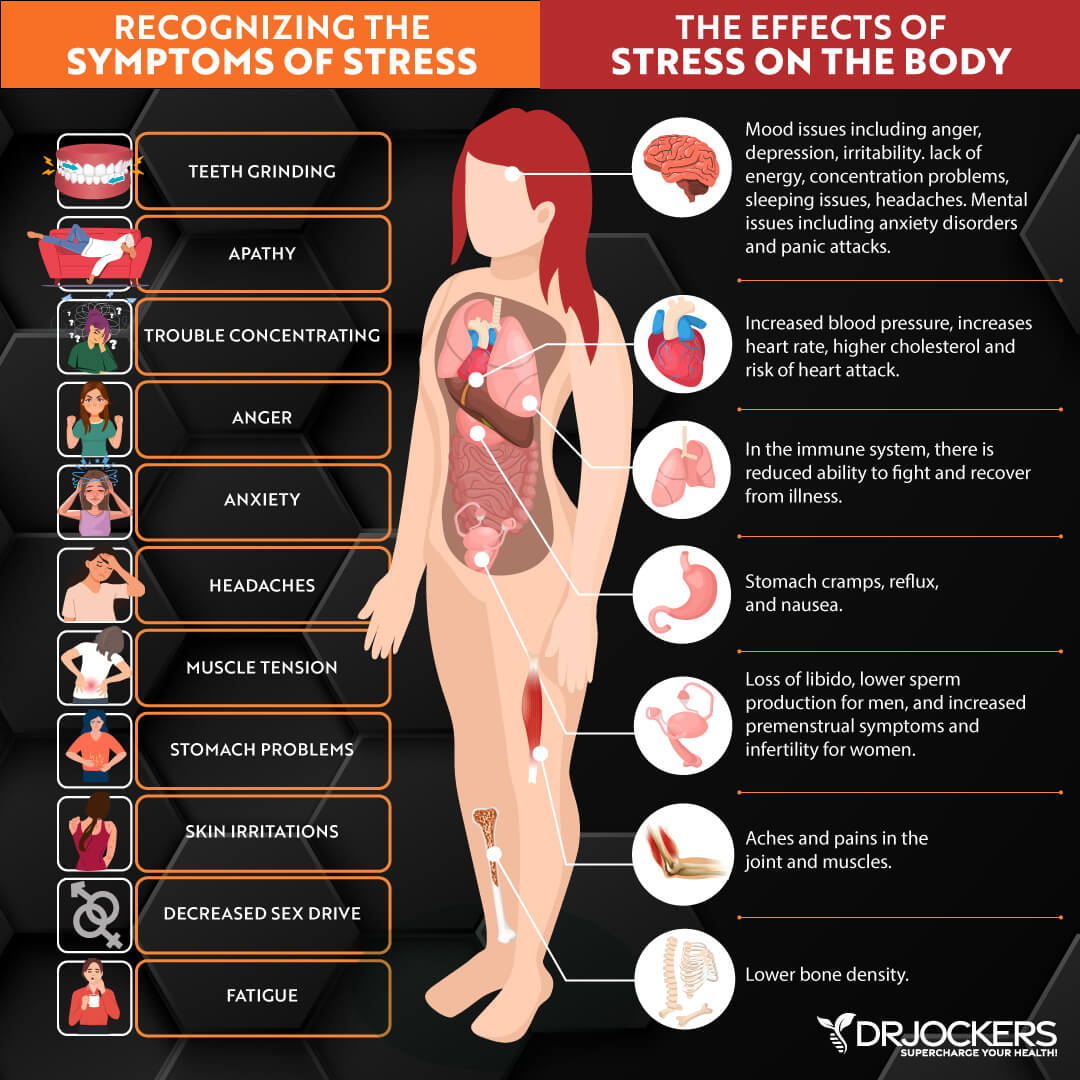
Chronic Stress & Poor Sleep
Chronic stress and poor sleep are major underlying issues behind most chronic symptoms and diseases, including stomach cancer. Unfortunately, chronic stress and poor sleep are rampant in our modern world. Chronic stress may increase chronic inflammation in your body which may lead to disease. Chronic stress may also contribute to poor sleep.
However, poor sleep may contribute to both chronic stress and chronic inflammation. Chronic symptoms from chronic inflammation may also lead to chronic stress and poor sleep. It can turn into a vicious cycle unless you address all factors.
A 2009 population-based study published in Cancer Research and Treatment has found that eliminating stress may prevent 68.9 percent of stomach cancer cases (14). On the other hand, a 2019 study published in Cell Death and Disease has found that chronic stress may contribute to both the progression and metastasis of stomach cancer (15). A 2021 study published in Science Reports has found that poor sleep and the disruption of the circadian rhythm may increase the risk of stomach cancer (16).
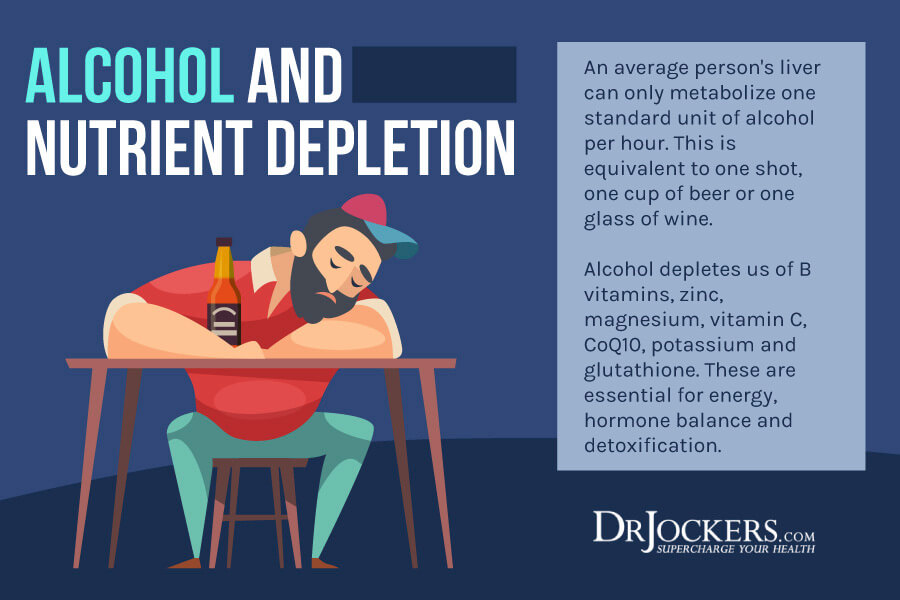
Smoking & Heavy Alcohol Use
Smoking cigarettes and heavy alcohol use can both have serious health consequences. We all know that smoking may, of course, damage your lungs and respiratory system, and too much alcohol may damage your liver. However, you may not know that smoking and heavy alcohol use may also increase your risk of stomach cancer.
A 2012 multiethnic cohort study published in Cancer Causes and Control has found that cigarette smoking may increase the risk of stomach cancer (17). They looked at 215,000 men and women. Researchers found a link between the number of cigarettes smoked per day and the duration of smoking for gastric cancer. They found that while former smokers had an increased risk in men, it wasn’t true for women.
A 2018 study published in the European Journal of Cancer Prevention has found that smoking cigarettes may increase the risk of stomach cancer (18). Researchers found that the number of cigarettes smoked per day and the years smoked also determine the risk. They found that stopping smoking for 20 years may decrease the risk of stomach cancer as low as for non-smokers. A 2020 large cohort study published in Gastroenterology has found that smoking is another risk factor for stomach cancer in those with H pylori infection (5).
A 2017 meta-analysis published in Oncotarget has found a connection between drinking alcohol and an increased risk of stomach cancer (19). Another 2017 review and meta-analysis published in Medical Science Monitor has also found that moderate and heavy alcohol drinking may increase the risk of stomach cancer (20).
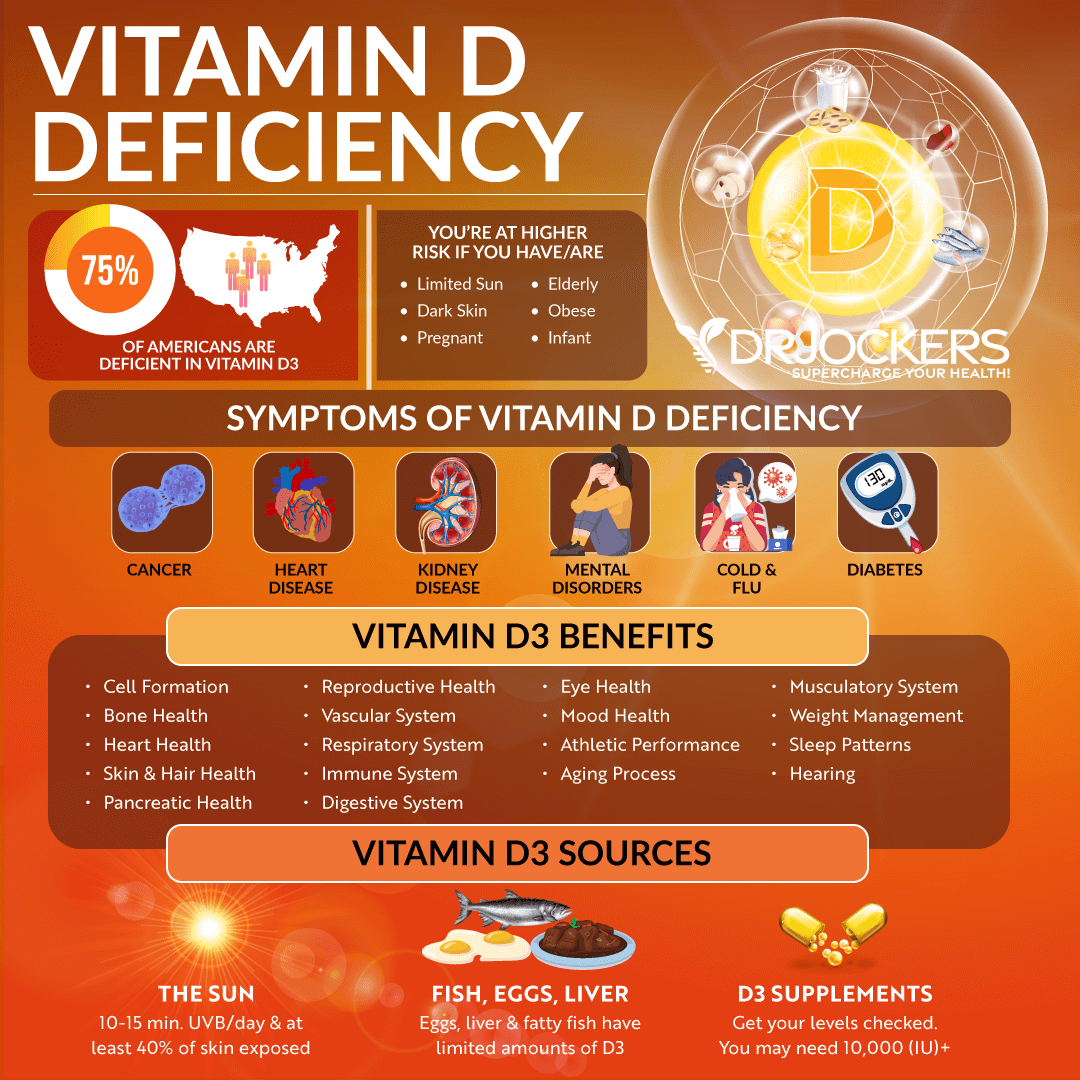
Vitamin D Deficiency
Vitamin D is a critical vitamin. Your body converts vitamin D when the UV rays of the sun hit your skin. Certain foods such as eggs, oily fish, and cod liver oil also include some vitamin D.
