 Improving Vagal Tone for Better Mental and Emotional Health
Improving Vagal Tone for Better Mental and Emotional Health
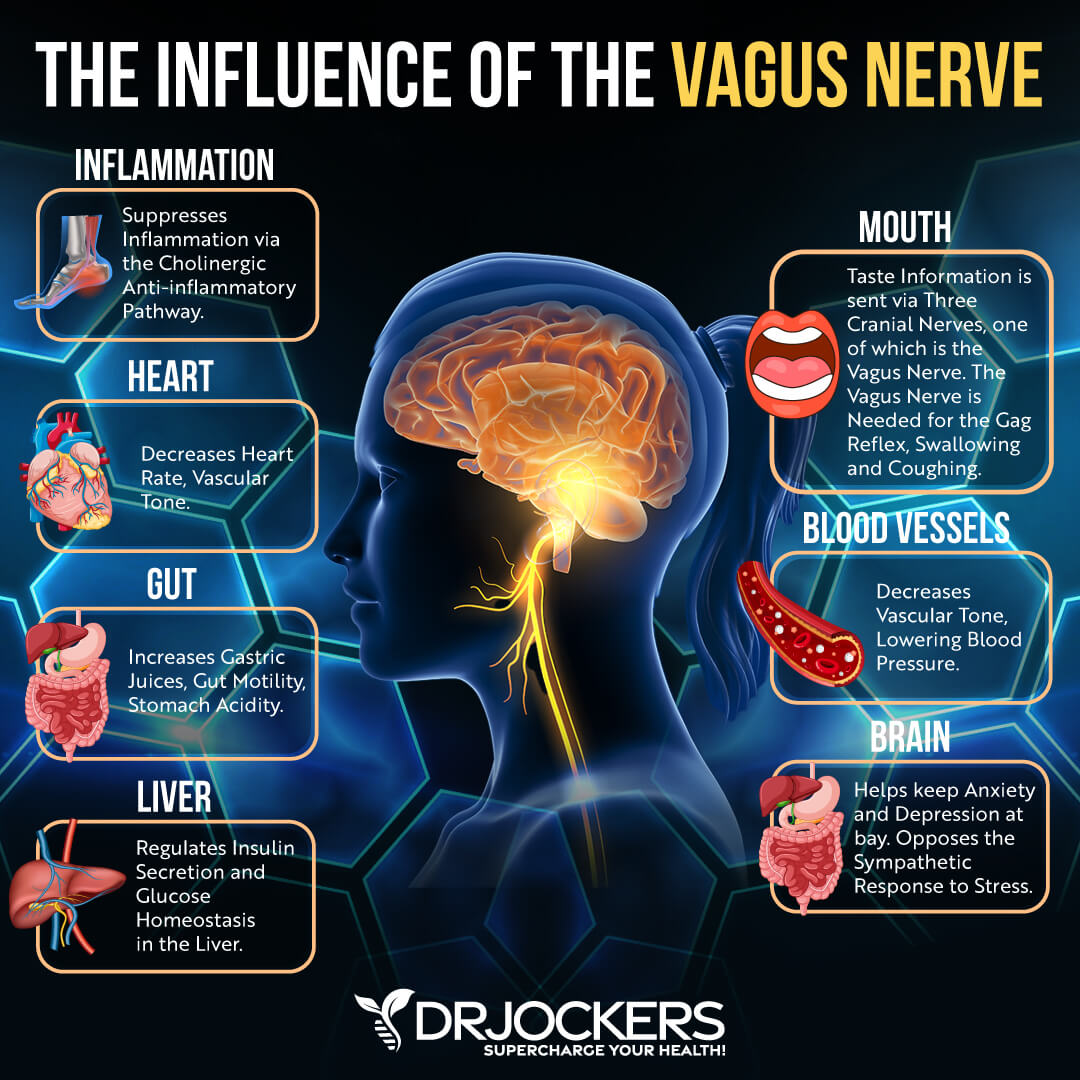
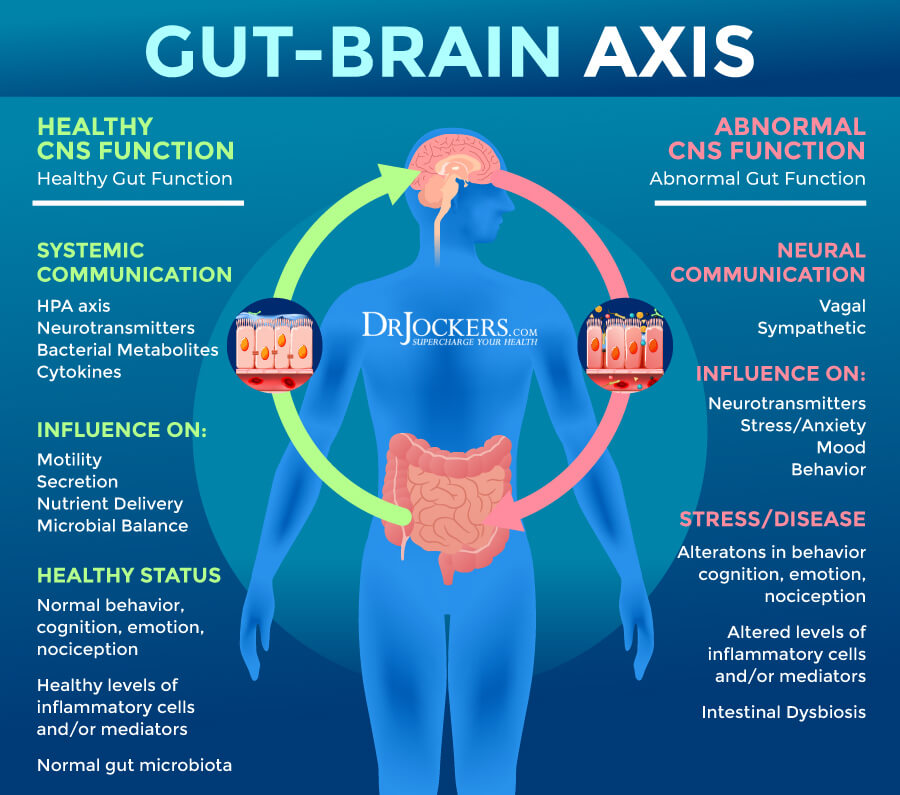
Your vagus nerve is one of the most important nerves that extends from your brain stem through your neck into your chest and abdomen and connects your brain and gut. It helps to regulate your heart rate, breathing, blood pressure, digestion, and emotional state among other functions. If you are experiencing anxiety, depression, stress, fatigue, or any emotional health symptoms, it may mean that you have a poor vagal tone, and your vagus nerve needs some care.
In this article, you will understand the function of the vagus nerve. You will learn more about the polyvagal theory. You will understand the importance of a good vagal tone and the symptoms and main causes of a poor vagal tone. I will explain how to test your vagal tone. I will also share some simple natural strategies to improve your vagal tone for better mental and emotional health.
Functions of the Vagus Nerve
Your vagus nerve, also known as the 10th cranial nerve, is one of your most important nerves in the body. It is also the longest nerve in your autonomic nervous system that extends from your brain stem through your neck into your chest and abdomen. While we refer to them together as ‘the vagus nerve,’ there are actually two vagus nerves, one on the left and one on the right. Vagus is latin for “wandering,” which appropriately describes the nerve.
Your vagus nerve is critical for many functions of our physiology. It connects our brain to our gut. It carries important sensory and motor information. Our vagus nerve supplies innervation to our major blood vessels, heart, lungs, airways, stomach, esophagus, and intestines.
It helps to regulate our heart rate, digestion, blood pressure, sweating, and speech, among other areas of your health. By controlling the muscles of your throat and voice box, it plays an important role of speaking and eating. It also helps your entire gastrointestinal tract working together, regulating your heart rate, and connecting your brain to the rest of your body.
Vagal Tone and Parasympathetic Function
When it comes to the vagus nerve, one of its most important functions is its role as your body’s major parasympathetic nerve. It helps to slow your heart rate, regulate your blood pressure, control sweating, control the gag reflex, allow the involuntary constriction and relaxation of the muscles of your gut, and control vascular tone.
Excessive vagus nerve function can result in nervous system issues and can present in dysautonomias, which are conditions in which the autonomic nervous system (ANS) does not work properly, such as postural orthostatic tachycardia syndrome (POTS).
If the vagus nerve is suddenly stimulated, it may result in a vasovagal reflex that may lead to a slowing heart rate, sudden blood pressure drop, pain, sudden stress, or gastrointestinal symptoms. On the other hand, stimulating the vagus nerve also offers some benefits, including stopping hiccups or supraventricular tachycardia (SVT) and diagnosing heart murmurs.
Since the vagus nerve has many functions and plays an enormous role in your health, scientists, healthcare professionals, and mental healthcare professionals have been interested in its role and how to support it.
The electronic stimulation of the vagus nerve through vagus nerve stimulating (VNS) devices have been used for epilepsy and depression and is under investigation for inflammatory disorders, tinnitus, migraines, fibromyalgia, hypertension, weight loss, and other conditions.
Polyvagal therapy is an emerging theory looking at the role of the vagus nerve in emotion regulation, social connection, fear response, stress, mental health, and trauma recovery (1, 2, 3, 4, 5, 6, 7).

The Polyvagal Theory
The animal world can bring us some great examples to help us understand our own behavior and the nervous system. Imagine a group of gazelles peacefully grazing. Suddenly they notice that a lion is nearby. One gazelle becomes hyper aware. The lion notices her fear and begins to chase her. The gazelle is running until it gets caught.
As soon as it is caught, her parasympathetic nervous system kicks in and she goes limp. Instead of eating her right away, the lion plays with it for a while. One moment, the lion gets distracted, the gazelle’s sympathetic nervous system kicks in, seeing an opportunity, she sprints away despite her injuries.
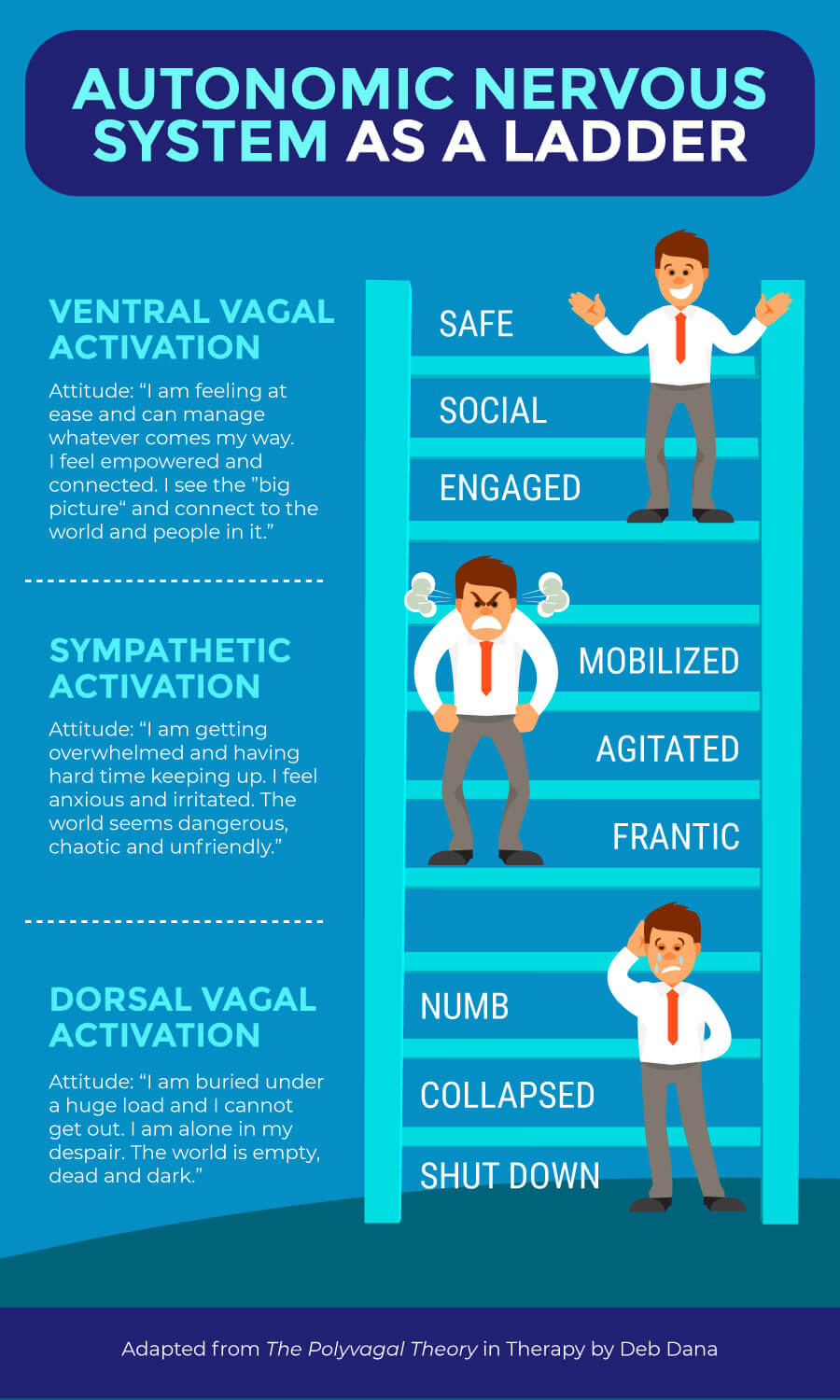
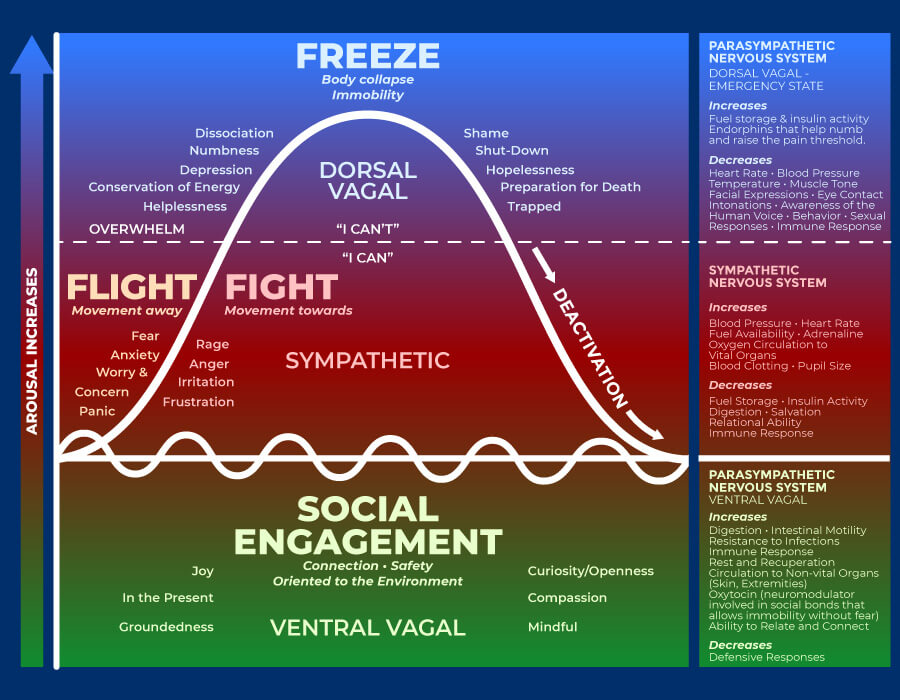
While grazing, the gazelle felt safe and connected, when she was caught, her body went through a shutdown, but when the opportunity arose, flight-or-fight kicked in and ran away. This story covers the exact same three states that the polyvagal theory focuses on connection, fight or flight, or shutdown.
