![]()

Lyme’s disease is caused by the spirochete bacterium Borrelia burgdorferi (Bb) which is transmitted to humans through the black-legged tick bite. This condition is extremely serious and very challenging to overcome. Many researchers believe that lyme’s disease may be one of the most overlooked and underdiagnosed health conditions in the world.
There are 300,000 new cases diagnosed each year making it the fastest-growing infectious disease in the United States. This is ten times more Americans than what was previously reported.
The Problems With Chronic Lyme
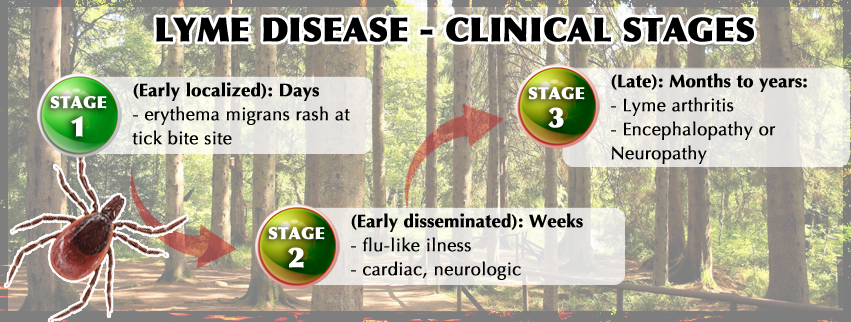
Early diagnosis and treatment are extremely critical for Lyme disease. If caught early, one can destroy the spirochete’s much quicker and with less collateral damage than after the bacterium has had a chance to spread and infiltrate multiple tissues throughout the body.
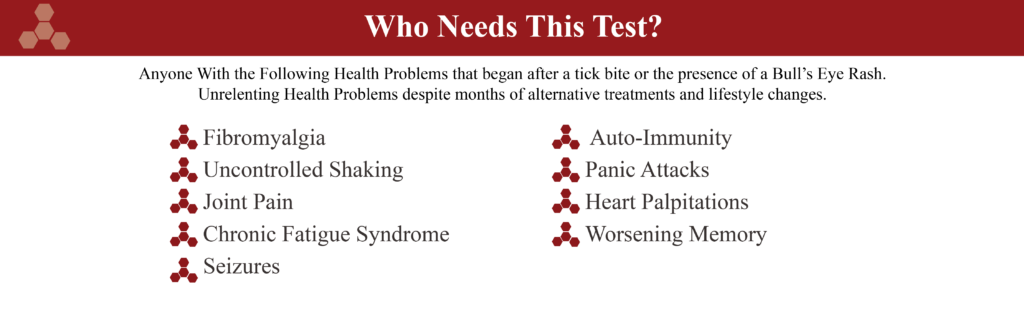
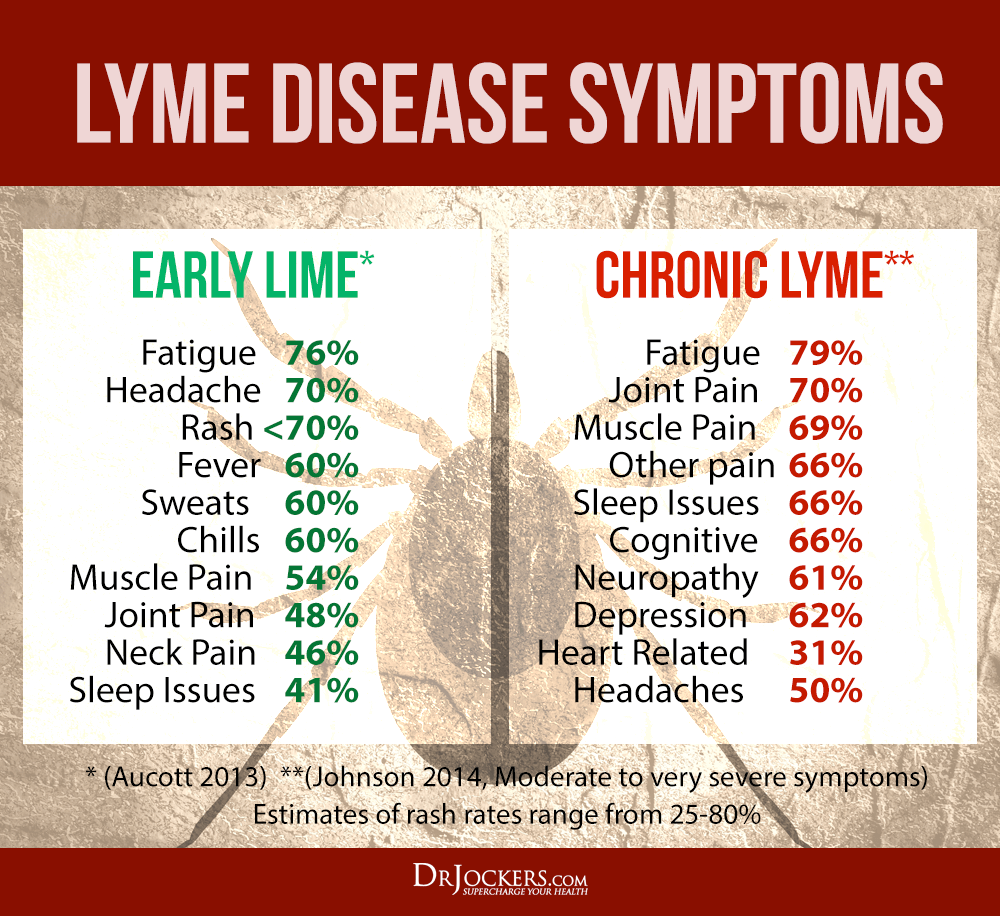
Chronic Lyme disease patients will face a long hard fight to wellness. Chronic lyme affects every system of the body and is very similar to fibromyalgia, rheumatoid arthritis and chronic fatigue syndrome. It can also progress deeper into the nervous system and create symptoms associated with Parkinson’s, ALS and multiple sclerosis.