Vitamin D is critical for your bone, muscle, immune, brain, and overall health. Yet deficiencies in vitamin D are rampant and can contribute to chronic inflammation and various chronic and serious health issues, including stomach cancer.
A 2016 retrospective chart analysis published in the World Journal of Gastrointestinal Oncology has found a link between vitamin D levels and stomach cancer (21). They found that vitamin D deficiency may increase the risk of stomach cancer. A 2021 study published in Cureus has also found a correlation between vitamin D deficiency and an increased risk of stomach cancer (22).
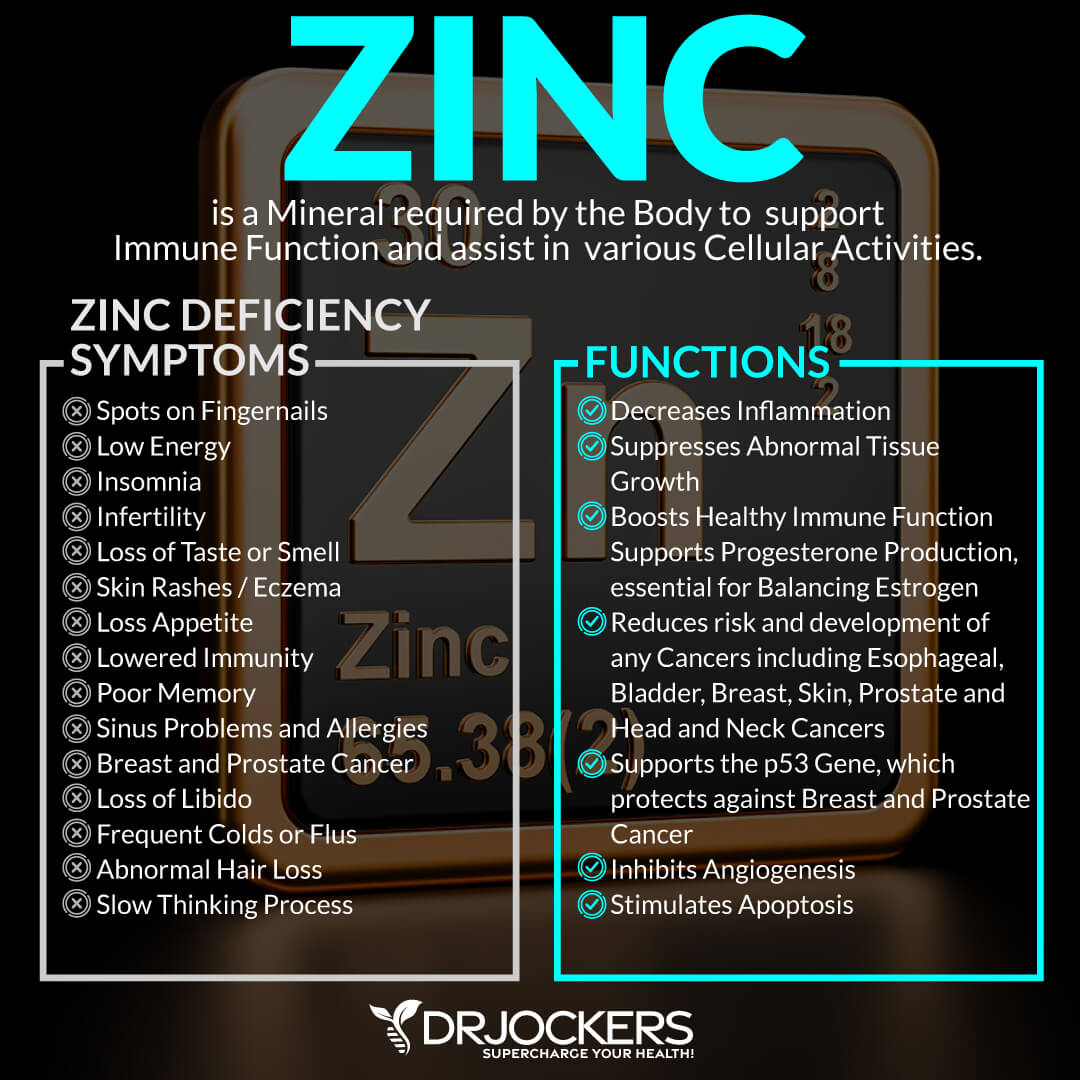
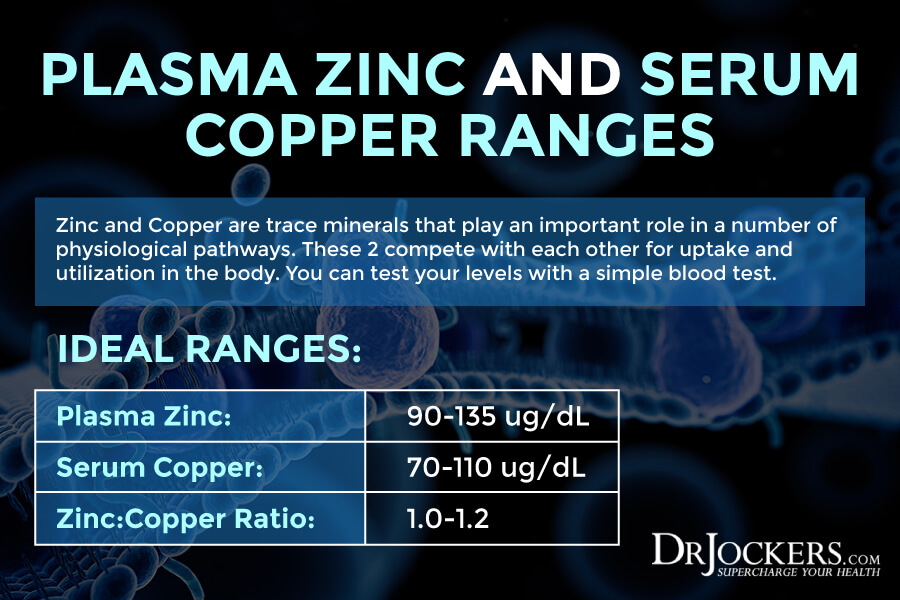
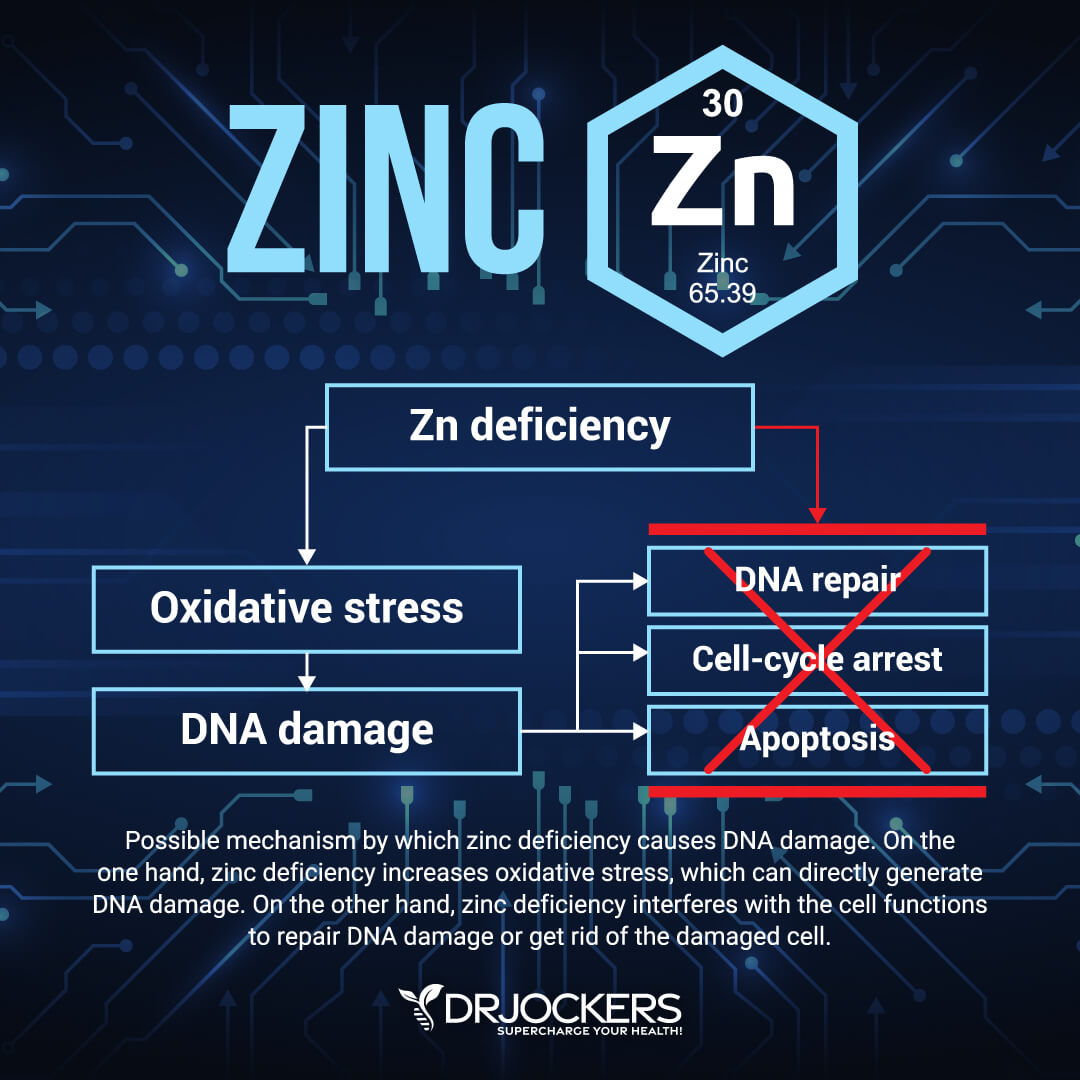
Zinc Deficiency
Zinc is found in meat, poultry, shellfish, eggs, dairy, seeds, nuts, legumes, sweet potatoes, quinoa, green leafy vegetables, and other foods. It is an important mineral for your immune and overall health. Deficiencies in zinc are common and can lead to all sorts of health issues. Zinc deficiency may contribute to the increased risk of stomach cancer.
A 2014 systematic review and meta-analysis published in Clinical Nutrition has found a link between zinc deficiency and an increased risk of digestive tract cancers, including stomach cancer (23). A 2015 review published in Advanced Biomedical Research has also found a link between zinc serum levels and stomach cancer (24).
A 2018 study published in Oncogene has found that improving zinc levels may be beneficial for stomach cancer patients (25). A 2020 case-control study published in the Japanese Journal of Cancer Research has found that not only zinc levels, but your copper/zinc ratio matters too (26). A high copper/zinc ratio may increase the risk of stomach cancer.