Before the emergence of the polyvagal theory, we only understood the nervous system as a two-part system with more activation and less calm or less activation and calmer. The polyvagal theory identified the social engagement system as a third type of nervous system response.
If you are emotionally healthy in a non-stressful situation, you are in a normal state the polyvagal theory refers to as connection. In this state, you are able to make healthy connections with humans and feel safe. At this point, you feel happiness, peace, openness, calm, groundedness, and curiosity. You sleep well. You eat normally without overeating or undereating. Your immune system is functioning well. Your face is expressive, your body is calm, and you are able to relate to others emotionally.
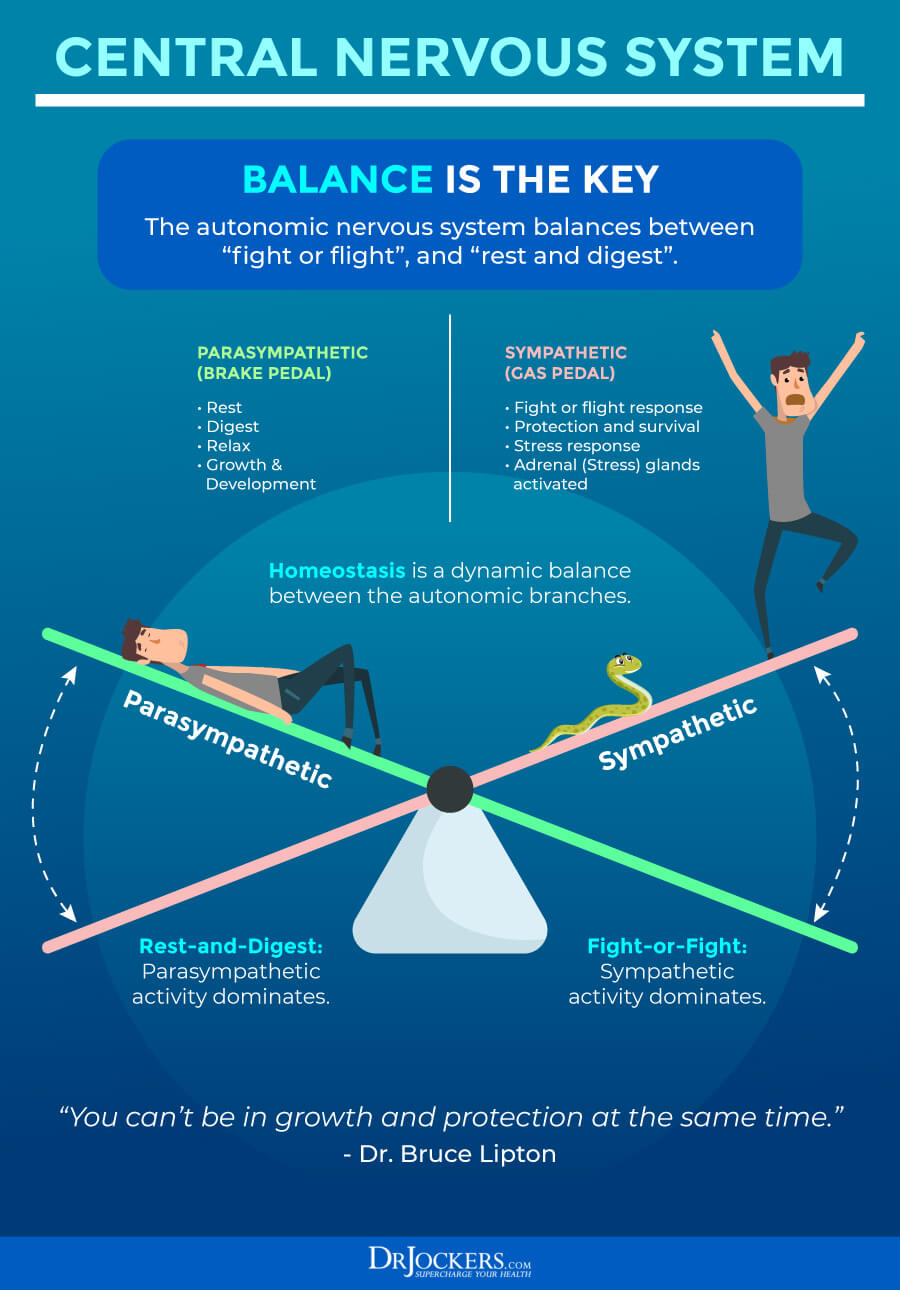
Fight or Flight vs Rest and Heal
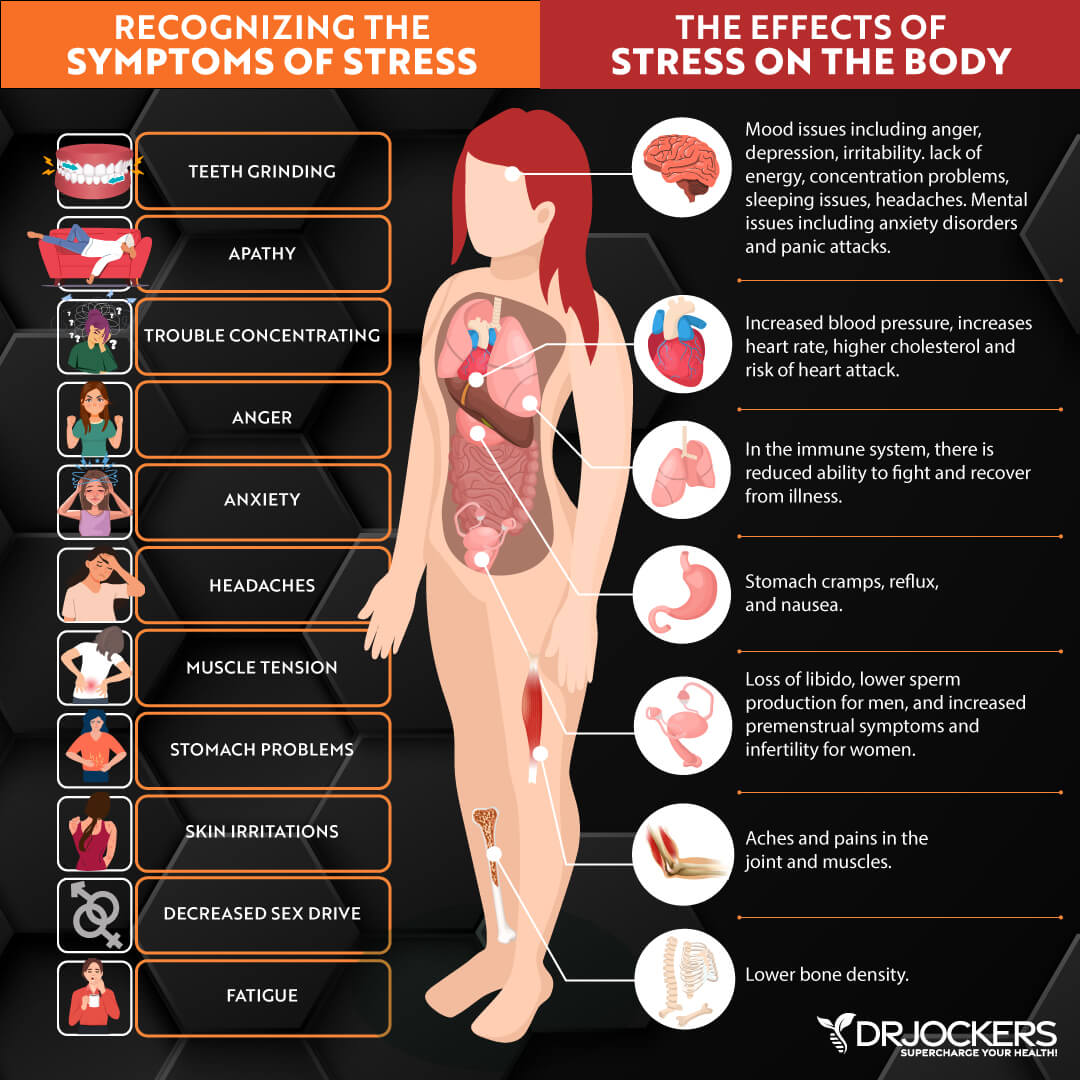
When you are under stress, it affects your entire body. Your sympathetic nervous system causes a flight-or-fight response to keep you alive. Even if you are not in real danger, but only experiencing daily stress, your body wants to keep you safe.
If your body senses a threat, it may freeze and look for danger around you. It raises cortisol, epinephrine, and norepinephrine. You feel anxious, angry, or afraid that may be apparent on your face too. You start sweating, your heart rate increases, your digestion slows down, and your blood vessels constrict. You feel tension, pain, trembling, or vibration. You may clench your fist; you may show guarded body language or want to appear bigger. You may feel like running away.
Another way your body may react to stress is by shutting down or freezing, just like the gazelle did when caught. If your body feels real danger or senses that it can’t escape, the parasympathetic nervous system may kick in to create a shutdown. You may feel hopeless, numbness, shame, a sense of feeling trapped, disconnected, or dizziness. You may disassociate. You may feel nauseous, breathe slower, or experience a decrease in your heart rate, blood pressure, immune response, sexual desire, and sensation of pain. Your digestive system slows down, your eyes become fixated, and you have difficulty speaking.
Experiencing a flight-or-fight or shutdown response to something scary, stressful, or triggering is absolutely healthy. We all do it. If there is a flash of lightning, or your boss calls you into their office unexpectedly, or someone suddenly cuts you off on the highway, you may experience signs of flight-of-fight, including increased heart rate, heavier breathing, or a need to scream.
These experiences of flight-or-fight or shutdown are supposed to be acute, short events. A healthy nervous system and the vagal nerve are supposed to shake off this stress and bounce back to a calm, safe, and connected state. However, people who are experiencing poor vagal tone due to childhood abuse, trauma, or other factors, are experiencing this response constantly. When flight-or-fight or shutdown becomes a chronic state, it becomes a problem. It increases the risk of both mental and physical health issues.
Vagal Tone and Polyvagal Therapy
Having a history of trauma can increase your perception of physical or emotional danger around you. You may be more likely to find yourself regularly in a flight-or-fight or shutdown mode instead of a peaceful connection mode even in so-called normal situations. Your body may perceive certain incidents threatening that are less or not threatening to others. Those with a trauma history may live in a constant state of fear or disconnect.
War veterans are often triggered by thunderstorms or fireworks. Survivors of abuse may feel triggered and go into flight-or-fight or shutdown mode when they hear someone yelling or even raising their voice mildly. This is why the polyvagal theory and polyvagal therapy can be so beneficial for the treatment of post-traumatic stress disorder (PTSD) and other trauma-related mental health or psychophysiological issues. It helps bring the body back to connection and safety.
What if you haven’t experienced serious trauma? First, you have to understand the trauma may not always come from so-called serious events. When we talk about trauma, we usually talk about war, sexual abuse, physical violence, emotional abuse, serious accidents, and so on. These big traumatic events are also referred to as “big T’s.” However, there are also “little t’s.” These are less distressing events that may still impact your life.
For example, a teacher not complimenting a child on their work that they are proud of or your best friend not attending your birthday party may leave a mark. These “little t’s” can add up and lead to triggers later in life. Besides trauma though, there are also lifestyle, dietary, and health factors that may affect your vagal tone and lead to the same emotional and mental health symptoms. You will learn about these contributing factors in a later section of this article (8, 9, 10, 11, 12, 13).
