 Gut Inflammation: Causes, Testing & Support Strategies
Gut Inflammation: Causes, Testing & Support Strategies
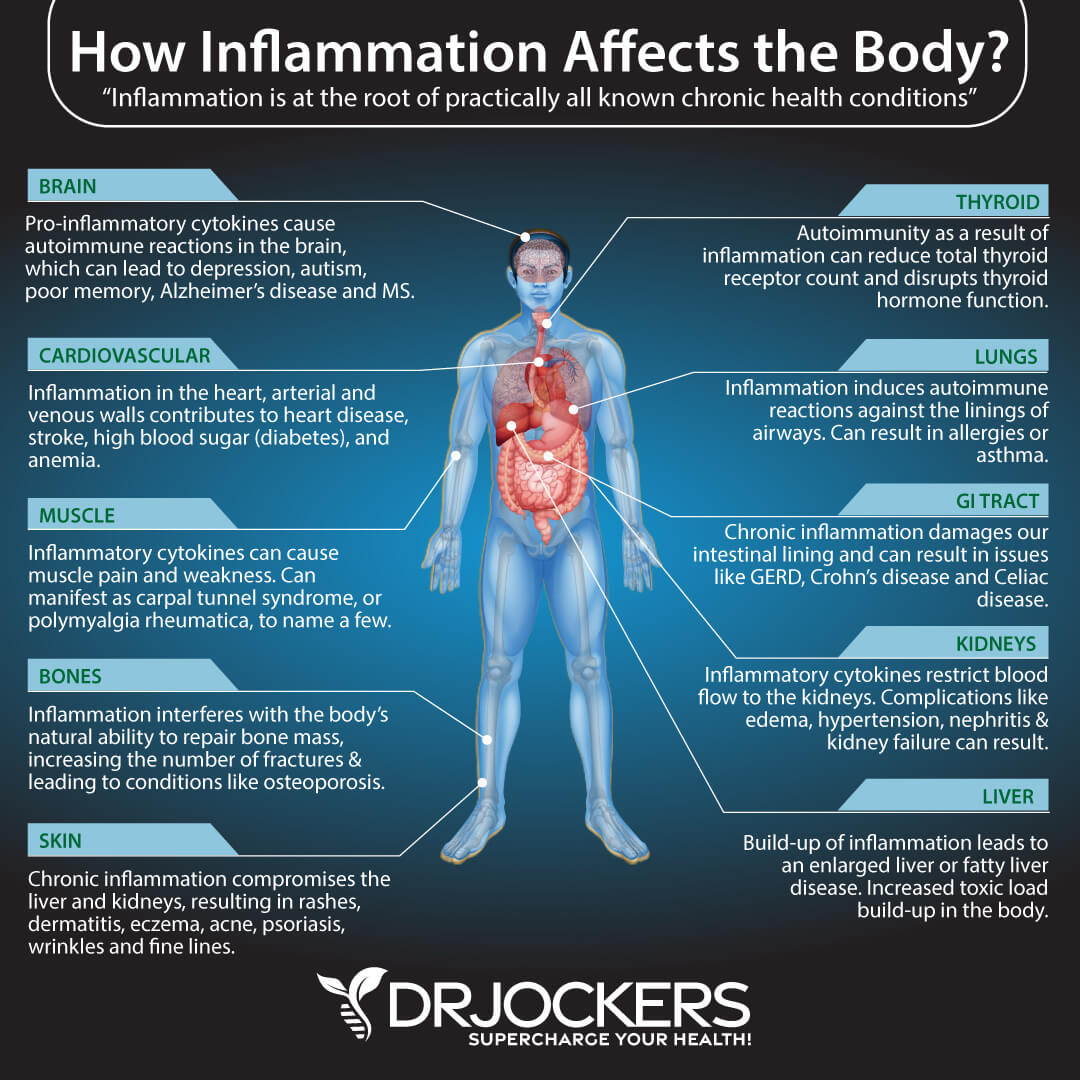
Your gut health affects your entire body, including your immune, brain, mental, and skin health, energy levels, and overall wellness. If you have gut inflammation and your gut health is compromised, you will start experiencing both gut health and non-gut health symptoms and health issues.
Gut inflammation can compromise your entire health. There is good news though. With the help of some testing and natural support strategies, you can reduce gut inflammation and related symptoms.
In this article, you will learn what gut inflammation is. You will understand the symptoms of gut inflammation. I will explain the connection between gut inflammation and leaky gut syndrome. You will learn about the root causes of gut inflammation. I will recommend some testing to identify the root causes of gut inflammation and related health issues. I will share my top natural support strategies to help you overcome gut inflammation and regain your health and wellness.
What Is Gut Inflammation
There are two types of inflammation: acute and chronic inflammation. Acute inflammation is a healthy and normal response from your body to any injury, allergen, infection, or illness. If you fall off your bike and scrape your knee, your body will start to generate inflammation. You will notice some redness, swelling, bruising, or pain. If you catch a respiratory infection or have seasonal allergies, your body will try to fight it with acute inflammation. You may experience some congestion, a sore throat, sneezing, irritation, red eyes, or watery eyes.
Acute infection is normal. As you recover, acute inflammation will subside and disappear. Acute inflammation will only last a day, a few days, or a few weeks, depending on the cause and severity. It will not result in ongoing, long-term problems.
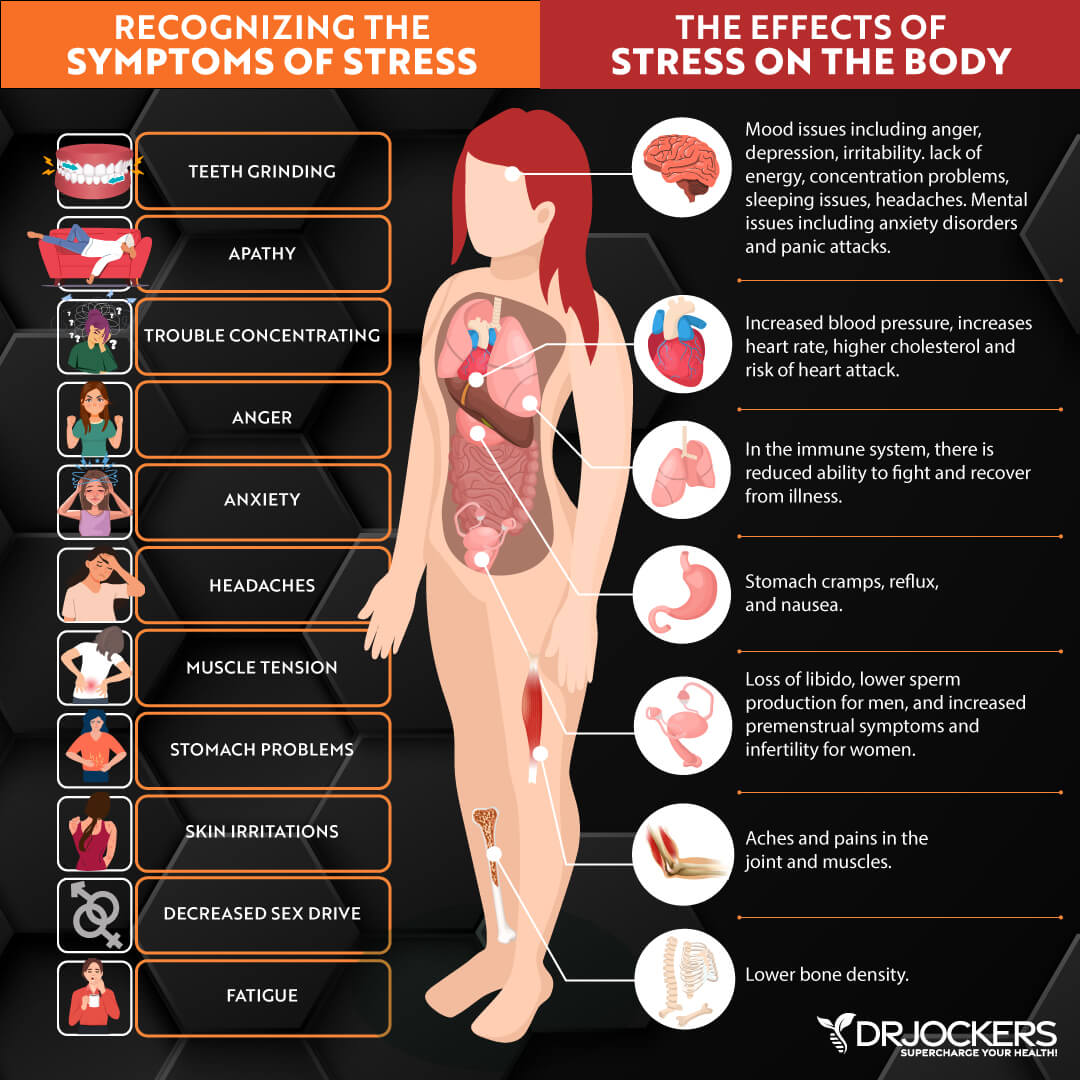
Chronic inflammation on the other hand is long-term, long-grade inflammation without a single specific triggering event or clear cause. Poor dietary and lifestyle choices, environmental factors, chronic stress, poor sleep, and other factors can result in chronic inflammation.
Chronic inflammation means that your body is experiencing triggers all the time and reacting with inflammation constantly. The problem is that chronic inflammation will lead to chronic symptoms and chronic health issues. In fact, chronic inflammation is one of the root causes of most major chronic diseases.
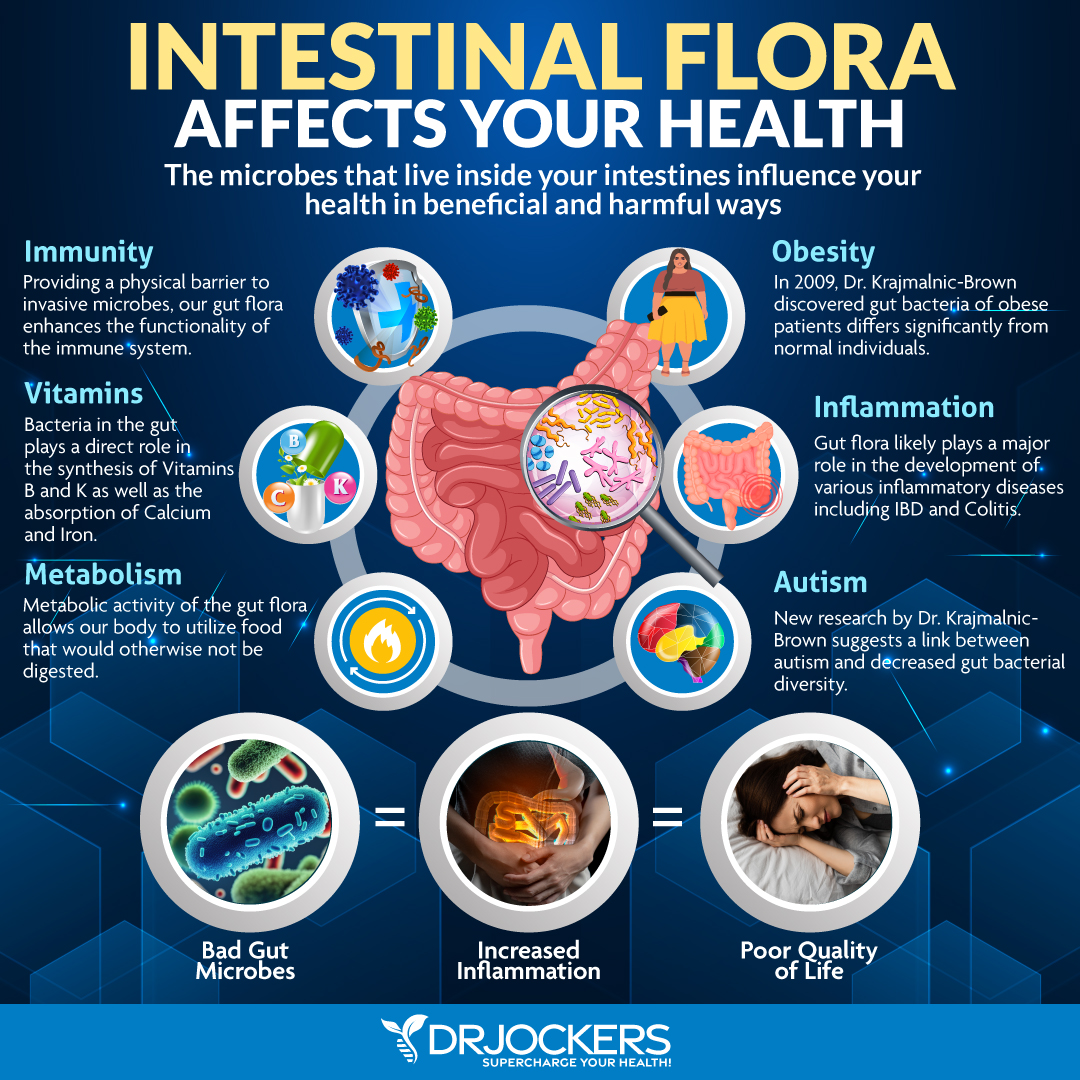
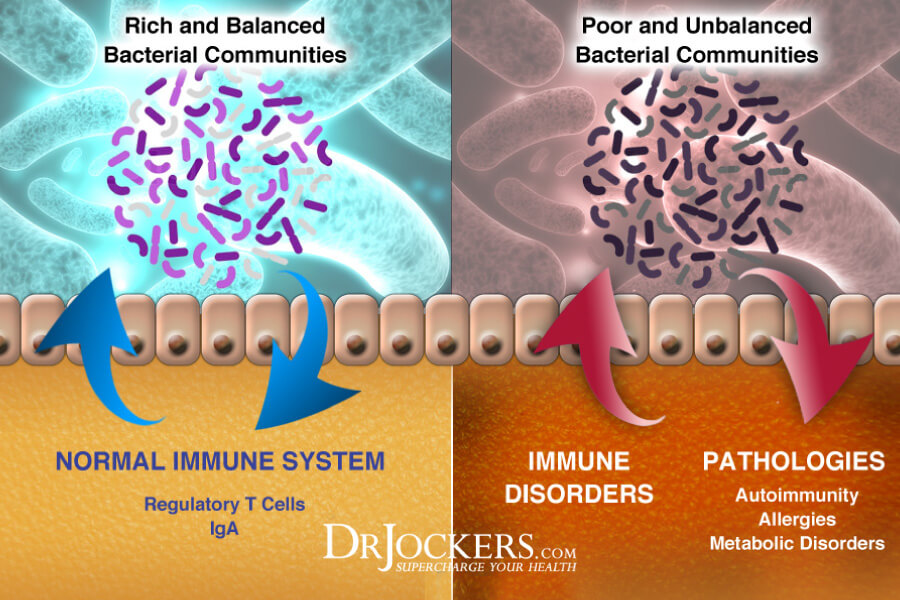
When we are talking about gut inflammation, we are talking about chronic inflammation affecting your gut. It means that your intestines become inflamed and are chronically inflamed. Chronic gut inflammation is also characterized by gut microbiome imbalance and an array of chronic gut health symptoms. Since your gut is connected to your entire body, chronic gut inflammation also increases the risk of chronic symptoms and health issues in other parts of your body.
Gut Inflammation Symptoms
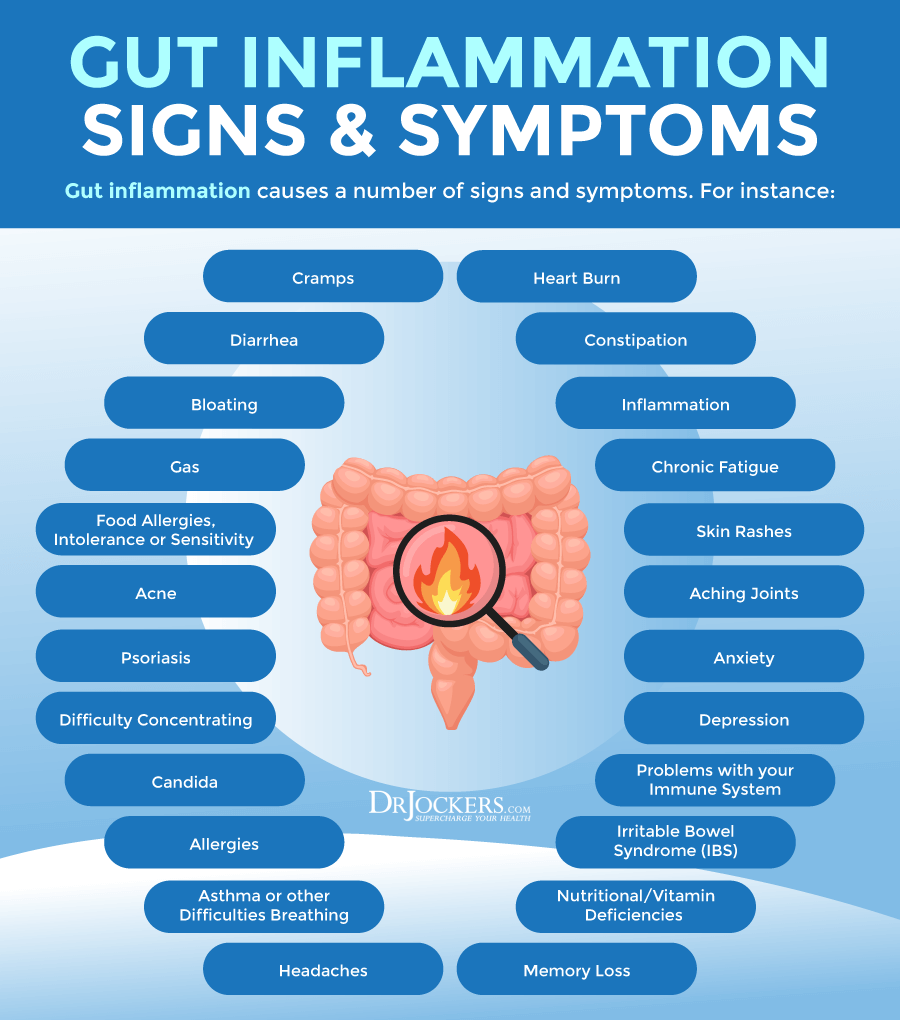
Symptoms of gut inflammation may include but are not limited to the following (1, 2):
- Abdominal pain or cramping
- Bloating
- Gas
- Diarrhea
- Constipation
- Nausea
- Vomiting
- Mucus in stool
- Unusual stool (eg. unusual color, texture, or smell)
- Mixed bowel habits
- Feeling of incomplete bowel movements
- Blood in stool
- Loss of appetite
- Unintentional weight loss
- Weight gain
- Sugar cravings
- Low energy
- Fatigue
Gut inflammation may also result in non-gut-related symptoms, including but not limited to the following (1, 2):
- Brain fog
- Headaches or migraines
- Skin issues
- Mouth sores
- Painful joints
- Allergies
- Redness or pain in the eyes
- Mental health issues
- Night sweats
- Menstrual changes
- Kidney stones
- Fever
Gut Inflammation & Leaky Gut Syndrome
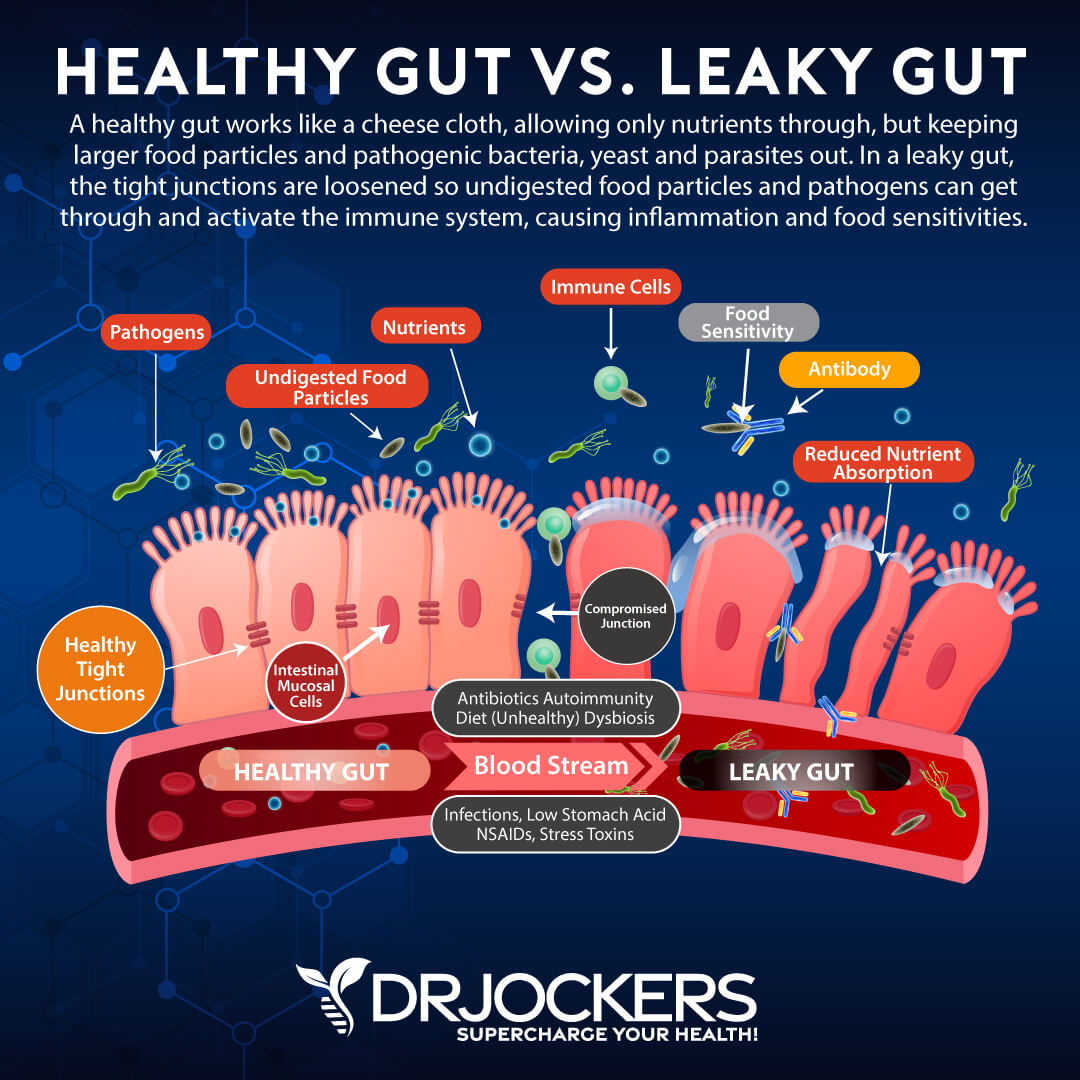
Your gut is critical for the breakdown, digestion, and absorption of nutrients from your food for repair, growth, energy, health, and well-being. It is also important for protecting you from pathogens, like bad bacteria, fungi, parasites, and toxins in your gut. If you have leaky gut syndrome, your gut health is compromised and can’t do its job.