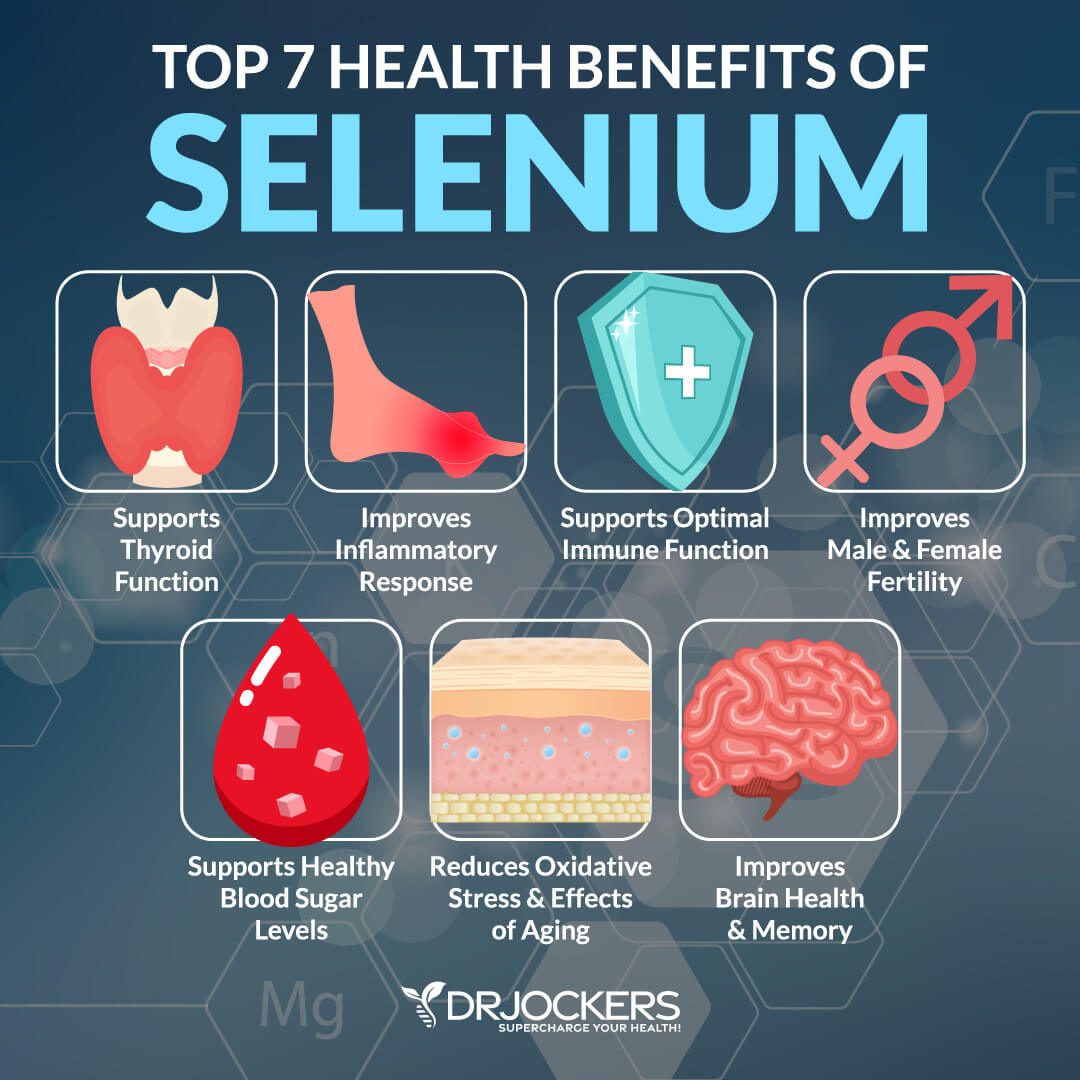
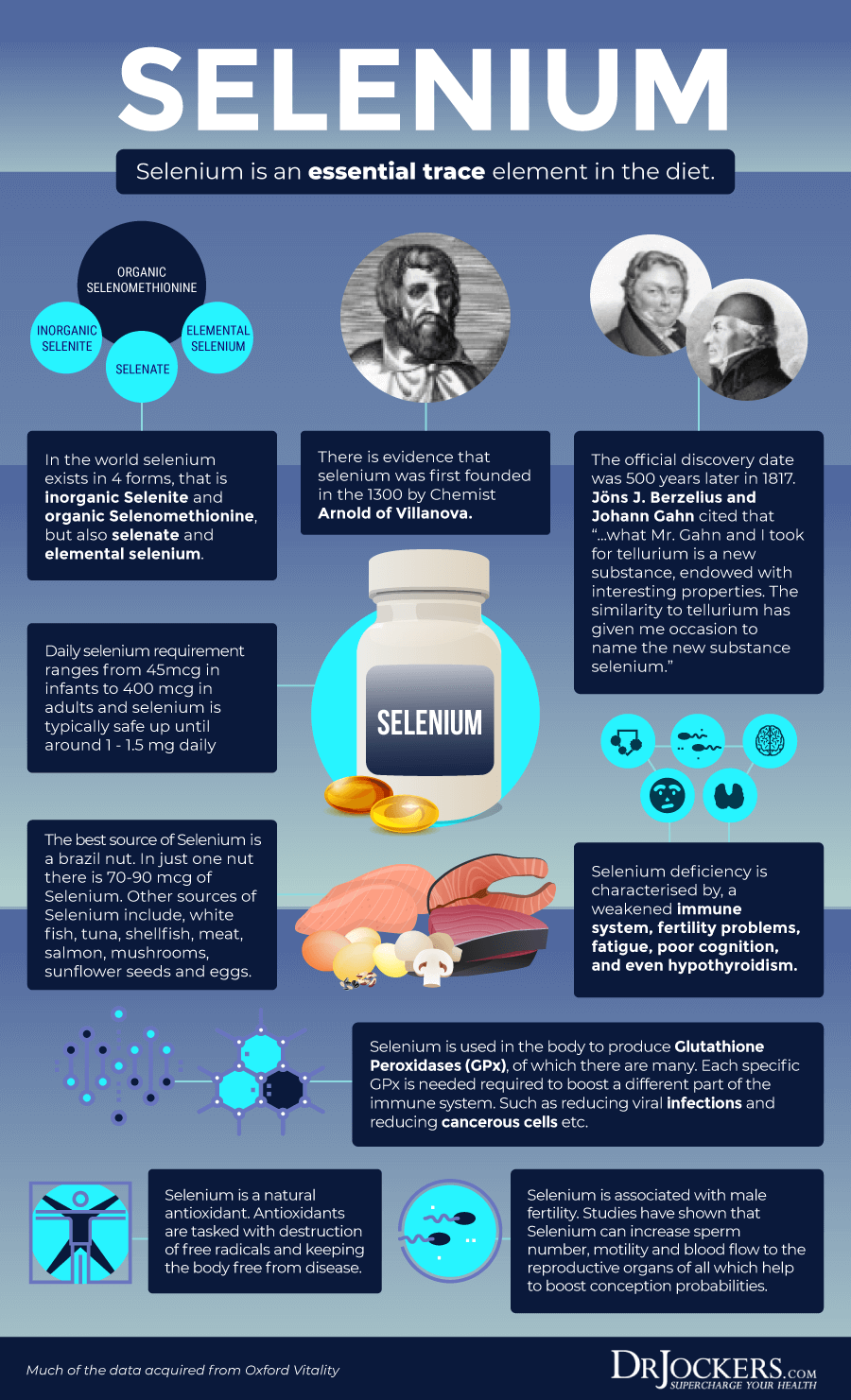
Selenium Deficiency
Selenium is a powerful antioxidant and important mineral found in Brazil nuts, as well as sunflower seeds, cashew, mushrooms, spinach, seafood, meat, and eggs. Healthy selenium levels may be important for your immune health and the reduced risk of cancer, heart disease, and other health issues. Selenium deficiency may increase your risk of stomach cancer.
A 2015 study published in the Iranian Journal of Medical Sciences has found that low selenium levels are common in stomach cancer patients (27). A 2016 review published in Oncotarget has found that selenium deficiency may lead to an increased risk of stomach cancer (28).
A 2012 study published in the Journal of Gastric Cancer has found a correlation between selenium levels and the location of stomach cancer and a link between poor zinc levels and advanced stomach cancer (29).
Chemical Exposures
Toxins and chemical exposure may increase the risk of chronic inflammation and all kinds of serious health issues. People working in certain occupations have an increased risk of chemical exposure. This population is also at a higher risk of chemical exposure-related stomach cancer.
A 1998 study published in Epidemiology has found that occupation chemical exposure may contribute to increased stomach cancer risk (30). A 2020 pooled analysis published in the International Journal of Epidemiology has found that occupational exposure to chemicals may increase the risk of stomach cancer (31).
Occupations that are at a higher risk of chemical exposure and related stomach cancer include agricultural and animal husbandry workers, miners, well-drillers, quarrymen, and related professionals, toolmakers, blacksmiths, and machine-tool operators, stationary engine and related equipment operators, carpenters, bricklayers, and construction workers.
Furthermore, workers that are exposed to pesticides, herbicides such as glyphosate, coal derivatives, aromatic amine, wood dust, radiation, magnetic fields, and chromium may also have an increased risk of stomach cancer (31).
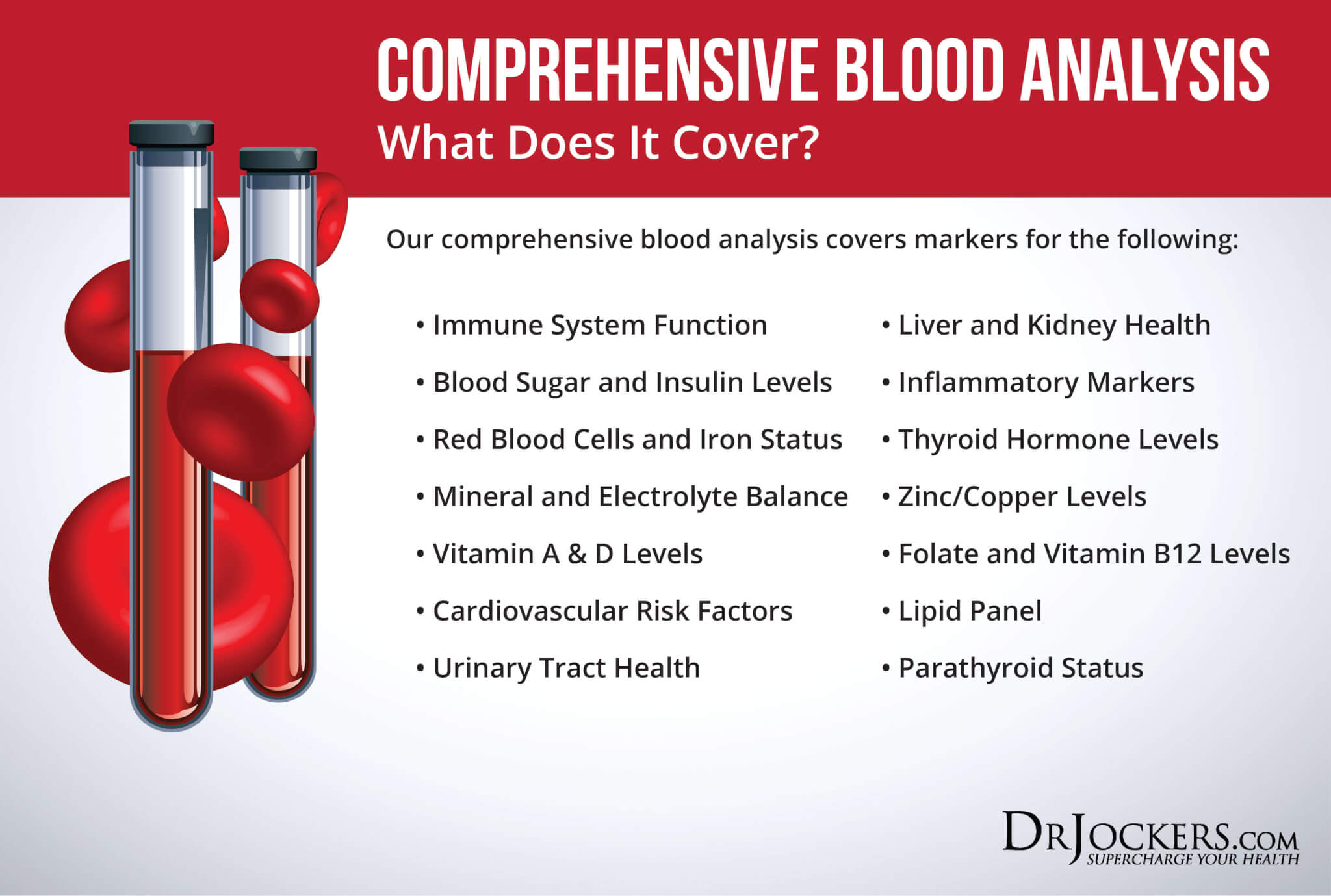
Key Functional Labs
There are a number of key functional labs I use and recommend to determine your risk factors and uncover the root causes of stomach cancer. Here is what I recommend.