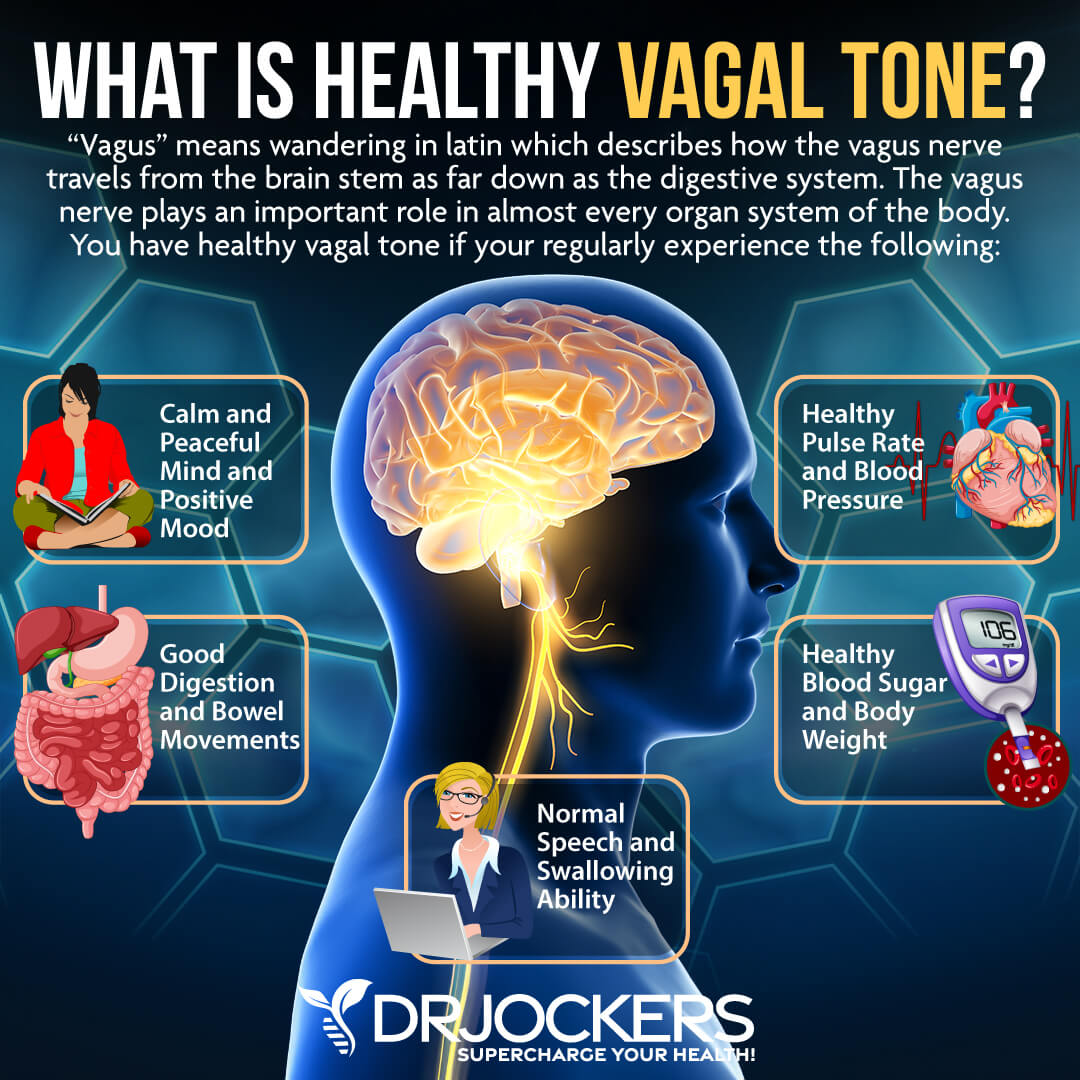
The Importance of Good Vagal Tone
The vagal nerve is involved in many areas across your body making a good vagal tone very important. A good vagal tone is important for
- Lowering blood pressure
- Lowering heart rate
- Managing stress and anxiety
- Regulating mood
- Decreasing inflammation or pain
- Delivering information between the brain and the gut
- Providing sensory information from the throat, lungs, and heart
- Regulating swallowing
- Regulating speech
Symptoms of Poor Vagal Tone
Sometimes the vagal nerve is damaged resulting in poor vagal tone. Symptoms of poor vagal tone due to nerve damage may include:
- Abdominal pain
- Nausea
- Vomiting
- Unusual heart rate
- Unusual blood pressure
- Loss of gag reflex
- Earache
- Lowered stomach acid
- Loss of voice
Even if your vagus nerve isn’t damaged, you may experience poor vagal tone. Symptoms of poor vagal tone even without nerve damage may include:
- Anxiety
- Depression
- Poor emotional regulation
- High stress
- Being in flight-or-fight mode
- Lowered attention span
- Increased inflammation
- Pain

Major Causes of Poor Vagal Tone
You may experience poor vagal tone due to a variety of reasons, including past life experiences, health issues, and lifestyle choices. Let’s look at the major causes of poor vagal tone.
Chronic Stress & Poor Sleep
Chronic stress and poor sleep may both interfere with your sense of inner safety and lead to poor vagal tone. When your body is experiencing stress, your body will go into a flight-or-fight mode to protect you. Your amygdala signals your hypothalamus to increase your heart rate, heighten your senses, generate heavier breathing, cause greater oxygen intake, increase cortisol levels, and rush adrenaline across your system.
While this response is certainly important, when you are under chronic stress, your body will be in a constant flight-or-fight mood leading to chronically increased cortisol levels. This can wear your brain down, interrupt the vagal tone, disrupt synapse regulation, impair brain function, and compromise your mood.
Chronic poor sleep increases chronic stress and ends up feeding a vicious cycle of a stressful state over safety. This cycle can increase your risk of mental health issues, fatigue, dementia, Alzheimer’s disease, and other neurodegenerative diseases (14, 15, 16, 17, 18).
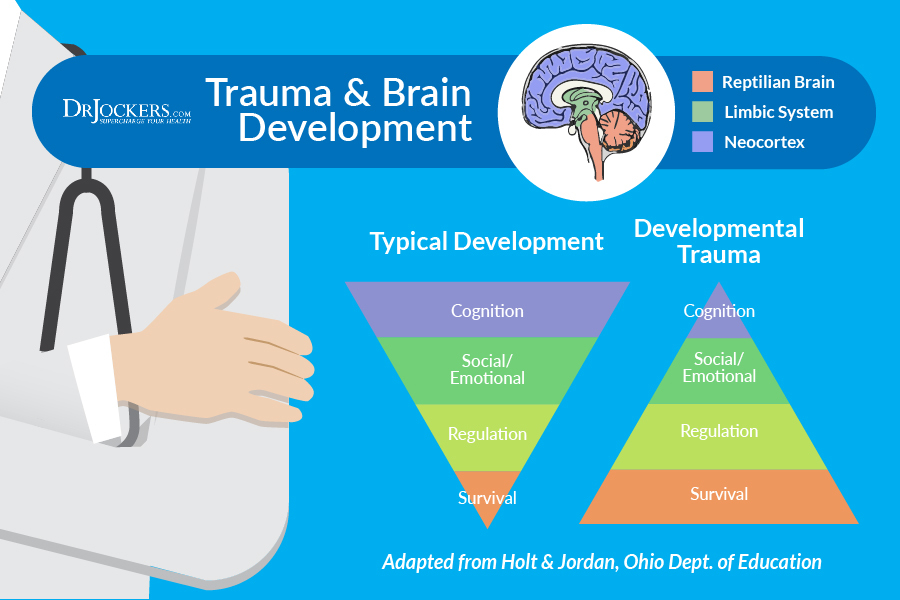
Early Childhood Traumatic Experiences
Your early years are incredibly important for your neurological and overall development. This is the time when you are looking for safety and comfort. This is the time when you are learning safe social cues that you can rely on later in life. However, children who grow up in an abusive home either don’t receive safe social cues or see these safe social cues within an abusive environment and receive mixed messages.
Children who experience trauma also experience an interruption of safety. This feeds a chronic state of flight-or-fight or shutdown danger state they may continue to experience throughout their lives.
Experiencing other forms of trauma, including serious car accidents, serious illness or hospitalization, losing a parent or loved one, deep poverty, or war also negatively affect the vagus nerve and may lead to a chronic flight-or-fight or shutdown danger state. Those who score high on the Adverse Childhood Experiences (ACEs) test tend to have a poor vagal tone and are more likely to be in a chronic flight-or-fight or shutdown mode and develop various mental and physical health issues as a result (19, 20).
While our early childhood years are the most critical for healthy development, traumatic experiences later in childhood, during your teenage years, or adult years can affect your vagal tone as well. Post-traumatic stress disorder, which is accompanied by a poor vagal tone, often develops due to traumatic experiences later in life, for example, experiencing war, physical or sexual assault, domestic abuse, car accidents, losing a loved one, or serious illness (21).
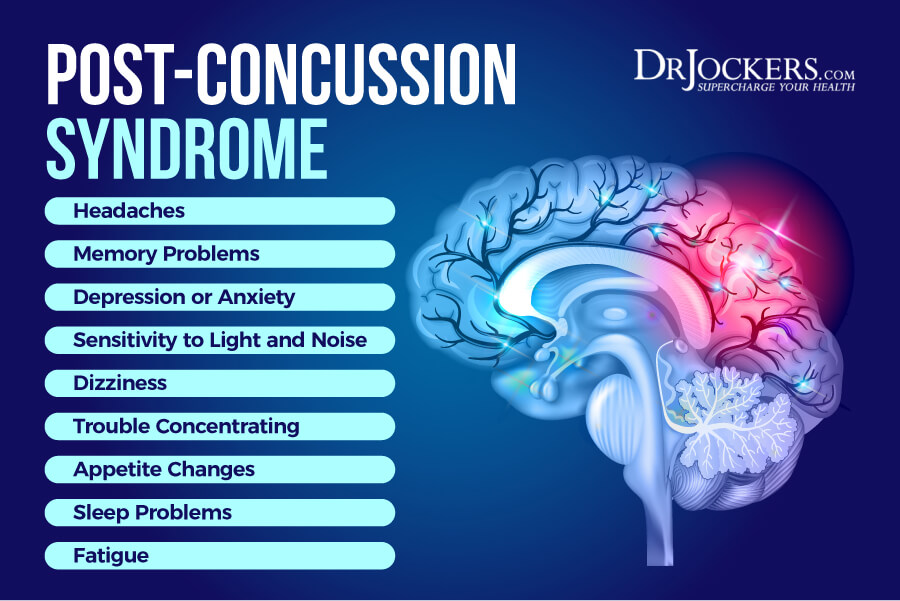
Head Injuries and Vagal Tone
Head injuries may lead to poor vagal tone. These injuries may specifically cause an injury to the vagal nerve leading to symptoms of a poor vagal tone. In some cases, a concussion or traumatic brain injury affects the function of the vagus nerve.
Even if the head injury doesn’t have a lasting impact, it may become a traumatic experience that feeds into the problem of a poor vagal tone. Stimulation of the vagus nerve may have neuroprotective benefits and may help recovery from traumatic brain injury (22).
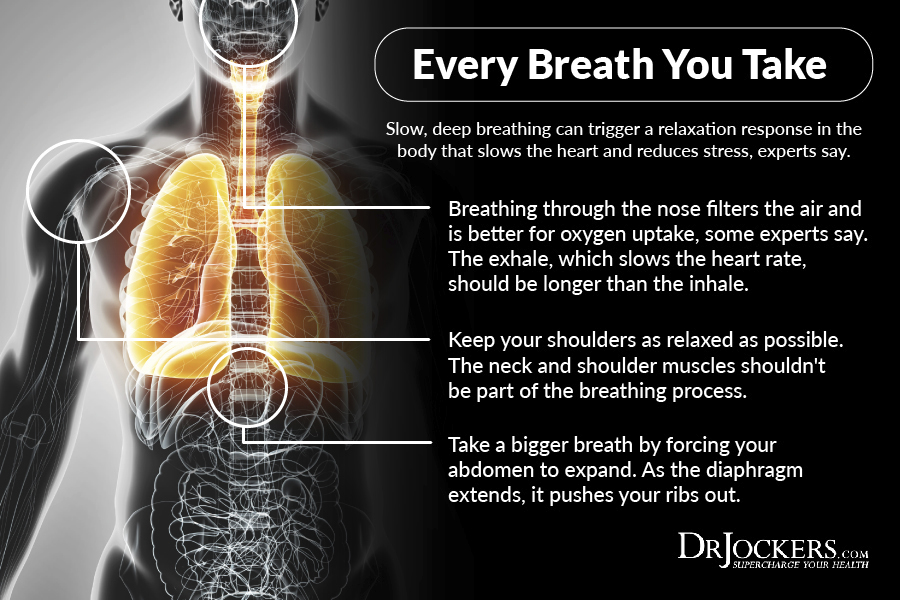
Poor Breathing Mechanics
Throughout your day, you are probably taking shallow breaths that you don’t even notice. When you are under stress, you may notice your breathing and heart rate speeds up. If you have anxiety, you may experience increased breathing out of nowhere for no apparent reason.
If you have a poor vagal tone, your breathing may be erratic and likely not conscious. Poor breathing techniques can interrupt your vagus nerve function and feed into the symptoms of poor vagal tone. On the other hand, being more conscious about your breath and taking slow, deeper breaths from your belly can benefit your vagal tone and get you out of a flight-or-fight state (23).
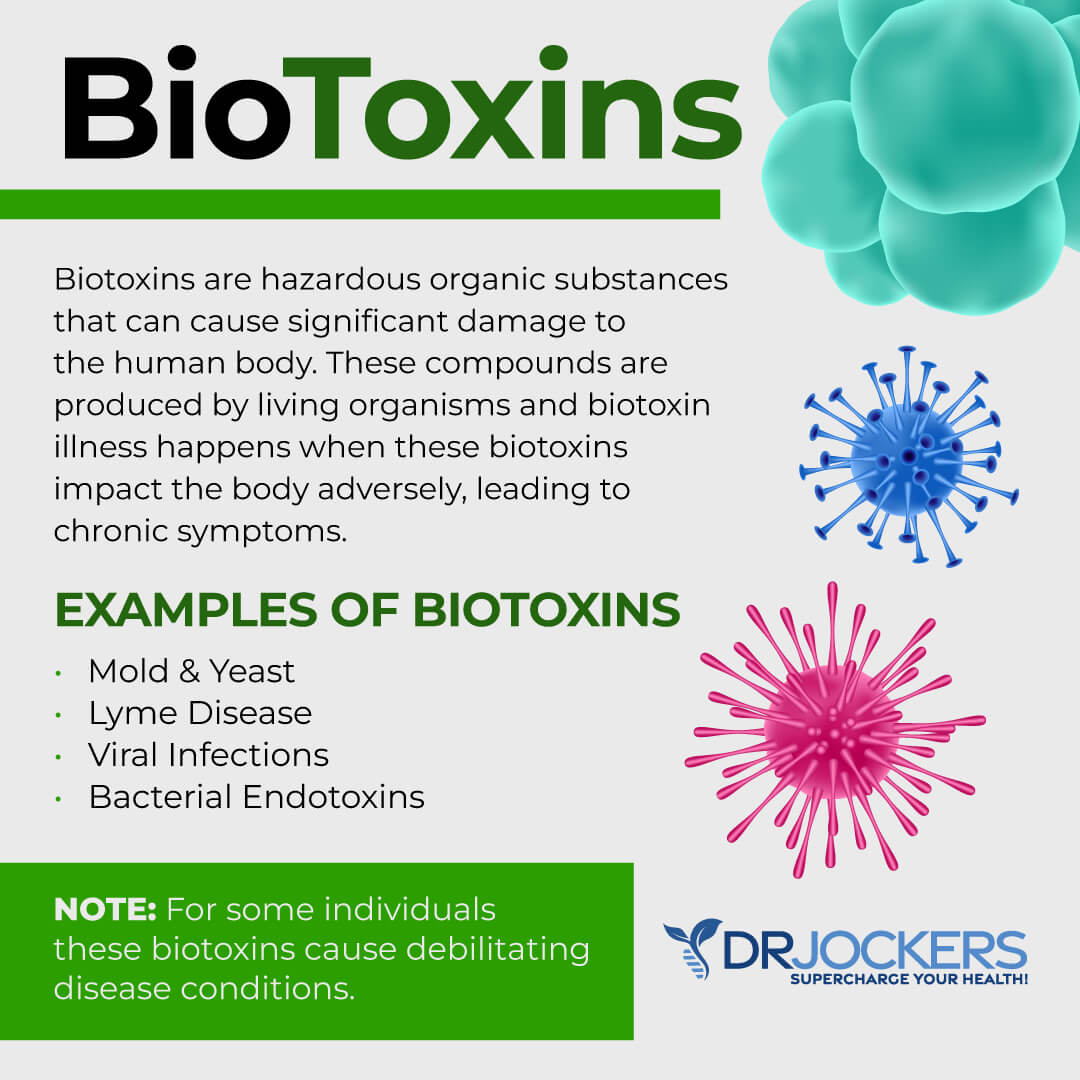
Chronic Infections
Chronic systemic infections, including infections from the Epstein Barr Virus (EBV), the Borrelia bacterium responsible for Lyme disease, enteroviruses, Varicella zoster virus, chickenpox, and HHV-6 play an important role in your brain and nervous system health.