Leaky gut syndrome develops when your intestinal barrier becomes leaky. Under normal circumstances, your intestinal barrier has tiny holes in it. They are large enough to allow water and nutrients to pass through but they are too small for invaders to enter your bloodstream. However, when due to chronic inflammation, a poor diet, poor lifestyle choices, toxin exposure, or chronic stress, these openings can become larger.
When these holes in your intestinal wall become too big, you develop leaky gut. This means that microbes, undigested food particles, and toxins can now escape into your bloodstream. While chronic inflammation is one of the underlying causes and triggers of leaky gut syndrome, leaky gut syndrome also feeds chronic inflammation, creating a vicious cycle.
Leaky gut syndrome can trigger chronic inflammation and an autoimmune reaction. It can result in digestive troubles, fatigue, brain fog, digestive troubles, skin problems, histamine intolerance, and autoimmunity. According to a 2015 study published in Intestinal Research, leaky gut syndrome plays a role in the development of inflammatory bowel disease (3). According to a 2019 study published in PNAS, leaky gut syndrome may cause autoimmune diseases, such as autoimmune diabetes mellitus (4).
Root Causes of Gut Inflammation
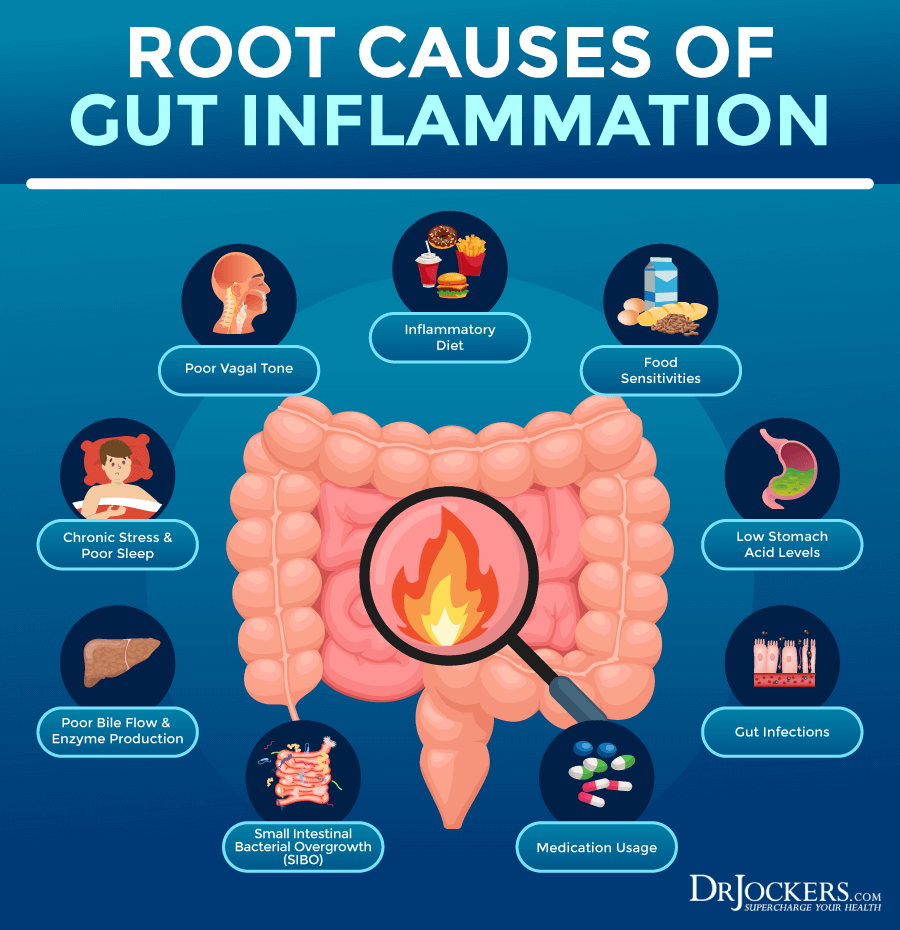
Gut inflammation may be a result of a variety of dietary, lifestyle, environmental, and health factors. Root causes of gut inflammation include:
Inflammatory Diet
Following an inflammatory diet high in refined sugar, refined oil, artificial ingredients, additives, gluten, processed foods, and junk food is one of the common root causes of any chronic inflammation, including gut inflammation. A 2021 study published in BMJ has found that dietary factors may determine the risk for gut inflammation (5).
Researchers examined 173 dietary factors in 1425 people divided into four groups, including those with Crohn’s disease, ulcerative colitis, irritable bowel syndrome (IBS), and those without gut health issues. They found that eating a diet high in processed foods, processed sugar, alcohol, and processed animal foods was associated with increased intestinal inflammatory markers, gut inflammation, and gut microbiome imbalance.
They also found that a whole food anti-inflammatory diet with lots of omega-3 fatty acids, vegetables, legumes, and fish may reduce intestinal inflammatory markers and lower the risk of gut inflammation and related diseases.

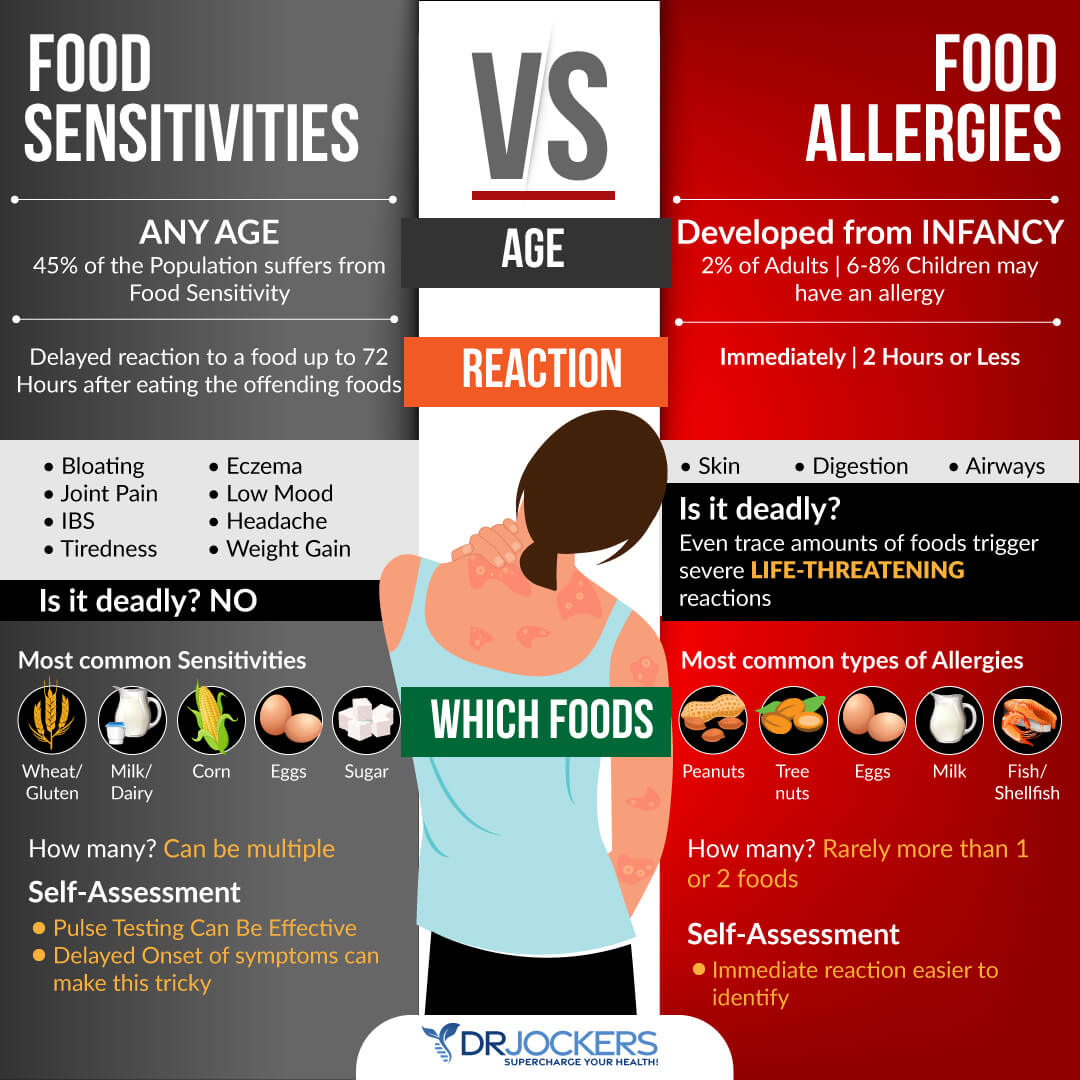
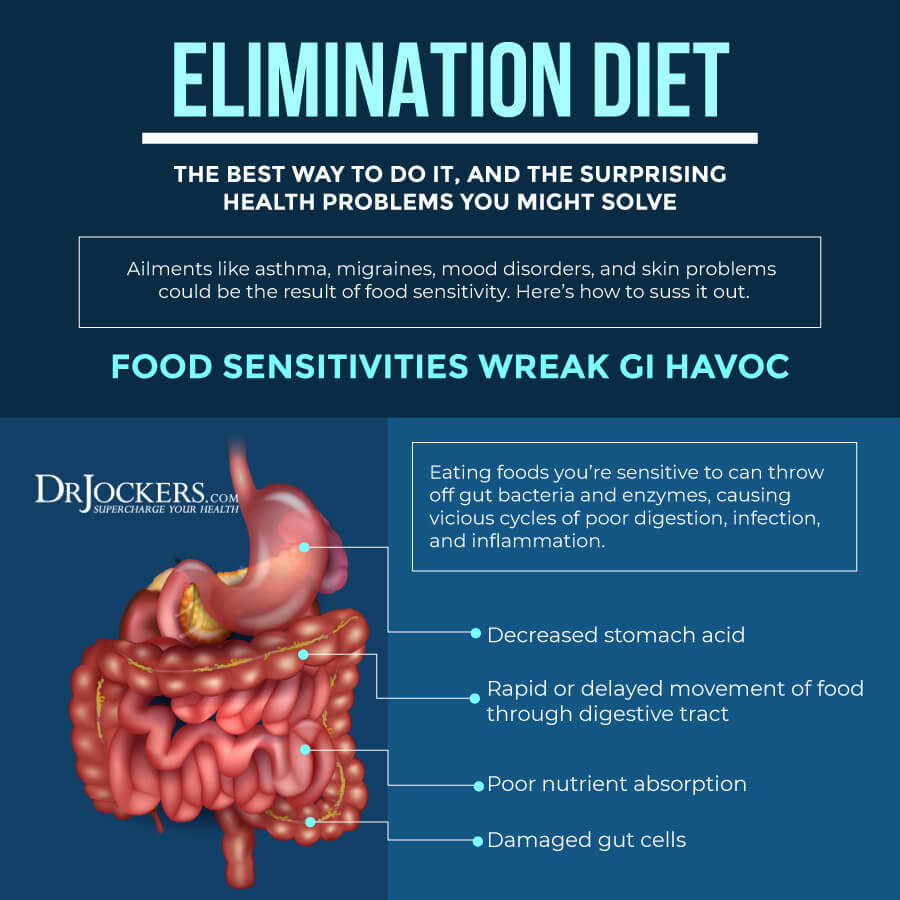
Food Sensitivities
Food sensitivities are another common cause of gut inflammation. Food sensitivities are different from food allergies. Food allergies result in an immediate reaction after eating a certain food, such as hives, swelling, difficulty breathing, or digestive issues. Food sensitivities don’t result in an immediate reaction but cause a delayed and milder response.
You may experience symptoms, like digestive issues, headaches, skin issues, or fatigue, hours or even days after eating a certain food without even connecting it to that food. When you are consuming food you are sensitive to regularly, you will experience chronic inflammation and chronic symptoms without realizing that it’s caused by the food you eat daily.
Common food sensitivities include gluten, dairy, sugar, corn, soy, legumes, shellfish, and eggs. However, you may be sensitive to a less common food item that may even be healthy for most people. Food sensitivities may also change over time. You may become sensitive to a food that you were able to eat without a problem only a year ago.
When it comes to gut inflammation, gluten is often a common culprit. According to a 2016 study published in Tissue Barrier, gluten triggers the release of zonulin, which is a protein that causes the breakdown of tight protein junctions between intestinal epithelial cells (6). This can result in gut inflammation and leaky gut syndrome. Additionally, according to a 2019 study published in the International Journal of Molecular Sciences, gluten also causes the activation of your mast cells, which release histamine increasing the risk of gut inflammation (7).
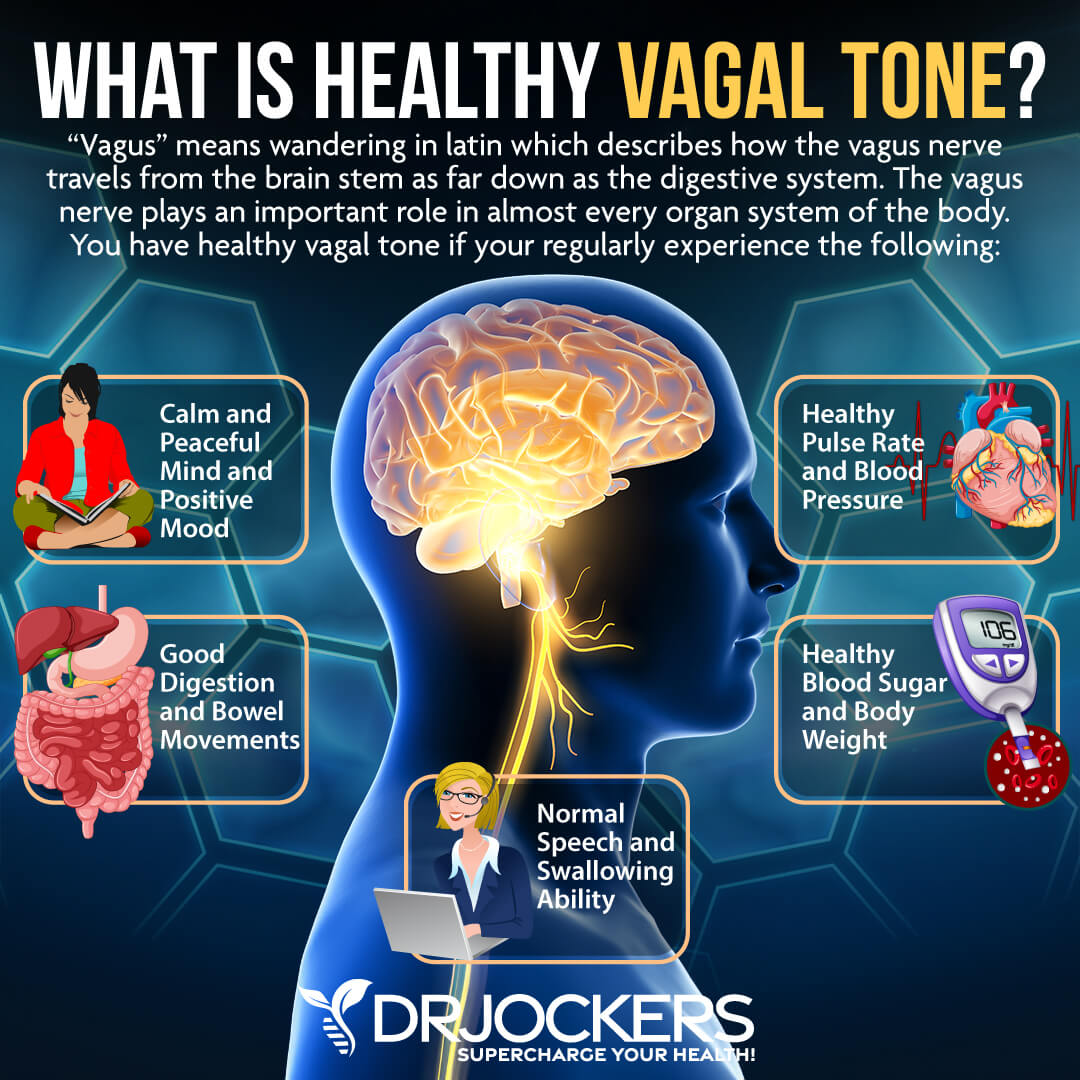
Poor Vagal Tone
Your vagus nerve is the tenth cranial nerve. It is your body’s major parasympathetic nerve that helps to slow your heart rate, control gag reflex, allow involuntary constriction and relaxation of the muscles of your gut, control sweating, regulate blood pressure, and control vascular tone. Vagal tone is the activity of the vagus nerve.
Excessive vagus nerve function can lead to a variety of nervous system issues and present in dysautonomias, such as postural orthostatic tachycardia syndrome (POTS). Vagus nerve stimulation can result in sudden stress, sudden blood pressure drop, slow heart rate, and gastrointestinal symptoms.
Poor vagal tone can also lead to mental and emotional health issues, such as anxiety, panic attacks, and depression. It may play a role in a variety of health issues, including migraines, headaches, tinnitus, hypertension, fibromyalgia, weight problems, and inflammatory issues.
Your vagal tone is also connected to your gut health and poor vagal tone can result in gut inflammation and gut health issues. Your brain and gut are connected through nerve activity. Your vagus nerve is one of the main nerves that play a role in this connection.
Stress can interfere with signaling from your vagus nerve and cause gastrointestinal symptoms. A 2014 study published in PLoS One has found that people with conditions characterized by gut inflammation, such as IBS and Crohn’s disease, tend to have reduced vagus nerve function and poor vagal tone (8).
Chronic Stress & Poor Sleep
Chronic stress and poor sleep are two major lifestyle factors that can increase chronic inflammation in your body and, therefore, increase the risk of gut inflammation. A 2017 study published in Oxidative Medicine and Cellular Longevity has found that a sedentary lifestyle can increase inflammatory molecules in the gut while exercise can improve the gut microbiome and reduce inflammation (9). A 2015 review published in Exercise Immunology Reviews has found that exercise can improve the gut microbiome and gut health (10).
A 2018 study published in Frontiers in Microbiology has found that the interruption of the body’s natural circadian rhythm or sleep-wake cycle can disrupt the health of the gut microbiome, increase the growth of inflammatory gut bacteria, discourage the growth of beneficial gut bacteria, and increase the risk of leaky gut syndrome (11).
According to a 2016 study published in Molecular Metabolism, only two nights of poor, short sleep can increase pro-inflammatory gut bacteria growth (12). According to a 2009 study published in Sleep Medicine, poor sleep and sleep deprivation can worsen gut inflammation and interfere with recovery from gut inflammation related to colitis.
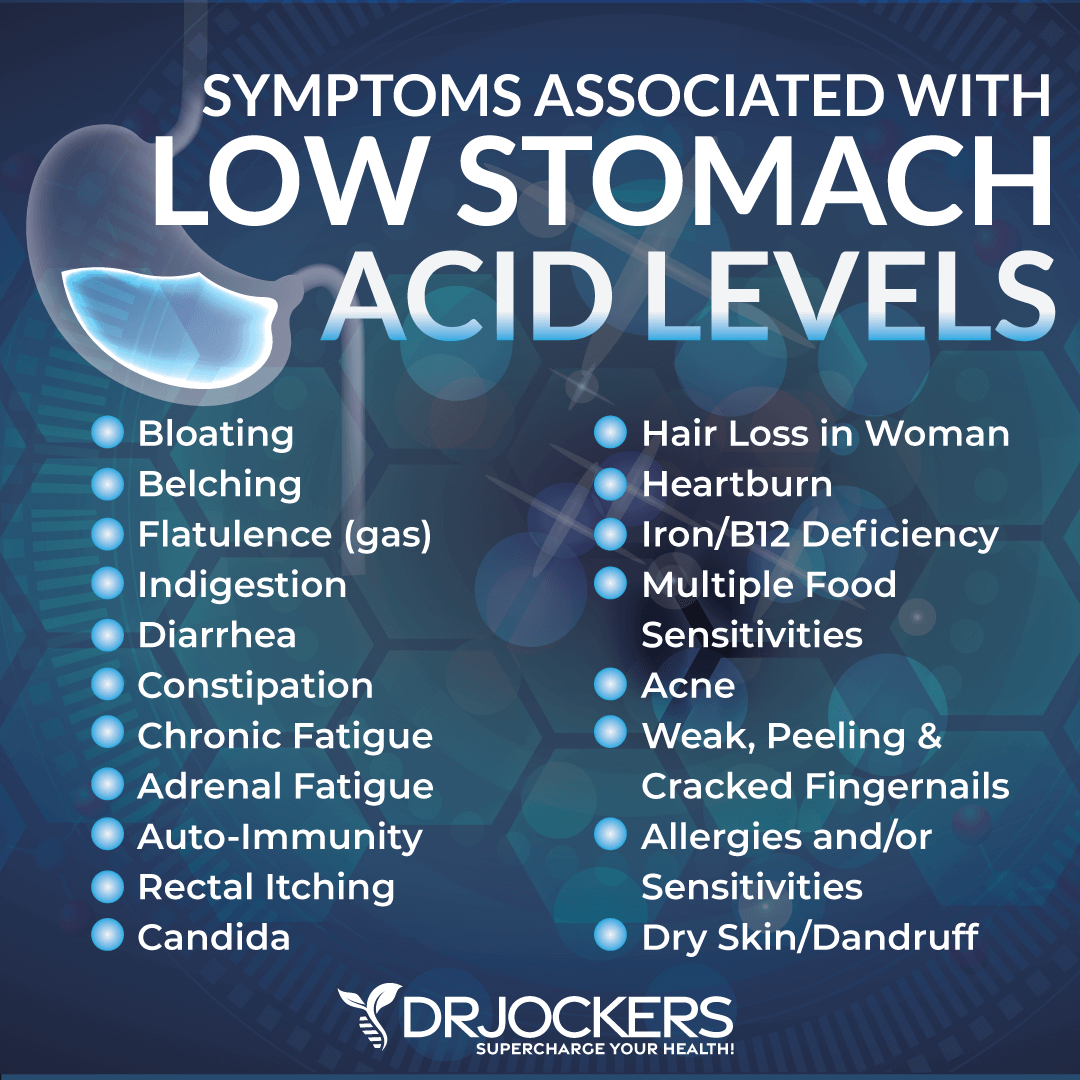
Low Stomach Acid Levels
Stomach acid is important for disinfection, killing of microbes, and optimizing digestion. When your body is unable to produce enough stomach acid and you have low stomach acid, it can set you up for microbial overgrowth, poor digestion, nutrient deficiencies, gut inflammation, and gut health issues.