Inflammation: Hs-CRP, ESR, LDH & Serum Ferritin
There are a number of tests I recommend to check for underlying inflammation, including Hs-CRP, ESR, LDH, and serum ferritin testing.
The C-Reactive Protein or CRP test is a key test I recommend. It measures a protein (CRP) produced in your liver that indicates inflammation levels in your body. The clinical range is between 0 and 3 mg/L while the optimal range is 0 to 1 mg/L. When I see levels over 1 mg/L, I know the individual is having an inflammatory response that could be due to acute trauma or chronic conditions.
The erythrocyte sedimentation rate (ESR) is a common hematology test to look for inflammation. It refers to the rate at which your red blood cells in anticoagulated whole blood go down in a standardized tube over a period of one hour. Optimal ESR rates for women under 50 are between 0 and 20 mm/hr, men under 50 are between 0 and 15 mm/hr, women over 50 are between 0 and 30 mm/hr, men over 50 are between 0 and 20 mm/hr, and children between 0 and 10 mm/hr.
Lactate Dehydrogenase (LDH) is an enzyme found in all living cells. Elevated levels may indicate inflammation. Optimal levels are between 140–180. Levels over 180 indicate inflammation.
Serum ferritin measures the level of ferritin in your body to detect iron deficiency anemia and other health issues. Elevated serum ferritin levels may indicate inflammation, liver disease, autoimmune disease, or even cancer. The clinical range is 30 to 400, and the optimal range is 25 to 100 for females and 50 to 150 for males. You can get these labs done on our Comprehensive Blood Analysis here.
Insulin Resistance: Fasting Insulin, HbA1C, Lipid Profile
I recommend a number of tests to check for insulin resistance, including fasting insulin levels, HbA1C, and a lipid profile.
Blood sugar imbalances may increase your risk of inflammation. In addition to testing your HbA1C levels, I recommend checking your fasting insulin levels. Testing your fasting insulin can recognize elevated blood sugar levels and can detect inflammation, insulin resistance, blood sugar issues, and diabetes. The clinical range for fasting insulin is 2.6 – 24.9 uIU/ml and the optimal range is 1.0 – 5.0 uIU/ml.
Blood sugar imbalances are one of the main causes of inflammation, so I recommend checking your hemoglobin A1C (HbA1C) levels. Your HbA1C levels measure your average blood sugar over the past 2 to 3 months. Hemoglobin A1C (HbA1c) gives the average amount of glucose in your blood or blood sugar over the past 3 months making it one of the top tests for inflammation and diabetes. The clinical range is between 4.8 and 5.6 while the optimal range is 4.5 – 5.2.
Having a balanced ratio of LDL to HDL and triglycerides to HDL is essential for your health. We are looking for low HDL or high triglycerides as a sign of insulin resistance. Ideally, we are looking for an LDL: HDL ratio: 3:1 or less, 2:1 being optimal. For triglycerides, we are looking for an HDL ratio: 2:1 or less, 1:1 being optimal. Higher rates may indicate insulin resistance and inflammation. Optimal levels:
- VLDL cholesterol: The ideal range is 5 to 30 mg/dl.
- HDL cholesterol: The ideal range is 55 to 80. Levels above 100 can indicate chronic inflammation or active infection in the body.
- Triglycerides: The ideal range is 40 to 80.
Vitamin D, Plasma Zinc: Serum Copper Ratio
Since vitamin D and zinc deficiencies and high copper levels may increase the risk of stomach cancer, I recommend checking your vitamin D and zinc: serum copper ratio.
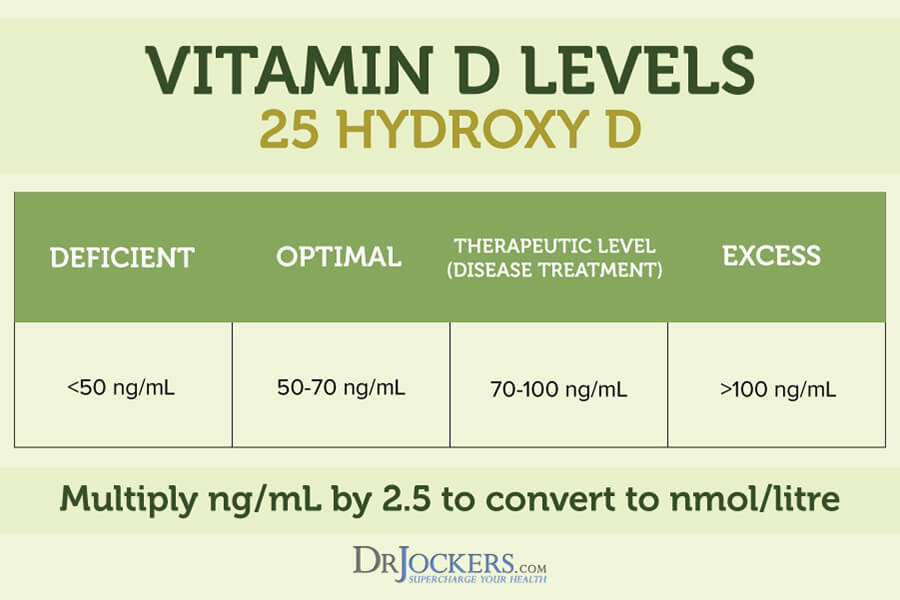
Vitamin D3 is an important vitamin that most of our population is deficient in. Poor levels may indicate inflammation. You want your vitamin D (25-OH) levels to be up over 50 ng/mL with the optimal range being between 60-100 ng/mL
Checking your plasma zinc levels is the best way to determine zinc levels in your body. Ideal plasma zinc levels are between 90–135 ug/dL and for serum copper it should be 70–110 ug/dL. Zinc and copper compete against each other as antagonists to regulate physiological pathways. A proper balance between the two is essential for maintaining good health. I recommend checking your plasma zinc and serum copper levels and their balance. The proper zinc:copper ratio should be between 1–1.2.
Testing for H Pylori Infection:
There are several different ways of testing for an H Pylori infection.
1) Stool Testing: This is considered the gold standard in H Pylori diagnosis as it counts the actual particles of the H Pylori organism. This is the test I use with clients to find out if they are infected.
2) Blood Tests: These tests look for antibodies to the H Pylori organism and will test for IgA, IgG and IgM reactions. If these antibodies test positive it is a clear diagnosis of an infectious process. Research has shown that this is a good test for acute infections but long-term infections and individuals with weakened immunity often do not have elevated anti-bodies.
The other issue with H Pylori antibodies is they may be present even when the infection is under control. This means you will test positive even you are actually negative and the organisms are in their proper numbers.
3) H Pylori Breath Test: The H Pylori organism produce urease which breaks down urea in the stomach into ammonia and carbon dioxide. The breath test measures for elevated CO2 that is produced from this reaction.
4) Endoscopy: This is a highly invasive procedure where a scope is inserted into the esophagus and stomach. This is stressful on the body and does a poor job of analyzing for the presence of this infection but it can see the results of the infection such as irritation, ulcerations and cancer in the stomach.
The most well rounded test that looks at H Pylori with great accuracy and also maps out the entire microbiome and looks for a wide variety of pathogens and markers of gut health is the GI MAP stool analysis you can find here
Natural Support Strategies
You can support your stomach and overall health through diet, lifestyle, and other natural methods. Here are the natural support strategies I recommend to support your health and well-being:
Anti-Inflammatory Nutrition Plan
Chronic inflammation is one of the main functional root cause factors in stomach cancer (8, 9, 10). Following an inflammatory diet high in refined sugar, refined oil, artificial ingredients, junk food, and highly processed foods, is one of the driving factors of chronic inflammation. According to a 2018 study published in The American Journal of Clinical Nutrition, a poor diet may increase the risk of stomach cancer (32).
A 2019 study published in PLoS One has also found that the inflammatory potential of the diet may play a role in determining the risk factor for stomach and lung cancer (33). Researchers found that an anti-inflammatory diet was linked to a lower risk for cancer.
Thus following an anti-inflammatory nutrition plan may help you to reduce chronic inflammation and your risk factors. I recommend removing all inflammatory foods and choosing an anti-inflammatory, nutrient-dense, whole foods diet instead. Eat a diet rich in greens, vegetables, herbs, spices, sprouts, low glycemic index fruits, grass-fed meat, pasture-raised poultry and eggs, wild-caught fish, and wild game.
Eat lots of healthy fats, including avocadoes, coconut oil, coconut butter, olives, extra-virgin olive oil, grass-fed butter and ghee, and fatty fish. Include anti-inflammatory herbs and spices, such as turmeric, ginger, basil, rosemary, oregano, and cinnamon.