These infections may appear around the vagus nerve and may be responsible for Chronic Fatigue Syndrome (CFS), mental health, and neurodegenerative issues. These systemic infections can compromise your brain health, trigger inflammation, pain, and a variety of symptoms. Chronic infections may increase your risk of anxiety, depression, fatigue, brain fog, memory issues, cognitive issues, and other mental health or neurological problems (24).
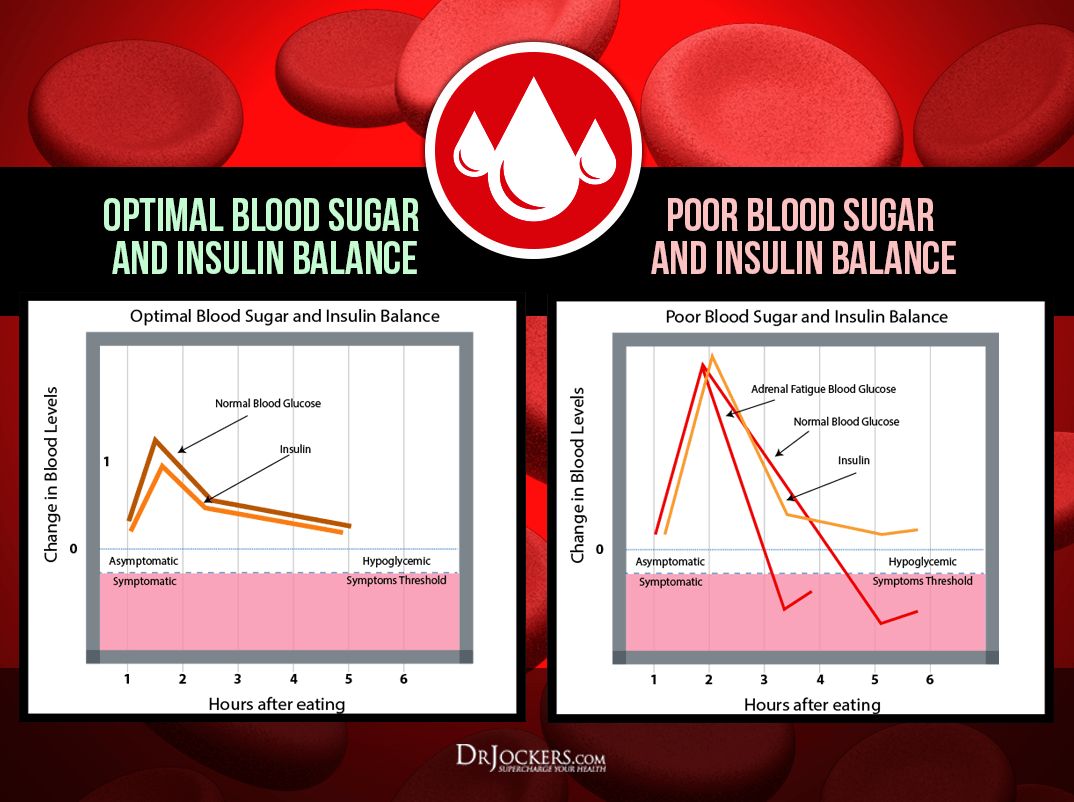
Blood Sugar Imbalances
A diet high in refined sugar and processed carbohydrates and low in vegetables, brain-protecting healthy fats, and clean protein, may lead to blood sugar imbalances. High-carb snacks and carb-heavy meals may provide short-term energy but they cause a sudden blood sugar drop characterized by fatigue and brain fog.
Blood sugar imbalances can compromise your sympathetic and vagal nerve function as well as your brain and neurological health. Blood sugar imbalances can result in various symptoms that may be related to poor vagal tone, including brain fog, irritability, lightheadedness, mood fluctuations, anxiety, fatigue, and cravings (25, 26, 27).
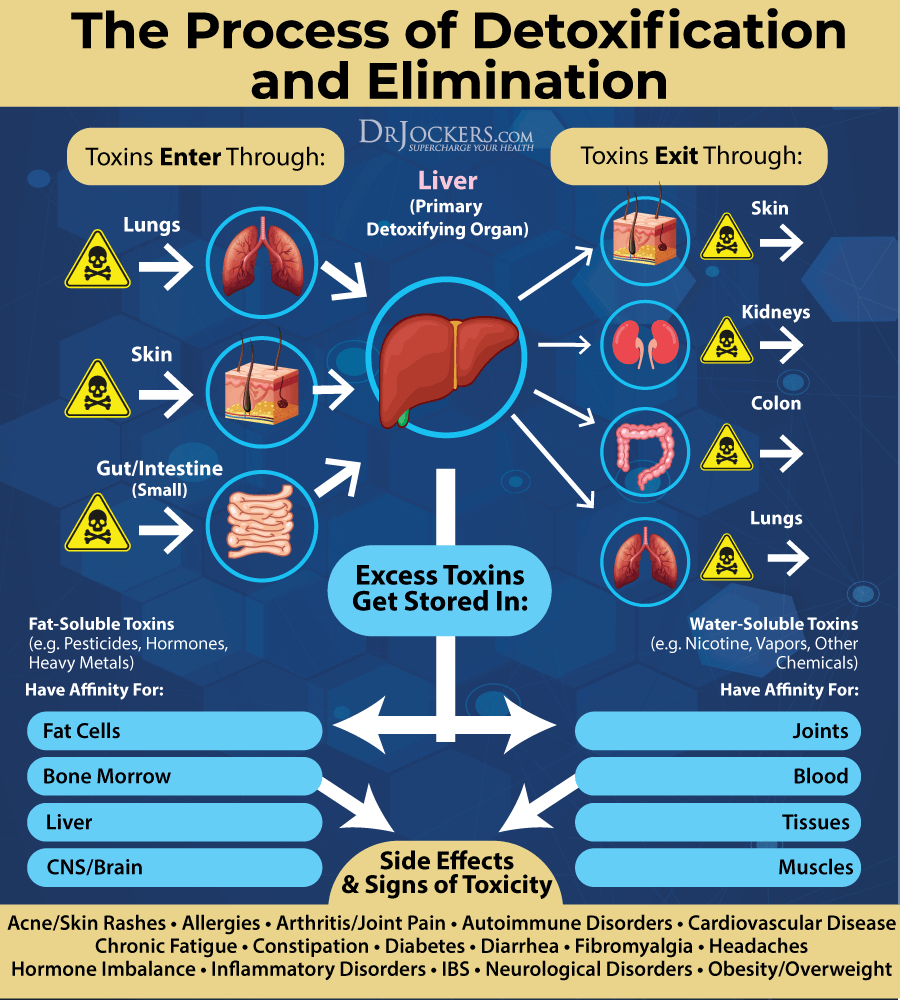
High Toxic Load
Unfortunately, our environment is full of toxins. You may encounter toxins through polluted air, municipal tap water, non-organic and processed foods, moldy indoor spaces, plastic products, and conventional beauty, body, and household products, medications, cigarette smoke, and more.
A high toxic load may have a tremendous impact on our brain, neurological function, and overall health. Neurotoxins, such as ethanol (in alcohol), monosodium glutamate (MSG), heavy metals (such as aluminum, lead and mercury), botulinum toxin (in Botox), tetrodotoxin, and tetanus toxin, are particularly damaging to your brain function.
Toxins from non-organic food products may travel up to your brain and compromise your cognition, mood, and brain health. Environmental toxicity may lead to poor vagal tone, anxiety, depression, fatigue, memory problems, brain fog, dementia, and neurodegenerative diseases (28, 29, 30).
Testing Your Vagal Tone
Besides looking at your symptoms and risk factors, there are several ways you can test if you have a poor vagal tone.
Heart Rate to Breath Rate Comparison
Heart rate is the speed of your heartbeat based on the number of contractions or beats per minute. Your heart rate depends on your actual activity. Normal resting heart rate is defined as 60 to 100 beats per minute by the American Heart Association. A normal breath rate is 12 to 20 breaths per minute.
If you are really athletic, fit, or very calm, it is on the lower end or lower. Your breath rate is about a fifth of this. If your heart rate is regularly too high or the comparison between your heart rate and breath rate is irregular or abnormal, you may have a poor vagal tone (31).
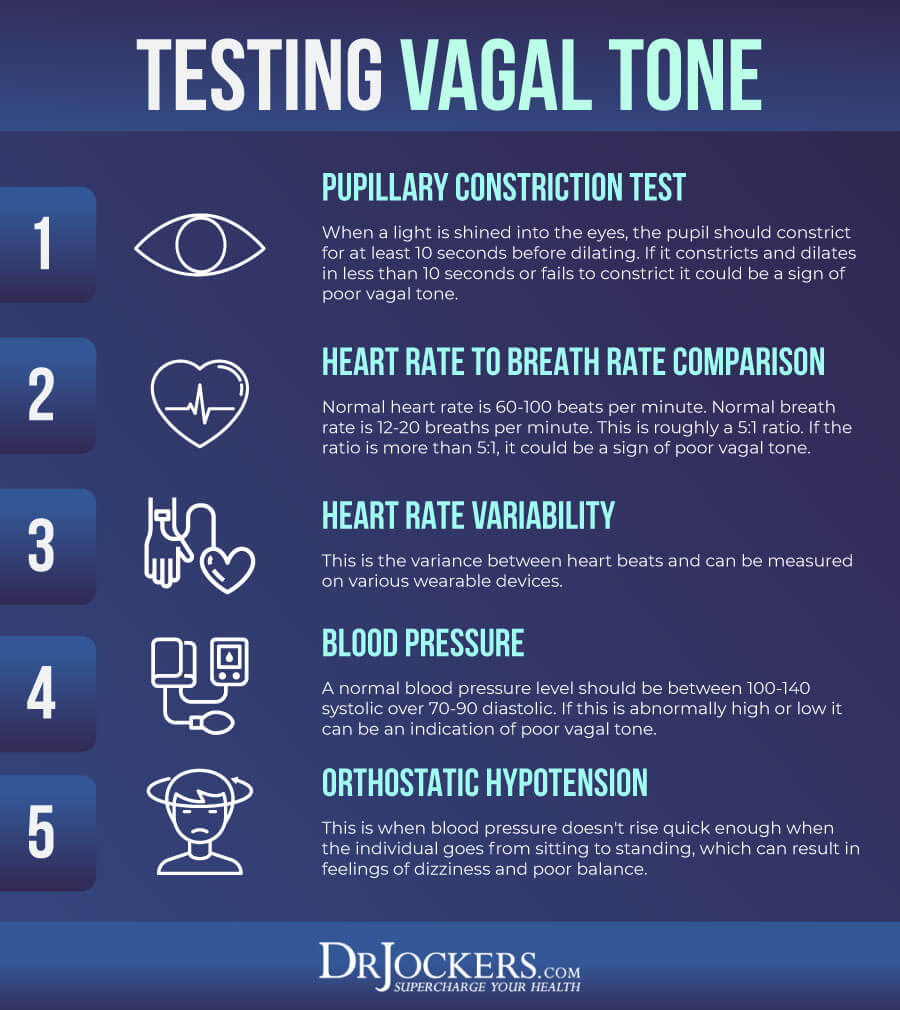
Blood Pressure:
The adrenals and vagal nerve activity play a big role in helping to maintain normal blood pressure levels. A normal resting blood pressure should be in the range of 100–140 mm/Hg systolic over 60-90 mm/Hg. diastolic. Individuals with sympathetic dominance (high stress hormones) will have high blood pressure while individuals with parasympathetic dominance (low stress hormones) will have low blood pressure.
A resting blood pressure over 140/90 mm/Hg can be a sign of poor vagal tone and high sympathetic drive. A resting blood pressure under 100/60 mm/Hg may be a sign of dorsal vagal output causing the “freeze” impact on the body which reduces circulation and healthy blood pressure leading to fatigue.