According to a 2008 study published in Infection and Immunology, low stomach acid can increase your risk of bacterial pathogen overgrowth, gut infections, and consequently, gut inflammation (13). Low stomach acid production is very common in individuals as they get older or if they have dealt with infections or chronic stress in the past.
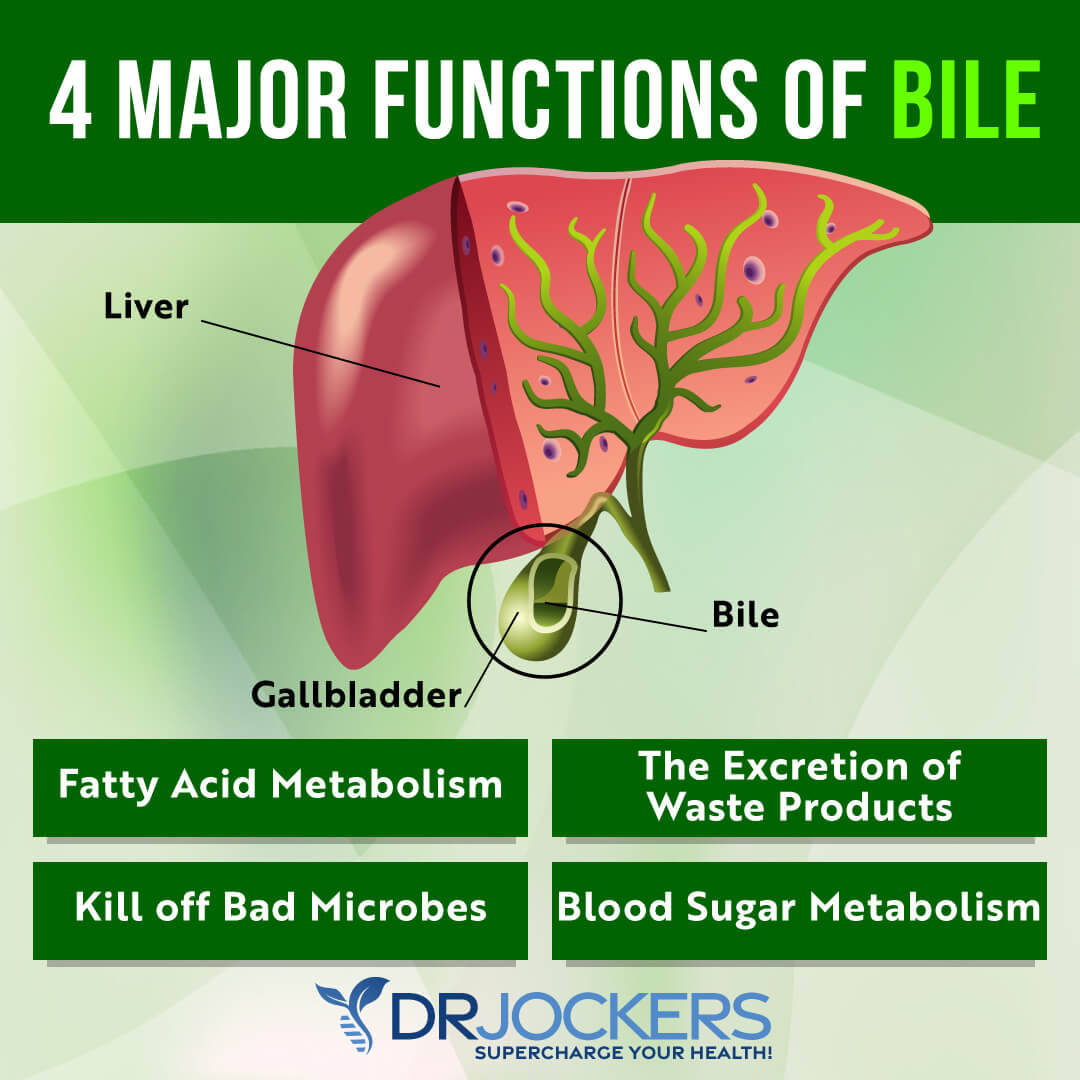
Poor Bile Flow & Pancreatic Enzyme Production
Bile is produced by your gallbladder. It is a greenish-brown liquid primarily made of cholesterol, bile salts, and bilirubin. It’s a digestive secretion that helps to digest fats. However, it’s important for your overall digestion and gut health. Pancreatic enzymes are secreted by your pancreas to break down fats, protein, and carbohydrates.
Problems with both bile flow and pancreatic enzyme production can result in gut inflammation. A 2018 study published in the Annals of Gastroenterology has found that poor bile flow can contribute to the development of inflammatory bowel disease (IBD) (14). A 2018 review published in the Journal of Clinical Medical Research has found that pancreatic dysfunction may be linked to IBDs (19).
Gut Infections
H Pylori, parasites, yeast, bacterial, and viral infections can all increase the risk of gut inflammation. A 2019 study published in FEBS Open Biology has found that H Pylori infection can cause pro-inflammatory bacteria growth in the gut and gut inflammation (16). A 2018 study published in Frontiers in Immunology has found that viral infections, including respiratory viral infections and secondary bacterial pneumonia, can also alter the gut microbiome and cause gut inflammation (17).
A 2019 study published in Peer Journal has found that parasitic infections can disrupt the gut microbiome health resulting in gut inflammation (18). A 2019 randomized control trial published in Digestive Diseases and Sciences has found that even a short, acute food poisoning incident can trigger gut inflammation, inflammatory autoantibody production, and the development of IBS (19).
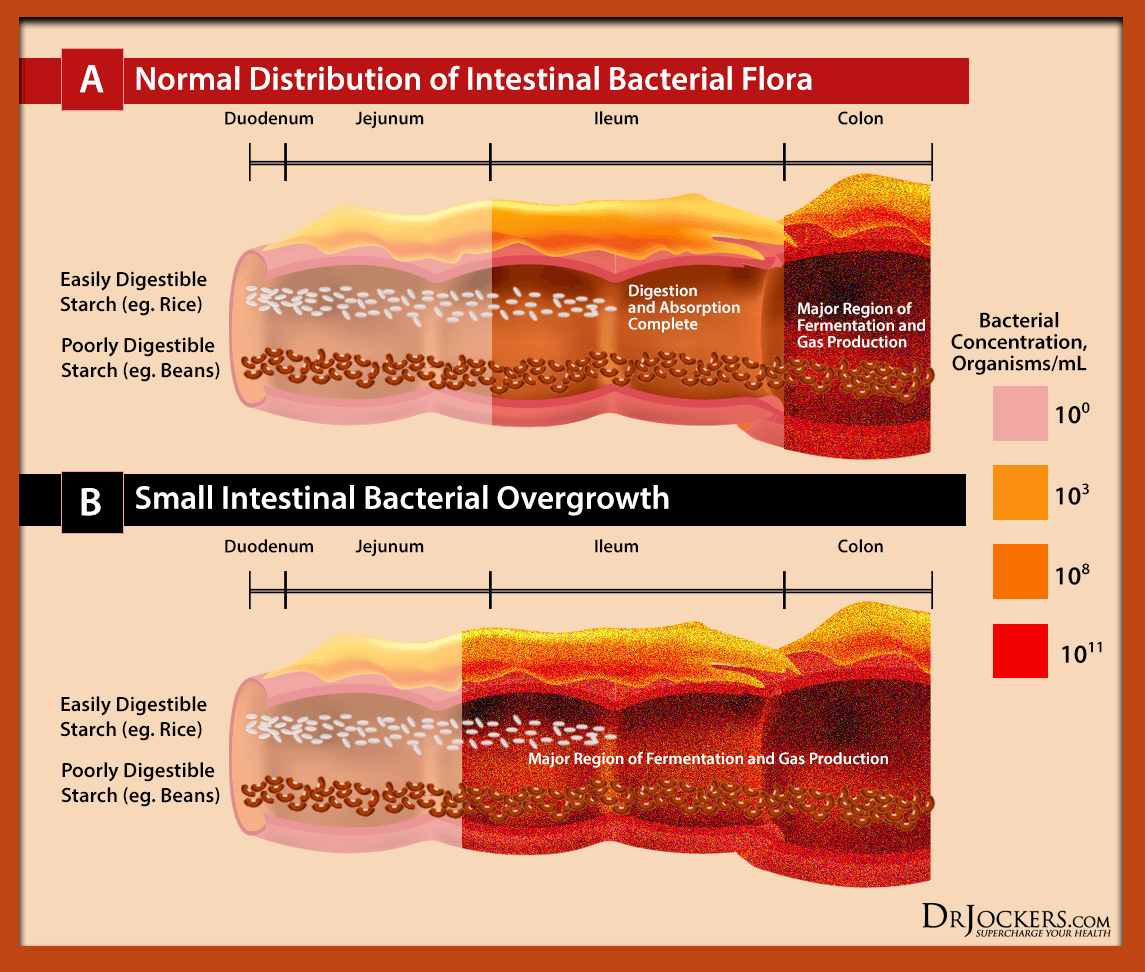
SIBO
Small intestinal bacterial overgrowth or SIBO refers to bacterial overgrowth in your small intestines. SIBO is characterized by abdominal pain, bloating, constipation, diarrhea, fatigue, malnutrition, food sensitivities, and a list of other chronic issues.
According to a 2007 review published in Gastroenterology and Hepatology, the excess bacteria presence in SIBO can trigger an intestinal inflammatory response and cause gut inflammation (20). This gut inflammation can cause even further microbial imbalance and bad bacterial overgrowth resulting in a vicious cycle and chronic gut health issues.
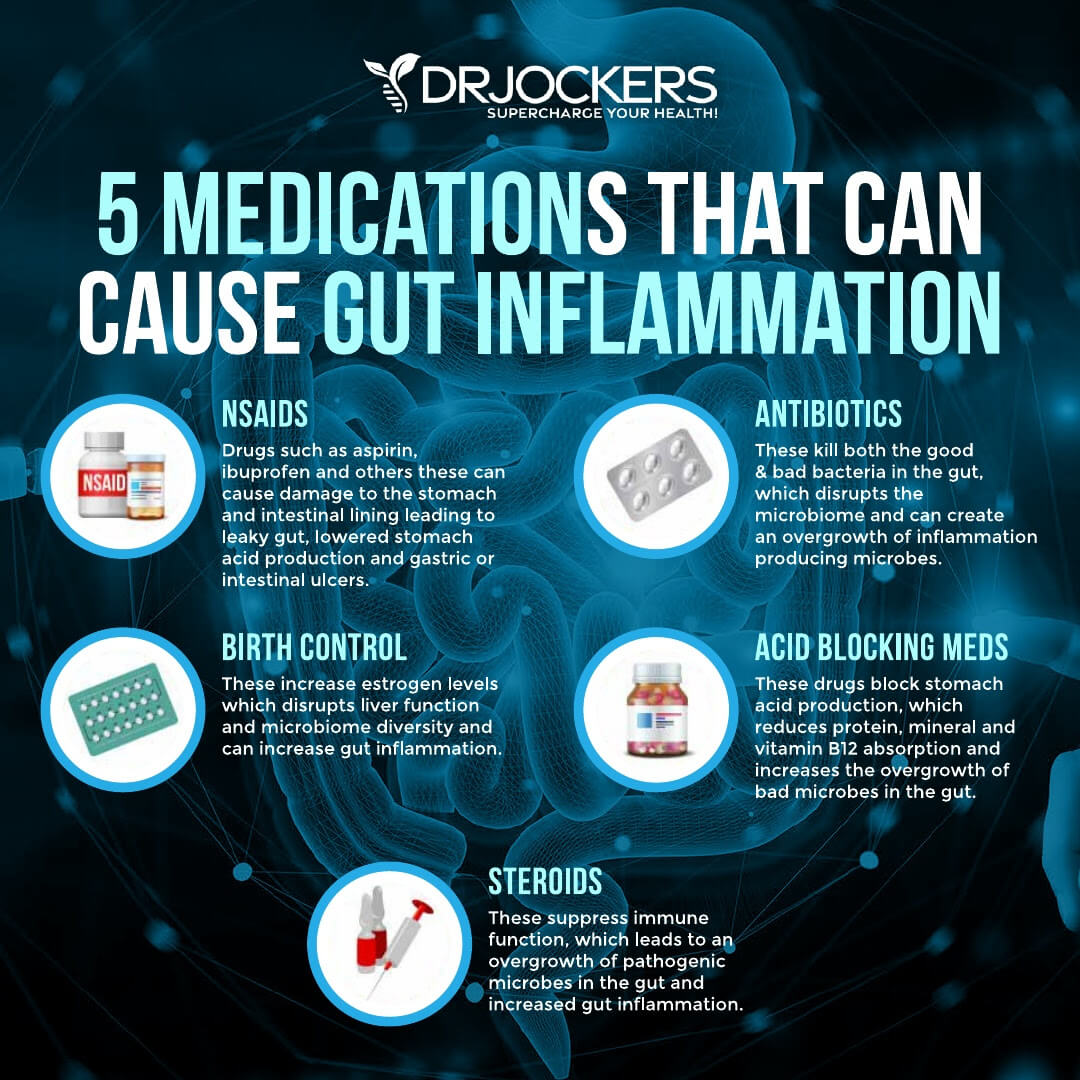
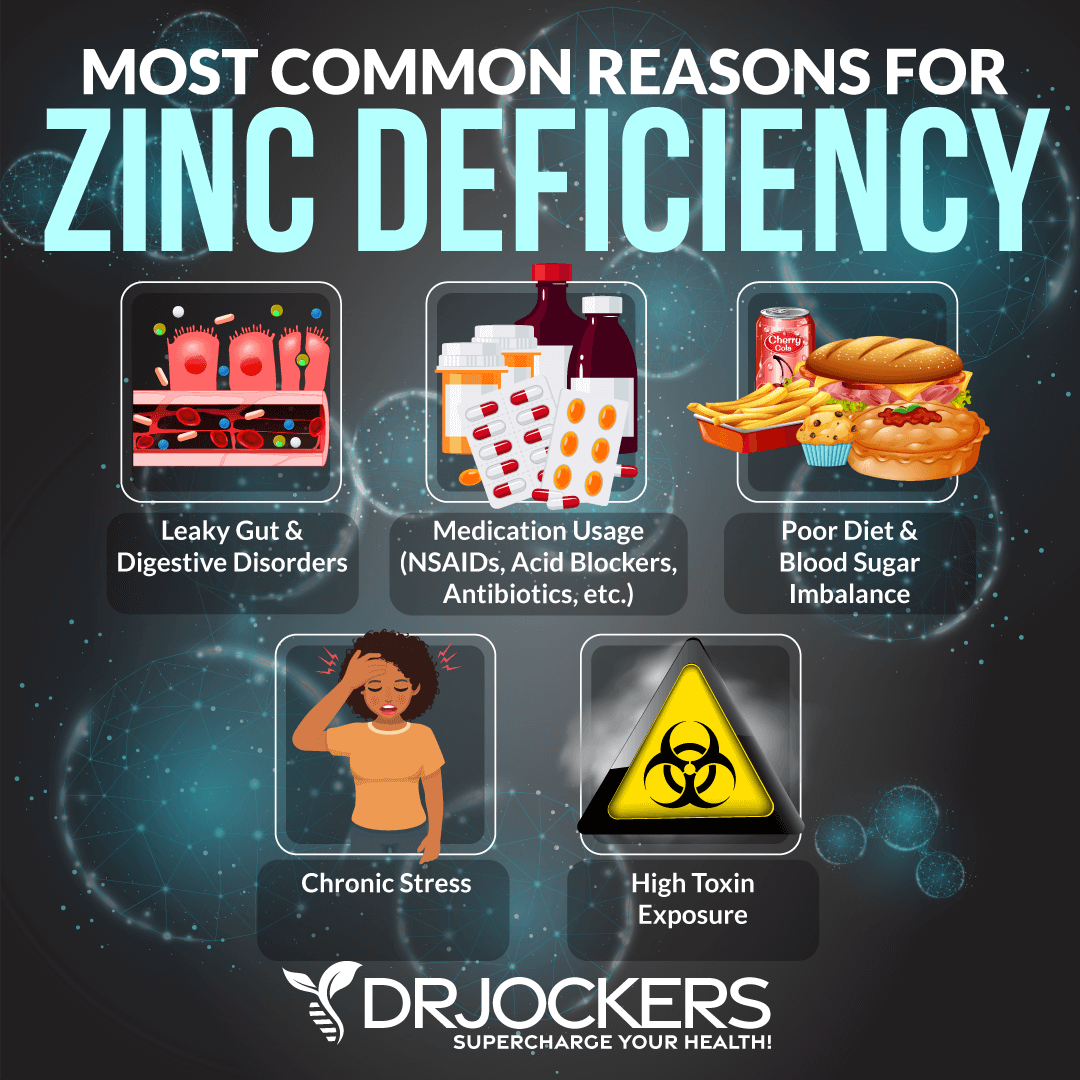
Medications
The use and overuse of certain medications can increase the risk of gut inflammation. Some of these medications that may lead to gut inflammation and related issues include antibiotics, proton pump inhibitors (PPI’s), selective serotonin reuptake inhibitors (SSRIs), non-steroidal anti-inflammatory drugs (NSAIDs), and oral contraceptives.
Antibiotics are designed to fight bacterial infections. However, as a 2018 study published in Yonsei Medical Journal explains, they also clean out gut bacteria leading to gut flora imbalance and the risk of inflammation (21). A 2015 study published in PLoS One has found that antibiotics can also increase the risk of leaky gut syndrome and gut inflammation (22).
A 2019 study published in Scientific Reports has found that PPIs used long-term can decrease good, anti-inflammatory gut bacteria and increase bad bacteria overgrowth and gut inflammation (23). A 2019 study published in Peer Journal has found that SSRIs can increase the risk of gut dysbiosis and inflammation (24).
A 2015 study published in Clinical Microbial Infections has found that NSAIDs can also disrupt the gut microbiome and increase the risk of gut inflammation (25). Lastly, a 2016 study published in Gastroenterology has found that long-term use of oral contraceptives may increase the risk of gut inflammation and complications in Crohn’s disease (26).
Gut Inflammation Testing Strategies
To check if you are dealing with gut inflammation and identify gut-related root causes of your symptoms and health problems, I recommend several gut inflammation testing strategies.
GI MAP
My favorite test to look at your gut health and identify gut inflammation, bacterial pathogens, parasitic pathogens, viral pathogens, normal flora, dysbiotic flora, potential autoimmune triggers, and all intestinal health markers is the GI Map Stool Analysis. This test looks for gut function markers, such as calprotectin, zonulin, and sIgA.
Calprotectin can detect gut inflammation and markers associated with gut infections, irritable bowel syndrome, and inflammatory bowel diseases. Zonulin is used as a biomarker for an impaired gut barrier, leaky gut syndrome, autoimmune diseases, cancer, and neurodegeneration.
Secretory IgA (sIgA) looks at markers of mucosal immunity, immunological reactions to pathogenic infections, and signs of gut inflammation. This is the best and most comprehensive gut test I have found and it helps me tremendously to identify the root cause of my patients’ health issues and help them to repair their body and regain their health naturally.
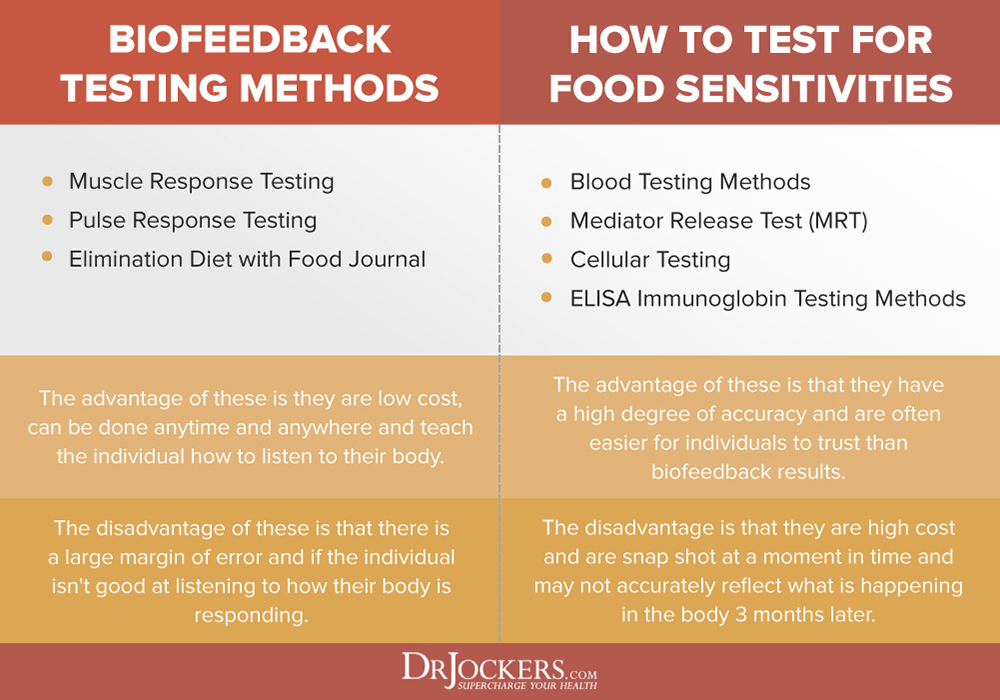
Food Sensitivities
I also recommend food sensitivity testing. There are many blood tests for food sensitivities are on the market. The best one I could find and often recommend to my patients is the Advanced Food and Chemical Sensitivities test. However, it’s impossible to test for every single food through a blood test.
I also recommend that you try a Pulse Test or Muscle Response Testing. These two biofeedback tests should help you to identify your food sensitivities and get to know your body better. Additionally, I also recommend an elimination diet to spot your food sensitivities for certain. Since food sensitivities can change over time, I recommend repeating testing once a year or if new symptoms arise.