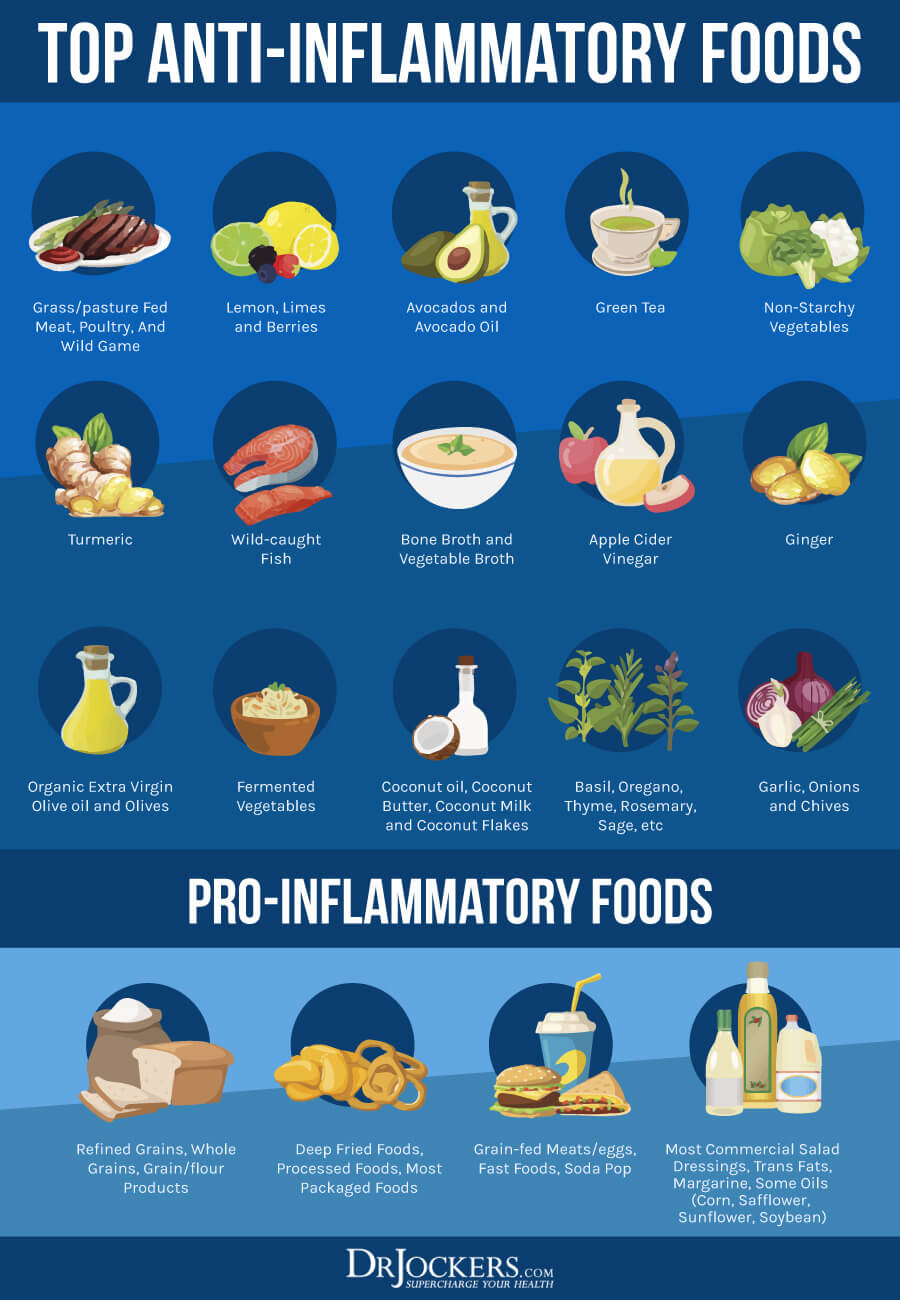
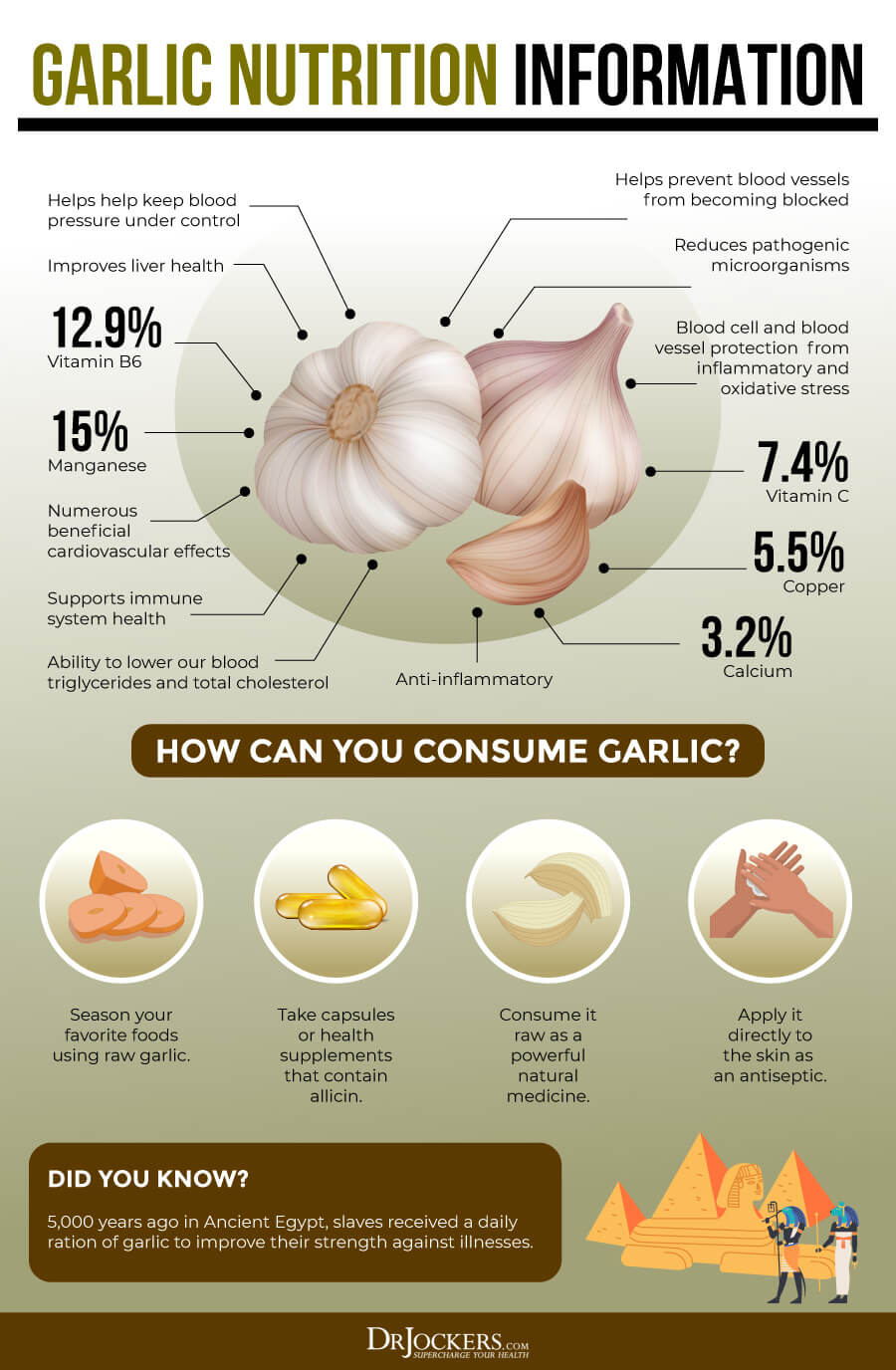
Eat Onions and Garlic
Onions and garlic are an important part of any anti-inflammatory diet. They offer anti-inflammatory and antioxidant benefits. They are also excellent sources of prebiotics that feed the good bacteria in your gut and support your gut microbiome health. They may also offer powerful benefits for cancer.
A 2015 review published in Cancer Prevention Research (Philadelphia) has found that onions, garlic, shallots, chives, and leaks are allium vegetables that may help to deactivate carcinogens, offer antimicrobial properties, and may help to reduce the risk of cancer (34). Another 2015 meta-analysis has also found that eating allium vegetables, such as onions and garlic, may help to reduce the risk of stomach cancer (35).
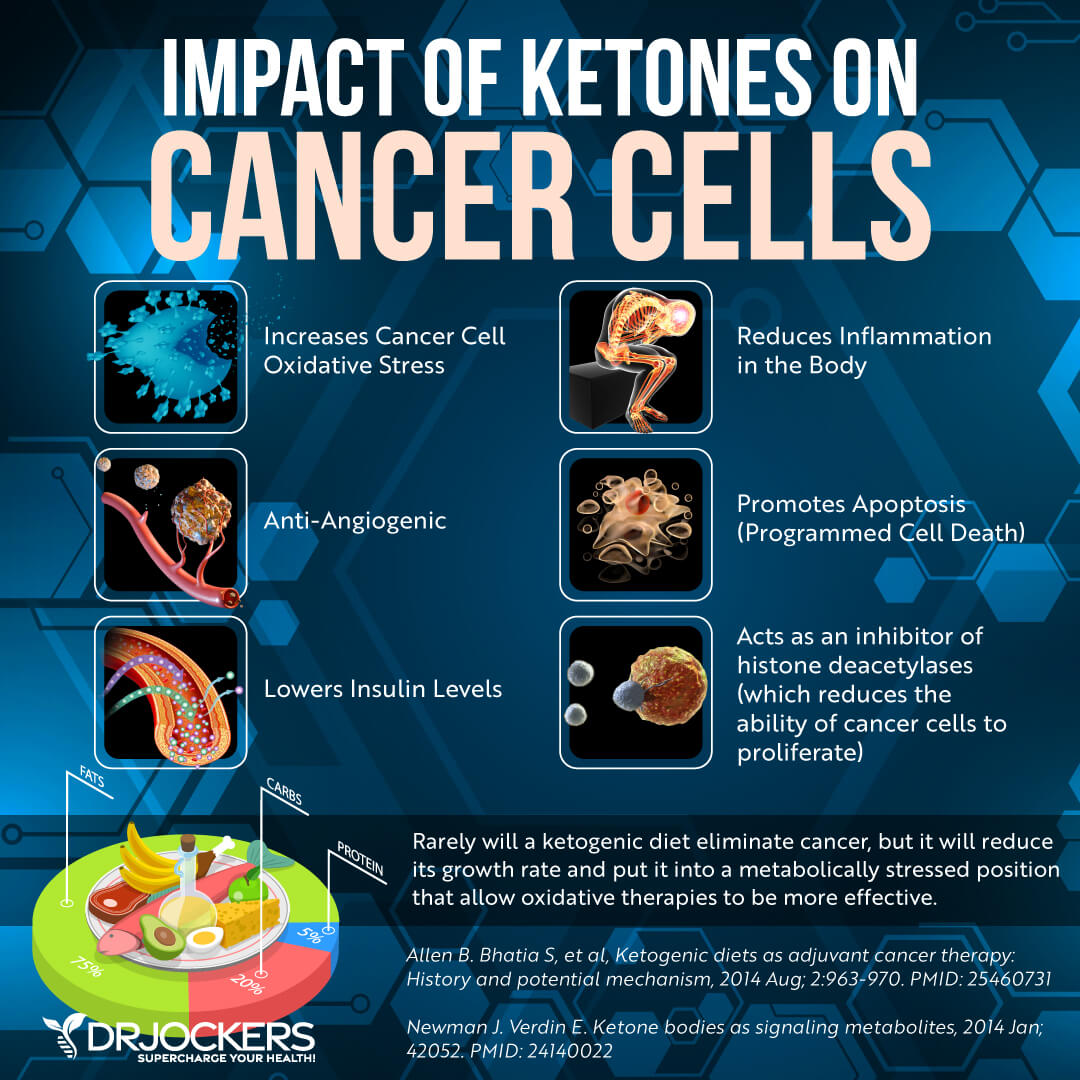
Get Into Ketosis
According to a 2017 systematic review published in the International Journal of Preventative Medicine, the ketogenic diet may help to reduce the growth of cancer cells (36). A 2021 systematic review and meta-analysis of animals studies published in Frontiers in Nutrition has found that according to preclinical evidence, the ketogenic diet may offer anti-tumor benefits (37). Though human research studies are still needed on the benefits of the keto diet on stomach cancer, due to its anti-inflammatory and other health benefits, the ketogenic diet may be a beneficial natural support strategy.