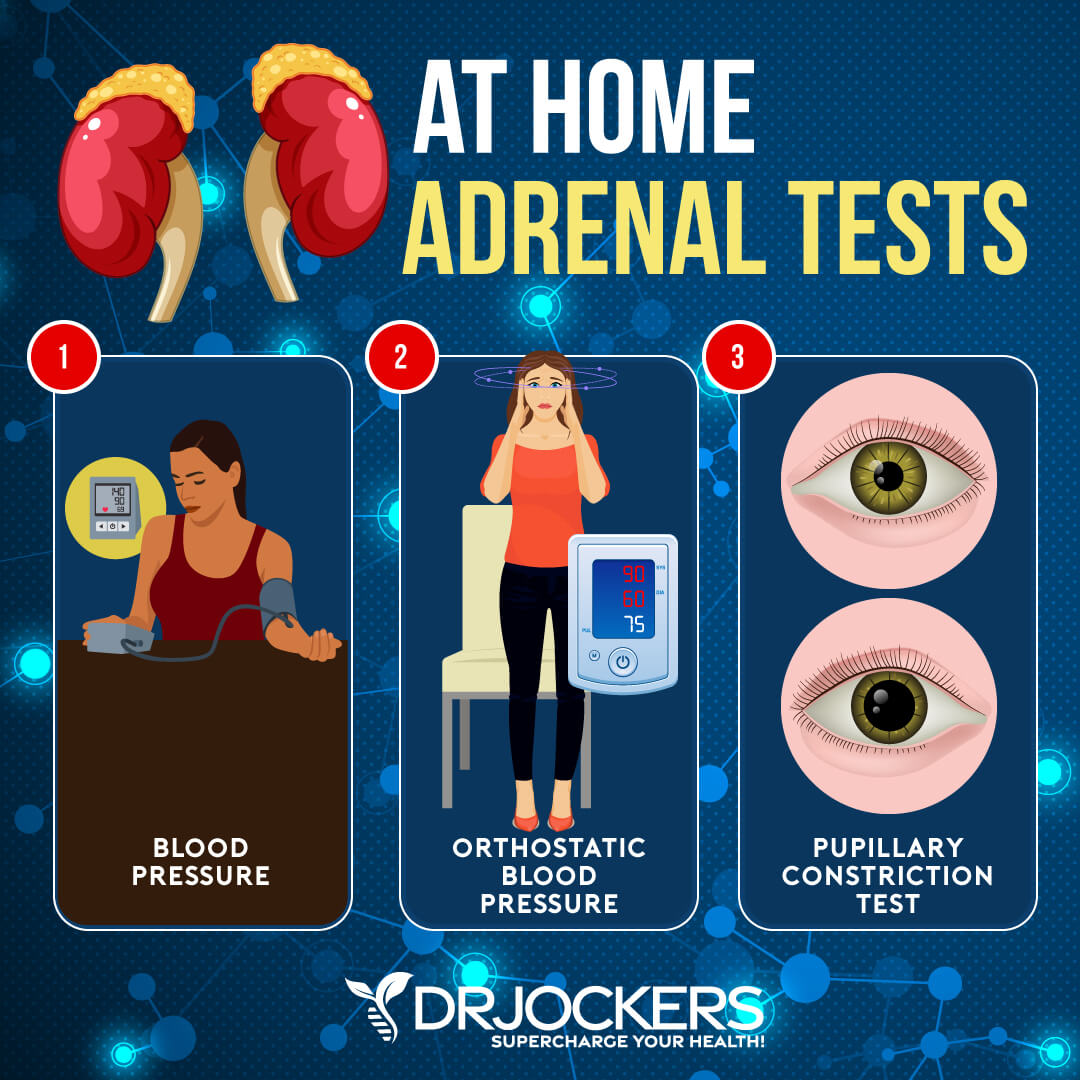
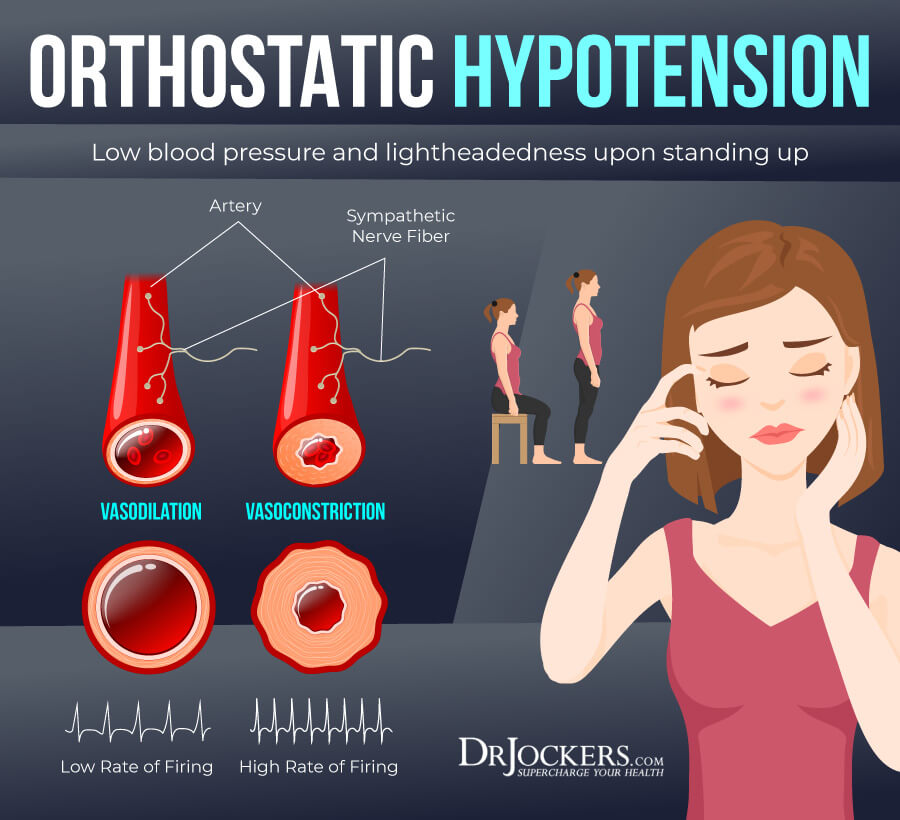
Orthostatic Hypotension Test:
All you need for this one is a blood pressure cuff. Lie down for 5 minutes and then take your blood pressure and make note of it (especially the systolic – top number). Then stand up and take your blood pressure again immediately. Healthy vagal and sympathetic balance will cause an increase in blood pressure upon standing which causes the appropriate amount of blood flow to get to your brain so you feel stable and unfazed by the movement.
The systolic pressure should naturally rise about 10 mm/hg when you go from sitting to standing. If the systolic pressure remained the same or it decreased, there is a chance you have adrenal fatigue. When we stand, epinephrine is normally secreted to increase the blood pressure to overcome gravity and pump blood towards the heart.
3. Pupillary Constriction Test:
This test was first described in 1924 by Dr. Arroyo. It measures the contraction of the iris in response to dark light exposure. The hypothalamic-pituitary-adrenal (HPA) axis helps to control the contraction of the iris.
When someone is dealing with poor vagal tone due to sympathetic dominance or high dorsal vagal activity, they are unable to maintain the contraction for a normal length of time. Here is how you do the test.
- Set up the Room: Sit in front of a mirror in a dimly lit room.
- Use a Flashlight: Take a flashlight and shine it into your eye from the side of your face (45 degree angle). When this happens, your eyes will naturally constrict and the diameter will reduce in size. Here are the possible results:
Pupillary Response: Possible Finding:
Stays constricted for 20+ seconds Healthy Vagal/HPA Axis
Fasciculates between 10–20 seconds Mild Vagal and HPA Axis Disruption
Fasciculates between 5–10 seconds Vagal/HPA Axis Fatigue
Immediate pulsation and dilation Vagal/HPA Axis Exhaustion/Failure
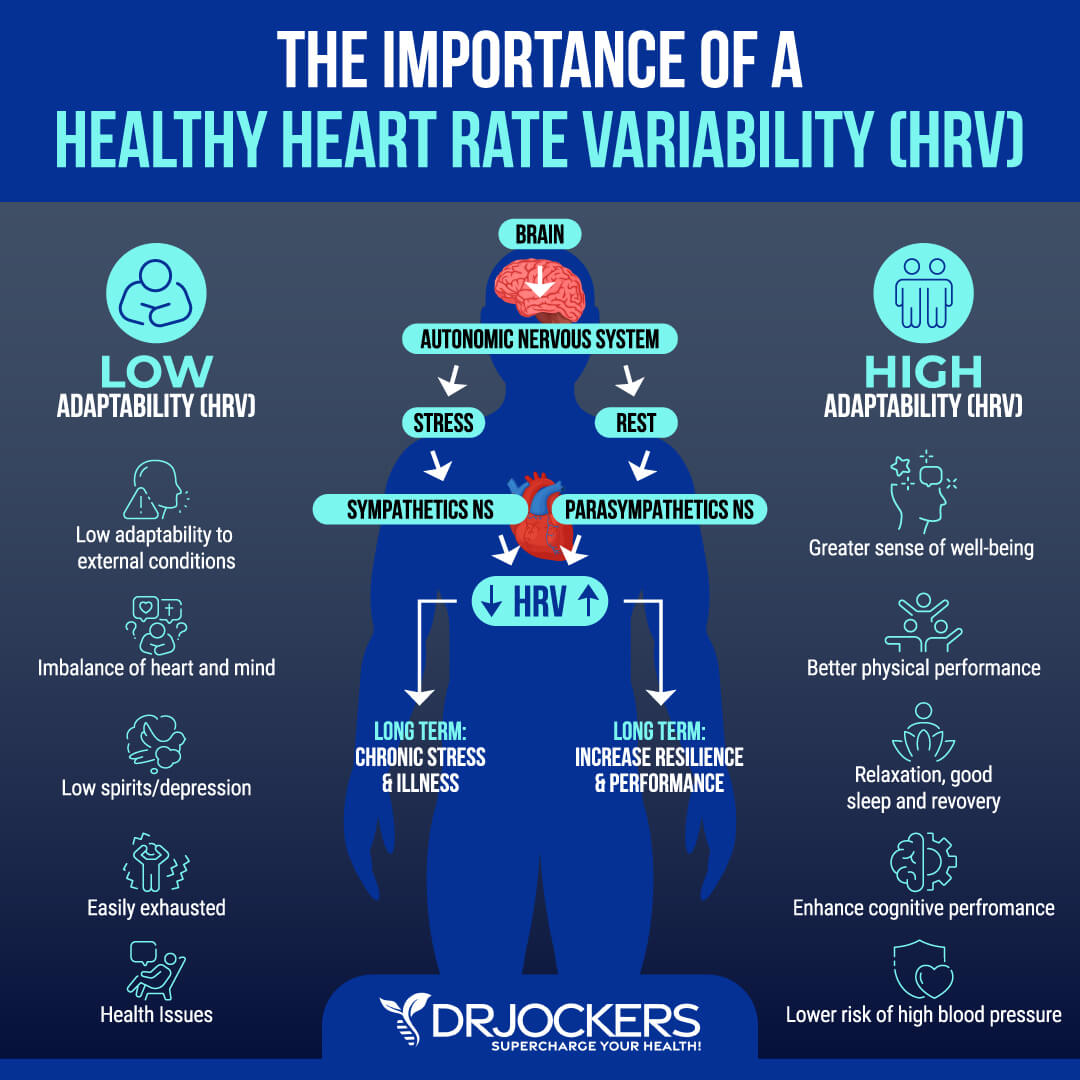
Heart Rate Variation
Heart rate variability (HV) refers to the variation in the time interval between your heartbeats or your beat-to-beat interval. There are various methods that can help to detect abnormal HRV, including ECG, blood pressure measures, ballistocardiography, and photoplethysmograph (PPG). An abnormal HRV may mean that you have a poor vagal tone (32).
Top 12 Strategies To Improve Vagal Tone
If you are experiencing signs and symptoms of a poor vagal tone, there are various strategies you can practice to improve your vagal tone. Here is what I recommend:
Reduce Stress & Improve Sleep
Reducing stress and improving your sleep can help your body to return to a safe and happy state. Sleep also allows rest, repair, and rejuvenation. Reduce stressful situations and time with people that bring you down. Engage in relaxing and de-stressing activities, including prayer, meditation, journaling, nature walks, exercise, healing baths, and reading.
Practice positive affirmations and develop a positive mindset. Make sure that you get 7 to 9 hours of sleep each night. Go to bed and wake up around the same time every day to support your body’s circadian rhythm. Avoid food, stress, and electronics close to bedtime, and engage in relaxing activities. Make sure that your bedroom is a safe and comfortable sanctuary.

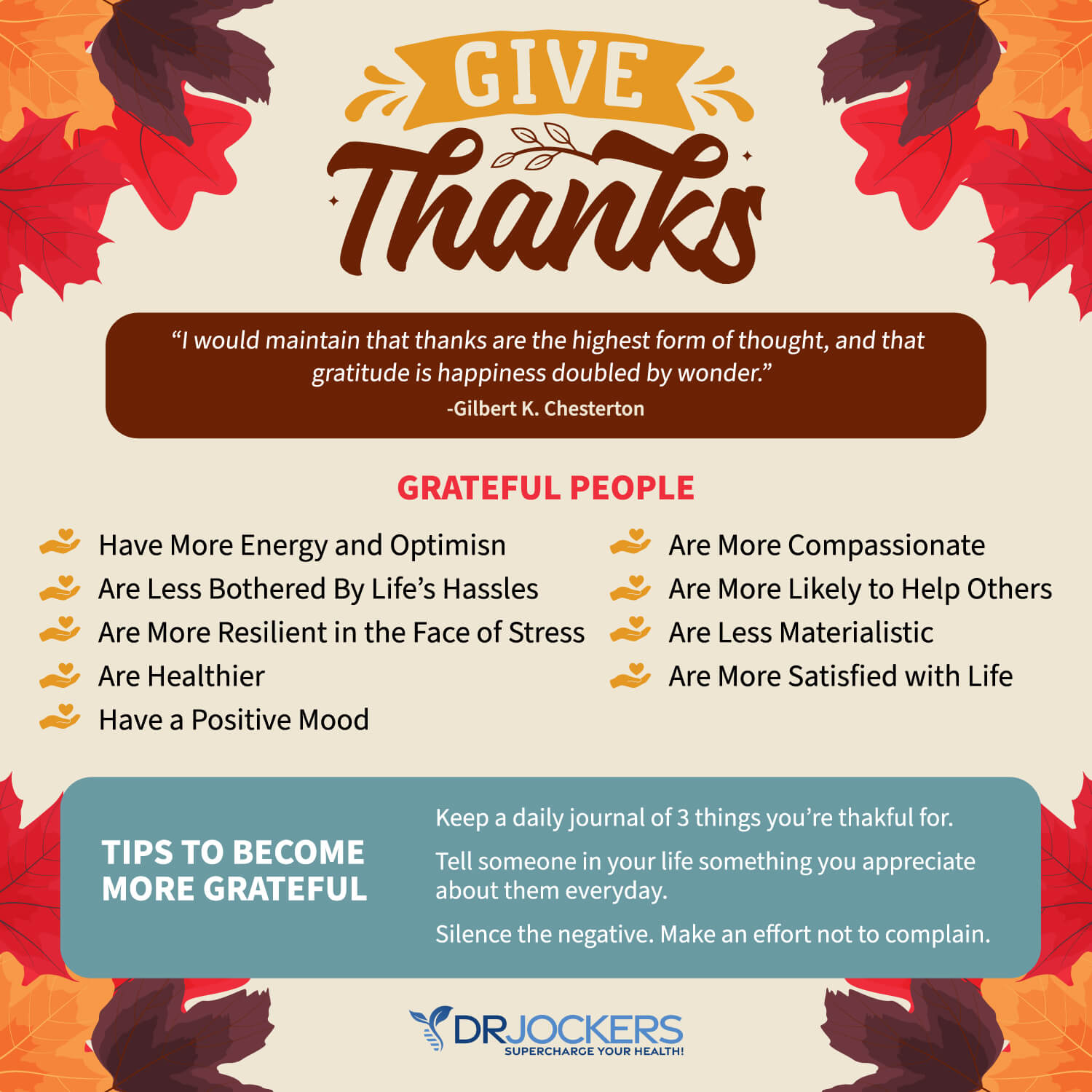
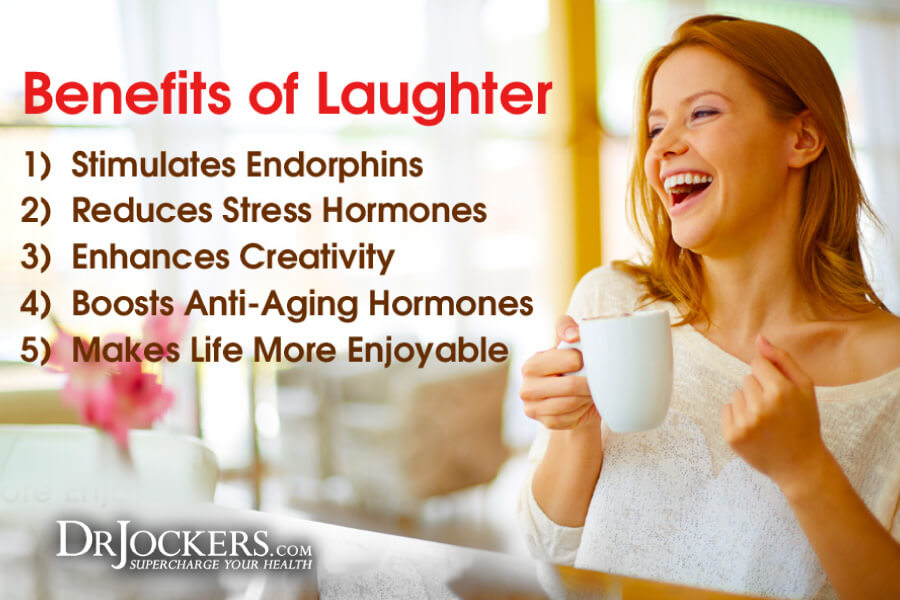
Practicing Gratitude and Laughter
Practicing gratitude is one of the best ways to keep your body and emotions at a happy, safe, and positive place. Keep a gratitude journal. Stop throughout the day to acknowledge the small things. If you notice that you are stressed, anxious, or angry, or find yourself in a flight-or-fight or shutdown state, stop, and identify three things that you can be grateful for. This can automatically bring you back to a safer state.