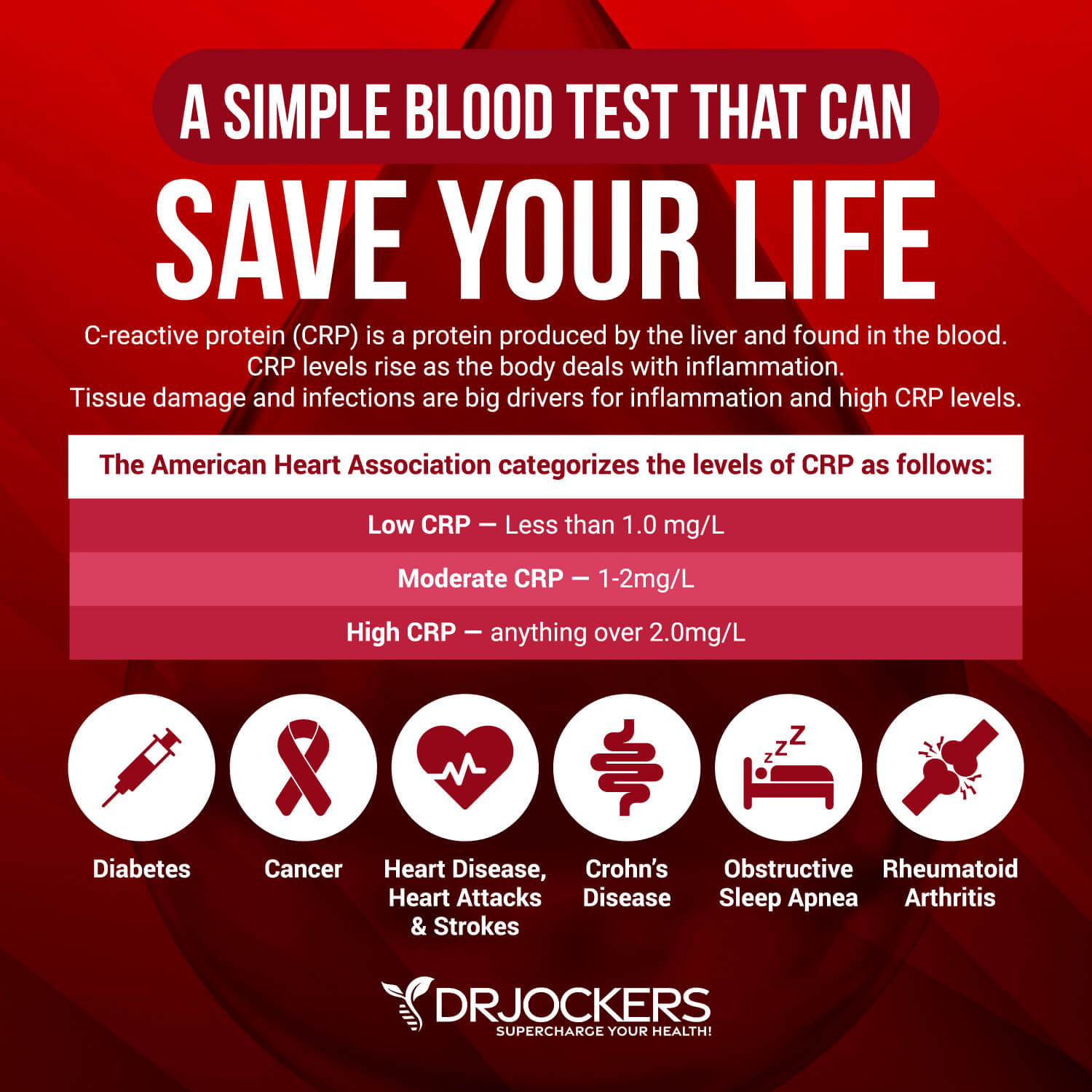
Blood Markers for Inflammation
I recommend several blood markers for inflammation, including. hs-CRP, ESR, serum ferritin, and liver enzymes.
Hs-CRP
The C-Reactive Protein or CRP test is a key test I recommend. It measures a protein (CRP) produced in your liver that indicates inflammation levels in your body. The clinical range is between 0 and 3 mg/L while the optimal range is 0 to 1 mg/L.
When I see levels over 1 mg/L, I know the individual is having an inflammatory response that could be due to acute trauma or chronic conditions.
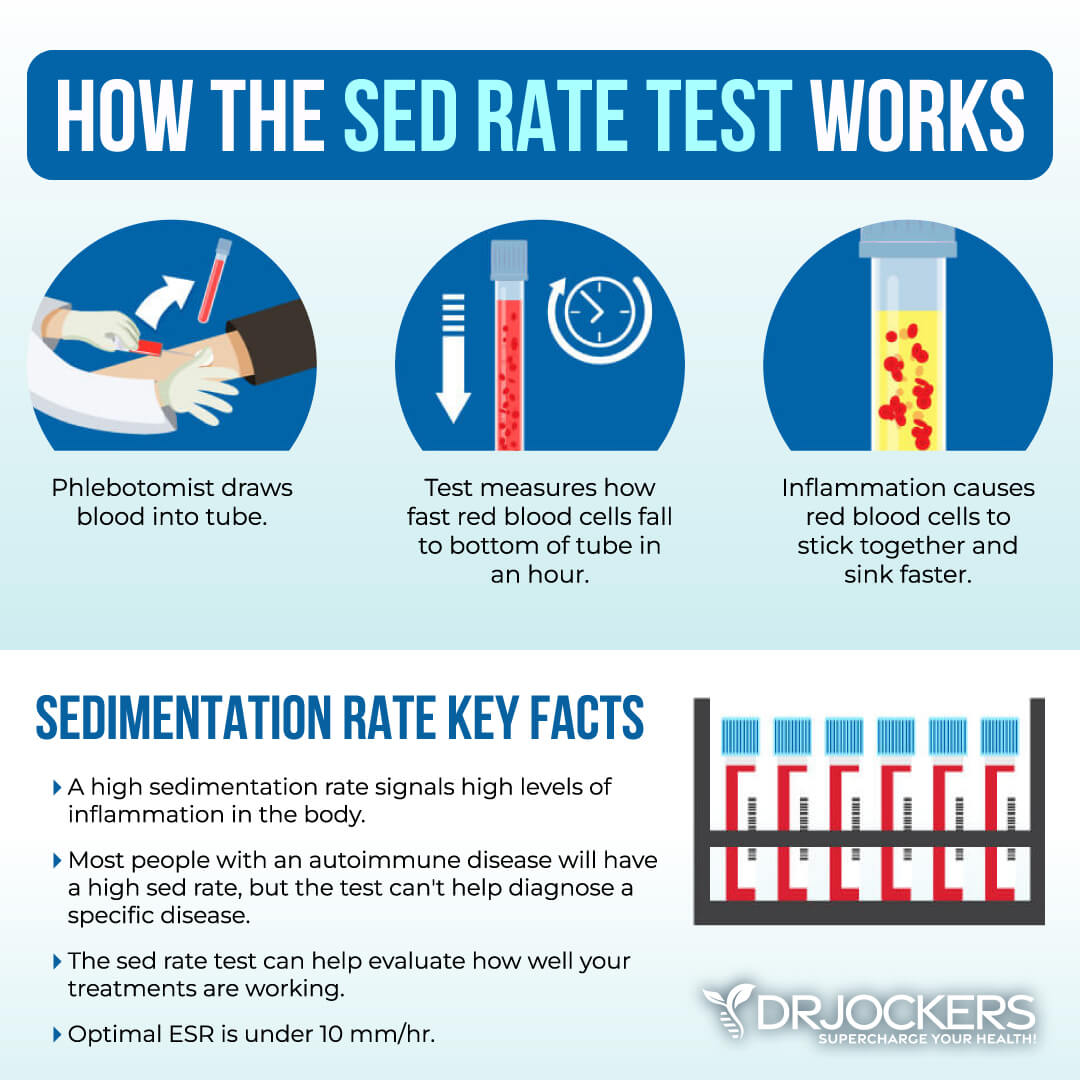
ESR
The erythrocyte sedimentation rate (ESR) is a common hematology test to look for inflammation. It refers to the rate at which your red blood cells in anticoagulated whole blood go down in a standardized tube over a period of one hour. Anything over 20 mm/hr is a sign of significant inflammation and optimal results should be under 10 mm/hr.
You can also look at platelets as a measurement tool for inflammation and the stickiness of blood. Platelets elevated above 250 is a sign of inflammation. The sweet spot for platelets is between 175 and 250. Below 175, immune function and blood clotting are compromised; the same is true for levels above 250.
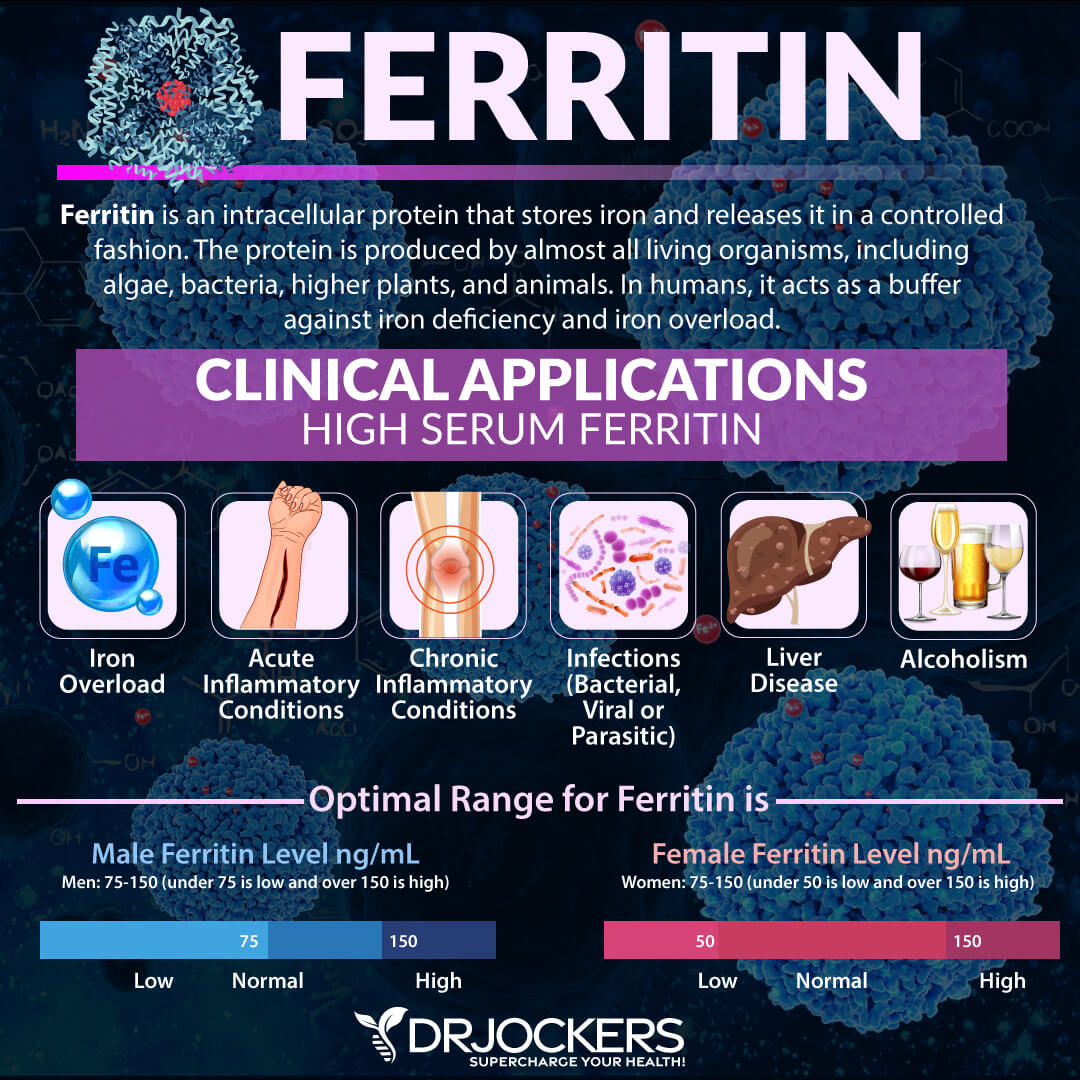
Serum Ferritin
Serum ferritin measures the level of ferritin in your body to detect iron deficiency anemia and other health issues. Elevated serum ferritin levels may indicate inflammation, liver disease, autoimmune disease, or even cancer.
The clinical range is 30 to 400 and the optimal range is 50 to 150 for females and 75 to 150 for males. Anything over 150 may be an indication of gut inflammation.
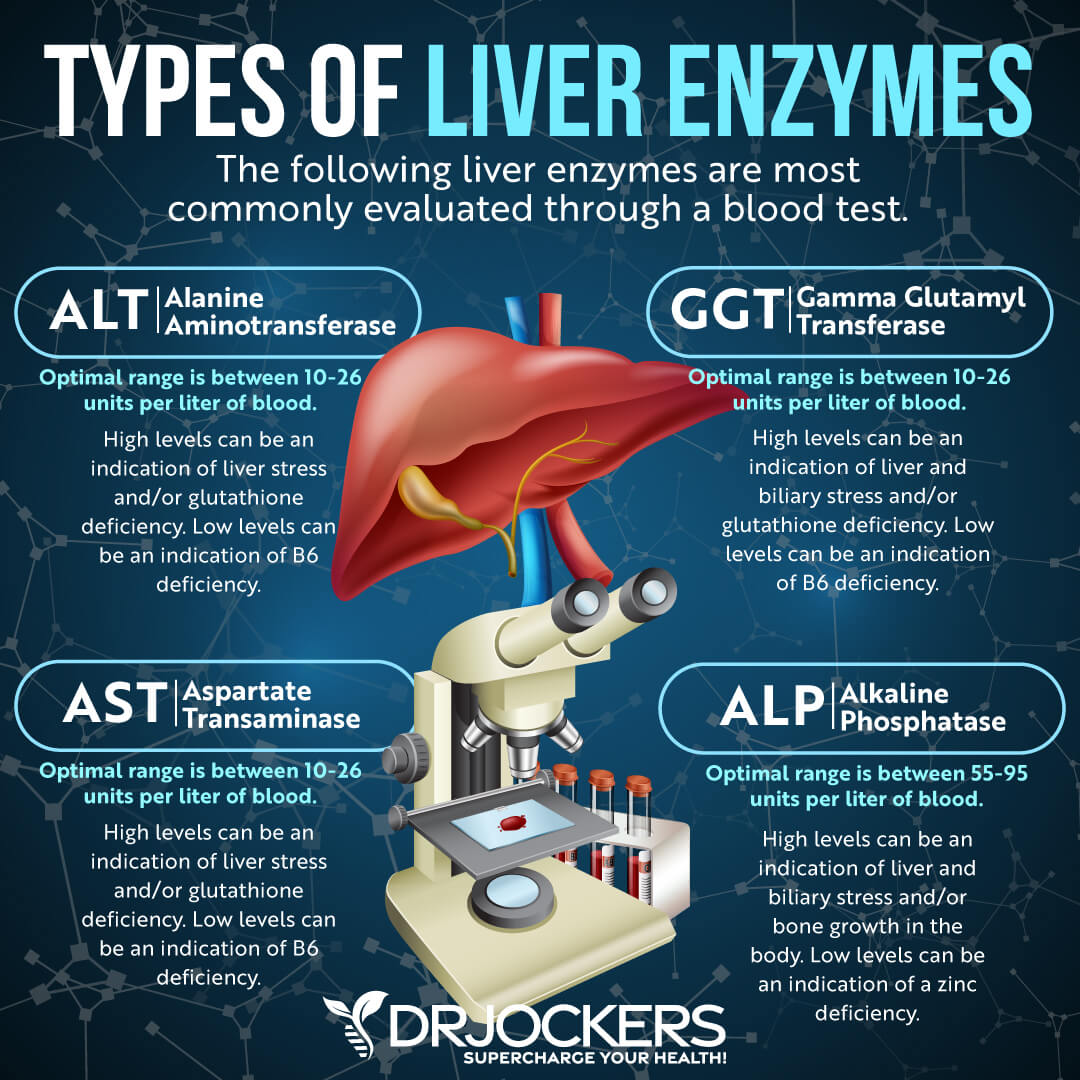
Liver Enzymes
Liver enzyme levels may also indicate inflammation, as well as liver, gallbladder, bile, or kidney issues. Alkaline phosphatase is a liver enzyme that is made by the mucosal cells that line the bile system of the liver and help normal bile flow. Elevated levels (over 95) may indicate inflammation and liver and gallbladder problems.
Alanine aminotransferase (AST) is a liver enzyme. Elevated levels may indicate inflammation. Normal levels are between 10 and 26 IU/L.
Aspartate transaminase (ALT) is an enzyme present in the liver that spills out during times of increased liver stress. Elevated levels may indicate inflammation Normal levels are between 10 and 26 IU/L.
Gamma-Glutamyl Transpeptidase (GGT) is an enzyme in the liver, pancreas, and kidneys. Elevated levels may indicate inflammation and liver disease, usually due to alcoholism and/or sluggish gallbladder or gallstone obstruction. Normal levels are between 10 and 26 IU/L. Levels lower than 10 IU/L can be an indication of a vitamin B6 deficiency.
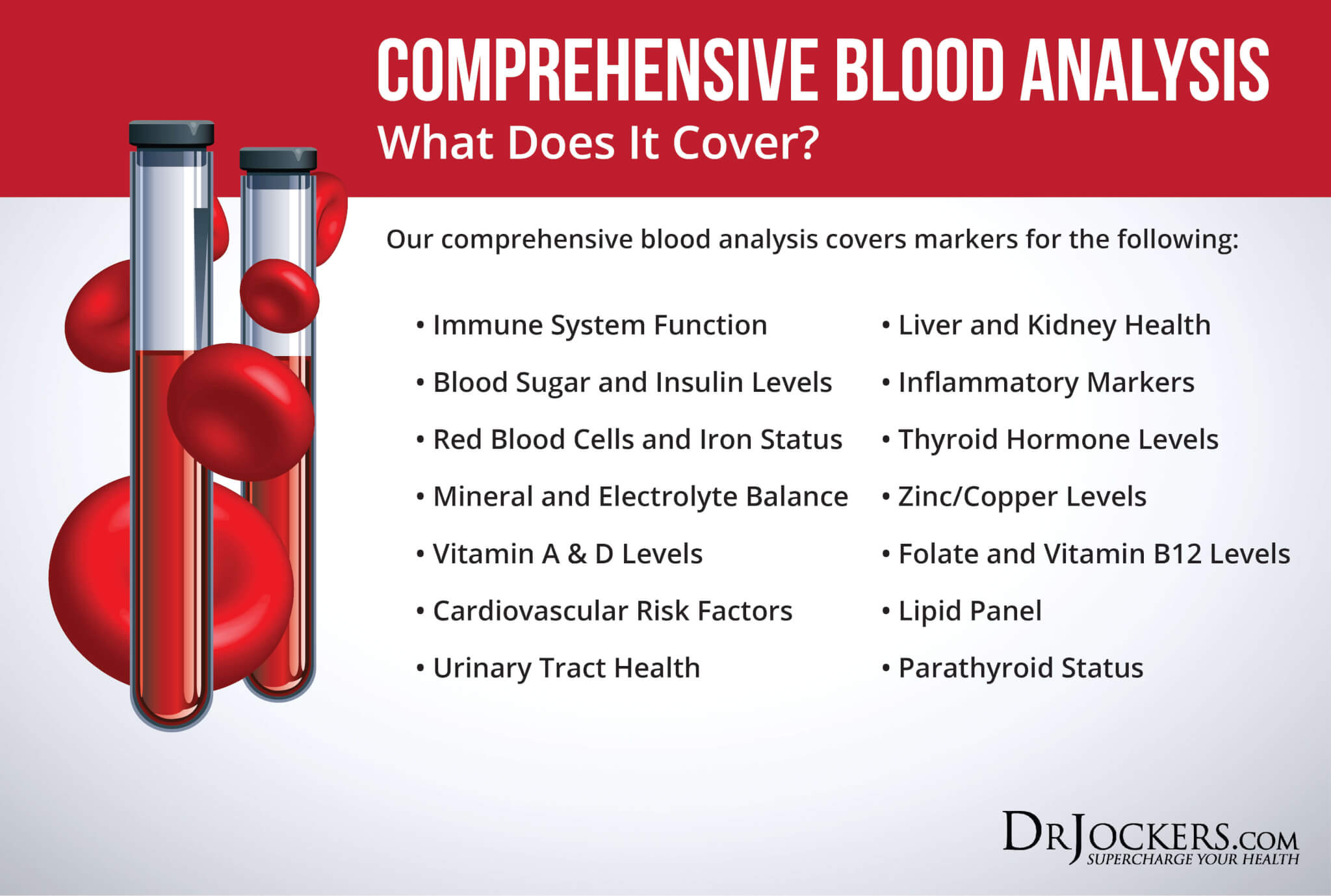
Comprehensive Blood Analysis
To check for these health markers, I recommend a Comprehensive Blood Analysis (CBA). This is the most detailed blood test that looks at all of these markers of inflammation. This test is more sophisticated than most conventional doctors are able to order.
It examines all parameters for inflammation, blood sugar levels, thyroid function, zinc and copper ratio, vitamin A and D levels, a complete metabolic panel, complete blood count, liver function, nutrient deficiencies, and more. I recommend getting the Comprehensive Blood Analysis done regularly both as a preventative measure and to monitor your inflammation levels and progress.
Home Testing
Finally, I also recommend several home tests for stomach acid, enzymes, bacterial overgrowth, and bile flow. These tests are simple, affordable, and easy to perform in the comfort of your home with the help of some foods that you already have in your kitchen.