To follow a ketogenic diet, follow a high-fat, low-carb, moderate-protein diet at around 60-70% fats, 20 to 30% protein, and 5 to 10% carbs. Most of your diet should be high-quality, nutrient-dense, healthy fats, such as avocadoes, coconut oil, coconut butter, olives, extra-virgin olive oil, grass-fed butter and ghee, fatty fish, and other animal fats.
Eat high-quality animal protein from grass-fed meat, pasture-raised poultry and eggs, wild-caught fish, and wild game. Your carbohydrate intake should be very low and should come from low glycemic index fruits, such as berries, cherries, and citrus, and vegetables, such as cucumber, bell pepper, broccoli, and carrots. Learn more in the real food keto diet article here.
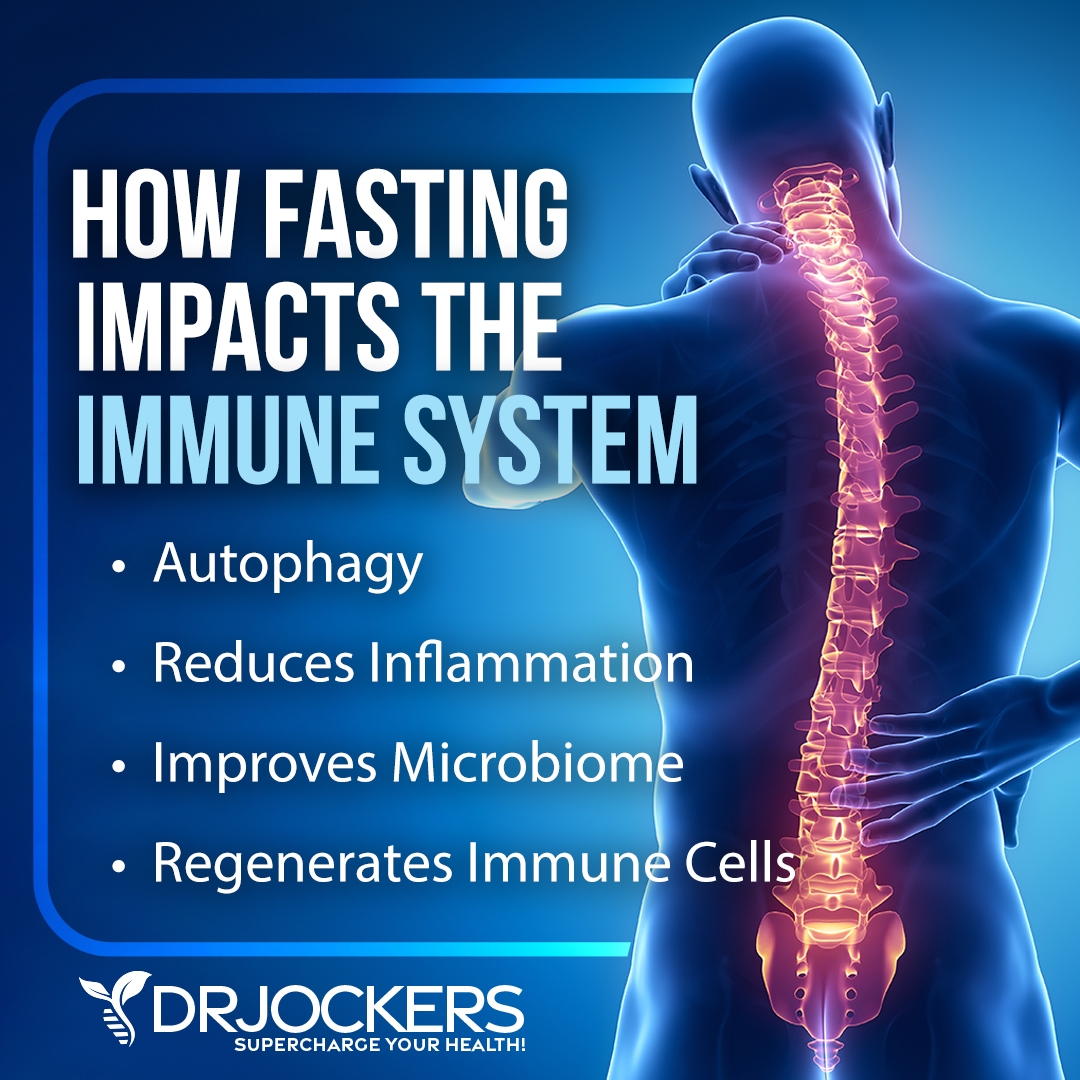
Intermittent Fasting
Intermittent fasting and other forms of fasting may offer many health benefits, including autophagy, insulin sensitivity, digestion, inflammation, and other factors of health. Research has shown that it may also help to reduce the risk of cancer and support recovery.
A 2018 review published in National Review Cancer has found that fasting and fasting-mimicking diets may help to support chemotherapy, immunotherapy, and other cancer treatments (38). A 2015 study published in Cell Metabolism has found that a fasting-mimicking diet may reduce the risk of cancer, among other health benefits (39).
Fasting may also be combined with the ketogenic diet for further benefits. Following a ketogenic diet during the eating windows of intermittent fasting, trying a fat or keto partial fasting strategy, and following a keto diet between extended fasting periods may all be helpful. A 2020 study published in Chemotherapy has found that the combination of fasting and the ketogenic diet may reduce the development of cancer, including stomach, colon, pancreatic, and breast cancer (40). Researchers found that this strategy may also support the treatment of chemotherapy.
Intermittent fasting is a type of eating. It cycles between a period of fasting and a period of eating within one day. The most common form of intermittent fasting includes 16 hours of fasting, including your overnight sleep and an 8-hour eating window.
If you are new to intermittent fasting, begin with a 12-hour fast, including your overnight sleep starting after dinner until the next day at breakfast. Gradually increase your fasting window until you figure out what works best for you. To learn more about the benefits of intermittent fasting and the best intermittent fasting strategies, I recommend this article.
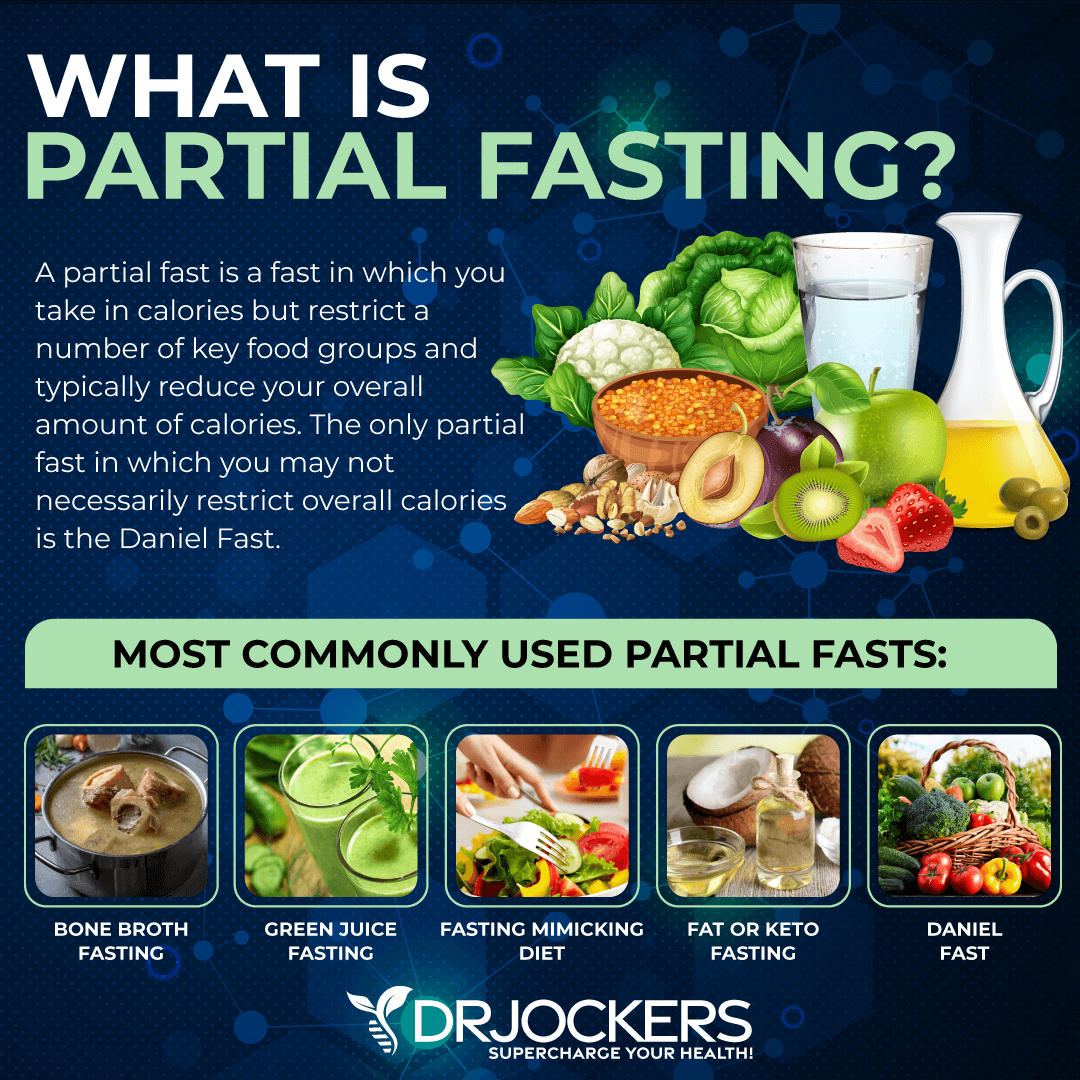
Partial and Extended Fasting:
If you are doing well on an intermittent fasting lifestyle, you may want to consider a 3-5 day water or partial fast. Partial fasting is a fasting strategy that doesn’t remove calories and food completely. You may choose a liquid partial fast, such as Bone Broth Fasting or Green Juice Fasting, drinking only bone broth or green juice.
You may choose a strategy that only limits the type of foods and amount of food you are eating, such as the Fasting Mimicking Diet® (FMD®), Fat or Keto Fast, or Daniel Fast. You may learn more about partial fasting from this article.
If you are doing well on more advanced intermittent fasting and practicing partial fasting, you may be ready for an extended fast. Extending fasting or water fasting involves drinking only purified water for a period of time. In some cases, calorie-free herbal tea is also allowed.
Water fasting is a very advanced fasting strategy that I only recommend if you are experienced with fasting and only after a consult with your healthcare provider. You may learn more about water fasting here.
Reduce Stress & Improve Sleep
Chronic stress and poor sleep can cause chronic inflammation, compromise your health, increase your risk of stomach cancer, and compromise your recovery (14, 15, 16). Reducing stress and improving sleep, on the other hand, may reduce your risk factors and support your health through recovery.
I recommend practicing meditation, breathwork, and gratitude. Try guided visualization, guided relaxation, journaling, yoga, tai chi, or qi gong. Spend time in nature and with supportive people. Develop a relaxing nighttime routine.