Laughter is another great way to stimulate your vagus nerve, bring your energy up, and create safety. Find a funny video, watch a comedy, engage in activities and social situations that bring on laughter, and don’t be afraid to laugh at yourself. If you feel anxiety, stress, or a lack of safety, think about something funny to bring yourself back to a safe state.
Social Connections with Others
According to the polyvagal theory, our healthy state is a safe and connected state. Poor vagal tone can create a chronic flight-or-fight or shutdown response. Social connections with supportive and loving people can help you to feel safe and create a connected state.
Spend time with friends and family. Go to church or participate in other uplifting groups. Volunteer. Take some arts and crafts workshops or other community classes.
Join a community walking group. If you are a woman, you may look for a women’s circle. Join a book club, film club, or coloring group. Look for activities at your library. If it is difficult for you to put yourself out there or if you struggle with social anxiety, it may be beneficial for you to join a support group led by a therapist or a small supportive group led by a life coach or spiritual counselor.
Deep Breathing, Meditation, and Prayer
Deep breathing, meditation, and prayer are fantastic ways to improve your vagal tone and calm your system. During our everyday lives, most of us tend to take very shallow breaths from our chest. Set aside time to practice some deep breathing. Take a long breath deep into your belly to stimulate your vagus nerve and create energy.
Set aside time for daily prayer and meditation to tone your vagus nerve, create safety in your body, and calm your mind. You may use guided meditation, loving-kindness meditation, somatic tracking, or other strategies. Find what works for you. Prayer of any kind helps to connect to a higher purpose and allows you to find safety and connection and helps to create a sense of calmness (33).
Stimulating the Palatal Muscles
Poor vagal tone negatively affects your muscles in your throat and mouth which may affect your speech and ingestion of food. Your vocal cords are also connected to your vagus nerve. Stimulating your palatal muscles and vocal cords help to stimulate your vagus nerve and improve your vagal tone.
Humming, singing, chanting, talking, and gargling are great practice to improve your vagal tone. Chances are, you will also feel instantly uplifted and out of flight-or-fight danger mode.
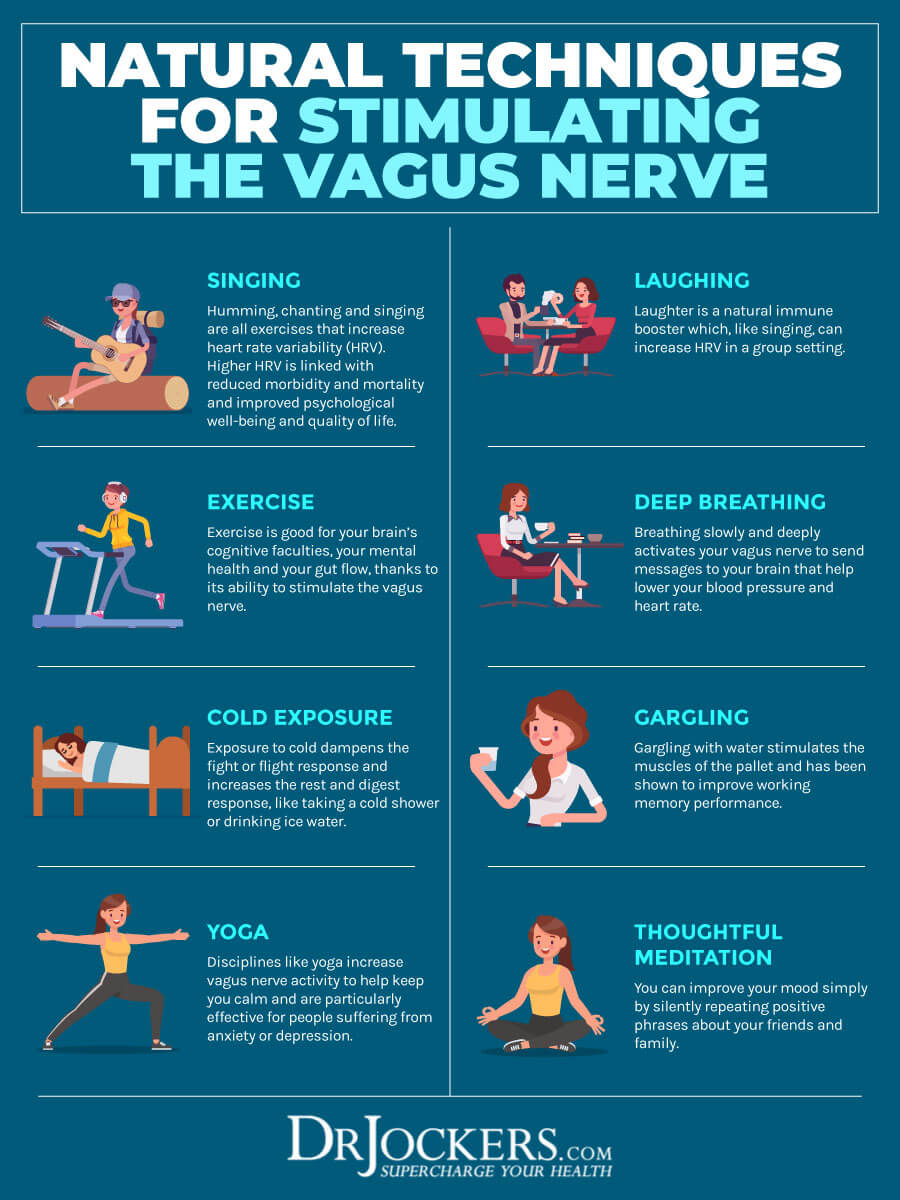
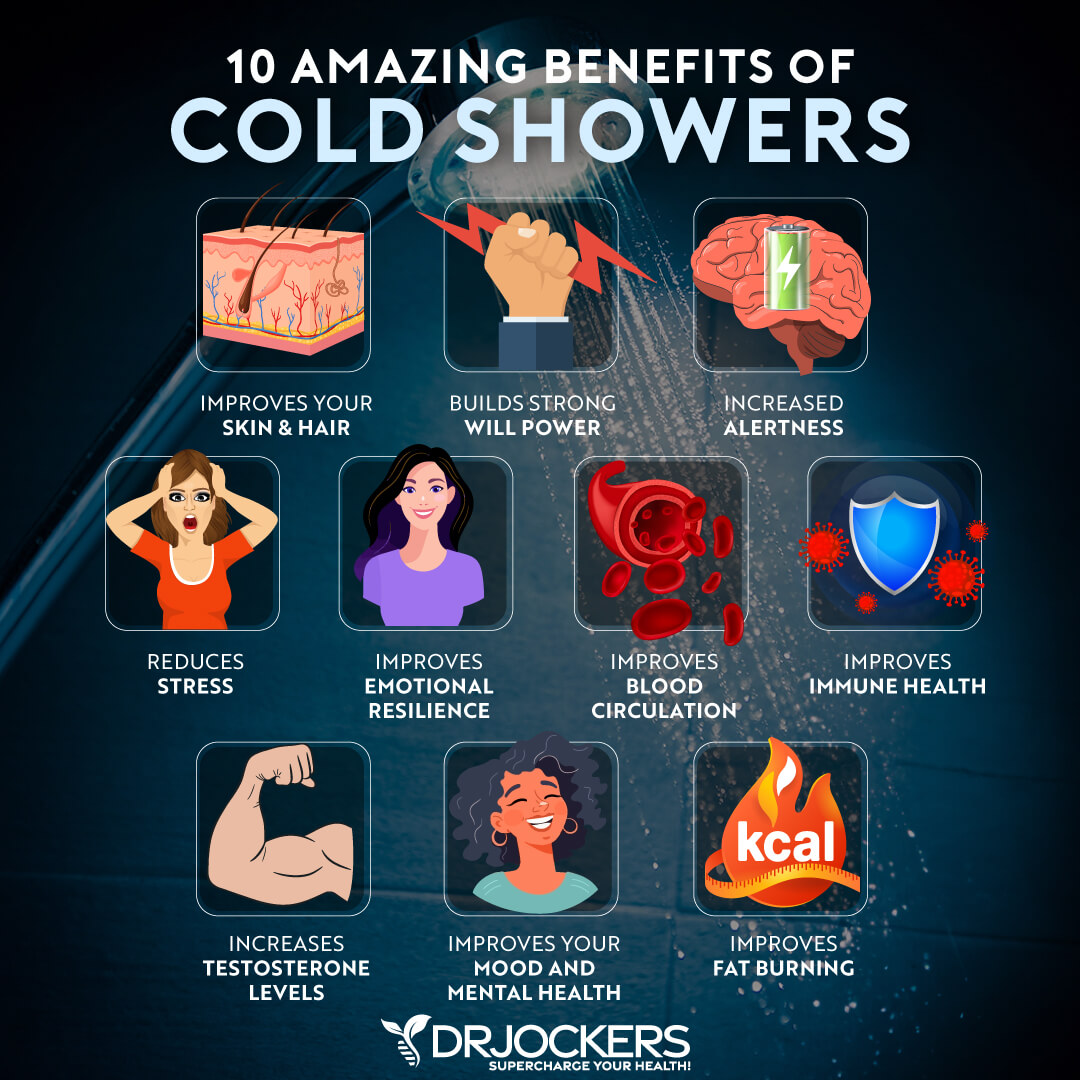
Cold Water
Cold water is one of the simplest ways to stimulate your vagus nerve and improve your vagal tone. Research has found that exposure to cold water may bring observable results.
While taking a cold shower or immersing in a cold pool is one of the best ways to experience benefits, you don’t have to start with that if you are not used to cold water exposure. Start with washing your face with cold water then slowly move up to taking a 30-second cold water shower (34). Most people find that it is easiest to do a warm shower and finish with 30–60 seconds of cold water at the end.
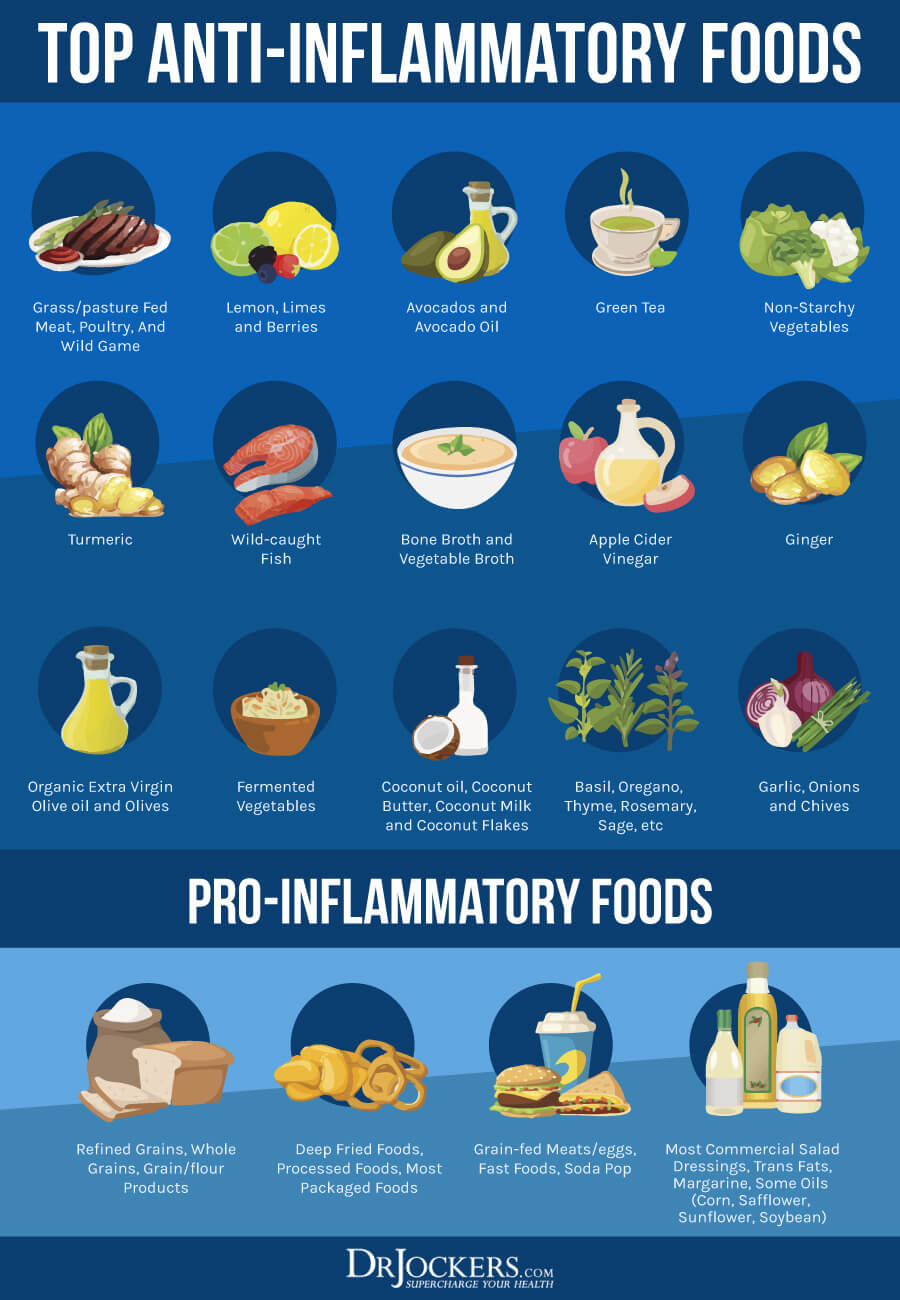
Anti-Inflammatory Nutrition Plan
Eating an anti-inflammatory diet rich in nutrient-dense foods is very critical for supporting your physical and mental health. An anti-inflammatory nutrition plan supports your gut health, which is important because your gut is closely connected to the health of your nervous system. It also offers nutrients that support healthy nervous system function, help to reduce symptoms of stress, and lower inflammation.