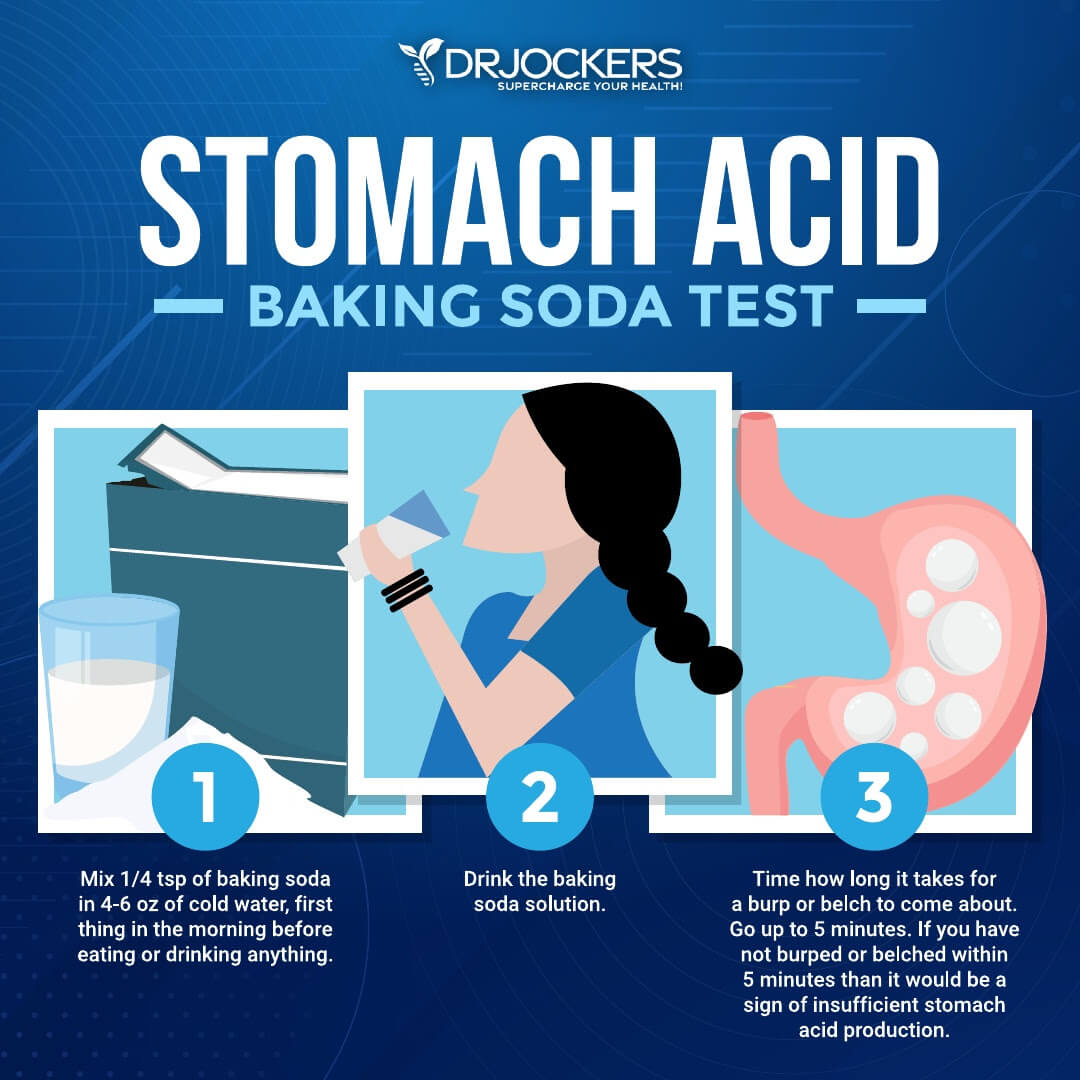
Baking Soda Test for Stomach Acid
I recommend the Baking Soda Test for stomach acid levels. Mix ¼ teaspoon of baking soda with 4–6oz of cold water and drink it first thing in the morning before drinking or eating anything. It should make you burp or belch. Time how long it takes for you to burp or belch. If it takes longer than 5 minutes, your body likely produces insufficient stomach acid.
If you burp or belch very early or several times, it may be due to too much stomach acid. Make sure not to confuse these with small burps from swallowing air from drinking too quickly. If you belch after 3 minutes, you may have low stomach acid levels. You may read more about this strategy here.
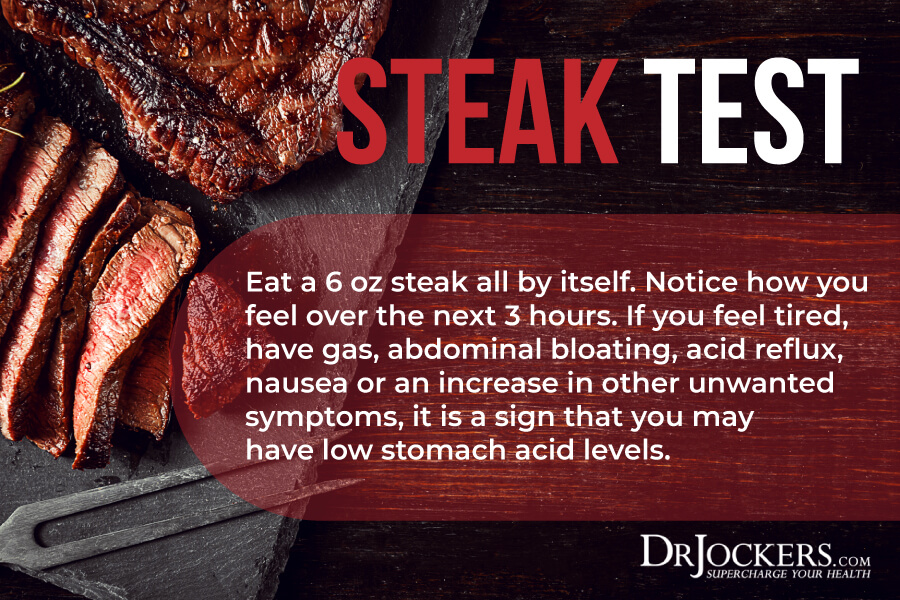
Steak Test for Stomach Acid
Another test I recommend for stomach acid is the Steak Test. Eat a steak all by itself and see how you feel over the next 3 hours.
If you feel tired, have acid reflux, nausea, gas, bloating, or other symptoms, you may have low stomach acid. If you feel great after eating a steak, you likely have optimal stomach acid levels.
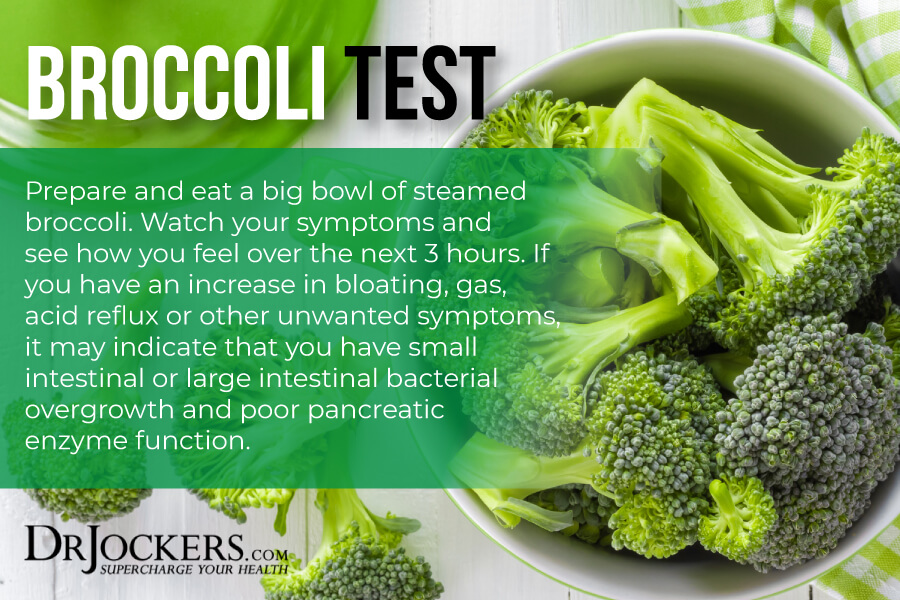
Broccoli Test for Enzymes & Bacterial Overgrowth
I recommend the Broccoli Test for enzyme levels and bacterial overgrowth. Have a big bowl of steamed broccoli and see how you feel over the next 3 hours.
If you have gas, bloating, cramping, acid reflux, or other digestive symptoms, it means that you may be experiencing signs of bacterial overgrowth and poor pancreatic enzyme function.
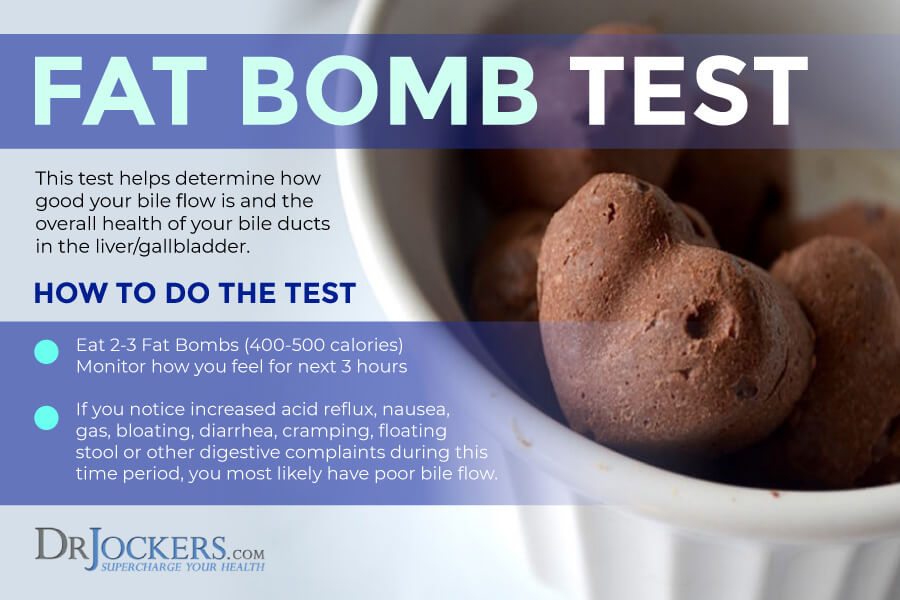
Fat Bomb Test for Bile Flow
I recommend the Fat Bomb test for bile flow. The fat bomb test challenges your body to excrete a good amount of bile to emulsify and metabolize a load of fat.
To do this test, simply eat 2-3 of these chocolate fat bombs and monitor how you feel over the next 3 hours. If you feel tired, have acid reflux, nausea, gas, bloating, diarrhea, cramping, floating stool, or other digestive complaints, you may have poor bile flow.
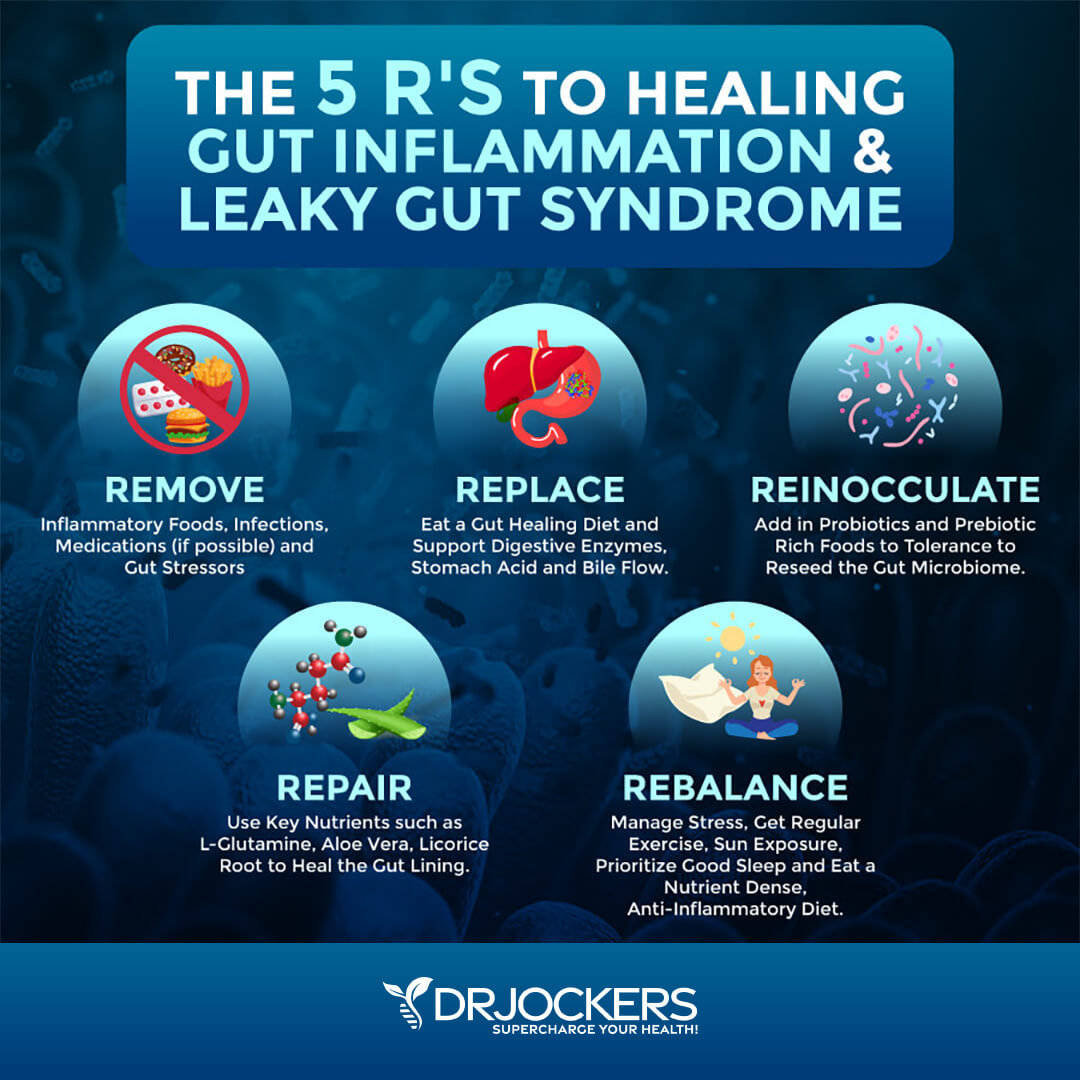
Natural Support Strategies
If you are experiencing symptoms of gut inflammation, I have good news. You can reduce inflammation and improve your health naturally.
Here are the natural support strategies I recommend for gut inflammation:
Avoid Gut-Damaging Medications
The long-term use and overuse of certain medications, especially antibiotics, PPIs, NSAIDs, SSRIs, and oral contraceptives can damage your gut and cause gut inflammation (21). A 2015 study published in PLoS One has found that antibiotics can also increase the risk of leaky gut syndrome and gut inflammation (22, 23, 24, 25, 26).
I recommend that you avoid using these gut-damaging medications, especially long-term. If you have been or are taking any of these medications, I recommend that you work with a functional medicine practitioner and follow the recommendations in this article to reduce the risk of gut inflammation and related symptoms.
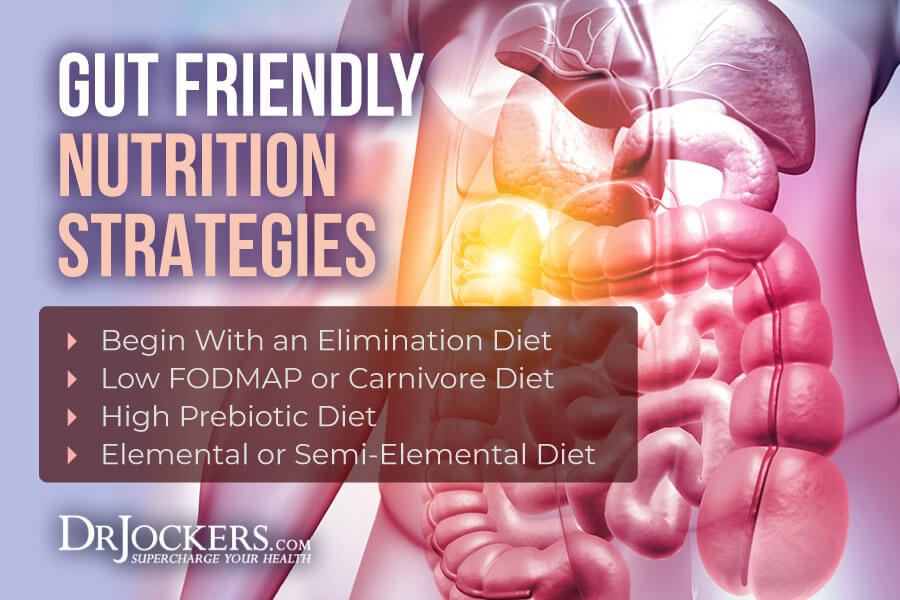
Gut-Friendly Nutrition Strategies
A 2021 study published in BMJ has found that eating a diet high in processed foods, processed sugar, alcohol, and processed animal foods were associated with increased intestinal inflammatory markers, gut inflammation, and gut microbiome imbalance (5). Food sensitivities, gut infections, and SIBO may also lead to gut inflammation and gut dysbiosis (6, 7, 16, 17, 18, 19, 20).
One of the best ways to support your gut health and reduce gut inflammation is by following gut-friendly nutrition strategies. Here is what I recommend:
Try an Elimination Diet
Going on an elimination diet is the best strategy to find out what food sensitivities you may have. To start, take out the following food groups from your diet for two weeks: gluten, dairy, refined sugar, corn, soy, eggs, all grains, vegetable oils, shellfish, tree nuts, legumes, and nightshade vegetables.
Make sure that you remove these foods completely, follow the plan, and don’t cheat. Eating just a bit of these triggering foods can cause symptoms and compromise your efforts off.
After a two-week elimination period, introduce foods to your diet one by one. Eat new food for two to three days. Notice your symptoms. If you have symptoms, remove them. Add a new food, note your symptoms, and continue. However, I recommend that you remove highly inflammatory foods, such as gluten, refined sugar, vegetable oils, and conventional dairy from your diet for good.
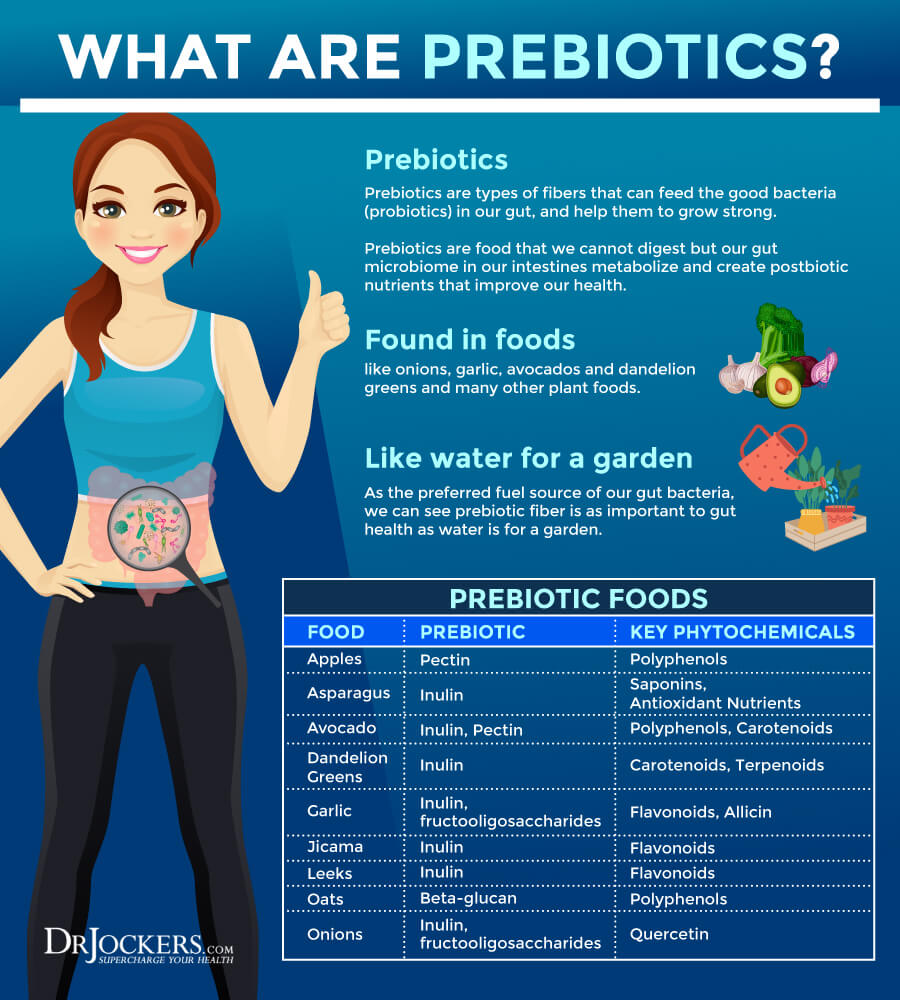
Try a Prebiotic-Rich Diet
Probiotics are not always enough. You may have to support them with prebiotics. Prebiotics are a specific dietary fiber that feeds the good bacteria or probiotics in your gut. Prebiotic-rich foods include Jerusalem artichokes, leek, onion, garlic, asparagus, dandelion, chicory greens, jicama, apples, and bananas.
However, prebiotic-rich foods are not right for everyone. Some people find too many prebiotics in their diet is triggering for them. If you notice digestive complaints from a prebiotic-rich diet, back off. If you are following a low-FODMAP diet, you shouldn’t follow a prebiotic-rich diet either. Unless you are on these diets, I recommend that you try a prebiotic-rich diet. Pay attention to your symptoms and reduce your intake if you find it triggering.
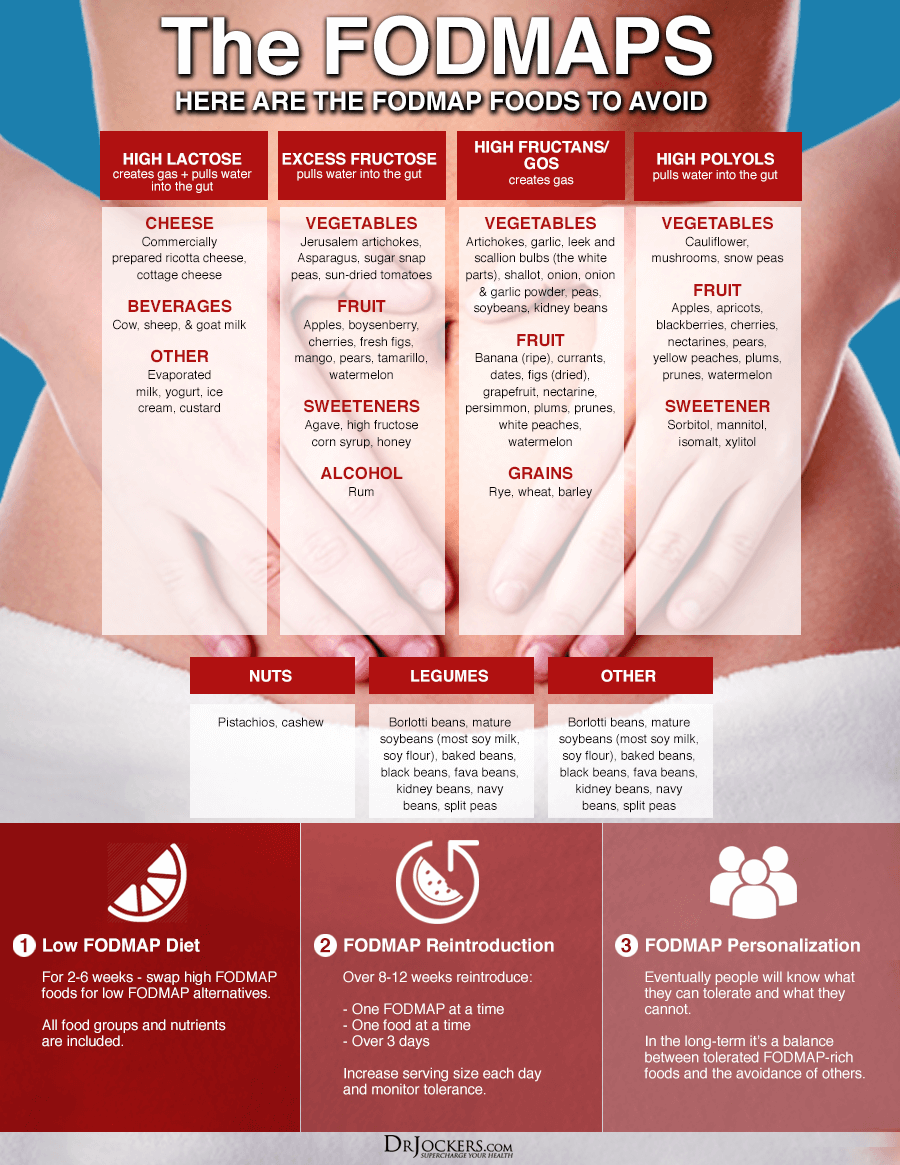
Try a Low-FODMAP Diet
The low-FODMAP diet is a diet low in fermentable oligo-, di-, monosaccharides, and polyols or FODMAPS, certain sugars that may cause intestinal distress. It is generally recommended for people with small intestinal overgrowth (SIBO), however, it may be beneficial for other gut health issues as well.