Avoid electronics and eating close to bedtime. Invest in a supportive bed, mattress, bedding, and pillows. Try a blackout curtain or an eye mask to help your sleep.

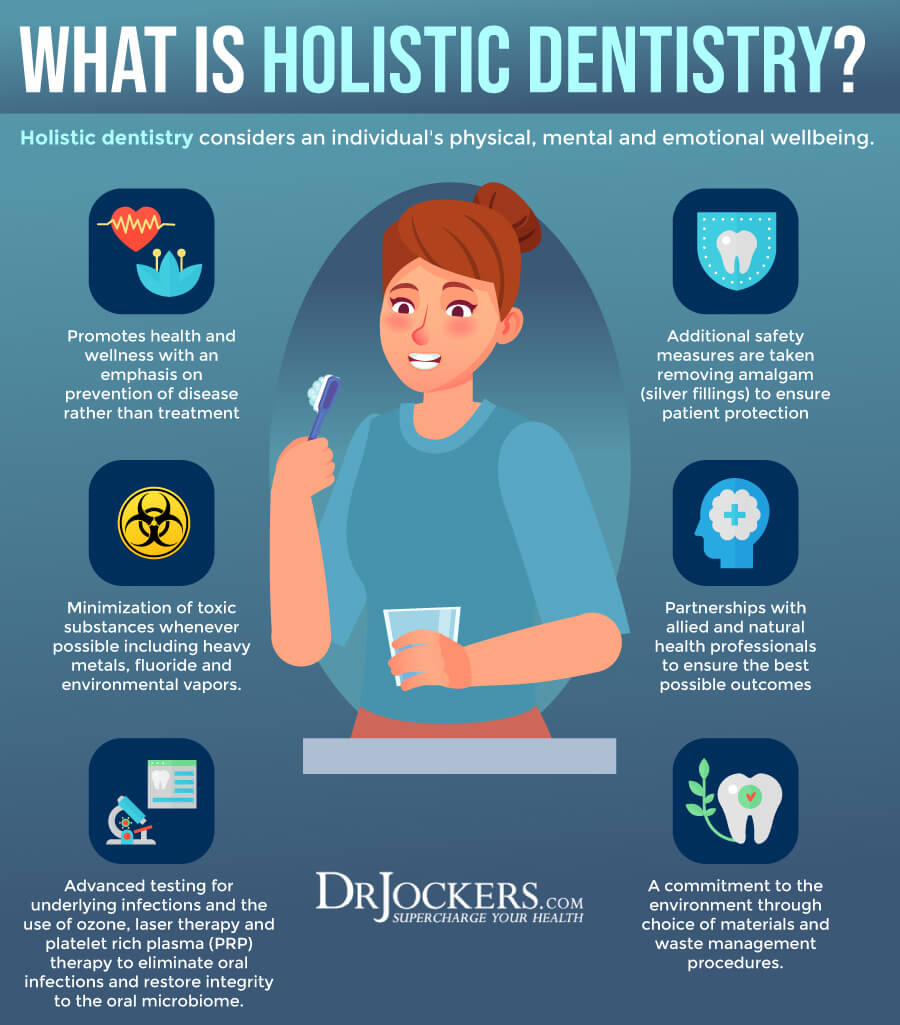
Improve Oral Health
Poor oral health may compromise your gut health, increase gastric infections, and contribute to the risk of stomach cancer (11, 12, 13). Improving your oral health is key. Reduce sugar consumption and avoid unhealthy processed foods that may increase bacterial overgrowth, cavities, and dental issues.
I recommend oil pulling every morning. Use fluoride-free, organic toothpaste and dental products. Choose holistic dental care and work with a holistic dentist. Holistic dentists use safer diagnostic care, avoid dental amalgam fillings and root canals, offer non-fluoride-based dental care, and offer herbal and natural recommendations for oral health.
Optimize Vitamin D Levels
Vitamin D is essential for your bone, muscle, brain, immune, and overall health. Your body makes vitamin D when the rays of the sun penetrate your skin, and you may also get vitamin D through some food and supplementation. Due to our indoor lifestyle and lack of supplementation, vitamin D deficiency is very common unfortunately and it can lead to chronic pain and chronic health issues.
According to a 2020 randomized clinical trial published in Cancers (Basel), vitamin D supplementation may improve the outcome of digestive cancers and increase relapse-free survival (41). A 2021 review published in Translational Cancer Research has found that vitamin D may modulate the expression of some miRNAs in deregulated cancer cells thus may offer therapeutic benefits for stomach cancer (42).
To improve your vitamin D levels, I recommend spending time out in the sun and eating vitamin D-rich fatty fish, egg yolks, and beef liver. Most people are not getting enough sunshine or consuming enough vitamin D from food. Therefore, most people need supplements to optimize their vitamin D levels.
Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and inflammation control. I recommend taking a vitamin D3 supplement with at least 3,000-5,000 IU’s of vitamin D3 and at least 90 mcg of vitamin K2.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for major health conditions is going to be between 70-100 ng/ml.
Reduce Toxin Exposure
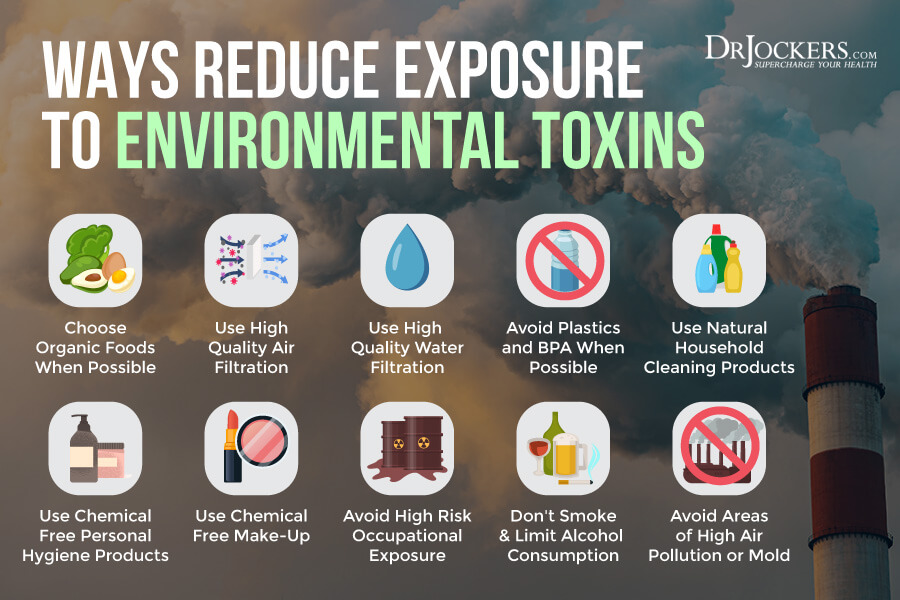
Smoking and chemical or toxin exposure may increase your risk of stomach cancer (17, 18, 5, 30, 31). Reducing your toxins exposure is critical. If you are a smoker, stop smoking. Avoid second-hand smoke. Improve your indoor air with the help of a high-quality HEPA air filtration system. Choose organic food to avoid pesticides, herbicides, and hormones.
Drink purified water instead of tap water. Avoid using plastics, especially BPA. Choose organic, natural, and homemade cleaning, hygiene, and beauty products instead of conventional options. If you are working at an at-risk occupation, consider changing your job if possible and absolutely focus on detoxifying your body.
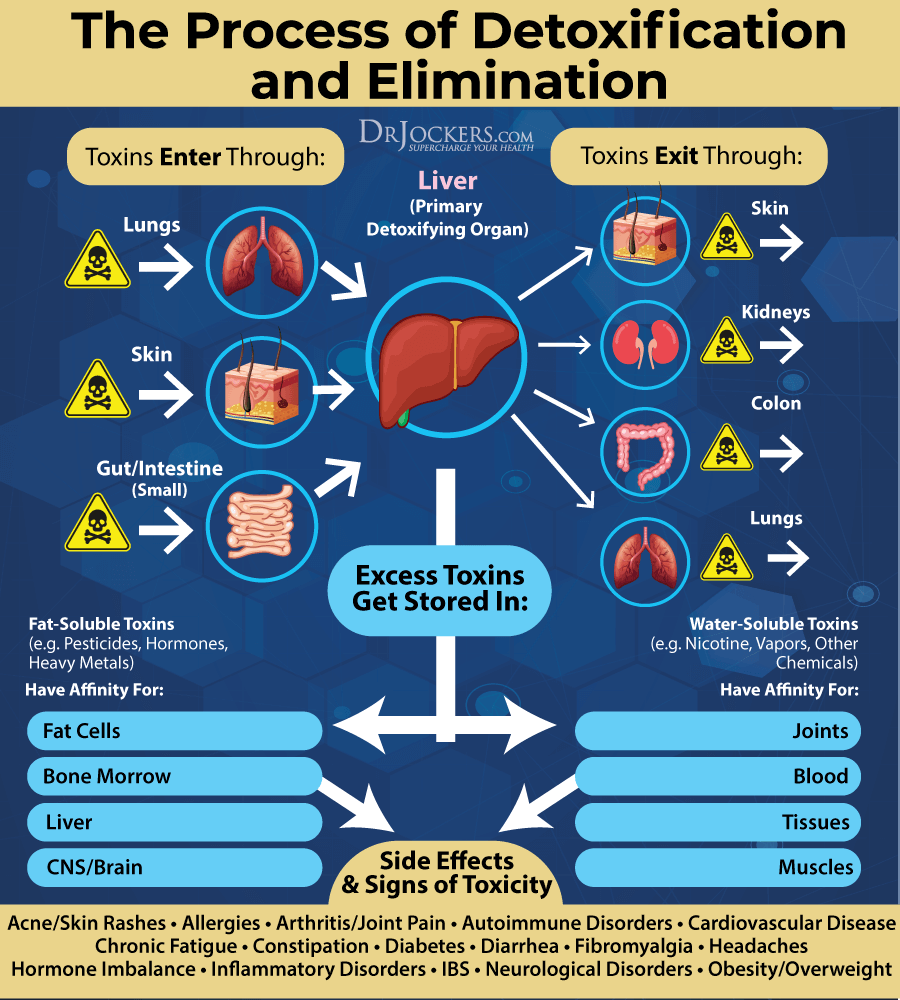
Detoxify Your Body
Since toxins can increase chronic inflammation and contribute to the risk of stomach cancer, detoxifying your body is essential (17, 18, 5, 30, 31). Follow a gut-supporting, anti-inflammatory, and antioxidant-rich diet. Hydrate your body well throughout the day to support detoxification through urine and sweating.
Try rebounding to move your lymphatic system and increase sweating. Exercise regularly and use an infrared sauna several times a week to support detoxification through the skin. Dry brush your skin daily before your shower for lymphatic health, detoxification support, and removing dead skin cells. Try coffee enemas to remove toxins and waste from your bowels.
Optimize Zinc Levels
Zinc deficiency may increase your risk of stomach cancer. (23, 24, 25, 26). A 2014 study published in the World Journal of Gastrointestinal Pathophysiology has found that zinc may support the gastrointestinal barrier and gut health (43).