People with chronic Lyme can have extremely debilitating symptoms. Without proper treatment, chronic Lyme patients have a poorer quality of life than patients with diabetes or heart disease.
The Biggest Mistake Doctors Make
Most doctors make several key mistakes when it comes to accurately dignosing Lyme’s disease and it results in a very high level of false negatives.
- Asking About the Tick Bite: This itself is not a mistake as that is the method of transmission for the infection. However, research has shown that fewer than 50% of Lyme patients recall the actual tick bite. Due to lack of education on Lyme, most physicians don’t consider Lyme in their differential diagnosis unless the patient tells them about a tick bite.
- Looking for the Tick Rash: Many individuals who develop Lyme’s disease develop a characteristic “Bull’s Eye” rash called Erythema Migrans. This rash is pathognomonic of Lyme disease and requires no further testing. However, up to 50% of patients culture proven Lyme’s do not have this rash. A doctor who is uneducated on this may rule out Lyme when they do not see the characteristic rash.
- Following the CDC Protocol: Research has indicated that the standard CDC protocol for detecting the presence of Lyme is flawed. The CDC uses a 2-tier system and the initial test is called an enzyme immunoassay (EIA or commonly ELISA test). If this test is negative than Lyme is ruled out of the differential diagnosis. However, this test has been shown to miss 35% of culture proven Lyme disease.
The Igenex Lyme Test
IgM & IgG Anti-bodies are Tested: This test incorporates a Western Blot for both IgM and IgG antibodies. IgM antibodies are present in an active or recent infection. IgG antibodies are produced once the infection has been present for a while, typically 6 weeks or longer.
This test is more sensitive than the CDC’s version in that it only wants to see 2 or more IgG anti-body bands as opposed to the CDC who want to see 5 or more IgG anti-body bands. This lab also ranks the intensity of the bands from none-low-medium-high so if there is only one band present but it is high than there is still a chance the bacterium is present.
Whole Blood & Serum PCR: This test uses a DNA Polymerase Chain Reaction to look for parts of the Bb organism throughout the blood. This helps complete the testing as the immune system may be too weak or tricked by the spirochete organism and may not be able to produce anti-bodies. This test is actually looking for the real DNA pieces of Bb.
Why I Love This Test
Lyme disease can be very challenging to effectively diagnose and using the traditional CDC guidelines there is a high level of false negatives. The Bb organisms are able to change shape and protein structure and trick the immune system. When the immune system cannot effectively identify the organism it is unable to produce anti-bodies.
Some people with Lyme show high levels of positive anti-bodies while others show lower amounts and other none at all. The CDC guidelines will only diagnose those who are producing high amounts of anti-bodies while the other groups will not.
This test uses the most sensitive anti-body screenings in order to effectively diagnose individuals even when there anti-body formation is lower. The IGENIX also searches the blood for genetic material of the Bb organism. So even if you aren’t producing anti-bodies this highly sensitive test should be able to identify the organism.
Total Cost: $658.00
(This test requires an additional blood draw fee which is typically between $20-$40)
If you live in New York or New Jersey, some lab testing may not be able to be completed. Please contact our team at (847) 222-9546 to verify that this request can be fulfilled.


Fortunately, because of the many thousands of newsletter readers and social media followers, my team has been able to network with a great lab distributor and get the best possible pricing for everyone.
The retail value (using market value and insurance based rates) is highly inflated and driving up the cost of health care. This is the old, archaic method that many people are still using and paying way more for insurance and co-pays than they really should be.
Many intelligent people are saving insurance premium dollars and turning to pay by order labs such as DirectLabs and others. These skip the middle man (doctors’ visits) and cut down costs for the patient.