Low-FODMAP vegetables include carrots, green beans, arugula, mint, basil, pepper, olive, pumpkin, tomato, potatoes, sweet potatoes, cucumber, zucchini, Swiss chards, lettuce, radishes, parsnip, sprouts, kale, and collard greens.
Low-FODMAP fruits include lemon, lime, kiwi, grapes, papayas, strawberries, raspberries, blueberries, melon, pineapples, and tangerines. Other low-FODMAP foods include egg, meats, fish, brazil nuts, chestnuts, butter, bone broth, seafood, quinoa, millet, rice, walnuts, and pine nuts.
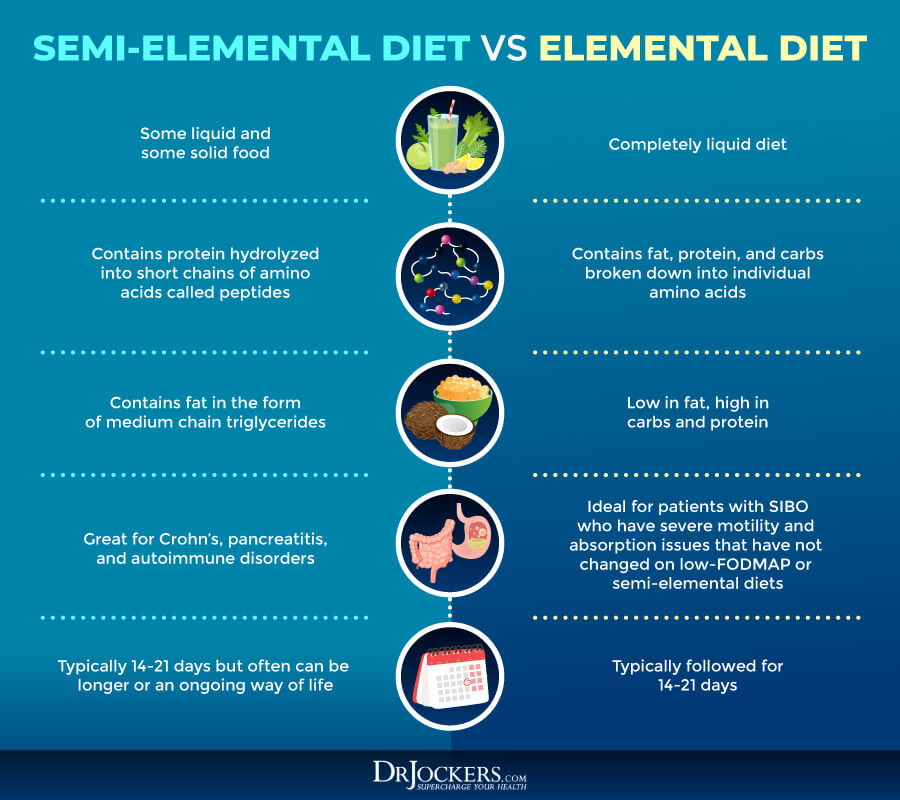
 Try a Semi-Elemental or Elemental Diet
Try a Semi-Elemental or Elemental Diet
The elemental diet is a diet using nutritional formulas with pre-digested foods. These powders include vitamins, minerals, and complete macronutrients, and are used to replace all or some of your meals.
The elemental diet or a semi-elemental diet is commonly used to improve SIBO, Crohn’s disease, and eosinophilic esophagitis. I only recommend this diet short-term and with the guidance of your healthcare professional until you resolve your issues.
Reduce Stress & Optimize Sleep
Poor sleep and chronic stress can result in gut inflammation (9, 10, 11, 12). I recommend that you reduce your stress and optimize your sleep. Taking a few deep breaths can reduce your dress levels immediately.
Practicing meditation, gratitude, mindfulness, guided relaxation, and prayer can help you learn how to respond to stress better and lower your stress levels. Journaling, positive mindset shifts, and positive affirmations can also help. Exercise, grounding, and time spent in nature are also great ways to calm your mind and reduce stress.
Developing a regular sleep routine, going to bed, and waking up around the same time helps to support your body’s natural circadian rhythms. Avoid electronics, sugar, caffeine, heavy foods, and stress in the evening. Choosing calming activities instead, such as reading, coloring, taking a healing bath, sipping on herbal tea, crossword puzzles, journaling, and good conversations.
If the weather permits, you may want to sit outside on your porch or balcony taking in the evening sky. Create a safe sanctuary in your bedroom with a supportive bed, comfortable sheets and pillow, calming decoration, an essential oil diffuser with lavender or other calming oils, a salt lamp, and blackout curtains.

Improve Stomach Acid Levels
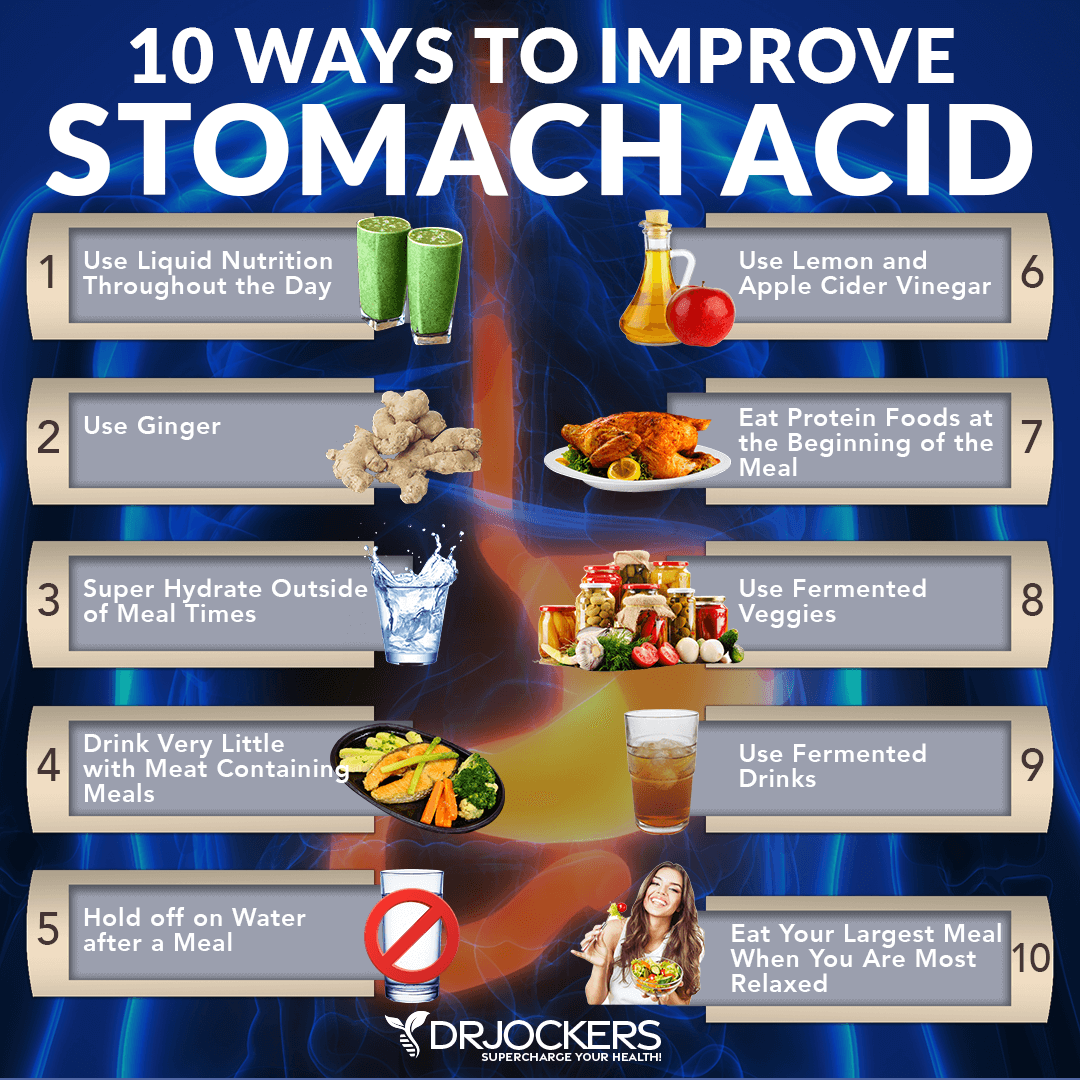
Poor stomach acid levels can increase the risk of gut inflammation (13). To support your stomach acid levels, I recommend the following:
- Use Liquid Nutrition Throughout the Day: Try to make sure that at least half of your meals are in a liquid form, such as a protein shake or green smoothie. Protein shakes are pre-metabolized and very easy to digest and do not depend upon HCL production. If you have low HCL, it may be helpful to drink one to two protein shakes daily to support amino acid absorption, reduce extra stress on your digestion, and support healthy stomach acid levels.
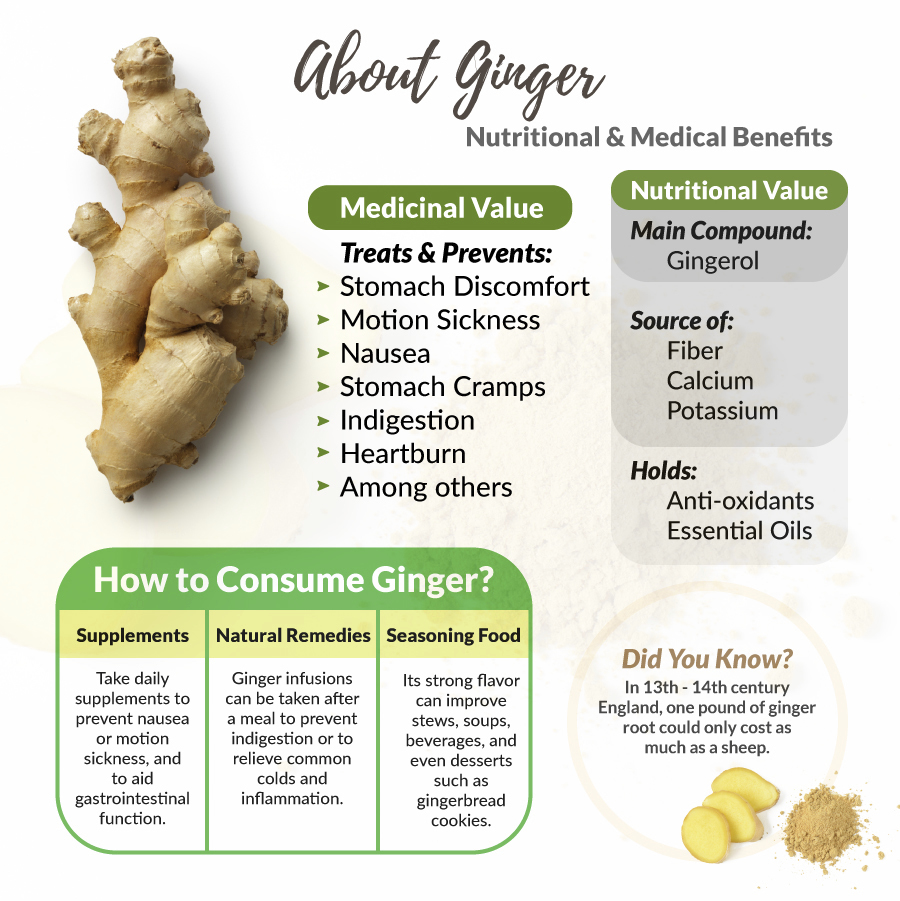
- Use Ginger: Ginger is one of the best things for improving digestive juices. I recommend drinking 2 to 3 cups of ginger tea each day. You can put ginger essential oil in water (2 to 3 drops in 8 oz of water), juice a ½ inch of fresh ginger root in green juice each day, and use ground ginger on your foods. You can also add fermented ginger to your diet, which is common in Asian dishes such as kimchi.
- Super Hydrate Outside of Meal Times: Good hydration can help activate bowel motility and push contents through the digestive system, which will reduce microbial fermentation and toxicity in the body. This can help to support your stomach acid levels.
- Drink Very Little With Meat Containing Meals: When you are eating meat or any sort of heavier food, you should stop drinking water or other liquids at least 30 minutes before the meal, except if you need to take a supplement with 2 ounces of water. Holding off water during these meals will reduce any potential dilution of the gastric juices and allow for better digestion.
- Hold Off On Water After a Meal: To allow for optimal digestion, I also recommend not drinking water or other liquids until at least 30 minutes after a meal. This allows for proper stomach acid activity, sterilization, and protein metabolism.
- Use Lemon and Apple Cider Vinegar: Squeezing fresh lemon or using lemon juice or apple cider vinegar on your meat and vegetables helps to pre-metabolize the food and support better digestion and nutrient absorption. You can either marinate foods in a lemon or ACV base or just add them as a dressing right before consuming them.
- Eat Protein Foods at the Beginning of the Meal: The stomach will begin churning out its stomach acid when you start eating, especially when consuming protein. While it’s culturally common to have a salad before their protein dish, this is not great for your HCL production. It is a much better idea to eat your protein with salad or vegetables instead of after.
- Use Fermented Veggies: Fermented foods such as sauerkraut, kimchi, pickles, pickled ginger, and other fermented vegetables all contain organic acids, enzymes, and probiotics which help to improve digestive juice secretions. I recommend using one of these with all of your heavier meals especially any meal with protein.
- Use Fermented Drinks: Fermented drinks such as apple cider vinegar, coconut kefir, and kombucha offer anti-microbial benefits and help to reduce the bacterial load, especially the bacteria in the stomach such as H Pylori. Keeping H Pylori levels down is critical for the body to be able to produce enough stomach acid.
- Eat Your Largest Meal When You Are Most Relaxed: Your body needs to activate the parasympathetic nervous system to produce enough stomach acids. If you are busy and on the go, you will be in fight or flight sympathetic mode. If you struggle with low stomach acid, this fight or flight state will not allow your body to produce anywhere near enough. Relaxing before the meal is important to improve stomach acid production.
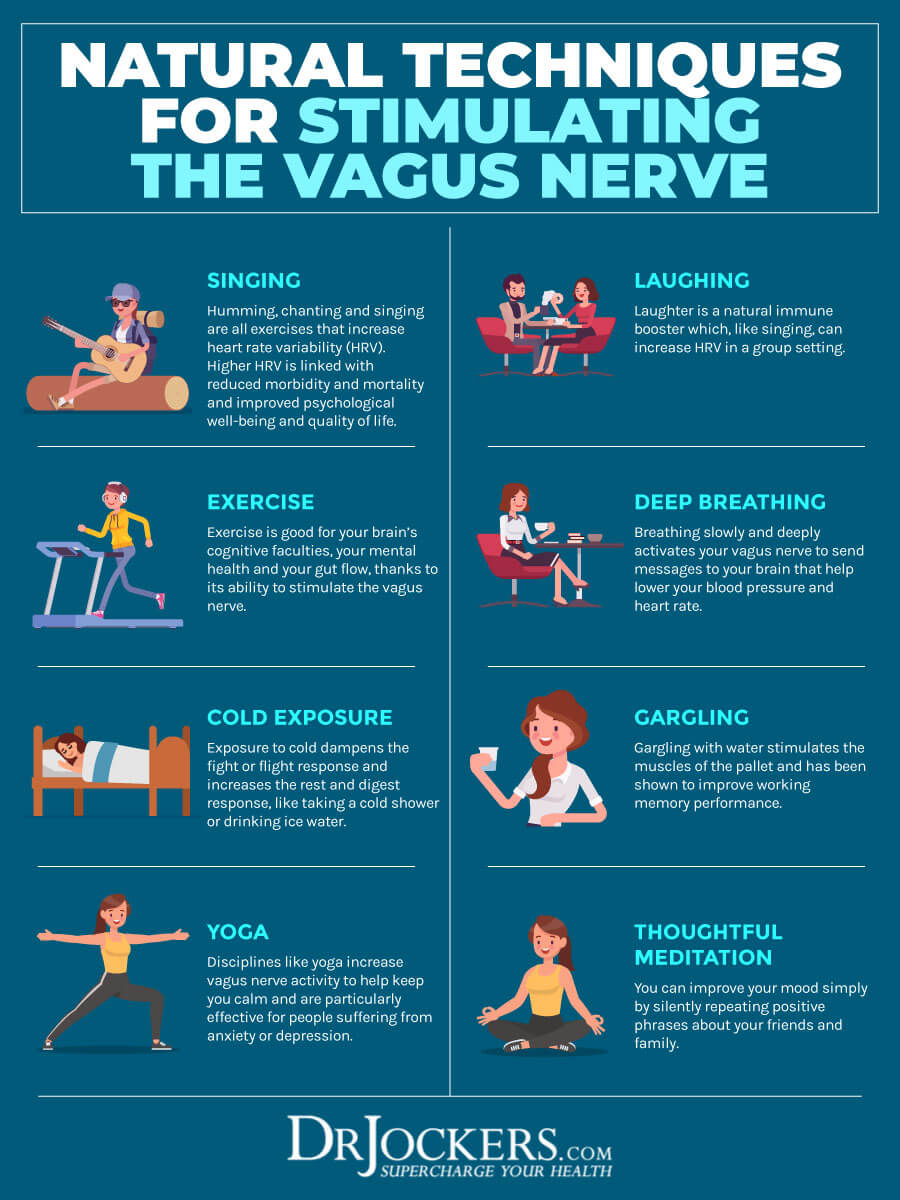
Improve Vagal Tone
Poor vagal tone may result in gut inflammation and gut health issues (8). I recommend that you support your vagal nerve activity and improve your vagal tone to reduce gut inflammation, improve bowel motility, and better your digestion.
Some strategies that help to improve your vagal tone include practicing gratitude and laughter, getting good sleep, meditation, prayer, deep breathing, stimulating your palatal muscles, signing, yoga, gargling, connecting with others, cold exposure, exercise, and movement, and following an anti-inflammatory nutrition plan. You may learn more about these strategies to improve your vagal tone by reading this article.
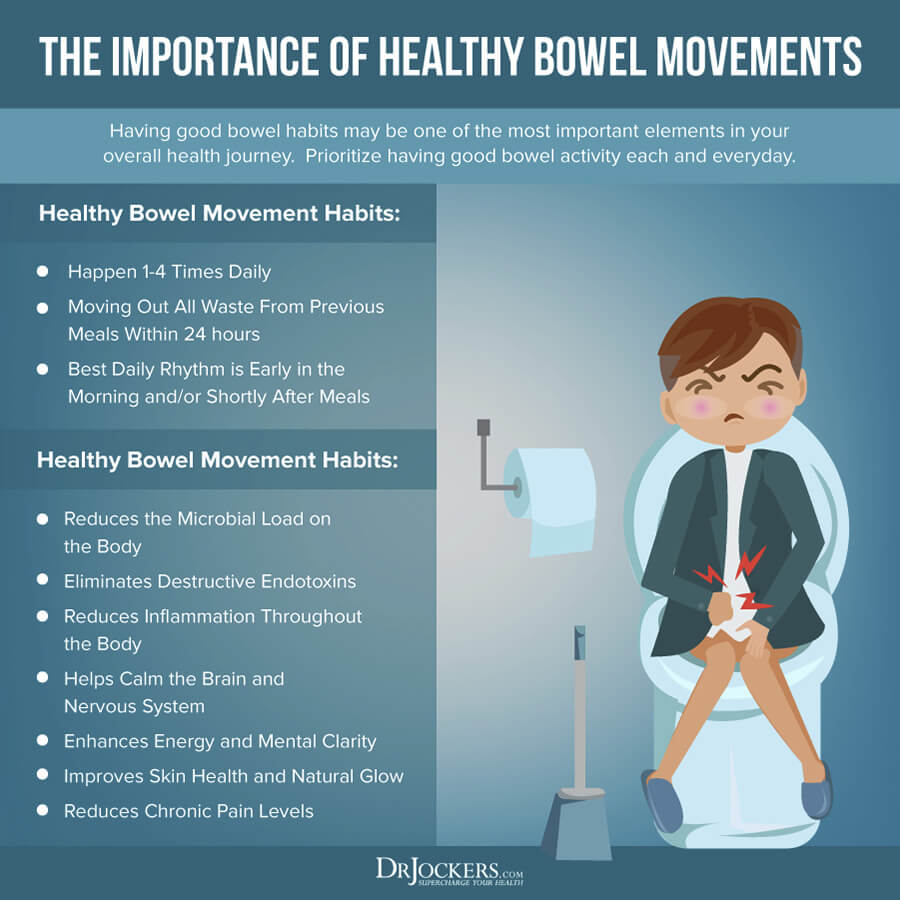
Improve Bowel Motility if Needed
Eliminating toxins and waste through regular bowel movements is critical. If you have constipation or irregular bowel movements, try these strategies to improve your bowel motility.
Begin your day with 32 oz of water. Drink regularly throughout the day, at least ten glasses a day or more if you are working out a lot, sweating, sick, or simply thirsty. If you are feeling thirsty it means that you are probably already dehydrated. To prevent this, drink water regularly.
Use sticky notes, set reminders on your phone, or add a new rubber band on your water bottle after every 8 oz of water you drink. Add a pinch of salt to your water, eat mineral-rich vegetables, and try an electrolyte balance powder to avoid electrolyte imbalance from dehydration.
Eating prebiotics and fiber may benefit bowel motility. But remember, not everyone does well on prebiotics, and they don’t work well with the low-FODMAPS and the carnivore diet. Know your body and experiment to find what works best for you. If prebiotics and fiber are triggering, reduce the amount or back off completely.