I recommend eating plenty of foods that are rich in zinc, such as meat, poultry, shellfish, eggs, dairy, seeds, nuts, legumes, sweet potatoes, quinoa, and green leafy vegetables. Additionally, I recommend a zinc supplement for optimal zinc levels.
Optimize Selenium Levels
Selenium deficiency is one of the root cause factors for stomach cancer (27, 28, 9). According to a 2016 study published in the Tohoku Journal of Experimental Medicine, selenium may be beneficial for cancer (44).
I recommend eating two Brazil nuts a day which includes your daily recommended selenium levels. Consuming sunflower seeds, cashew, mushrooms, spinach, seafood, meat, and eggs may also improve your selenium levels. If you are deficient in selenium, you may benefit from supplementation as well.
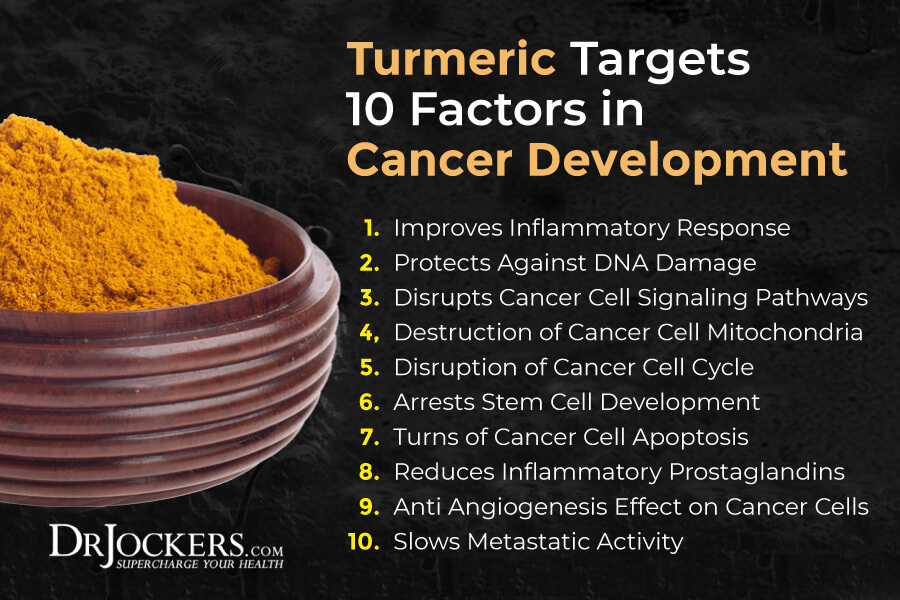
Consider Using Curcumin
Curcumin is the active compound of the spice turmeric. It offers anti-inflammatory and antimicrobial benefits. It may also help to reduce pain and support gut health. A 2019 review published in the Journal of Gastrointestinal Cancer has found that curcumin may help to reduce cancer cell proliferation, invasion, metastasis, and angiogenesis in stomach cancer (45).
A 2020 review published in Nutrition and Cancer has found that curcumin may offer therapeutic, anti-tumor, anti-inflammatory, and antioxidant benefits for stomach cancer (46). A 2021 study published in Open Life Sciences has found that curcumin may help to decrease the progression of stomach cancer (47). I recommend using turmeric in your cooking in soups, dressings, baked dishes, and green juices. I also recommend taking a high-quality curcumin supplement.
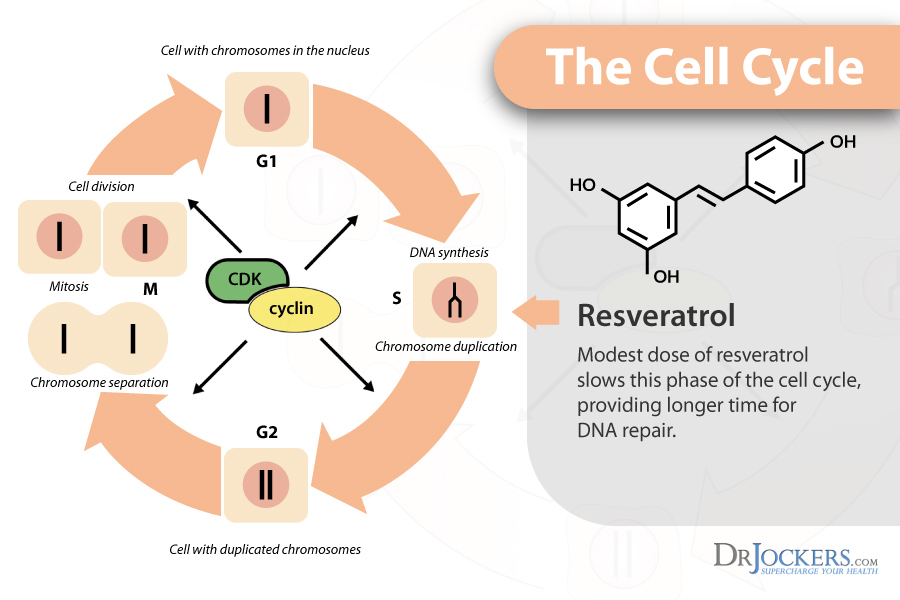
Consider Using Resveratrol
Resveratrol is a powerful antioxidant found in the skin of grapes, berries, and red wine. It greatly compliments the benefits of quercetin. A 2020 study published in the Archives of Biochemistry and Biophysics has found that resveratrol may help to suppress cancer cell proliferation in stomach cancer (48).
A 2021 review published in Cancer Cell International has found that resveratrol may offer anti-tumor benefits for stomach cancer (49). I recommend that you eat resveratrol-rich foods and take a resveratrol supplement daily.
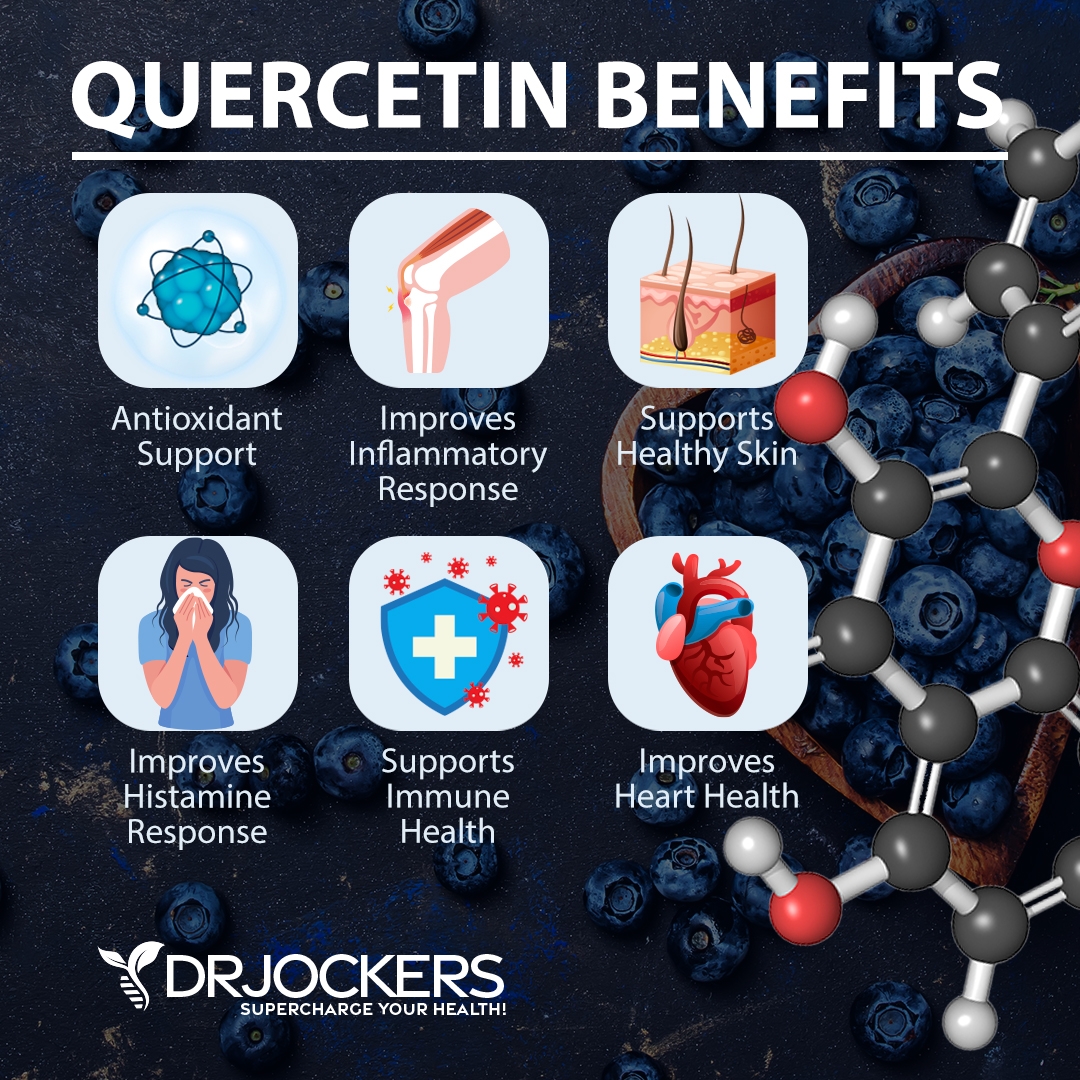
Consider Using Quercetin
Quercetin is an antioxidant and flavanol found in many plant foods, including black currants, cherries, blueberries, black plums, cranberries, apples, grapes, sage, broccoli, olive oil, pepper, kale, romaine lettuce, red leaf lettuce, raw red onions, snap peas, cabbage, raw asparagus, sprouts, and herbs. A 2011 study published in the Annals of Oncology has found that quercetin may reduce the risk of stomach cancer (50).
A 2018 study published in Integrative Cancer Cell Therapies has found that quercetin may have anti-metastatic effects on cancer cells in stomach cancer (51). I recommend that you eat plenty of quercetin-rich foods and take a daily quercetin supplement. You may find supplements for inflammation that include quercetin, resveratrol, and curcumin as well.
Final Thoughts
Stomach cancer is a type of cancer that develops when cancer cells start to grow and spread in your stomach. Unfortunately, stomach cancer doesn’t usually have any symptoms during the early stages. Most stomach cancer cases are caught at a more advanced stage after symptoms appear.
This makes treatment more difficult. Thus, supporting your body naturally becomes more important. I recommend that you follow my top natural support strategies outlined in this article to improve your health and well-being.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. On our website, we offer long-distance functional health coaching programs. For further support with your health goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!




I am a holistic nutritionist based in Mississauga, Ontario, Canada and I commend you greatly for your detailed articles from which I learn so much. When so many articles dangle a carrot when it comes to supportive therapies, yours are comprehensive and thorough and clearly originate from a genuine desire to help. Are you able to support clients in Canada?
Thank you so much Farida. Yes, our health coaching team does work with people virtually all over the world. https://drjockers.lpages.co/long-distance-coaching-dr-jockers/
Any useful suggestions for eradicating H. Pylori? Are the antibiotic regimes the only effective options for eradication? What about those who cannot tolerate them and thus discontinue?
Looking forward to your reply, many thanks…
Yes absolutely: https://drjockers.com/damaging-effects-h-pylori-infections/
Yes absolutely, here is a helpful article: https://drjockers.com/h-pylori-protocol/