First, cut out all inflammatory foods, including refined sugar, gluten, refined oils, deep-fried and processed foods, conventional dairy, grain-fed meat and eggs, soda and sugary drinks, and foods that you are sensitive to. Instead, focus on an anti-inflammatory nutrition plan and load up on greens, vegetables, low glycemic index fruits, herbs, spices, fermented foods, healthy fats, grass-fed meat, and wild-caught fish. To learn more about an anti-inflammatory diet, read this article as well (35, 36, 37, 38, 39, 40, 41, 42, 43, 44).
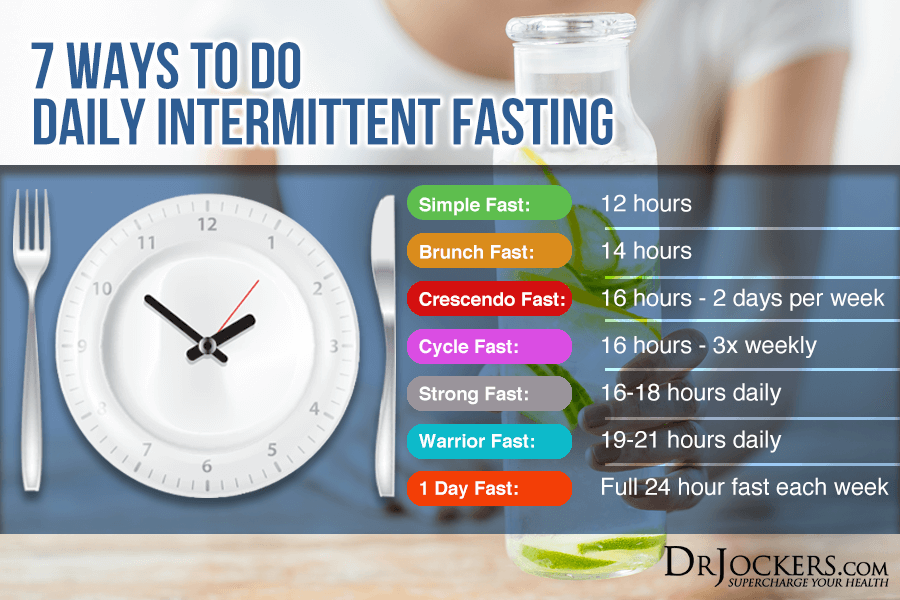
Intermittent Fasting and Vagal Tone
Intermittent fasting is a type of fasting that cycles between not eating (fasting) and eating (feasting) over a period of time. The benefits of intermittent fasting include cellular repair, increased autophagy, immune regulation, decreased, inflammation levels, lower inflammation, better insulin sensitivity. It also helps to reduce your risk of chronic diseases, including neurodegenerative conditions and mental health issues.
If you are new to intermittent fasting, I begin with the Simple Fast. The Simple Fast includes 12 hours of fasting including your overnight sleep. Increase your fasting window gradually. Most people feel the most benefits at a 16-hour fasting window. To learn more about the benefits of intermittent fasting and best intermittent fasting practices, I recommend this article (45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57).
Improve Gut Health For Better Vagal Tone
Your gut and nervous system are closely connected. Poor vagal tone can disrupt your gut health and digestion. Poor gut health on the other hand has negative effects on your nervous system and vagal tone. Improve your gut health by removing inflammatory foods and eating gut-friendly, anti-inflammatory, and nutrient-dense diets abundant in veggies, healthy fats, clean protein as I explained earlier. Probiotics are incredibly important for good gut bacteria balance.
However, you cannot forget about prebiotics either that feed the good bacteria and support your gut health. For many people, it is beneficial to eat plenty of prebiotic-rich foods, including onion, garlic, leek, asparagus, and Jerusalem artichokes, and probiotic-rich foods, such as sauerkraut, kimchi, and kefir.
Some people seem to feel better as a whole on a diet with less fiber and prebiotics and more protein and fat. Experiment and find what works best for you. For additional support, I recommend taking a daily probiotic supplement.
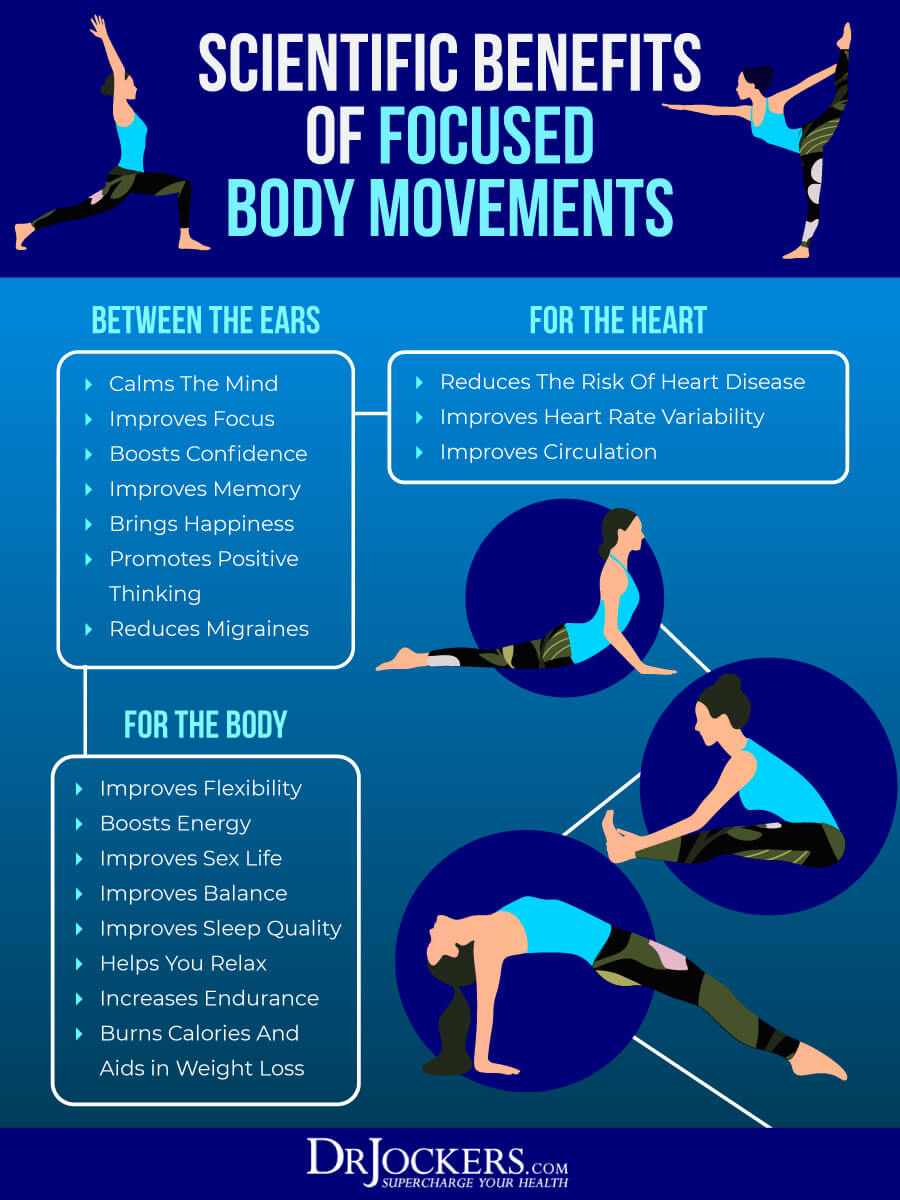
Movement and Exercise
Regular movement and exercise are absolutely essential for the health of your nervous system. Movement and exercise help to release energy and tension from your body, help you to move out of flight-or-fight mode, increase endorphins, and boost your mood. Start your day with a short stretch or yoga routine, some grounding, and maybe a loop around the block. Move throughout the day by strolling down the park during lunch, stretching regularly, walking your dog, and playing with your kids.
Exercise for 20 to 30 minutes at least five times a week. In the beginning this may just mean taking a walk. Over time as you get healthier, you should challenge yourself with resistance training and other exercises to get your heart rate up. High-intensity interval training (HIIT) is a great way to fit some cardio and strength training to your day within a short time. Add lower impact workouts, including pilates, Barre workouts, or yoga. End your day by stretching out.

Movement Therapies
If you experience something stressful or scary and find yourself in flight-or-fight mode, you may release energy by shaking out your arms and legs, doing a little dance, running around the block, bouncing on the trampoline, or doing something physical while being mindful of this release of energy to return to a calm, safe, and connected state with a healthy vagal tone. It is best if you are being very mindful and intentional when releasing energy from your body to get back to a safe, connected state, instead of distracting yourself with music or other thoughts.
To improve your vagal tone, you may employ various body-based somatic exercises and therapies. Yoga therapy has shown wonderful benefits for trauma therapy and mental health and may be a complementary part of polyvagal therapy. Nia, 5rhythm dancing, ecstatic dance, Quia, and embody dance helps to stimulate the vagal tone, allow emotional release, and help create safety within the body.
Somatic experiencing is a body-based therapy that allows your body to release tension and trauma and recreate safety and connection. Tension, stress and trauma relief (TRE) therapy helps your body to release tension and calm the nervous system through therapeutic muscle tremors.
Both somatic experiencing and TRE has been shown to help with symptoms of PTSD and trauma. You may find other trauma-informed therapists that can help you with other somatic and mind-body-based strategies to support your vagal tone through body movement (58, 59, 60, 61, 62, 63, 64, 65, 66, 67).
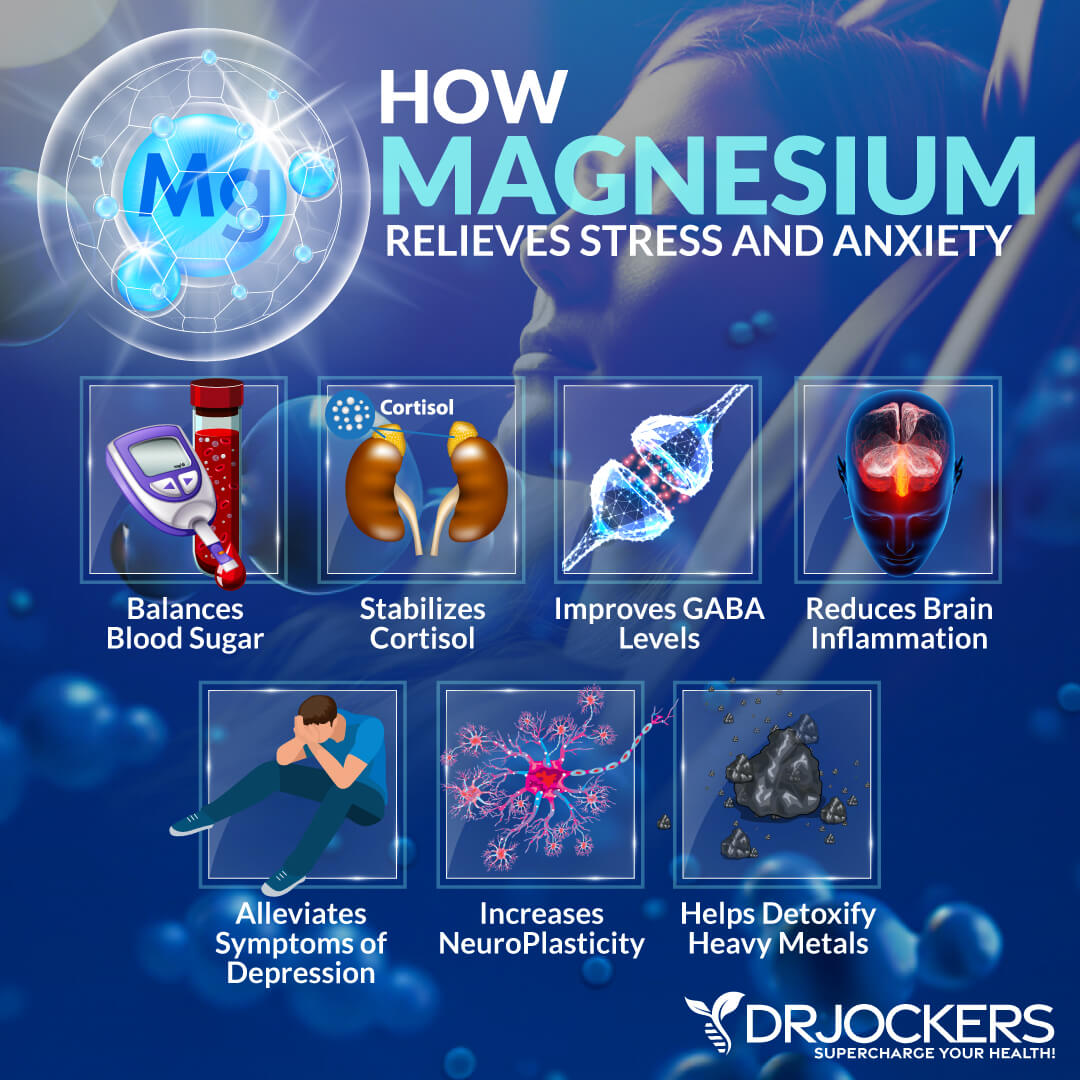
Use Magnesium & Zinc
Magnesium and zinc are critical for neurological health, brain health, mental health, stress relief, and relaxation. Research has shown its potential benefits for traumatic brain injury, depression, anxiety, and other mental health issues. Studies have also shown the potential benefits of zinc for depression, psychosis, other mental health issues, and neurological conditions.
Magnesium-rich foods include almonds, spinach, avocados, kale, pumpkin seeds, sunflower seeds, and cashews. Zinc-rich foods include eggs, oysters, lamb, cashews, turkey, pumpkin seeds, and sesame seeds.