I recommend digestive enzymes, such as Super D-Zyme to support your digestion. If you have low stomach acid, using an HCL supplement, such as Super Digest HCL can be helpful. For GI mucosal membrane health, I recommend GI Clear. If you have trouble with elimination and have constipation, a supplement like Bowel Mover can help until your body recovers enough and regains its normal rhythms of elimination.
Magnesium supplementation can also support bowel motility and smooth bowel movements. You may want to try magnesium and oxygen-based colon cleansers. It improves bowel motility, prevents and relieves constipation, improves your microbiome balance, and removes toxins from your colon. I recommend CalMag Support.
Use Probiotics
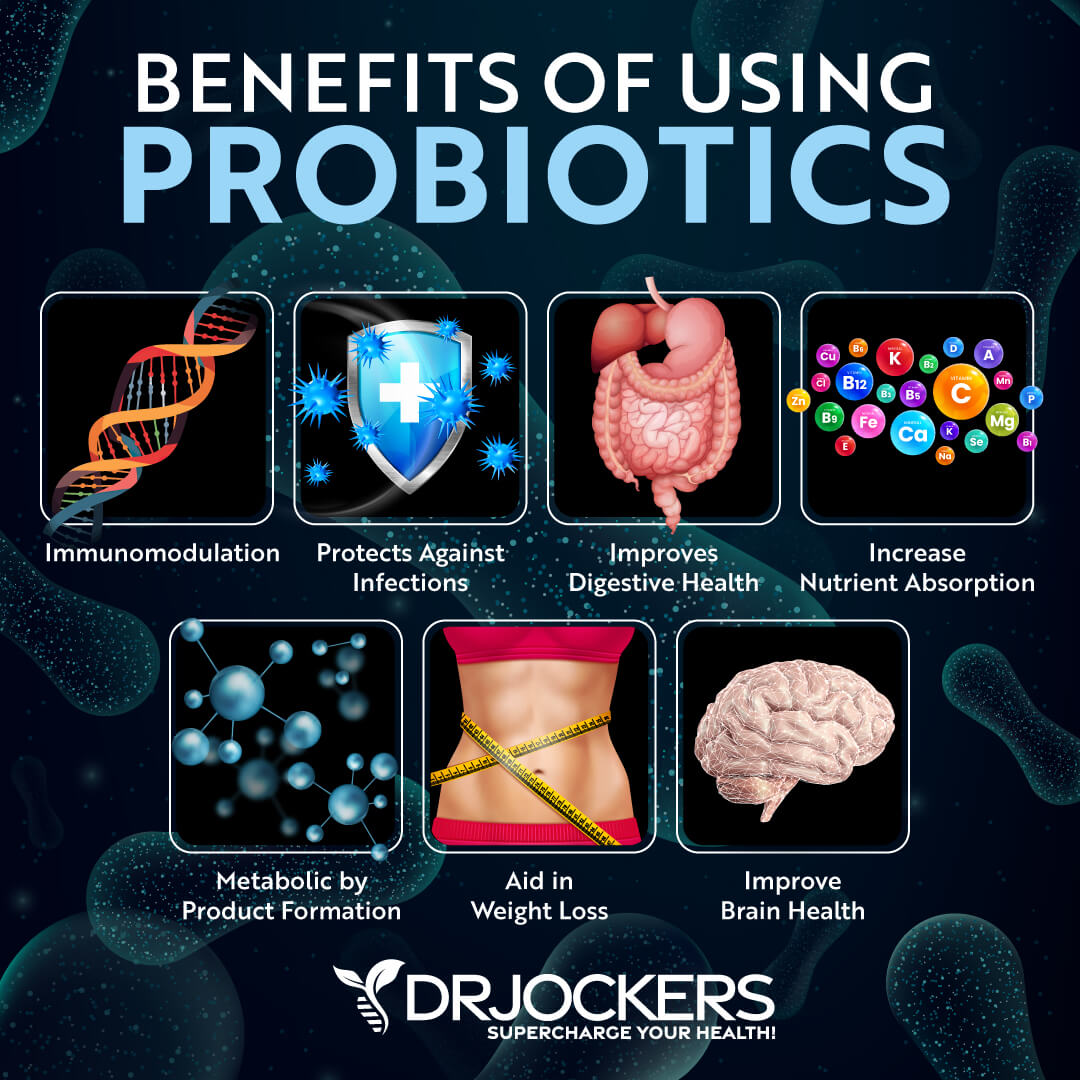
Probiotic supplements contain good bacteria that can help to repopulate your gut with beneficial bacteria, rebalance your gut microbiome, and reduce gut inflammation and gut health symptoms. A 2003 study published in the Journal Of Royal Society Medicine has found the probiotics can help improve inflammatory bowel disease, which is characterized by gut inflammation and related symptoms (27).
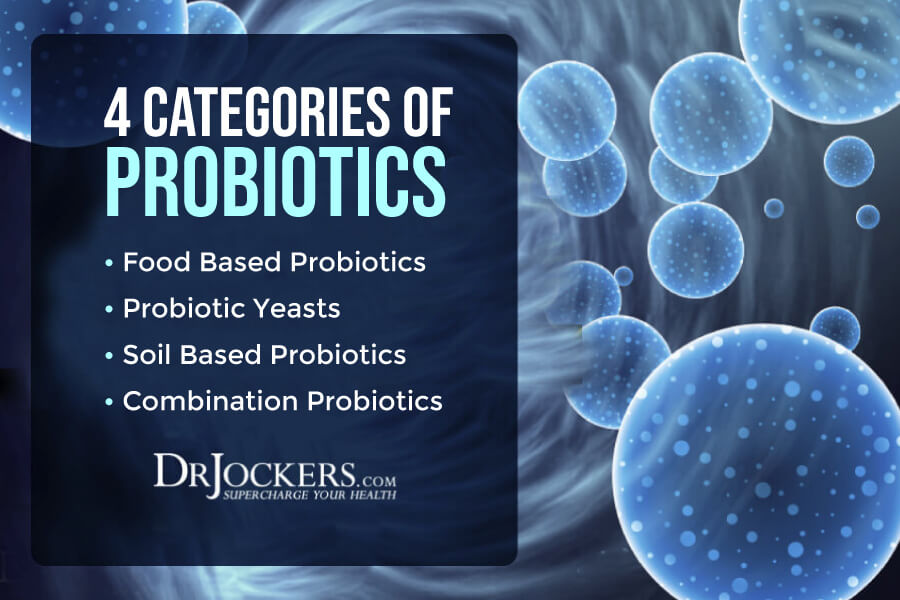
I recommend that you include probiotic-rich foods in your diet, including sauerkraut, kimchi, fermented vegetables, coconut kefir, pickles, and kombucha. I recommend that you also take a daily probiotic supplement. There are different types of probiotics and probiotic supplements:
- Food-based Probiotics: Lactobacillus acidophilus La-14 is a common inhabitant of the human mouth, intestinal tract, urinary tract, and vagina. It is found in some traditional fermented milk (e.g., kefir) and is widely used in probiotic foods and supplements. L acidophilus has excellent adhesion to the gut lining. Bifidobacterium lactis is a strain with tremendous probiotic potential based upon its ability to survive the transit through the human gastrointestinal tract, adhere to epithelial cells, and proliferate. The Bifidobacterium longum B1-05 strain is well-accepted as safe for human consumption. It is resistant to low pH and bile salts and is well-suited to the intestinal environment.
- Probiotic Yeasts: Saccharomyces boulardii is a natural, non-pathogenic probiotic yeast. One of the main benefits of Saccharomyces boulardii is that it is resistant to stomach acids and antibiotics. It promotes immune and digestive health.
- Soil-Based, Spore-Forming Probiotics: Soil-based probiotics can form bacterial spores and are often used to treat gastrointestinal disorders. Spore-based strains have an innate resistance to the stressors of heat, light, stomach acid, and time. This ensures long-term viability and protects them against degradation so that they reach the lower GI tract intact and alive. Spore-forming probiotics are a promising alternative for people affected by recurring gut problems.
- Combination Probiotics: Combination probiotics blend different types of probiotics into one formula. For example, a combination probiotic blend may contain food-based lactobacillus and bifidobacterium probiotics, soil-based, spore-forming probiotics Bacillus subtilis and Bacillus coagulans, and beneficial yeast, Saccharomyces boulardii into one capsule. They often contain prebiotic inulin, which feeds and supports the strength of the probiotics in each capsule. This probiotic supports healthy immune system function, healthy gut function, and a healthy gastrointestinal tract.
Everyone tolerates different probiotics differently. I recommend that you give a trial run to each probiotic before you commit to one long-term. If you are a highly sensitive individual, I would recommend starting with a soil-based probiotic formula as those tend to be the most well-tolerated. If you feel better after the 7-day trial, then that is a sign that this particular probiotic is benefiting you, and if you feel worse, then it is not.
Never stay with one particular probiotic or brand for too long. Rotating probiotics helps to diversify your gut flora. Once you find the probiotics that are working well for you, it is a good idea to cycle probiotics every 1-3 months or so. If you are only responding well to one type of probiotic, then stay on that and don’t worry about rotating.
However, if you respond well to all three types of probiotics, then rotating between them or between combination probiotics can be very helpful. You can learn more about how to select the best probiotic supplements and how to rotate various types of probiotics in this article.
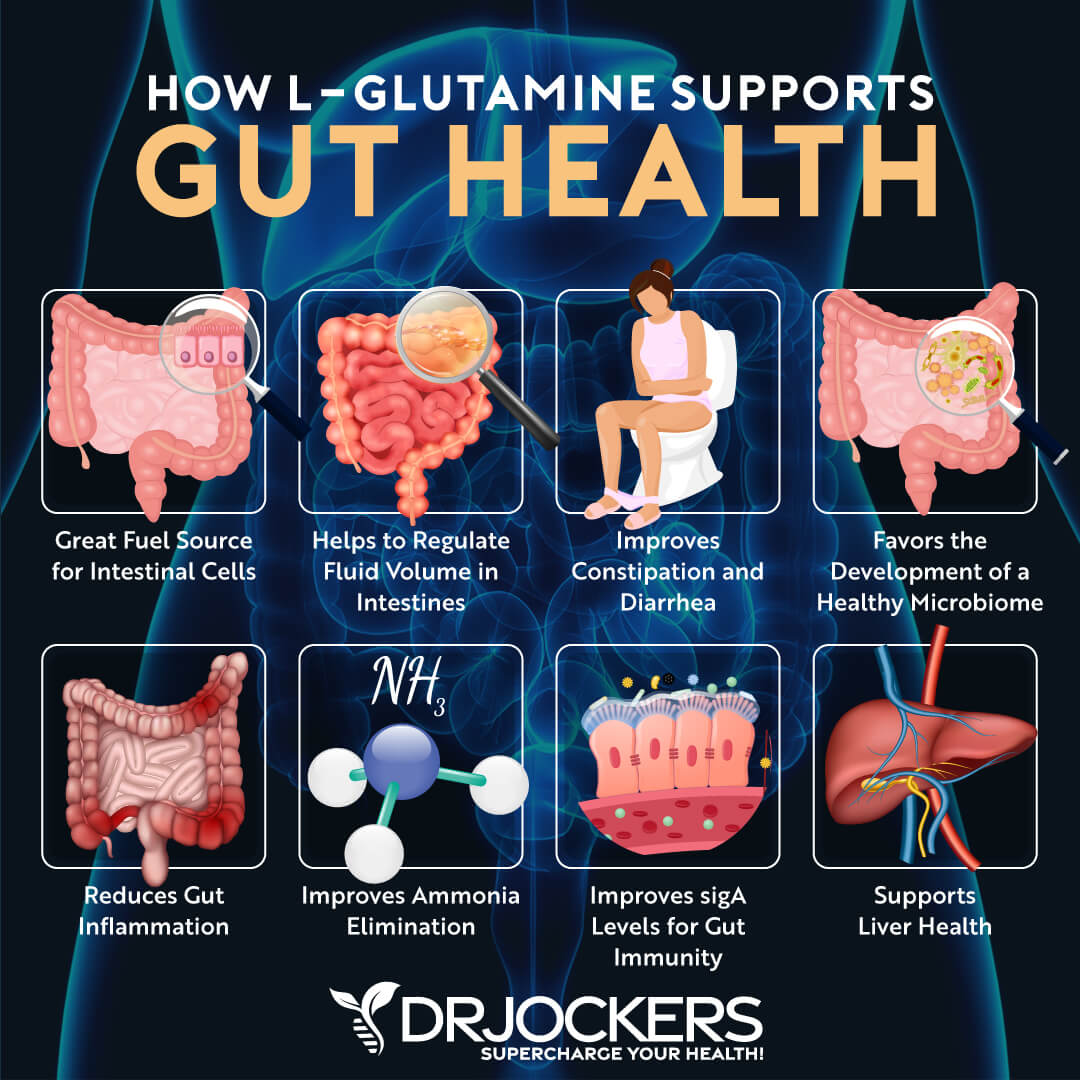
Consider Using L-Glutamine
L-glutamine is a non-essential amino acid that serves as an energy source for both your intestinal and immune cells. It helps to keep your intestinal barrier healthy and ensures the healthy growth and function of your intestinal cells.
According to a 2012 study published in the Journal of Epithelial Biology and Pharmacology, l-glutamine plays an important role in the gut barrier function, gut mucosal health, metabolism, and the reduction of gut inflammation (28). According to a 2017 study published in the Journal of Molecular Sciences, L-glutamine can be beneficial for intestinal diseases and gut inflammation (29).
To lower gut inflammation and protect your gut, I recommend taking a daily L-glutamine supplement. Begin by taking a low dose of around 4-6 grams and see how you feel. If you don’t notice anything, bump up your dose to 4-6 grams – 2-3 times daily. In some cases, taking around 20-30 grams daily in divided doses is necessary to get over the hump and heal the gut.
Consider Improving Zinc, Selenium & Vitamin D Levels
Zinc is an essential mineral that your body cannot make on its own. This means that you need to meet your needs through food and supplements. It’s important for your immune health and metabolism. A 2014 study published in the World Journal of Gastrointestinal Pathophysiology suggests that supplementing with zinc may help to prevent gastrointestinal disease (30).
Foods that are rich in zinc include meat, poultry, seafood, eggs, nuts, and seeds. Since meeting your needs through diet alone can be difficult, I recommend daily supplementation. I highly recommend Zinc Charge as a high-quality, potent zinc supplement. Taking 20-40 mg of zinc can be extremely helpful for turning off gut inflammation and healing the gut lining.
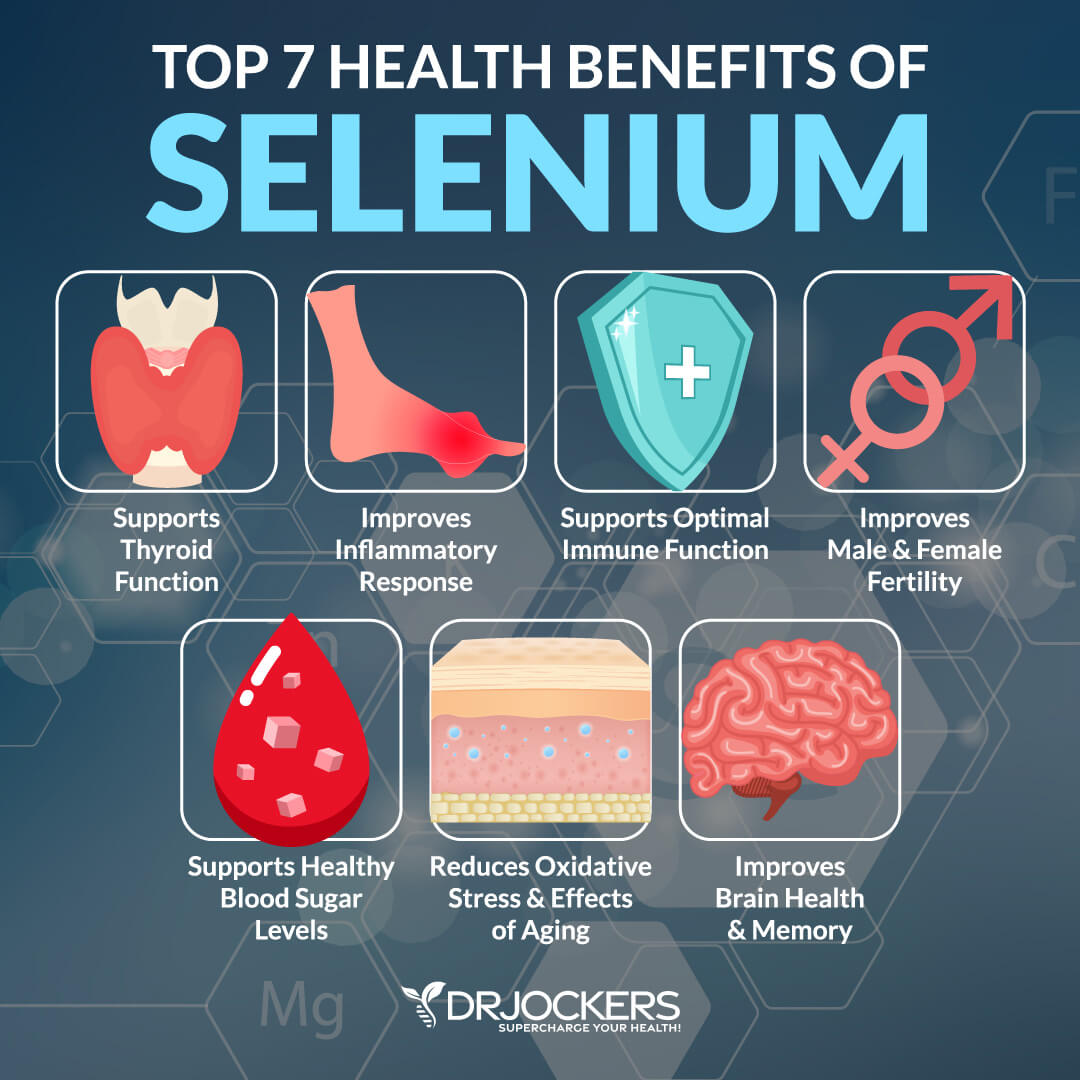
Optimize Selenium Levels
Selenium is another important mineral that is important for your immune health and helps to reduce inflammation and oxidative stress. It may also be important for your gut health. A 2015 study published in the American Journal of Physiology – Gastrointestinal and Liver Physiology has found that low selenium levels may contribute to irritable bowel diseases and improving selenium levels can help (31).
Meeting your selenium needs a day is simple. All you have to do is to eat two Brazil nuts a day. Meat, poultry, eggs, nuts, and seeds are also good sources of selenium. In some cases taking an extra 100-400 mg of selenium is necessary to address an underlying deficiency and turn off gut inflammation.
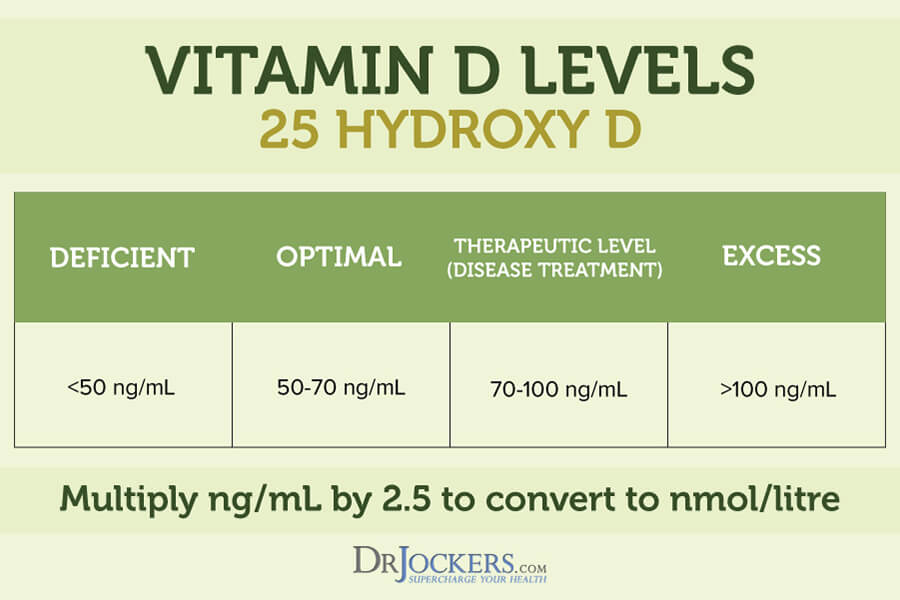
Optimize Vitamin D Levels
Vitamin D is an essential vitamin for muscle, bone, brain, and immune health in everyone. It’s also important for your gut. A 2018 study published in Food Technology and Biotechnology has found that vitamin D has immunomodulating benefits and can help to improve the symptoms of inflammatory bowel disease, which is characterized by gut inflammation (32).
Most people are not getting enough sunshine or consuming enough vitamin D from food. Therefore, most people need supplements to optimize their vitamin D levels. Pairing vitamin D3 with vitamin K2 helps improve calcium absorption and inflammation control. I recommend taking a vitamin D3 supplement with at least 3,000-5,000 IU’s of vitamin D3 and at least 90 mcg of vitamin K2. I recommend taking D3/K2 Power for your daily dose of vitamin D3 and K2.
Typically, taking 1,000 IU per 25 lbs. of body weight will help you get your levels into a healthy range. You want to test your vitamin D levels at least 1-2 times each year and get your levels between 50-100 ng/ml. It has been hypothesized that a therapeutic level for major health conditions is going to be between 70-100 ng/ml.
Consider Using Anti-Inflammatory Herbs & Compounds
I recommend a variety of anti-inflammatory herbs and compounds for gut inflammation.
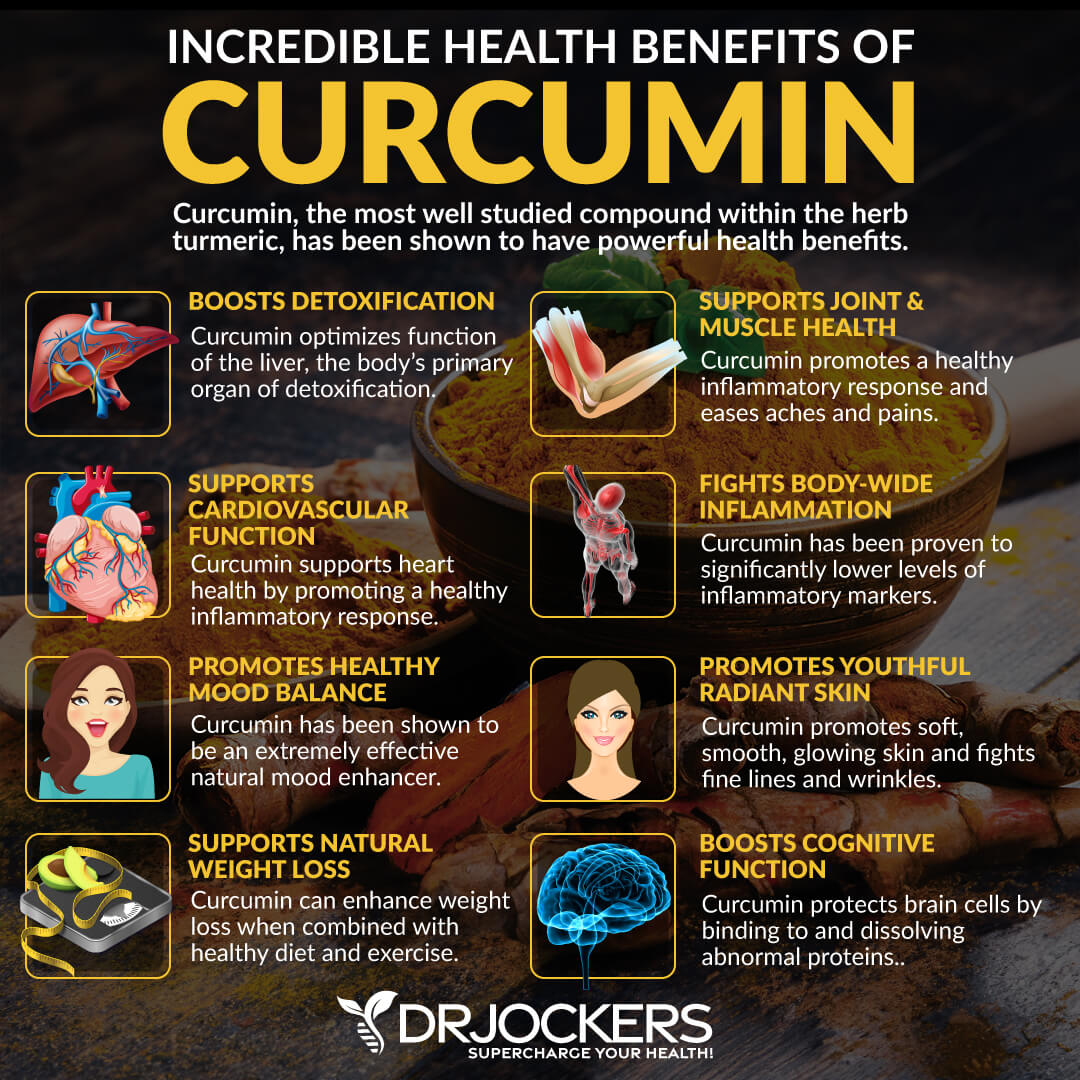
Turmeric
Curcumin is the active compound of the spice, turmeric. It can prevent chronic inflammation by controlling the inflammatory pathways that lead to tissue damage, histamine release, immune cell activation, and digestive disturbances.
Associated with improving the immune response of patients with autoimmune diseases in clinical trials, curcumin may aid recovery from leaky gut. A 2019 study published in the International Journal of Molecular Sciences has found that using curcumin can be beneficial for intestinal inflammatory diseases (33).
I recommend that you use turmeric in your curries, vegetable dishes, soups, dressings, smoothies, and juices. I also recommend that you supplement your diet with 1,000-2,000 mg of curcumin daily to limit inflammation and enhance natural immunity.
Ginger
Sometimes referred to as its active component, 6-gingerol, ginger exhibits comparable inflammation prevention control as do drugs like aspirin and ibuprofen, Ginger is a digestive stimulant that promotes gastric flow and contains enzymes that aid in proper digestion. It has been known to reduce digestive discomfort, nausea, pain, and inflammation. A 2018 systematic review has found that ginger is beneficial for reducing risks and symptoms of gastrointestinal disorders (34).
I recommend that you add ginger to your diet by adding it to tea, smoothies, dressings, soups, and warm dishes. You may also benefit from a supplement with ginger, like Inflam Defense or Gut Healing Protein Powder.
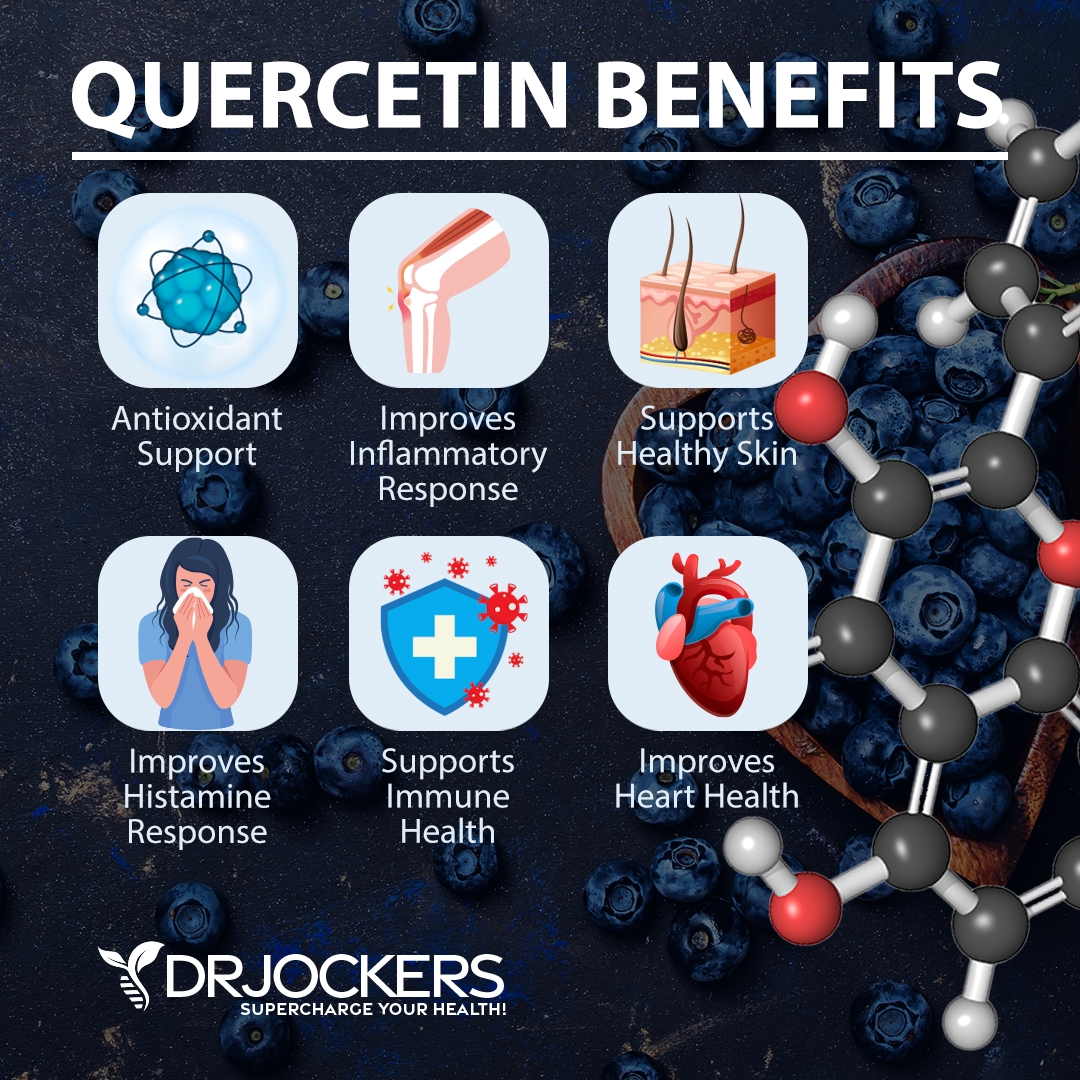
Quercetin
Quercetin is a plant compound known for its antioxidant, histamine-reducing, and anti-inflammatory properties. According to a 2019 study published in Frontiers in Microbiology, quercetin helps to improve microbial diversity in the gut and reduce gut inflammation and inflammatory intestinal issues (35).
It is found in grapes, apples, blueberries, black currants, cherries, black plums, cranberries, cruciferous vegetables, kale, red leaf lettuce, romaine lettuce, chicory greens, cabbage, sprouts, snap pea, red onion, peppers, herbs, and olive oil. Additionally, to load up on these quercetin-rich foods, you may also benefit from a supplement with quercetin, like Inflam Defense or Gut Healing Protein Powder.
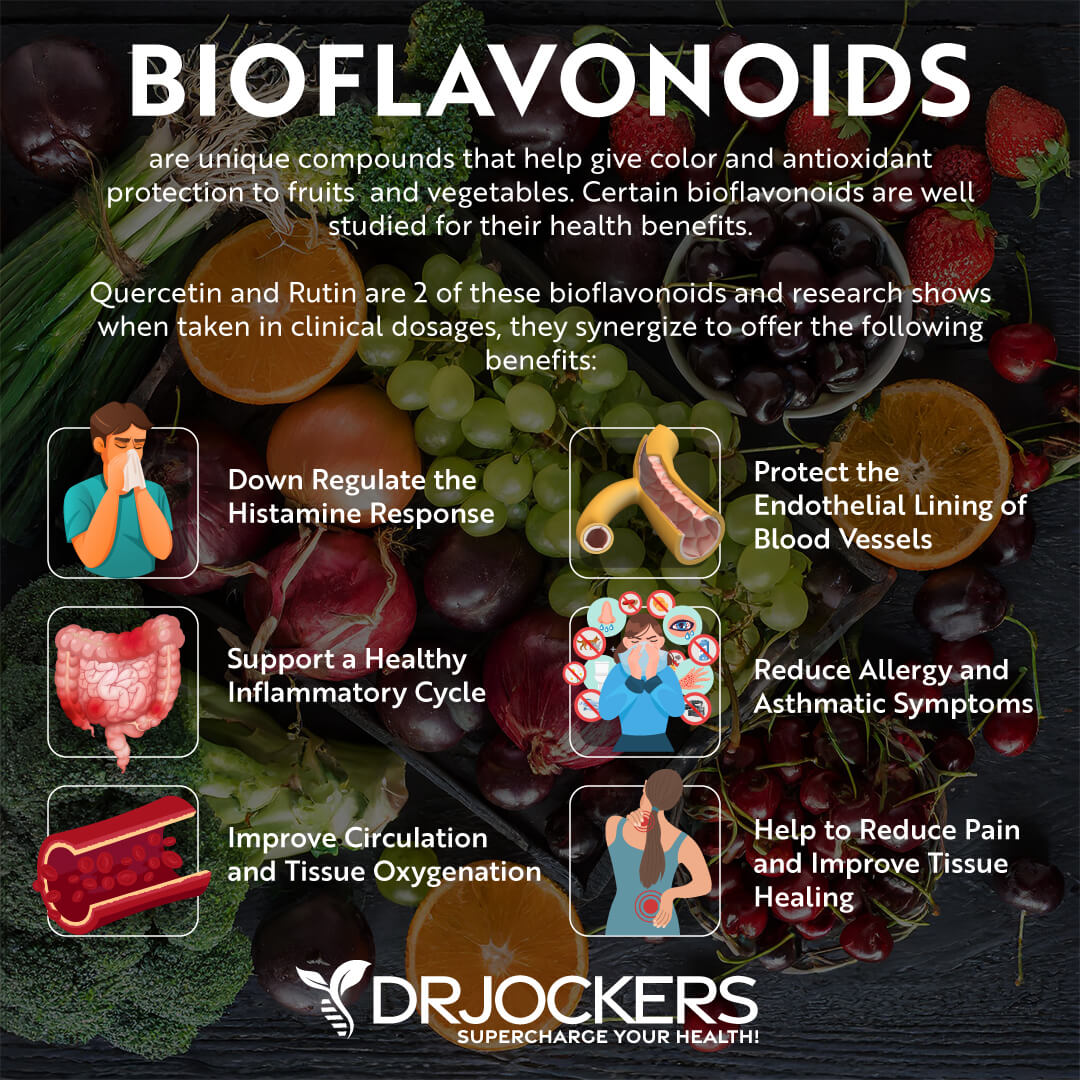
BioFlavonoids
Bioflavonoids, also called flavonoids, are a group of “polyphenolic” plant-derived compounds. A 2011 study published in the World Journal of Gastrointestinal Oncology has found that bioflavonoids have anti-inflammatory properties that can play an important role in gastrointestinal health (36).
Foods that are rich in bioflavonoids include lemons, lime, oranges, cherries, grapes, red onion, and broccoli. Additionally to consuming these foods, I recommend using our Gut Healing Protein which has therapeutic dosages of bioflavonoids.
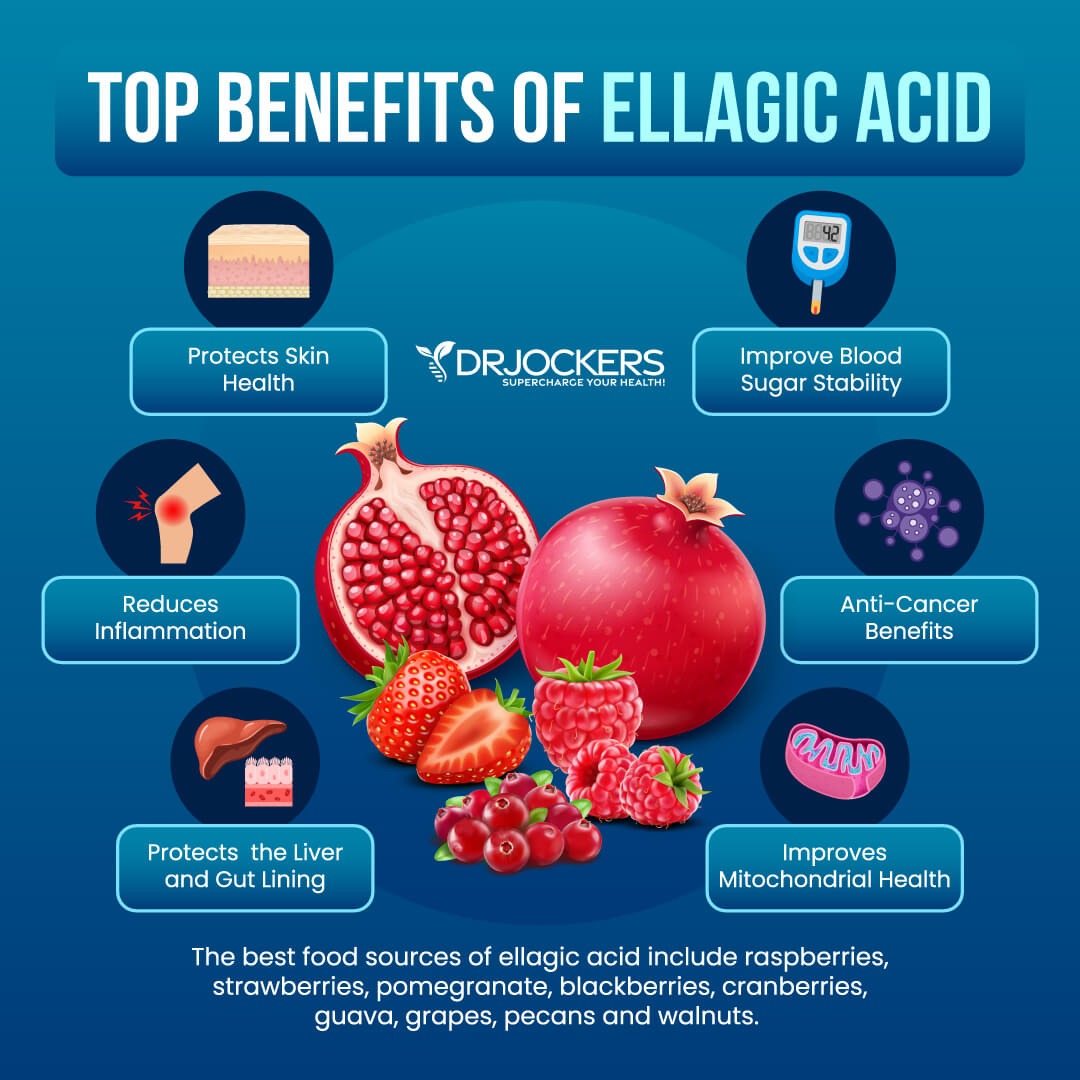
Ellagic Acid
Ellagic acid is a micronutrient and polyphenol found in mostly red fruits and vegetables, such as strawberries, blackberries, pomegranates, cherries, grapes, guava, red cabbage, red peppers, red onions, tomatoes, and radishes. It offers antioxidant and anti-inflammatory properties.
According to a 2020 study published in the World Journal of Gastroenterology, ellagic acid can support your gut microbiome health and offer gastrointestinal protection (37). Beyond consuming these foods, you may benefit from a supplement with ellagic acid, such as Gut Healing Protein Powder.
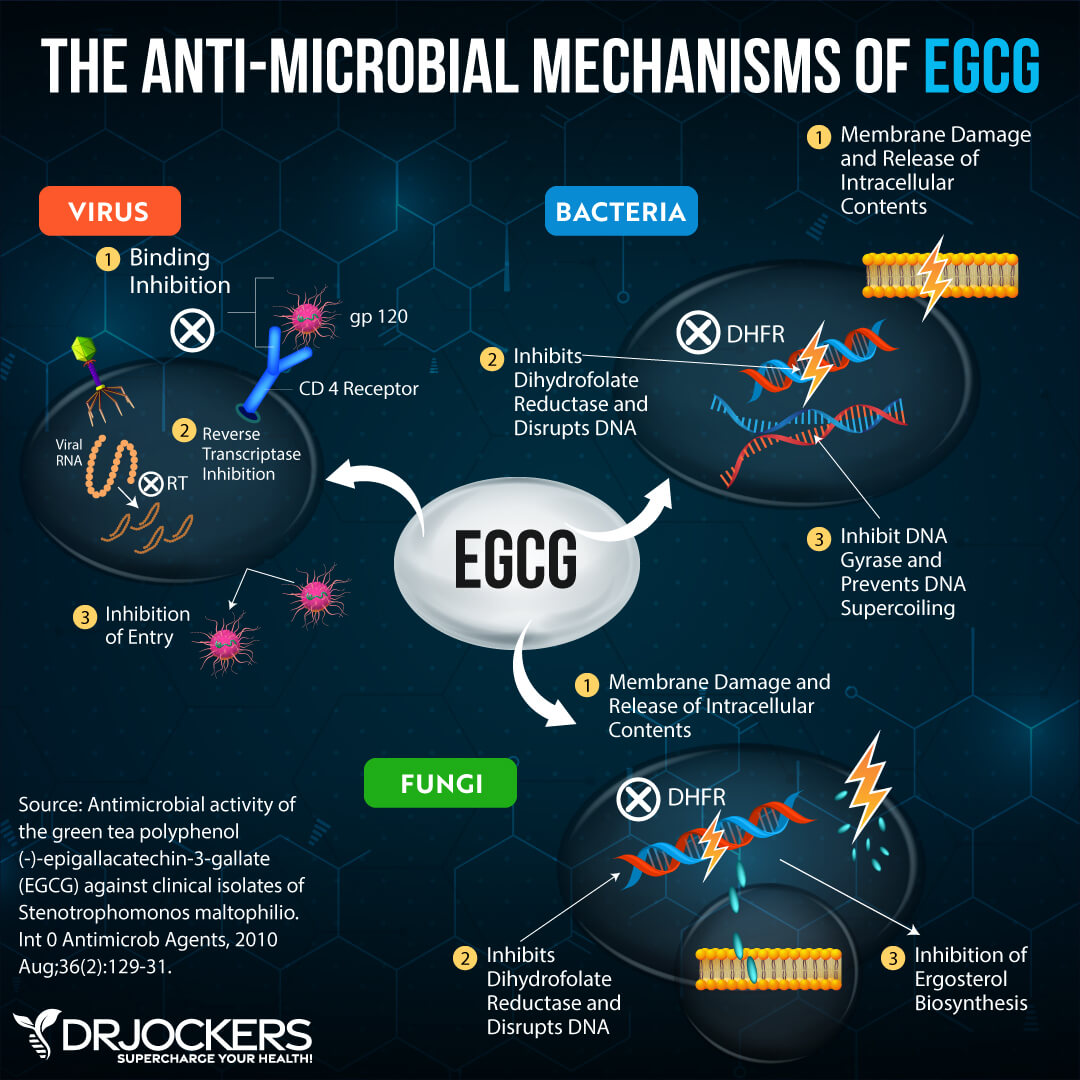
EGCG
Epigallocatechin gallate, EGCG is a type of plant-based compound found in green tea. It offers antioxidant and anti-inflammatory benefits. It also has powerful anti-microbial properties to prevent bacterial, fungal, and viral infections.
A 2017 study published in Nutrients found that green tea polyphenols like EGCG can help reduce gut inflammation and aid recovery from chronic inflammatory diseases (38). Other than consuming green tea regularly, you may benefit from a supplement with EGCG to support your gut health.
MSM
MSM is a natural compound that can help to reduce inflammation, lower joint pain, and support immune health. According to a 2016 study published in the Journal of Sports Medicine (Hindawi) MSM can help to reduce inflammation (39).
Foods that are rich in MSM include leafy green vegetables, alfalfa sprouts, apples, tomatoes, raspberries, tea, and coffee. If you want to reduce gut inflammation, you may also benefit from supplementing with MSM.

Gut Healing Protein Powder
If you want to reduce gut inflammation and improve your gut health with the help of these natural, gut-supporting, anti-inflammatory herbs and compounds, I recommend that you try this Gut Healing Protein Powder.
It contains curcumin, quercetin, bioflavonoids, ellagic acid, green tea extract, MSM, selenium, and zinc to support your microbiome health, reduce inflammation, support your gastrointestinal health, aid detoxification, and nourish you with clean protein.
Final Thoughts
Gut inflammation can compromise your entire health. It can affect your immune, brain, mental, and skin health, energy levels, and overall wellness. It can lead to gut-related and non-gut symptoms and an array of health issues. With the help of some testing and natural support strategies, you can reduce gut inflammation and related symptoms. I recommend that you follow my tips and support strategies to overcome gut inflammation and regain your health and wellness.
If you want to work with a functional health coach, I recommend this article with tips on how to find a great coach. Our website offers long-distance functional health coaching programs with our world-class team of health coaches. For further support with your health and other goals, just reach out—our fantastic coaches are here to support your journey.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!



Guidance and advices from Dr. Jockers are wonderfull for recovering health and energy !
Thanks for all your support Jorge! Blessings to you!
Excellent coverage of this issue…..all in one spot!
Thank you Kat!
So many wonderful supplements, how do we know which to start taking first ? And what protocol to follow. How can we decide which issues tackle first if there seem to multiple gut issues.