However, eating magnesium-rich and zinc-rich foods is usually not enough to optimize your health, especially if you have deficiencies or signs of vagal tone issues. I recommend Brain Calm Magnesium and Zinc Charge to help healthy nerve conduction, neurological function, energy production, mood, and mental health (68, 69, 70, 71, 72).
Use Adaptogenic Herbs
When you are in a flight-or-fight state or experiencing chronic stress due to poor vagal tone, your cortisol levels are running high. It is difficult to return to a calm state with chronically high cortisol levels. This is why I recommend Cortisol Defense.
It is a natural stress buster supplement made with adaptogenic herbs, such as Magnolia officinalis, ashwagandha, L-theanine, banaba leaf, and maral extract that help to reduce stress, promote mental clarity, and support restful sleep and relaxation. Take one capsule twice a day, in the morning and before bed, or for advanced use, take two capsules twice a day.
Use The Brain Tap System
The Brain Tap System is a brilliant system that helps to restore your brain’s natural ability to balance. It helps to soothe your brain. It enhances relaxation and revitalization. This system activates the vagus nerve and provides you with a range of brain waves to achieve balance.
It is an incredibly quick easy, and effective way to improve your brainwaves, lower stress, feel calm and controlled, improve cognition, experience more energy, and positivity, and feel overall healthier. Only 10 to 20 minutes a day can make a tremendous difference in your brain health, mental health, energy, and physical well-being.
Bonus Strategies For Improving Vagal Tone
There are a few other bonus strategies that you may try. Here is what I recommend:
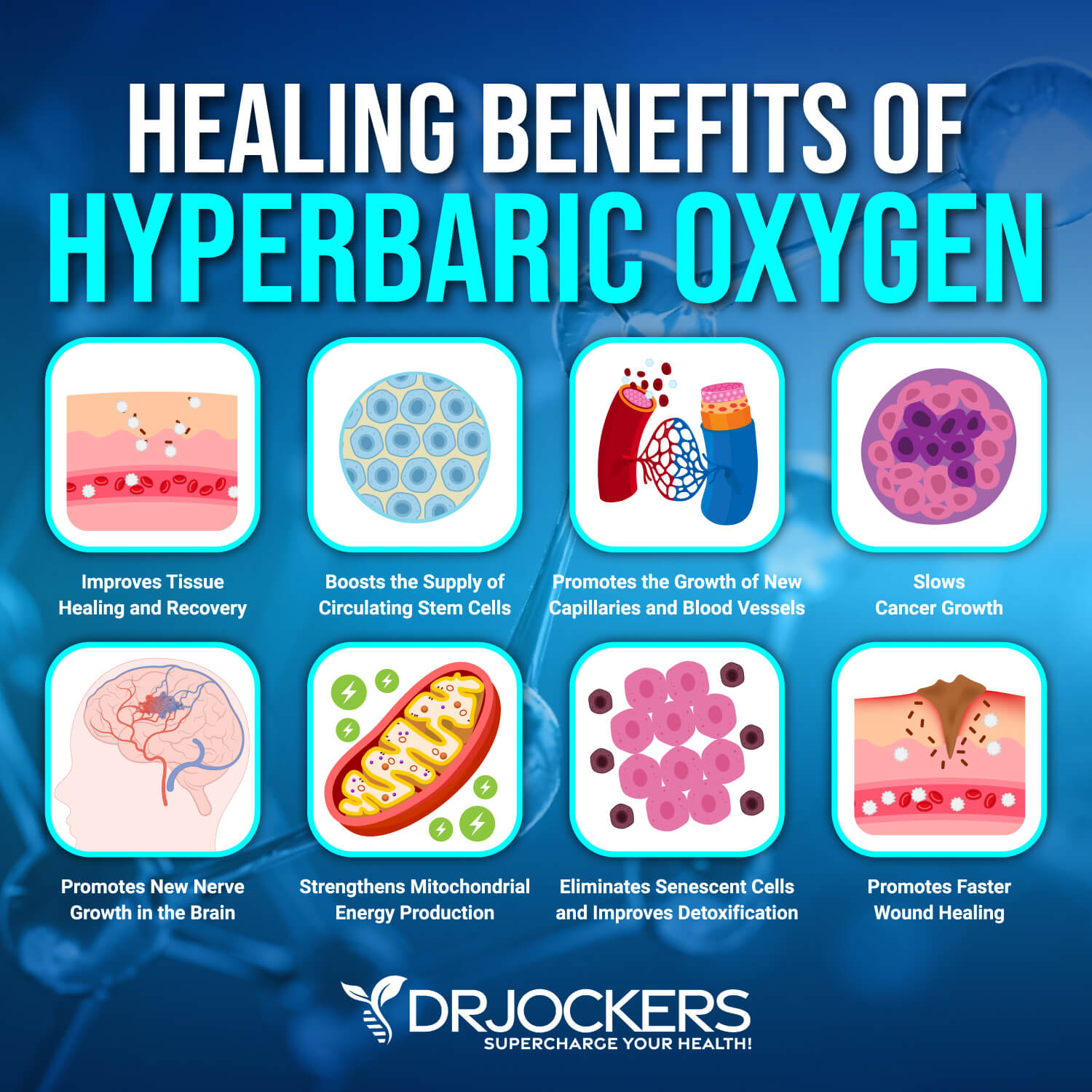
Hyperbaric Oxygen
Hyperbaric oxygen therapy has been used as a treatment for decompression sickness, a hazard of scuba diving. The hyperbaric chamber has pure oxygen coming in at pressures 1.5 – 3 times the normal atmospheric pressure. Treatment times range from 30–90 minutes.
Using oxygen at higher pressures causes up to 20 times more oxygen to be absorbed by the blood and transferred to injured organs and tissues. It may be a fantastic treatment for brain health. Research has shown that hyperbaric oxygen may help to reduce heart rate, improve heart rate variability, and support vagal nerve function (73).
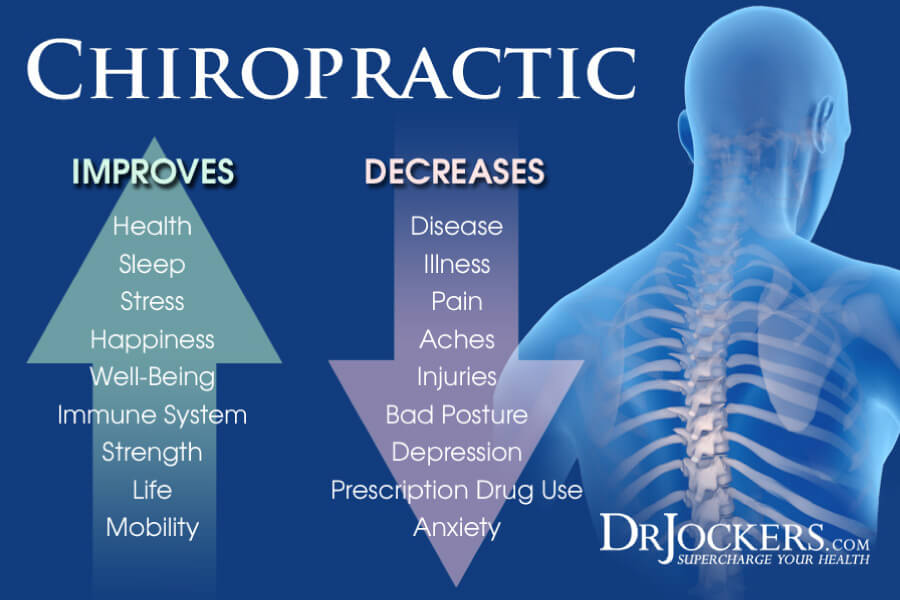
Chiropractic, Massage & Acupuncture Therapies
Chiropractic, massage, acupuncture, and craniosacral therapy may also help to improve your vagal tone. Chiropractic care specializes in neuromuscular health and uses adjustments to your spine and eliminates misalignments in the spine that may be causing physical, neurological, or even emotional health problems. It may help to improve your heart rate variability and vagal tone (74).
Massage therapy works with your muscles and helps to relieve tension. It may help to reduce stress, inflammation, and pain, and help to recreate safety in your body and emotional state. Massaging certain areas of your body may be particularly good for vagal stimulation (75).
Craniosacral therapy is a form of alternative therapy that helps balance and heal with a gentle touch to palpate the synarthrodial joints of the cranium. Somato-Emotional Release (SER) is a form of craniosacral therapy that is particularly beneficial for emotional release of emotions and trauma stored in your body. It helps to improve the social nervous system, improve vagal tone, inhibit the SNS, address the cranial nerves, and regulate the entire nervous system (76).
Acupuncture is a form of traditional Chinese medicine, an alternative healing method in which thin needles are inserted into the body to recreate balance and allow healing. It helps to stimulate the vagus nerve, regulate the nervous system, and reduce inflammation (77).
Additionally, if you need further personalized support, especially if you’ve experienced abuse or other trauma, you can find a trauma-informed therapist who is well-versed in polyvagal therapy and somatic techniques. They can offer a safe space and personalized support to heal.
Final Thoughts on Vagal Tone
Your vagus nerve is one of the most important nerves that are responsible for many important functions, including regulating your heart rate, breathing, blood pressure, digestion, and emotional state.
Some common symptoms of poor vagal tone include anxiety, depression, stress, fatigue, inflammation, irregular heart rate, digestion issues, or any emotional health symptoms. If you experience these symptoms, it may mean that you have a poor vagal tone, and your vagus nerve needs some care. I recommend that you follow my simple natural strategies to improve your vagal tone for better mental and emotional health.
Inflammation Crushing Ebundle
The Inflammation Crushing Ebundle is designed to help you improve your brain, liver, immune system and discover the healing strategies, foods and recipes to burn fat, reduce inflammation and Thrive in Life!
As a doctor of natural medicine, I have spent the past 20 years studying the best healing strategies and worked with hundreds of coaching clients, helping them overcome chronic health conditions and optimize their overall health.
In our Inflammation Crushing Ebundle, I have put together my very best strategies to reduce inflammation and optimize your healing potential. Take a look at what you will get inside these valuable guides below!



A most excellent article, my dear friend! This is very informative & essential knowledge. Love the simple terms used, as well as the charts. One of the best single pieces I have read on the subject. This is an area I have been addressing in myself, having come to understand a bit about the vital role of the vagus nerves in so very many common health issues. I just wish all my loved ones would be willing to read this & follow through on suggestions. Addressing vagal tone is the missing piece for so very many people for so very long a time (myself included) Again, thanks!!
Great to hear that!
Congratulations. This is the best written and comprehensive article on a the subject. You will help so many people who absolutely must learn this information in order to heal and live well.
Wow! I’m an Energy Psychologist who has been increasingly focusing on helping others to both understand and improve their functioning to increase resilience and aliveness. I stumbled on this just now in doing a search for my newsletter and am amazed and oh so grateful for all that you have put together here. People will be receiving this from me for a long time. Thank you again! Holly Timberlake, Ph.D.
Thank you Holly! Blessings!
Thank you so much for this wonderful article. I recognized myself in it and found why I usually get these symptoms in time of holidays, too much sweets and carbs. I will like to add that eyes exercise help a lot.
Thanks for sharing and we appreciate your support. Blessings!
Thank you very much, this is a very interesting article.
I had my vagus nerve cut in 1972, in an American Hospital in Belgium. They did this because I had a duodenal ulcer!
I now have very high blood pressure which is proving very difficult to control and a high heart rate. I have Sjogren’s Syndrome (auto immune) and have put myself on the type of diet you were recommending, as I became gluten intolerant and very poorly.
I am now wondering if all this was because of my vagus nerve, and would like to ask you if there is anything that can be recommended. Thank you very much Jean.
Yes vagal nerve dysfunction can contribute to many health problems in the body! We are praying for fast healing for you!
This a truly excellent, complete and right on the mark. Boy oh Boy if
we only learned this in school, we would have no need for “all-pathetic medicine”. Let food be your medicine and medicine your food. You captured it all and very doable when we are educated. Thank you for sharing your knowledge and wisdom for the ages.
Thank you Monik! Blessings!
Thank you, Dr. Jockers, for your work. What are your thoughts on vagus nerve detoxifying creams that supposedly stimulate and open the vagus nerve?
I think it is possible they may have some benefit.
I tested out the heart rate to Breath rate comparison and it doesn’t make much sense to me. My heart rate today was 82, breath rate 7 breaths/min. 82/7 is a 12:1 ratio. To reach the 5:1 recommended ratio, either my pulse has to be 35 or I have to breathe 16 times/min, both of which don’t seem realistic on a regular basis 😲
Very nice article sir
Thank you!
I have a wonderful ten year old who has been diagnosed with PTSD type symptoms brought on by 2 years of continued worry over Covid/Lockdown he is very slowly getting better but sadly his anxiety levels are off the scale and he cannot do a full day at school after 2 months. I have thought there is a physiological reason behind his changing behaviour and this article has been an absolute god send to read. Thank You. I’ve suspected there may be a link with diet and sleep, on top of Covid/lockdown fears. Is there anything you can recommend for the little people out there.
Sorry to hear about this! Yes, I would recommend the NDF Happy product here: https://store.drjockers.com/products/ndf-happy
Forge on, ( top comment). You took the words right out of my mouth. !!! thankyou Dr J. So very much appreciated. The simplicity but effectiveness, the drawings, the way its written, etc etc etc, 100 out of 100. Cheers kiwi girl. Gonna beat this vagal bad boy and tinnitus.
Thanks so much TJ!
i love the information you gave and your infographics as well 😀
Thank you and blessings to you!
I truly believe the combination of whiplash, concussion and great emotional trauma triggered autoimmune disease (Hashimoto’s). What recommendations would you have for managing or even reversing?
Yes absolutely, here is some helpful info for you: https://drjockers.com/hashimotos-thyroiditis/
Dr. Jockers,
I have a 22 y/o son who started stuttering in the 4th grade. He just graduated from college and it has had a big impact on his personality going from being a loud extrovert to a quiet introvert. Do you think doing something with the vagus nerve could help?!
Yes this may be due to a lower functioning vagal tone. I would try the exercises and see if it helps.
Thank you so much for this article and your diagrams and pictures it has been really really helpful. I’ve been trying to learn more about The vagus nerve and this was Very very helpful especially with the things that we can implement right away. Thank you for your continued work
Jennifer
Glad to hear this!
Dear Dr Jockers,
I am doing a certificate program in Self-Reg in Early Childhood with Dr Stuart Shanker and Susan Hopkins. Our Module this week is on ‘Temperament’ and the presenters speak of the influence of The Vagul Tone. I would like to ask your permission to share this article in my course with all the students. It is very clear and easy to understand.
Thank you ☺️